Abstract
A 31-year-old man presented with a large cardiac mass that originated from the basal posterior left atrial wall and occupied most of the dilated atrium. Minimally invasive studies yielded inconclusive results, but the patient was considered at high risk for an open cardiac biopsy due to the size of the mass. To establish a tissue diagnosis for definitive treatment, we performed a transseptal cardiac biopsy guided by 3-dimensional transesophageal echocardiography. We thereby determined that the mass was a primary left atrial sarcoma. To the best of our knowledge, this is the first report concerning the use of 3-dimensional transesophageal echocardiography for biopsy of a left atrial mass.
Key words: Biopsy/methods; echocardiography, 3-dimensional; echocardiography, transesophageal; heart atria/ultrasonography; heart neoplasms/diagnosis; sarcoma/diagnosis; tumors, cardiac
Cardiac tumors are infrequently encountered in clinical practice. Treatment options are guided by location, stage, and tissue diagnosis. If imaging does not provide a conclusive diagnosis, a biopsy is performed. In obtaining specimens for biopsy, the operator encounters more difficulty with left-sided than with right-sided masses. We describe a left atrial tumor in which the biopsy specimen was obtained by means of a transseptal puncture with 3-dimensional (3D) transesophageal echocardiographic (TEE) guidance.
Case Report
A 31-year-old man with a 6-month history of progressive shortness of breath, weight loss, and fatigue was admitted to the hospital. Echocardiography and computed tomography led to the discovery of a left atrial mass, prompting referral to our center for further management.
The patient's personal and family medical histories were unremarkable. On admission to our hospital, he had tachycardia at rest, with a regular rhythm; his vital signs were otherwise unexceptional. All digits showed prominent clubbing. Cardiac auscultation revealed an early diastolic sound initiating a mid-diastolic apical murmur, without signs of heart failure or embolic phenomena. Electrocardiography showed sinus tachycardia and anterior T-wave inversion. Laboratory testing disclosed microcytic anemia and elevated inflammatory marker levels.
Transesophageal echocardiography (TEE) was performed to better delineate the left atrial mass (Fig. 1), which originated from the basal posterior left atrial wall and occupied most of the dilated atrium. A mobile portion of the mass prolapsed into the left ventricle, causing functional mitral stenosis with a gradient of 8 mmHg and moderate mitral regurgitation. The left superior pulmonary vein was compressed externally and had high-velocity flow on Doppler interrogation. The left ventricle appeared normal in size and function, but the right ventricle was mildly dilated and hypokinetic, with an estimated pulmonary artery systolic pressure of 55 to 60 mmHg.

Fig. 1 Transesophageal echocardiogram shows the left atrial mass, which originated from the basal posterior left atrial wall and occupied most of the dilated atrium.
A computed tomographic scan with intravenous contrast material, followed by cardiac magnetic resonance imaging with gadolinium, revealed a highly vascular left atrial mass of about 4.6 cm in diameter, which emerged from and invaded the posterior left atrial wall and possibly extended beyond the atrium (Fig. 2). The mass caused narrowing of the left upper pulmonary vein and extended to the right pulmonary vein without resulting in narrowing of that vessel. Invasion of the left main stem bronchus was suspected, and lymphadenopathy was evident.

Fig. 2 Magnetic resonance image shows the left atrial mass, which emerged from and invaded the posterior left atrial wall and possibly extended beyond the atrium.
The patient was considered at high risk for an open cardiac biopsy, so we attempted a video-assisted cervical and mediastinal biopsy, targeting lymph nodes seen on the radiologic studies. On histologic examination, only reactive tissue was identified. A subsequent bronchoscopic biopsy did not identify any malignant tissue. To establish a tissue diagnosis for definitive treatment, we performed a transseptal cardiac biopsy with the patient under general anesthesia in the cardiac catheterization laboratory.
Using a long electrophysiology sheath for support, we performed a transseptal puncture. We then used a Ceres bioptome (Ceres Medical Systems, LLC; Sugar Land, Texas) to perform multiple biopsies of the complex left atrial mass with 2-dimensional (2D) and 3D TEE guidance (Fig. 3). A concurrent selective coronary angiogram confirmed the vascular nature of the mass but was otherwise unremarkable (Fig. 4). A hemodynamic study showed moderate mitral stenosis with a gradient of 9 mmHg and a pressure half-time of 284 ms (Fig. 5). The patient had a cardiac index (Fick) of 2.58 L/min. Table I presents other hemodynamic values.

Fig. 3 Two orthogonal echocardiographic views show the complexity of the left atrial mass.

Fig. 4 Selective coronary angiogram, obtained during transseptal biopsy, shows the blood supply of the left atrial mass.
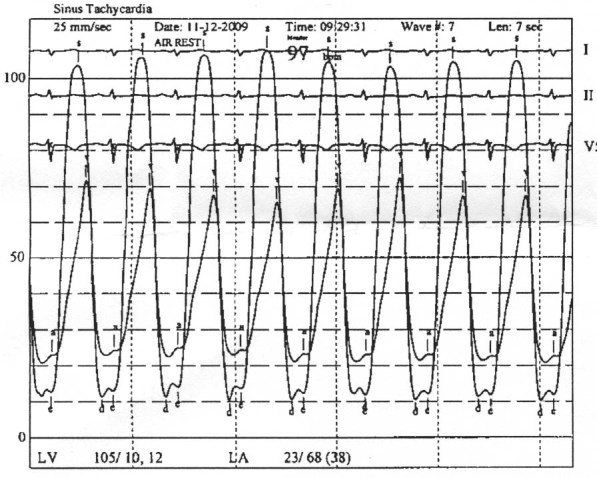
Fig. 5 Left ventricular-to-left atrial pressure gradient indicates moderate mitral stenosis, as measured during cardiac catheterization and biopsy.
TABLE I. Hemodynamic Values Measured during Transseptal Biopsy

