Abstract
Evidence from both epidemiological and experimental observations has fuelled the belief that the high consumption of fruits and vegetables rich in nutrients and phytochemicals may help prevent cancer and heart disease in humans. This concept has been drastically simplified from the dietary approaches to the use of single bioactive components both as a single supplement or in functional foods to manipulate xenobiotic metabolism. These procedures, which aim to induce mutagen/carcinogen detoxification or inhibit their bioactivation, fail to take into account the multiple and paradoxical biological outcomes of enzyme modulators that make their effects unpredictable. Here, we show that the idea that the physiological roles of specific catalysts may be easily manipulated by regular long-term administration of isolated nutrients and other chemicals derived from food plants is not viable. In contrast, we claim that the consumption of healthy diets is most likely to reduce mutagenesis and cancer risk, and that both research endeavours and dietary recommendations should be redirected away from single molecules to dietary patterns as a main strategy for public health policy.
1. Introduction
Strategies for cancer prevention necessarily focus on eliminating unhealthy lifestyle habits such as alcoholism or cigarette smoking or improving both diet and exercise patterns which are believed to contribute to about one-third of annual cancer deaths worldwide [1–4]. Over the last decades, accumulating epidemiological evidence and animal investigations have suggested that consumption of a diet rich in food plants significantly reduces the risk of several types of cancers and recent recommendations point to plant-based diets [5–7]. This raises the theoretical possibility that such protective effects could be attributed to specific micronutrient or phytochemical constituents of food plants and that such components might have beneficial effects in the field of cancer chemoprevention either as naturally occurring dietary constituents/pharmaceuticals or in functional foods [8–10].
It has been speculated that they could manipulate the activity of metabolic enzymes that break down chemical mutagens and carcinogens to reduce lifetime cancer risk. It is indeed widely believed that the postoxidative enzymes (also, i.e., phase II enzymes), such as glutathione S-transferase, UDP-glucuronosyl transferase, sulphotransferase, and acetyl transferase, are able to promote health by detoxifying xenobiotics. On the contrary, the oxidative enzymes (e.g., phase I), represented mainly by the superfamily of cytochrome P450 (CYP) and FAD-containing monooxygenases, raise cancer risk by the bioactivation of ubiquitous mutagenic compounds [11–17]. This rather simplistic dichotomy has in turn suggested that food plant-derived nutrients or phytochemicals might be employed to reduce the risk of cancer through two enzyme-based strategies such as boosting the “good” detoxifying phase II enzymes (using, for example, representative phytochemical-containing fruits and vegetables such as grapes, cauliflower, kale, and broccoli), or inhibiting the “bad” activating phase I enzymes (using those contained in garlic, tea, and onion).
We must remember here that these strategies were extrapolated from epidemiological observations on populations consuming diets varying in both quantity and type of food plant containing thousands of chemical agents which are able to modulate the specific activity of the metabolizing enzyme battery in a very complex way. They have been popularized by the media and exploited by marketers of supplements of phytochemicals and desiccated vegetables labelled as containing suitable amounts of detoxifying enzyme modulators.
However, this approach totally fails to address the complexity of the multiple interactions between dietary components and xenobiotic metabolism simultaneously generating health benefits or harmful outcomes, depending on circumstances that cannot yet be predicted. Consequently, the potential effects of whole-food plant-derived single constituents on xenobiotic metabolism and cancer risk are also uncertain.
2. The Metabolic Manipulation Approach
This modulation strategy foresees large-scale induction of postoxidative phase II enzymes that “detoxify” xenobiotics by means of single green constituents, thereby accelerating the clearance of mutagens and protecting cells against cancer. The potential benefits of this strategy have stimulated active in vitro and in ex vivo studies on the molecular mechanism and specificity of such chemical compounds [18–23]. Particular attention has been devoted to cruciferous vegetables of the Brassica genus, such as kale, cabbage, broccoli, Brussels sprouts, and cauliflower. These vegetables contain considerable amounts of glucosinolates which are the precursors (via the enzymatic conversion by the enzyme myrosinase) of isothiocyanates [24–26], which are phase II enzyme inducers [27–30]. Some researchers have actually created hybrid plants specifically to produce higher amounts of single phytochemical inducers [31]. Resveratrol, a phytoalexin found in grapes and other food products, is also able to boost postoxidative-linked activities [23], but many other compounds contained in plants could be cited.
An alternative anticancer approach is to inhibit the oxidative “bioactivating” phase I enzymes [12, 13]. This hypothesis is emphasized by both the scientific literature and the media, as exemplified by numerous reports urging regular consumption of green or black tea containing catechins as well as onion and garlic rich in diallyl sulfide [32–34].
Finally, both proposed strategies also must be considered in the context of genetic metabolic polymorphisms, which may differentially, per sè, modulate the effects of any one dietary factors on individuals.
3. The Limitations of Such Strategies
We would like to point out that the main difficulty with these strategies is that they totally ignore the complexity of metabolizing enzymatic machinery. Indeed, if on one hand the consumption of food plants, which contain thousands and thousands of phytochemicals (an apple, e.g., seems to contain more than 700 chemical compounds, and a simple fruit salad?) is linked to a reduced cancer risk, on the other, the induction of xenobiotic metabolism by one specific food component may also stimulate the unwanted formation of highly reactive mutagens [35, 36]. The use of single naturally occurring dietary constituents such as isothiocyanates or individual drugs such as disulfiram, oltipraz, or food additives such as BHA [2(3)-tert-butyl-4-hydroxyanisole], for example, also elicits unhealthy effects [37–40].
