Abstract
Spontaneous coronary artery dissection and vertebral artery dissection are rare, life-threatening conditions. The pathophysiology of spontaneous coronary artery dissection during the peripartum period is poorly understood. We present a case of spontaneous multivessel dissection in a 32-year-old postpartum woman who presented with neck and chest pain. The patient's coronary and vertebral artery dissections were diagnosed with use of multiple imaging methods, and dissection of the internal mammary artery was discovered during surgery. The patient underwent successful coronary artery bypass grafting and remained asymptomatic 2 years later. To our knowledge, this is the first report of simultaneous coronary, vertebral, and internal mammary artery dissection in a postpartum woman. Early recognition and treatment is crucial, given the high mortality rate associated with spontaneous dissection.
Key words: Acute coronary syndrome/etiology; coronary artery bypass; postpartum period; pregnancy complications, cardiovascular/diagnosis; rupture, spontaneous/diagnosis/etiology/surgery; treatment outcome; vertebral artery dissection/epidemiology/surgery/ultrasonography
Spontaneous coronary artery dissection, which has been well described in the medical literature, is a highly unusual cause of acute coronary syndrome. It is most often associated with acute myocardial infarction in women during their 3rd trimester of pregnancy or the early postpartum period. The exact cause remains unknown, and there are no guidelines in regard to optimal treatment. Dissection of multiple arteries in the postpartum period is even less common: to our knowledge, only 2 cases of simultaneous spontaneous vertebral and coronary artery dissection have been reported. We present what we believe is the first report of a postpartum woman with spontaneous dissection involving the coronary, vertebral, and internal mammary arteries.
Case Report
In March 2010, a 32-year-old woman emergently presented one week postpartum with intermittent neck and chest pain. She reported that the pain had started as left-sided neck tenderness immediately after she had given birth. The pain was worse upon palpation, movement, deep inspiration, or coughing. She reported no other symptoms.
The patient's medical history was notable only for papillary thyroid cancer during the pregnancy and thyroidectomy 6 months before delivery. She reported no problems during her previous 2 pregnancies. She was taking no medications except for levothyroxine, and she had no drug allergies. She was a lifetime nonsmoker and said that she had never used illicit drugs. She reported nothing relevant in her family medical history.
On examination, her blood pressure and heart rate were normal and stable; on palpation, she had reproducible tenderness of the left side of the neck. No other results of physical examination were unusual. An electrocardiogram revealed sinus rhythm with no significant abnormalities. Results of initial laboratory evaluation, including a metabolic profile, a complete blood count, and 2 sets of cardiac markers, were within normal limits. A computed tomographic angiogram (CTA) of the chest and neck did not reveal any acute findings. Her pain subsided during her visit, and she asked to be discharged from emergency care. She was advised to maintain close follow-up with her primary care physician.
Six days later, the patient returned emergently with persistent neck pain that radiated to the chest. Her blood pressure was markedly elevated (180/102 mmHg). Results of physical examination were not unusual except for neck and chest-wall tenderness on palpation. An electrocardiogram showed sinus rhythm with slow R-wave progression in leads V1 through V3 (Fig. 1). Cardiac biomarkers included a creatine kinase level of 89 U/L (normal range, 33–211 U/L), a creatine kinase–MB fraction of 16 U/L (normal, <10 U/L), and a troponin I level of 4.34 ng/mL (normal, <0.01 ng/mL). A CTA of the chest and neck revealed a small flap within the mid-left vertebral artery at the level of C6–C7, consistent with vertebral artery dissection (Fig. 2). A transthoracic echocardiogram revealed normal left ventricular systolic function with no wall-motion or valvular abnormalities. The patient was admitted to the hospital. Her blood pressure was controlled with metoprolol, and therapy with aspirin, clopidogrel, and systemic heparin was initiated.
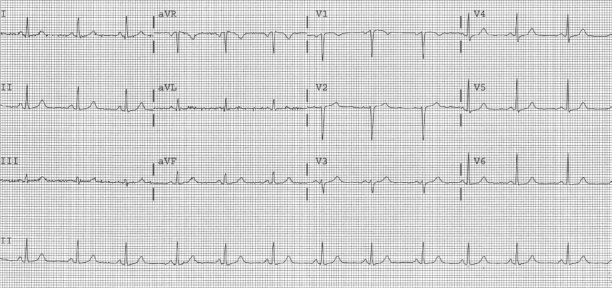
Fig. 1 Admission electrocardiogram shows sinus rhythm with slow R-wave progression in leads V1 through V3.