Histologic examination of the biopsy specimens revealed a poorly differentiated sarcoma, for which ifosfamide, doxorubicin, and mesna were administered. The patient tolerated the initial cycles of chemotherapy satisfactorily and was discharged from the hospital. Within a few days, he was readmitted with fever and leukocytosis, which were determined to be related to tumor fever. Among other investigations, cardiac magnetic resonance imaging was performed and showed no change in the size of the mass, but new regional left ventricular dysfunction was observed in the infero-apical segment, presumably due to embolic infarction from the mass to the left coronary artery territory. While still hospitalized, the patient sustained a fatal cardiac arrest. The cause of the arrest was unknown, but embolization of the mass was presumed. In accordance with the family's wishes, an autopsy was not performed.
Discussion
In the past, transseptal puncture was commonly performed for hemodynamic evaluation of left-sided cardiac lesions. With the advent of high-quality echocardiography and Doppler imaging, however, transseptal puncture became used only in pediatric populations. Recently, its use has increased among electrophysiologists and interventional cardiologists for ablation procedures performed to treat atrial fibrillation, patent foramen ovale, atrial and ventricular septal defects, left atrial appendage closure, and mitral valve disease in adults. Potential complications (prevalence, <1%) include left atrial perforation, cardiac tamponade, aortic perforation, clot formation, and embolization.1 Biopsy of left atrial or left ventricular masses entails the additional risk of tumor embolization, which can lead to stroke, tumor metastasis, or both.2
The literature includes a few reports of transseptal biopsies, including biopsy of a phyllodes tumor with the aid of TEE,3 fine-needle aspiration of a spindle-cell neoplasm,4 biopsy of a right atrial angiosarcoma,5 and computed-tomography–guided biopsy of a left atrial sarcoma.6 To the best of our knowledge, this is the first report concerning the use of 3-dimensional transesophageal echocardiography for biopsy of a left atrial mass.
Two-dimensional and 3D TEE, in conjunction with transseptal puncture, is increasingly being used in the electrophysiology laboratory. The additional dimension provided by 3D TEE enables better localization of the interatrial septum (in more than 1 plane), especially in cases of unusual septal anatomy.7
Chan and colleagues8 compared real-time surface 3D echocardiography with conventional 2D surface echocardiography in 106 patients who had a wide spectrum of cardiac conditions and who were referred for evaluation at a tertiary care center. The investigators reported that the 3D study provided a useful and unique anatomic perspective, without new findings in many cases; the 2 types of echocardiographic studies provided equivalent information in most instances.8
In our patient, 3D TEE was used to provide a unique anatomic perspective during transseptal catheterization and to safely guide the bioptome to obtain a biopsy specimen of a left atrial tumor. Our experience suggests that 3D TEE added incremental value over 2D imaging in the spatial localization of the intracardiac mass and bioptome and facilitated the biopsy procedure.
We conclude that at centers with experienced operators, transseptal biopsy of a left atrial mass with 3D TEE guidance—in addition to conventional 2D imaging in high-risk surgical patients—is a reasonable option when the results of other minimally invasive studies are inconclusive.
Footnotes
Address for reprints: James M. Wilson, MD, 6624 Fannin St., Suite 2480, Houston, TX 77030
E-mail: jmwil@sbcglobal.net
References
- 1.Babaliaros VC, Green JT, Lerakis S, Lloyd M, Block PC. Emerging applications for transseptal left heart catheterization old techniques for new procedures. J Am Coll Cardiol 2008; 51(22):2116–22. [DOI] [PubMed]
- 2.Pindyck F, Peirce EC 2nd, Baron MG, Lukban SB. Embolization of left atrial myxoma after transseptal cardiac catheterization. Am J Cardiol 1972;30(5):569–71. [DOI] [PubMed]
- 3.Jackson CE, Gardner RS, Connelly DT. A novel approach for a novel combination: a trans-septal biopsy of left atrial mass in recurrent phyllodes tumour. Eur J Echocardiogr 2009;10(1):171–2. [DOI] [PubMed]
- 4.Wong CW, Ruygrok P, Sutton T, Ding P, van Vliet C, Occleshaw C, Smith W. Transseptal fine needle aspiration of a large left atrial tumour. Heart Lung Circ 2010;19(7):438–9. [DOI] [PubMed]
- 5.Bhalla R, Nassar A. Cardiac angiosarcoma: report of a case diagnosed by echocardiographic-guided fine-needle aspiration. Diagn Cytopathol 2007;35(3):164–6. [DOI] [PubMed]
- 6.Daliri A, Oehring K, Moosdorf RG, Franke FE, Kalinowski M, Zahedi F, Froelich JJ. Percutaneous left atrial cardiac biopsy with CT fluoroscopy guidance. J Vasc Interv Radiol 2007; 18(7):909–13. [DOI] [PubMed]
- 7.Chierchia GB, Capulzini L, de Asmundis C, Sarkozy A, Roos M, Paparella G, et al. First experience with real-time three-dimensional transesophageal echocardiography-guided transseptal puncture in patients undergoing atrial fibrillation ablation. Europace 2008;10(11):1325–8. [DOI] [PubMed]
- 8.Chan KL, Liu X, Ascah KJ, Beauchesne LM, Burwash IG. Comparison of real-time 3-dimensional echocardiography with conventional 2-dimensional echocardiography in the assessment of structural heart disease. J Am Soc Echocardiogr 2004;17(9):976–80. [DOI] [PubMed]