It should be pointed out that in addition to the increase in xenobiotic clearance, each postoxidative (phase II) enzyme is also involved in electrophilic species generation and, therefore, must be considered as a “bioactivating system” for specific chemical classes such as halogenated hydrocarbons by glutathione S-transferases, for example, or polycyclic aromatic hydrocarbons (PAHs) by sulphotransferases [41–64]. So, the activation or inactivation of a compound depends on the chemical nature of the compound itself and not on the metabolic enzyme involved. More in general, the manipulation of the activity of one or more phase II enzyme can either increase or reduce the bioactivation of specific compounds. Whereas induction increases the detoxification of some promutagens, thereby favoring chemoprevention, it also increases the bioactivation of countless other foreign chemicals to which humans are simultaneously exposed. As the population is exposed to a myriad of potentially harmful molecules, any modification of the activity of these enzymes could actually lead to unexpected dangerous effects [40]. For example, cruciferous isothiocyanates such as the sulforaphane, widely considered as a beneficial phase II inducer, turn out to be genotoxic or a strong promoter of urinary bladder and liver carcinogenesis, also inducing cell cycle arrest and apoptosis [65–67]. Similarly, engineered Salmonella typhimurium TA1535 transfected with the plasmid vector pKK233-2 containing rat glutathione S-transferase 5-5 cDNA has been shown to activate many genotoxicants, whereas the nontransfected counterpart does not [68]; in addition, heterologous expression of mammalian theta class glutathione transferases in S. typhimurium and Escherichia coli systems has been used to demonstrate the role of glutathione conjugation in the genotoxicity of dihalomethanes [61, 69]. Paradoxically, liver metabolic S9 fractions isolated from rodents treated with the monofunctional postoxidative inducer BHA have been proposed as a “complementary” S9 metabolizing system to bioactivate pro-mutagens in typical short-term mutagenicity bioassays [70].
Similar considerations should be made for the inhibitory strategy, a hypothesis that has stimulated recommendations to increase, for example, consumption of green and black teas, as they contain phytochemicals such as catechins able to inhibit the oxidative (phase I) enzymes thus reducing the production of mutagens and carcinogens such as N-nitroso compounds [13, 71]. The inhibition of dimethylhydrazine-induced colon cancer by diallyl sulfide, a flavour component of garlic (Allium sativum), has encouraged garlic consumption increase [72, 73]. Moreover, the flavonoid naringin, present in grapefruit and related citrus fruits, has been found to inhibit aflatoxin B1 activation by CYP3A4 in cells and animal models supporting the general idea that green-based metabolism inhibition may reduce carcinogenesis risk [74].
The concept of metabolic manipulation, however, ignores the simple fact that the “institutional” role of CYP superfamily toward xenobiotics is to promote their detoxification from the cells and body as well [75]: it is our misfortune that some of them are bioactivated. In other words, due to the dual beneficial and detrimental nature of any of the P450 enzymes, the reduced activation of certain toxins occurs simultaneously with the reduced detoxification of other environmental toxicants to which humans are exposed daily, a phenomenon clearly unpredictable. Once again, it should be noted that the bioactivation of chemicals by phase I apparatus, as occurs for phase II ones, depends on the nature of the substance itself and not on the involved enzyme. Of course, as it is impossible to select safe, personalized human exposure levels to environmental toxins in such a way as to systematically avoid harmful compounds, the regular inhibition of oxidative enzymes might actually lead to an increase toxicological risk. In addition, it should take into account that a selective inhibitor of one CYP enzyme (and due to the existence of many CYP isoforms this strategy should foresee the use a cocktail of multiple inhibitors) may be an inducer of other CYPs; for example, phenethyl isothiocyanate derived from Brassica and diallyl sulfide from garlic are able to inhibit CYP2E1 but also induce CYP2B1 and CYP1A2 [76].
Paradoxically, in 1985 when Wattenberg proposed chemoprevention strategies [12], including the ones that foresee the above mentioned manipulation of metabolic (according to the belief that they are classified as “bad-phase I” and “good-phase II”) enzyme activities, Guengerich published a comprehensive review on the “dual bioactivating and detoxifying nature” of each metabolic enzyme regardless of whether belongs to the phase I or II battery (Figure 1) [41].
Figure 1.
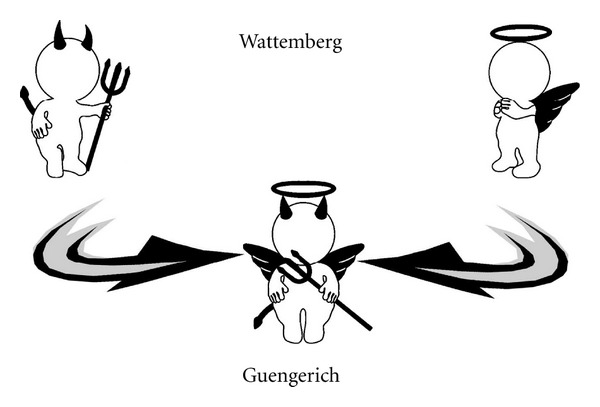
Allegoric representation of main difference between classic theory and data emerging from scientific literature. Since 1985 Wattenberg proposed chemoprevention strategies, including the ones that foresee the above mentioned manipulation of metabolic (according to the belief that they are classified as “bad-phase I” and “good-phase II”) enzyme activities, and Guengerich published a comprehensive review that suggested the “dual bioactivating and detoxifying nature” of each metabolic enzyme regardless of whether belongs to the phase I or II battery. The last theory (Guengerich) seems the correct ones, since the data emerging from scientific literature.