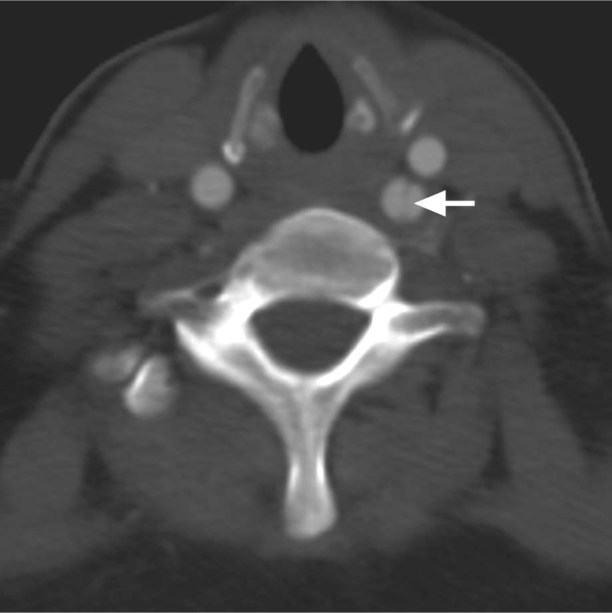
Fig. 2 Computed tomographic angiogram shows left vertebral artery dissection at the C6–C7 level. The arrow points to the dissection flap.
During day 2 of hospitalization, the patient developed acute chest pain associated with profuse diaphoresis. Electrocardiography revealed ST elevation of 1.5 to 2 mm in leads I, aVL, and V2, and 2-mm downsloping ST depression in leads III and aVF (Fig. 3). Coronary angiography showed a long arterial dissection in the proximal portion of the left anterior descending coronary artery (LAD) (Figs. 4 and 5). The dissection did not involve the left main coronary artery (LMCA). To rule out coronary spasm, 500 μg of intracoronary nitroglycerin was administered; however, the appearance of the arteries did not change.
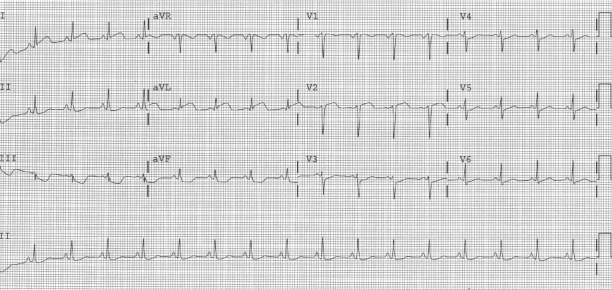
Fig. 3 Electrocardiogram performed during the patient's episode of acute chest pain shows ST elevation in leads I, aVL, and V2. Downsloping ST depression is seen in leads III and aVF.
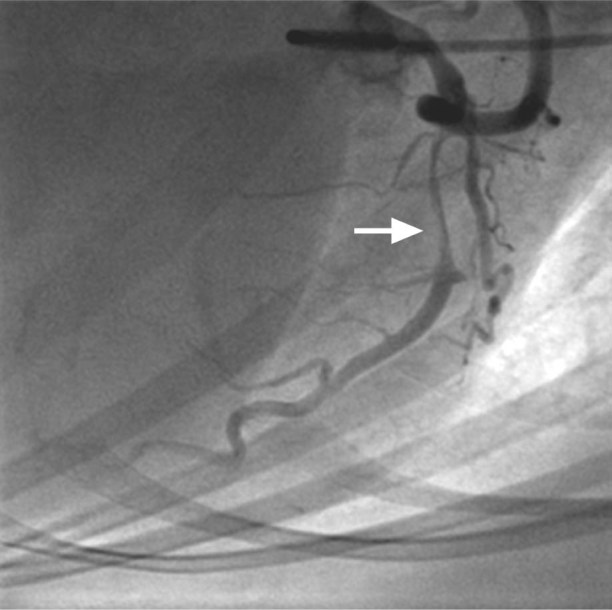
Fig. 4 Coronary angiogram (right anterior oblique cranial view) shows dissection of the proximal left anterior descending coronary artery (arrow).
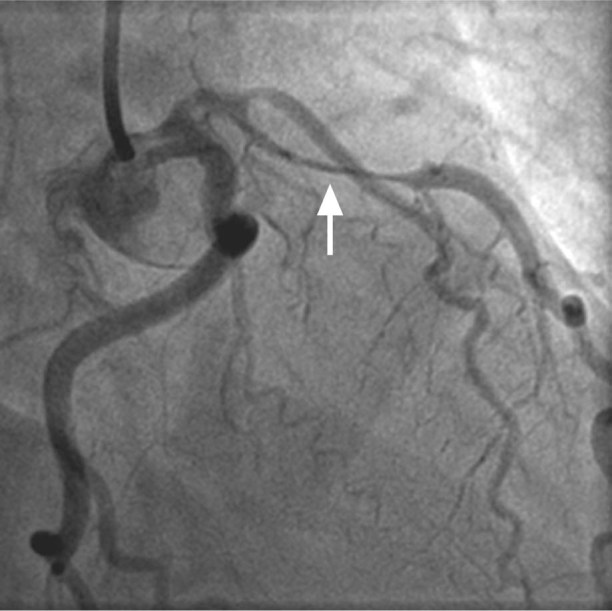
Fig. 5 Coronary angiogram (right anterior oblique caudal view) shows dissection of the proximal left anterior descending coronary artery (arrow).