Not least, the use of enzyme activity modulators can lead to other serious unhealthy consequences stemming from the alteration of endogenous metabolism where these catalysts are involved (e.g., arachidonic acid derivatives, nitric oxide, aldosterone, cholesterol, or vitamins) as well as alteration of fundamental physiological functions (growth, differentiation, apoptosis, homeostasis, and neuroendocrine functions) [77]; the effects on the pharmacokinetics of coadministrated drugs should not be overlooked as well.
4. The Role of Metabolic Polymorphisms
The illogical effects of single daily consumed dietary constituents on xenobiotic metabolism are further complicated by genetic (metabolic) polymorphisms that lead to the occurrence of high- or low-metabolizer phenotypes in the population, each at increased toxicological risk from exposure to specific chemicals [78, 79]. The multiple polymorphisms (e.g., occurrence of high or low (or intermediate in some cases) metabolizers for any oxidative or postoxidative isoforms) characterizing the so called “individual metabolic fingerprint” further complicate the issue. This phenomenon can indeed be interpreted as a sort of a “constitutive up- or down-regulation” of any phase I or II dependent enzyme. In other words, the infinite number of possible combinations of human genetic metabolic polymorphisms constitutes another set of variables in the xenobiotic metabolism [80]. Thus, it appears even more clear that the possibility of manipulating enzyme activity, which in its “constitutive” diversity already may determine genetic disorders as well as perturbations on the chemical biotransformation (including drugs), raises further questions about the effectiveness of the chemical-based enzymatic modulation of cancer risk [81, 82]. In our opinion, these considerations suggest the need for considerable caution before allowing for any form of enzyme-activity manipulation for a generalized prevention, particularly in healthy individuals.
5. On the Clinical Significance
What is the clinical significance of the perpetual manipulation of such enzymatic systems by single nutrient or phytochemicals? Summarizing the various aspects depicted above, the scenario that arises shows how both oxidative and postoxidative enzymes are highly multifunctional and can be induced or inhibited or both by a great number of dietary components. Noteworthy, is the often ignored existence of the dual activating and detoxicating nature of these enzymatic systems. So, the impressive number of chemical compounds that can modulate them, the presence in greens of chemicals that induce both activation and inhibition of mutagenesis, the genetically determined interindividual variability that may moderate (increasing and/or inhibiting) the effects of specific dietary factors on any metabolic enzyme, and the complexity of the interactions among food constituents and enzyme systems have fed the ongoing debates as to whether phytochemicals can alone explain the anticancer ability of plants [9, 83].
It is very difficult to imagine how a single phytochemical, today selected as representative of this or that green, such as lycopene in tomato, resveratrol in grapes, sulforaphane in broccoli, and beta-carotene in carrots, used as a food supplement would offer an advantage, since a variety of fruit and vegetables seems necessary to provide the mixture of vitamins and minerals that appear to favour protection against neoplasia [84]. How can we imagine that the beneficial effects of consuming entire fruits and vegetables, in which enzyme modulating components appear in varying amounts and proportions, and in which unpredictable synergistic and antagonistic (or both depending on the enzyme involved) interactions occur among thousands of different chemicals in their natural matrix, could be just reproduced by supplements of single representative phytochemicals? [85] The beneficial or harmful outcomes of a single compound (portio facit venenum, Paracelso) can be quite different from those elicited by the same compound within complex mixtures (portio and interactiones faciunt venenum) [86].
The fact that a great number of clinical investigations using single “natural” components failed to reproduce the beneficial effects of the plants from which they were derived should not be underestimated. For example, we can cite the “unexpected” results of cancer chemoprevention trials of antioxidant provitamins and vitamins which we believe can constitute an exemplary warning about the vulnerability of single-nutrient strategies [87–90]. Beta-carotene administered alone or in combination with Vitamins A, E, or C for the prevention of lung cancer and other cancers in heavy smokers or asbestos workers failed to reduce cancer risk and, in some cases, actually increased the risk, raising the suspicion that single chemical supplements may have harmful and beneficial effects as well [91–93]. It has been documented that the deleterious effect of beta carotene can be linked to its ability to stimulate the metabolizing machinery, such as activators of polycyclic aromatic hydrocarbons, and to generate an oxidative stress [94]. In addition, supplementation with commercial doses of vitamin C for 6 weeks is enough to induce DNA damage in human lymphocytes [95], probably by means of its ability to generate oxidative stress connected to phase I upregulation [96, 97].
6. Concluding Remarks
In the field of cancer prevention, the idea of producing the so called “magic-bullet,” as conceived by Paul Ehelich for antibacterials, too easily evokes the long-life elixir on a molecular level capturing the imagination of both the public and researchers. From the standpoint of cancer research policy, the possible role of single dietary constituents is of pivotal interest in cancer research but basic information about the role of metabolizing apparatus, however, makes it clear that the role of any single anticarcinogenic phytochemical cannot be understood except in the context of broader dietary patterns. The ongoing scientific controversy surrounding the effects of single molecules on cancer risk seems to provide a salutary warning for health policymakers. Considering that unhealthy lifestyle factors are also taken into account, educational campaigns encouraging the consumption of fruit, fibres, and greens should be encouraged.
Acknowledgment
Financial support from MIUR (Rome) is gratefully acknowledged.
References
- 1.Bailar JC, Gornik HL. Cancer undefeated. New England Journal of Medicine. 1997;336(22):1569–1574. doi: 10.1056/NEJM199705293362206. [DOI] [PubMed] [Google Scholar]
- 2.McGinnis JM, Foege WH. Actual causes of death in the United States. Journal of the American Medical Association. 1993;270(18):2207–2212. [PubMed] [Google Scholar]
- 3.Wicki A, Hagmann J. Diet and cancer. Swiss Medical Weekly. 2011;141 doi: 10.4414/smw.2011.13250.13250 [DOI] [PubMed] [Google Scholar]
- 4.Khan N, Afaq F, Mukhtar H. Lifestyle as risk factor for cancer: evidence from human studies. Cancer Letters. 2010;293(2):133–143. doi: 10.1016/j.canlet.2009.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Cancer Research Foundation and American Institute for Cancer Research, Food nutrition and the prevention of cancer: a global perspective, World Cancer Research Foundation and American Institute for Cancer Research, Washington, DC, USA, 1997.
- 6.Woyengo TA, Ramprasath VR, Jones PJH. Anticancer effects of phytosterols. European Journal of Clinical Nutrition. 2009;63(7):813–820. doi: 10.1038/ejcn.2009.29. [DOI] [PubMed] [Google Scholar]
- 7.American Cancer Society Advisory Committee on Diet. Nutrition and cancer prevention. CA Cancer Journal for Clinicians. 1996;46:325–341. doi: 10.3322/canjclin.46.6.325. [DOI] [PubMed] [Google Scholar]
- 8.Nestle M. Dietary recommendations for cancer prevention: public policy implementation. Journal of the National Cancer Institute. Monographs. 1992;(12):153–157. [PubMed] [Google Scholar]
- 9.Nestle M. Broccoli sprouts as inducers of carcinogen-detoxifying enzyme systems: clinical, dietary, and policy implications. Proceedings of the National Academy of Sciences of the United States of America. 1997;94(21):11149–11151. doi: 10.1073/pnas.94.21.11149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saldanha SN, Tollefsbol TO. The role of nutraceuticals in chemoprevention and chemotherapy and their clinical outcomes. Journal of Oncology. 2012;2012:23 pages. doi: 10.1155/2012/192464.192464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peto R, Doll R, Buckley JD, Sporn MB. Can dietary beta-carotene materially reduce human cancer rates? Nature. 1981;290(5803):201–213. doi: 10.1038/290201a0. [DOI] [PubMed] [Google Scholar]
- 12.Wattenberg LW. Chemoprevention of cancer. Cancer Research. 1985;45(1):1–8. [PubMed] [Google Scholar]
- 13.Morse MA, Stoner GD. Cancer chemoprevention: principles and prospects. Carcinogenesis. 1993;14(9):1737–1746. doi: 10.1093/carcin/14.9.1737. [DOI] [PubMed] [Google Scholar]
- 14.Gerhäuser C, You M, Liu J, et al. Cancer chemopreventive potential of sulforamate, a novel analogue of sulforaphane that induces phase 2 drug-metabolizing enzymes. Cancer Research. 1997;57(2):272–278. [PubMed] [Google Scholar]
- 15.Shimada T. Xenobiotic-metabolizing enzymes involved in activation and detoxification of carcinogenic polycyclic aromatic hydrocarbons. Drug metabolism and pharmacokinetics. 2006;21(4):257–276. doi: 10.2133/dmpk.21.257. [DOI] [PubMed] [Google Scholar]
- 16.Dadali VA, Makarov VG. Biologically active substances from medicinal plants as a factor of the organism detoxication. Voprosy Pitaniia. 2003;72(5):49–55. [PubMed] [Google Scholar]
- 17.Vereczkey L, Jemnitz K, Gregus Z. Human drug metabolizing enzymes II. Conjugation enzymes. Acta Pharmaceutica Hungarica. 1998;68(5):284–288. [PubMed] [Google Scholar]
- 18.Prestera T, Holtzclaw WD, Zhang Y, Talalay P. Chemical and molecular regulation of enzymes that detoxify carcinogens. Proceedings of the National Academy of Sciences of the United States of America. 1993;90(7):2965–2969. doi: 10.1073/pnas.90.7.2965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kelloff GJ, Boone CW, Crowell JA, et al. New agents for cancer chemoprevention. Journal of Cellular Biochemistry. 1996;63(26):1–28. doi: 10.1002/jcb.240630703. [DOI] [PubMed] [Google Scholar]
- 20.Gerhauser C, You M, Liu J. Chemopreventive potential of a novel sulforaphane analog. The Proceedings of the American Association for Cancer Research. 1996;37, article A189 [Google Scholar]
- 21.Zhang Y, Kensler TW, Cho CG, Posner GH, Talalay P. Anticarcinogenic activities of sulforaphane and structurally related synthetic norbornyl isothiocyanates. Proceedings of the National Academy of Sciences of the United States of America. 1994;91(8):3147–3150. doi: 10.1073/pnas.91.8.3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Y, Talalay P. Mechanism of differential potencies of isothiocyanates as inducers of anticarcinogenic Phase 2 enzymes. Cancer Research. 1998;58(20):4632–4639. [PubMed] [Google Scholar]
- 23.Jang M, Cai L, Udeani GO, et al. Cancer chemopreventive activity of resveratrol, a natural product derived from grapes. Science. 1997;275(5297):218–220. doi: 10.1126/science.275.5297.218. [DOI] [PubMed] [Google Scholar]
- 24.Verhoeven DTH, Verhagen H, Goldbohm RA, Van Den Brandt PA, Van Poppel G. A review of mechanisms underlying anticarcinogenicity by brassica vegetables. Chemico-Biological Interactions. 1997;103(2):79–129. doi: 10.1016/s0009-2797(96)03745-3. [DOI] [PubMed] [Google Scholar]
- 25.Verhoeven DTH, Goldbohm RA, Van Poppel G, Verhagen H, Van Den Brandt PA. Epidemiological studies on Brassica vegetables and cancer risk. Cancer Epidemiology Biomarkers and Prevention. 1996;5(9):733–748. [PubMed] [Google Scholar]