At operation, a dissection of the left internal mammary artery was found. The patient underwent successful coronary artery bypass grafting (CABG) with a reverse saphenous vein graft to the LAD. Her postoperative hospital course was uneventful, and she remained asymptomatic 2 years later.
Discussion
Spontaneous coronary artery dissection is an unusual cause of acute myocardial infarction; fewer than 400 cases have been reported.1 The condition was first described in a 42-year-old woman by Pretty in 1931.2 The reported prevalence is 0.2% to 0.3% as a cause of acute coronary syndrome in the general population.3 The condition occurs most often in young to middle-aged women during the peripartum period, in approximately 1 in 20,000 to 30,000 deliveries.4 Approximately 80% of pregnancy-related spontaneous coronary artery dissection occurs in the 3 months after delivery, at a median time of 13 days postpartum,5,6 and involves the LAD or LMCA in about 80% of cases.7 Most diagnoses of pregnancy-related dissection are made at autopsy, because the mortality rate for the condition is 50% to 70%.4 However, the survival rate improves to 85% in patients who receive appropriate treatment and survive the acute phase.8
Pregnancy-related spontaneous coronary artery dissection is not typically associated with classic coronary disease risk factors. The exact cause and pathogenesis is unclear, but it has been suggested that hormonal and hemodynamic changes during the peripartum period weaken the coronary artery walls and predispose them to dissection.8
If the patient survives the acute phase of spontaneous dissection, the diagnosis is typically confirmed with use of conventional coronary angiography. Coronary CTA has detected spontaneous coronary artery dissection; however, the sensitivity of detection is unknown, and diagnosis should be confirmed with use of conventional coronary angiography.9 Coronary dissections can also be missed on routine coronary angiography, so strong suspicion warrants the use of intravascular ultrasonography. We did not use that method of imaging in this patient, because of the definitive findings on coronary angiography.
No guidelines exist for the management of spontaneous coronary artery dissection. The spectrum of treatment includes medical therapy, percutaneous coronary intervention (PCI), and CABG. These approaches have not been universally successful. The lack of randomized trials comparing these strategies is not surprising, because spontaneous coronary artery dissection cases are rare and most are diagnosed at autopsy. Most evidence has been obtained from case reports or small case series. Therapy is challenging, and its primary use depends on the persistence of myocardial ischemia, the region at risk, and the number of vessels involved. Routine medical therapy for acute coronary syndrome has reportedly yielded good results in some spontaneous coronary artery dissection patients.10 Fibrinolytic agents have been used to lyse a compressive clot; however, they may worsen the dissection and lead to further compression of the true lumen.11 Fibrinolytic agents are not routinely recommended, especially in pregnant patients.
Given that medical therapy may not be the optimal treatment, PCI with stent placement can be considered to treat focal dissections that do not involve the LMCA.12 If a dissection is complicated by involved thrombus and a nearly occluded lumen, direct stenting of the true lumen could be difficult, if not impossible. Because of the higher compliance of the relatively nonfibrotic, nonatherosclerotic vessel walls in patients with spontaneous coronary artery dissection, accidental wire passage into the false lumen may occur more often.13 In cases of multivessel or LMCA involvement, CABG is typically the treatment of choice. Stenting was an option in our patient; however, given the location (the proximal LAD) and the risk of dissection propagation into the LMCA, we chose to proceed with CABG.
Spontaneous dissection of the vertebral artery is an even rarer postpartum event: we found only 8 published cases.1,14–17 The pathophysiology is presumed to be similar to that in the coronary arteries, including intimal injury from straining during vaginal delivery.16 More than half of patients with vertebral artery dissections present with neck or head pain, and this will typically precede the onset of ischemic symptoms by hours to days.14 Either magnetic resonance imaging or CTA is a good noninvasive diagnostic test for vertebral artery dissection.14 In the absence of intracranial hemorrhage, anticoagulation is the mainstay of therapy, because symptoms and sequelae are related to thrombosis of the vertebral artery or embolization of clots to the intracranial circulation.14 If the diagnosis is made early, the prognosis for vertebral artery dissection is typically very favorable, and recurrent dissection is rare.17
Our patient's case appears to be the 3rd documented report of simultaneous spontaneous dissection of the coronary and vertebral arteries in the postpartum period.1,10 To our knowledge, this is the first documented case of simultaneous spontaneous dissection of the coronary, vertebral, and internal mammary arteries in a postpartum woman.