- 26.Herr I, Büchler MW. Dietary constituents of broccoli and other cruciferous vegetables: implications for prevention and therapy of cancer. Cancer Treatment Reviews. 2010;36(5):377–383. doi: 10.1016/j.ctrv.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 27.Steinkellner H, Rabot S, Freywald C, et al. Effects of cruciferous vegetables and their constituents on drug metabolizing enzymes involved in the bioactivation of DNA-reactive dietary carcinogens. Mutation Research. 2001;480-481:285–297. doi: 10.1016/s0027-5107(01)00188-9. [DOI] [PubMed] [Google Scholar]
- 28.Lampe JW, Peterson S. Brassica, biotransformation and cancer risk: genetic polymorphisms alter the preventive effects of cruciferous vegetables. Journal of Nutrition. 2002;132(10):2991–2994. doi: 10.1093/jn/131.10.2991. [DOI] [PubMed] [Google Scholar]
- 29.Tan XL, Spivack SD. Dietary chemoprevention strategies for induction of phase II xenobiotic-metabolizing enzymes in lung carcinogenesis: a review. Lung Cancer. 2009;65(2):129–137. doi: 10.1016/j.lungcan.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barcelo S, Gardiner JM, Gescher A, Chipman JK. CYP2E1-mediated mechanism of anti-genotoxicity of the broccoli constituent sulforaphane. Carcinogenesis. 1996;17(2):277–282. doi: 10.1093/carcin/17.2.277. [DOI] [PubMed] [Google Scholar]
- 31.Faulkner K, Mithen R, Williamson G. Selective increase of the potential anticarcinogen 4-methylsulphinylbutyl glucosinolate in broccoli. Carcinogenesis. 1998;19(4):605–609. doi: 10.1093/carcin/19.4.605. [DOI] [PubMed] [Google Scholar]
- 32.Tadi PP, Teel RW, Lau BHS. Organosulfur compounds of garlic modulate mutagenesis, metabolism, and DNA binding of aflatoxin B1. Nutrition and Cancer. 1991;15(2):87–95. doi: 10.1080/01635589109514116. [DOI] [PubMed] [Google Scholar]
- 33.Hong JY, Smith T, Lee MJ, et al. Metabolism of carcinogenic nitrosamines by rat nasal mucosa and the effect of diallyl sulfide. Cancer Research. 1991;51(5):1509–1514. [PubMed] [Google Scholar]
- 34.Hernaez J, Xu M, Dashwood R. Effects of tea and chlorophyllin on the mutagenicity of N-hydroxy-IQ: studies of enzyme inhibition, molecular complex formation, and degradation/ scavenging of the active metabolites. Environmental and Molecular Mutagenesis. 1997;30:468–474. doi: 10.1002/(sici)1098-2280(1997)30:4<468::aid-em12>3.0.co;2-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Paolini M. Brussels sprouts: an exceptionally rich source of ambiguity for anticancer strategies. Toxicology and Applied Pharmacology. 1998;152(2):293–294. doi: 10.1006/taap.1998.8517. [DOI] [PubMed] [Google Scholar]
- 36.Paolini M, Legato MS. Healthy broccoli? Nature. 1992;357(6378):p. 448. doi: 10.1038/357448a0. [DOI] [PubMed] [Google Scholar]
- 37.Murakami A, Ohnishi K. Target molecules of food phytochemicals: food science bound for the next dimension. Food Function. 2012;3:462–476. doi: 10.1039/c2fo10274a. [DOI] [PubMed] [Google Scholar]
- 38.Brünen S, Vincent PD, Baumann P. Therapeutic drug monitoring for drugs used in the treatment of substance-related disorders: literature review using a therapeutic drug monitoring appropriateness rating scale. Therapeutic Drug Monitoring. 2011;33:561–572. doi: 10.1097/FTD.0b013e31822fbf7c. [DOI] [PubMed] [Google Scholar]
- 39.Pendyala L, Schwartz G, Bolanowska-Higdon W, et al. Phase I/pharmacodynamic study of N-acetylcysteine/oltipraz in smokers: early termination due to excessive toxicity. Cancer Epidemiology Biomarkers and Prevention. 2001;10(3):269–272. [PubMed] [Google Scholar]
- 40.Cantelli-Forti G, Hrelia P, Paolini M. The pitfall of detoxifying enzymes. Mutation Research. 1998;402(1-2):179–183. doi: 10.1016/s0027-5107(97)00296-0. [DOI] [PubMed] [Google Scholar]
- 41.Guengerich FP, Liebler DC. Enzymatic activation of chemicals to toxic metabolites. Critical Reviews in Toxicology. 1985;14(3):259–307. doi: 10.3109/10408448509037460. [DOI] [PubMed] [Google Scholar]
- 42.Hu Y, Kabler SL, Tennant AH, Townsend AJ, Kligerman AD. Induction of DNA-protein crosslinks by dichloromethane in a V79 cell line transfected with the murine glutathione-S-transferase theta 1 gene. Mutation Research. 2006;607(2):231–239. doi: 10.1016/j.mrgentox.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 43.Sherratt PJ, Williams S, Foster J, Kernohan N, Green T, Hayes JD. Direct comparison of the nature of mouse and human GST T1-1 and the implications on dichloromethane carcinogenicity. Toxicology and Applied Pharmacology. 2002;179(2):89–97. doi: 10.1006/taap.2002.9348. [DOI] [PubMed] [Google Scholar]
- 44.Sherratt PJ, Pulford DJ, Harrison DJ, Green T, Hayes JD. Evidence that human class Theta glutathione S-transferase T1-1 can catalyse the activation of dichloromethane, a liver and lung carcinogen in the mouse: comparison of the tissue distribution of GST T1-1 with that of classes Alpha, Mu and Pi GST in human. Biochemical Journal. 1997;326(3):837–846. doi: 10.1042/bj3260837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sherratt PJ, Manson MM, Thomson AM, et al. Increased bioactivation of dihaloalkanes in rat liver due to induction of class Theta glutathione S-transferase T1-1. Biochemical Journal. 1998;335(3):619–630. doi: 10.1042/bj3350619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hallier E, Schroder KR, Asmuth K, Dommermuth A, Aust B, Goergens HW. Metabolism of dichloromethane (methylene chloride) to formaldehyde in human erythrocytes: influence of polymorphism of glutathione transferase Theta (GST T1-1) Archives of Toxicology. 1994;68(7):423–427. doi: 10.1007/s002040050092. [DOI] [PubMed] [Google Scholar]
- 47.Wheeler JB, Stourman NV, Thier R, et al. Conjugation of haloalkanes by bacterial and mammalian glutathione transferases: mono- and vicinal dihaloethanes. Chemical Research in Toxicology. 2001;14(8):1107–1117. doi: 10.1021/tx0100183. [DOI] [PubMed] [Google Scholar]
- 48.Cho SH, Guengerich FP. Conjugation of butadiene diepoxide with glutathione yields DNA adducts in vitro and in vivo. Chemical Research in Toxicology. 2012;25(3):706–712. doi: 10.1021/tx200471x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Marsch GA, Botta S, Martin MV, McCormick WA, Guengerich FP. Formation and mass spectrometric analysis of DNA and nucleoside adducts by S-(1-acetoxymethyl)glutathione and by glutathione S-transferase-mediated activation of dihalomethanes. Chemical Research in Toxicology. 2004;17(1):45–54. doi: 10.1021/tx034156z. [DOI] [PubMed] [Google Scholar]
- 50.Hesse S, Jernstrom B, Martinez M. Inhibition of binding of benzo(a)pyrene metabolites to nuclear DNA by glutathione and glutathione S-transferase B. Biochemical and Biophysical Research Communications. 1980;94(2):612–617. doi: 10.1016/0006-291x(80)91276-0. [DOI] [PubMed] [Google Scholar]
- 51.Kayser MF, Vuilleumier S. Dehalogenation of dichloromethane by dichloromethane dehalogenase/glutathione S-transferase leads to formation of DNA adducts. Journal of Bacteriology. 2001;183(17):5209–5212. doi: 10.1128/JB.183.17.5209-5212.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim DH, Humphreys WG, Guengerich FP. Characterization of S-[2-(N1-adenyl)ethyl]glutathione as an adduct formed in RNA and DNA from 1,2-dibromoethane. Chemical Research in Toxicology. 1990;3(6):587–594. doi: 10.1021/tx00018a015. [DOI] [PubMed] [Google Scholar]
- 53.Thier R, Taylor JB, Pemble SE, et al. Expression of mammalian glutathione S-transferase 5-5 in Salmonella typhimurium TA1535 leads to base-pair mutations upon exposure to dihalomethanes. Proceedings of the National Academy of Sciences of the United States of America. 1993;90(18):8576–8580. doi: 10.1073/pnas.90.18.8576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pegram RA, Andersen ME, Warren SH, Ross TM, Claxton LD. Glutathione S-transferase-mediated mutagenicity of trihalomethanes in Salmonella typhimurium: contrasting results with bromodichloromethane and chloroform. Toxicology and Applied Pharmacology. 1997;144(1):183–188. doi: 10.1006/taap.1997.8123. [DOI] [PubMed] [Google Scholar]
- 55.Ozawa N, Guengerich FP. Evidence for formation of an S-[2-(N7-guanyl)ethyl]glutathione adduct in glutathione-mediated binding of the carcinogen 1,2-dibromoethane to DNA. Proceedings of the National Academy of Sciences of the United States of America. 1983;80(17 I):5266–5270. doi: 10.1073/pnas.80.17.5266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Marsch GA, Mundkowski RG, Morris BJ, Manier ML, Hartman MK, Guengerich FP. Characterization of nucleoside and DNA adducts formed by S-(1-Acetoxymethyl)glutathione and implications for dihalomethane - Glutathione conjugates. Chemical Research in Toxicology. 2001;14(5):600–608. doi: 10.1021/tx010006h. [DOI] [PubMed] [Google Scholar]
- 57.DeMarini DM, Shelton ML, Warren SH, et al. Glutathione S-transferase-mediated induction of GC → AT transitions by halomethanes in Salmonella. Environmental and Molecular Mutagenesis. 1997;30(4):440–447. [PubMed] [Google Scholar]
- 58.Cho SH, Loecken EM, Guengerich FP. Mutagenicity of a glutathione conjugate of butadiene diepoxide. Chemical Research in Toxicology. 2010;23(10):1544–1546. doi: 10.1021/tx100304f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Boogaard PJ, Sumner SCJ, Bond JA. Glutathione conjugation of 1,2:3,4-Diepoxybutane in human liver and rat and mouse liver and lung in vitro. Toxicology and Applied Pharmacology. 1996;136(2):307–316. doi: 10.1006/taap.1996.0037. [DOI] [PubMed] [Google Scholar]
- 60.Nieusma JL, Claffey DJ, Ruth JA, Ross D. Stereochemical aspects of the conjugation of epoxide metabolites of butadiene with glutathione in rat liver cytosol and freshly isolated rat hepatocytes. Toxicological Sciences. 1998;43(2):102–109. doi: 10.1006/toxs.1998.2461. [DOI] [PubMed] [Google Scholar]
- 61.Thier R, Pemble SE, Kramer H, Taylor JB, Guengerich FP, Ketterer B. Human glutathione S-transferase T1-1 enhances mutagenicity of 1,2-dibromoethane, dibromomethane and 1,2,3,4-diepoxybutane in Salmonella typhimurium. Carcinogenesis. 1996;17(1):163–166. doi: 10.1093/carcin/17.1.163. [DOI] [PubMed] [Google Scholar]
- 62.Humphreys WG, Kim DH, Cmarik JL, Shimada T, Guengerich FP. Comparison of the DNA-alkylating properties and mutagenic responses of a series of S-(2-Haloethyl)-substituted cysteine and glutathione derivatives. Biochemistry®. 1990;29(45):10342–10350. doi: 10.1021/bi00497a008. [DOI] [PubMed] [Google Scholar]
- 63.Monien BH, Herrmann K, Florian S. Metabolic activation of furfuryl alcohol: formation of 2-methylfuranyl DNA adducts in Salmonella typhimurium strains expressing human sulfotransferase 1A1 and in FVB/N mice. Carcinogenesis. 2011;32(10):1533–1539. doi: 10.1093/carcin/bgr126. [DOI] [PubMed] [Google Scholar]
- 64.Glatt H, Boeing H, Engelke CEH, et al. Human cytosolic sulphotransferases: genetics, characteristics, toxicological aspects. Mutation Research. 2001;482(1-2):27–40. doi: 10.1016/s0027-5107(01)00207-x. [DOI] [PubMed] [Google Scholar]
- 65.Hirose M, Yamaguchi T, Kimoto N, et al. Strong promoting activity of phenylethyl isothiocyanate and benzyl isothiocyanate on urinary bladder carcinogenesis in F344 male rats. International Journal of Cancer. 1998;77:773–777. doi: 10.1002/(sici)1097-0215(19980831)77:5<773::aid-ijc17>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 66.Kassie F, Pool-Zobel B, Parzefall W, Knasmüller S. Genotoxic effects of benzyl isothiocyanate, a natural chemopreventive agent. Mutagenesis. 1999;14(6):595–603. doi: 10.1093/mutage/14.6.595. [DOI] [PubMed] [Google Scholar]
- 67.Gamet-Payrastre L, Li P, Lumeau S, et al. Sulforaphane, a naturally occurring isothiocyanate, induces cell cycle arrest and apoptosis in HT29 human colon cancer cells. Cancer Research. 2000;60(5):1426–1433. [PubMed] [Google Scholar]
- 68.Thier R, Müller M, Taylor JB, Pemble SE, Ketterer B, Peter Guengerich F. Enhancement of bacterial mutagenicity of bifunctional alkylating agents by expression of mammalian glutathione S-transferase. Chemical Research in Toxicology. 1995;8(3):465–472. doi: 10.1021/tx00045a019. [DOI] [PubMed] [Google Scholar]
- 69.Oda Y, Yamazaki H, Thier R, Ketterer B, Guengerich FP, Shimada T. A new Salmonella typhimurium NM5004 strain expressing rat glutathione S-transferase 5-5: use in detection of genotoxicity of dihaloalkanes using an SOS/umu test system. Carcinogenesis. 1996;17(2):297–302. doi: 10.1093/carcin/17.2.297. [DOI] [PubMed] [Google Scholar]
- 70.Paolini M, Pozzetti L, Silingardi P, Della Croce C, Bronzetti G, Cantelli-Forti G. Isolation of a novel metabolizing system enriched in phase-II enzymes for short-term genotoxicity bioassays. Mutation Research. 1998;413(3):205–217. doi: 10.1016/s1383-5718(98)00005-9. [DOI] [PubMed] [Google Scholar]
- 71.Yang CS, Wang ZY. Tea and cancer. Journal of the National Cancer Institute. 1993;85(13):1038–1049. doi: 10.1093/jnci/85.13.1038. [DOI] [PubMed] [Google Scholar]
- 72.Fiala ES, Bobotas G, Kulakis C. Effects of disulfiram and related compounds on the metabolism in vivo of the colon carcinogen, 1,2-dimethylhydrazine. Biochemical Pharmacology. 1977;26(19):1763–1768. doi: 10.1016/0006-2952(77)90343-4. [DOI] [PubMed] [Google Scholar]
- 73.Wargovich MJ. Diallyl sulfide, a flavor component of garlic (Allium sativum), inhibits dimethylhydrazine-induced colon cancer. Carcinogenesis. 1987;8(3):487–489. doi: 10.1093/carcin/8.3.487. [DOI] [PubMed] [Google Scholar]
- 74.Guengerich FP, Kim DH. In vitro inhibition of dihydropyridine oxidation and aflatoxin B1 activation in human liver microsomes by naringenin and other flavonoids. Carcinogenesis. 1990;11(12):2275–2279. doi: 10.1093/carcin/11.12.2275. [DOI] [PubMed] [Google Scholar]
- 75.Langouët S, Welti DH, Kerriguy N, et al. Metabolism of 2-amino-3,8-dimethylimidazo[4,5-f]-quinoxaline in human hepatocytes: 2-amino-3-methylimidazo[4,5-f]quinoxaline-8-carboxylic acid is a major detoxication pathway catalyzed by cytochrome P450 1A2. Chemical Research in Toxicology. 2001;14(2):211–221. doi: 10.1021/tx000176e. [DOI] [PubMed] [Google Scholar]
- 76.Yang CS, Smith TJ, Hong JY, et al. Cancer prevention through modulation of xenobiotic metabolising enzymes: opportunities and limitations. The American Association for Cancer Research. 1996;37:665–666. [Google Scholar]
- 77.Nebert DW. Drug-metabolizing enzymes in ligand-modulated transcription. Biochemical Pharmacology. 1994;47(1):25–37. doi: 10.1016/0006-2952(94)90434-0. [DOI] [PubMed] [Google Scholar]
- 78.Nebert DW. Role of genetics and drug metabolism in human cancer risk. Mutation Research. 1991;247(2):267–281. doi: 10.1016/0027-5107(91)90022-g. [DOI] [PubMed] [Google Scholar]
- 79.Reszka E, Wasowicz W, Gromadzinska J. Genetic polymorphism of xenobiotic metabolising enzymes, diet and cancer susceptibility. British Journal of Nutrition. 2006;96(4):609–619. [PubMed] [Google Scholar]
- 80.Paolini M, Sapone A, Gonzalez FJ. Parkinson’s disease, pesticides and individual vulnerability. Trends in Pharmacological Sciences. 2004;25(3):124–129. doi: 10.1016/j.tips.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 81.Paolini M, Nicholl DJ, Bennett P, Bandmann O, Wood NW. Acetylator genotype and Parkinson’s disease. Lancet. 1998;351(9096):141–142. doi: 10.1016/s0140-6736(05)78116-2. [DOI] [PubMed] [Google Scholar]
- 82.Paolini M, Biagi GL, Cantelli-Forti G, et al. Glutathione transferase polymorphism and Parkinson’s disease. Lancet. 1999;353(9146):71–72. doi: 10.1016/S0140-6736(05)74835-2. [DOI] [PubMed] [Google Scholar]
- 83.Paolini M, Nestle M. Pitfalls of enzyme-based molecular anticancer dietary manipulations: food for thought. Mutation Research. 2003;543(3):181–189. doi: 10.1016/s1383-5742(02)00092-3. [DOI] [PubMed] [Google Scholar]
- 84.Gerrior SA, Zizza C. Nutrient Content of the US Food Supply 1909–1990. Washington, DC, USA: US Department of Agriculture; 1994. [Google Scholar]
- 85.Collins AR, Olmedilla B, Southon S, Granado F, Duthie SJ. Serum carotenoids and oxidative DNA damage in human lymphocytes. Carcinogenesis. 1998;19(12):2159–2162. doi: 10.1093/carcin/19.12.2159. [DOI] [PubMed] [Google Scholar]
- 86.Paolini M. Pharmaceuticals: reduce drug waste in the environment. Nature. 2011;478:36–37. doi: 10.1038/478036a. [DOI] [PubMed] [Google Scholar]
- 87.Hennekens CH, Buring JE, Manson JE, et al. Lack of effect of long-term supplementation with beta carotene on the incidence of malignant neoplasms and cardiovascular disease. New England Journal of Medicine. 1996;334(18):1145–1149. doi: 10.1056/NEJM199605023341801. [DOI] [PubMed] [Google Scholar]
- 88.Omenn GS, Goodman GE, Thornquist MD, et al. Risk factors for lung cancer and for intervention effects in CARET, the beta-carotene and retinol efficacy trial. Journal of the National Cancer Institute. 1996;88(21):1550–1559. doi: 10.1093/jnci/88.21.1550. [DOI] [PubMed] [Google Scholar]
- 89.Hinds TS, West WL, Knight EM. Carotenoids and retinoids: a review of research, clinical, and public health applications. Journal of Clinical Pharmacology. 1997;37(7):551–558. doi: 10.1002/j.1552-4604.1997.tb04336.x. [DOI] [PubMed] [Google Scholar]
- 90.Paolini M, Abdel-Rahman SZ, Cantelli-Forti G, Legator MS. Chemoprevention or antichemoprevention? A salutary warning from the β-Carotene experience. Journal of the National Cancer Institute. 2001;93(14):1110–1111. doi: 10.1093/jnci/93.14.1110. [DOI] [PubMed] [Google Scholar]
- 91.Lee IM, Cook NR, Manson JE, Buring JE, Hennekens CH. β-carotene supplementation and incidence of cancer and cardiovascular disease: the women’s health study. Journal of the National Cancer Institute. 1999;91(24):2102–2106. doi: 10.1093/jnci/91.24.2102. [DOI] [PubMed] [Google Scholar]
- 92.Marshall JR. β-carotene: a miss for epidemiology. Journal of the National Cancer Institute. 1999;91(24):2068–2069. doi: 10.1093/jnci/91.24.2068. [DOI] [PubMed] [Google Scholar]
- 93.Vainio H. Chemoprevention of cancer: lessons to be learned from beta-carotene trials. Toxicology Letters. 2000;112-113:513–517. doi: 10.1016/s0378-4274(99)00208-8. [DOI] [PubMed] [Google Scholar]
- 94.Paolini M, Cantelli-Forti G, Perocco P, Pedulli GF, Abdel-Rahman SZ, Legator MS. Co-carcinogenic effect of β-carotene. Nature. 1999;398(6730):760–761. doi: 10.1038/19655. [DOI] [PubMed] [Google Scholar]
- 95.Podmore ID, Griffiths HR, Herbert KE, Mistry N, Mistry P, Lunec J. Vitamin C exhibits pro-oxidant properties. Nature. 1998;392(6676):p. 559. doi: 10.1038/33308. [DOI] [PubMed] [Google Scholar]
- 96.Paolini M, Pozzetti L, Pedulli GF, Marchesi E, Cantelli-Forti G. The nature of prooxidant activity of vitamin C. Life Sciences. 1999;64(23):PL273–PL278. doi: 10.1016/s0024-3205(99)00167-8. [DOI] [PubMed] [Google Scholar]
- 97.Lee SH, Oe T, Blair IA. Vitamin C-induced decomposition of lipid hydroperoxides to endogenous genotoxins. Science. 2001;292(5524):2083–2086. doi: 10.1126/science.1059501. [DOI] [PubMed] [Google Scholar]