Footnotes
Address for reprints: Hutton P. Brantley, DO, Department of Cardiovascular Sciences, Brody School of Medicine at East Carolina University, 115 Heart Dr., Greenville, NC 27834
E-mail: brantleyh@ecu.edu
References
- 1.Sharma AM, Herrera B, Aronow HD. Simultaneous spontaneous coronary and vertebral artery dissection in a postpartum woman. J Invasive Cardiol 2010;22(12):E229–32. [PubMed]
- 2.Pretty HC. Dissecting aneurysm of coronary artery in a woman aged 42: rupture. Br Med J 1931;1(3667):667.
- 3.Mortensen KH, Thuesen L, Kristensen IB, Christiansen EH. Spontaneous coronary artery dissection: a Western Denmark Heart Registry study. Catheter Cardiovasc Interv 2009;74(5):710–7. [DOI] [PubMed]
- 4.Van den Branden BJ, Bruggeling WA, Corbeij HM, Dunselman PH. Spontaneous coronary artery dissection in the postpartum period. Neth Heart J 2008;16(12):412–4. [DOI] [PMC free article] [PubMed]
- 5.Hinojal YC, Di Stefano S, Florez S, Martinez G, de la Fuente L, Casquero E, Gualis J. Spontaneous coronary dissection during postpartum: etiology and controversies in management. Ital Heart J 2004;5(7):563–5. [PubMed]
- 6.Maeder M, Ammann P, Drack G, Rickli H. Pregnancy-associated spontaneous coronary artery dissection: impact of medical treatment. Case report and systematic review. Z Kardiol 2005;94(12):829–35. [DOI] [PubMed]
- 7.Koul AK, Hollander G, Moskovits N, Frankel R, Herrera L, Shani J. Coronary artery dissection during pregnancy and the postpartum period: two case reports and review of literature. Catheter Cardiovasc Interv 2001;52(1):88–94. [DOI] [PubMed]
- 8.Engelman DT, Thayer J, Derossi J, Scheinerman J, Brown L. Pregnancy related coronary artery dissection: a case report and collective review. Conn Med 1993;57(3):135–9. [PubMed]
- 9.Schroder C, Stoler RC, Branning GB, Choi JW. Postpartum multivessel spontaneous coronary artery dissection confirmed by coronary CT angiography. Proc (Bayl Univ Med Cent) 2006;19(4):338–41. [DOI] [PMC free article] [PubMed]
- 10.Motreff P, Souteyrand G, Dauphin C, Eschalier R, Cassagnes J, Lusson JR. Management of spontaneous coronary artery dissection: review of the literature and discussion based on a series of 12 young women with acute coronary syndrome. Cardiology 2010;115(1):10–8. [DOI] [PubMed]
- 11.McCann AB, Whitbourn RJ. Spontaneous coronary artery dissection: a review of the etiology and available treatment options. Heart Vessels 2009;24(6):463–5. [DOI] [PubMed]
- 12.Madu EC, Kosinski DJ, Wilson WR, Burket MW, Fraker TD Jr, Ansel GM. Two-vessel coronary artery dissection in the peripartum period. Case report and literature review. Angiology 1994;45(9):809–16. [DOI] [PubMed]
- 13.Velusamy M, Fisherkeller M, Keenan ME, Kiernan FJ, Fram DB. Spontaneous coronary artery dissection in a young woman precipitated by retching. J Invasive Cardiol 2002;14 (4):198–201. [PubMed]
- 14.Lam CS, Yee YK, Tsui YK, Szeto ML. Vertebral artery dissection: a treatable cause of ischaemic stroke. Hong Kong Med J 1999;5(4):398–401. [PubMed]
- 15.Sharshar T, Lamy C, Mas JL. Incidence and causes of strokes associated with pregnancy and puerperium. A study in public hospitals of Ile de France. Stroke in Pregnancy Study Group. Stroke 1995;26(6):930–6. [DOI] [PubMed]
- 16.Gasecki AP, Kwiecinski H, Lyrer PA, Lynch TG, Baxter T. Dissections after childbirth. J Neurol 1999;246(8):712–5. [DOI] [PubMed]
- 17.Arnold M, Bousser MG, Fahrni G, Fischer U, Georgiadis D, Gandjour J, et al. Vertebral artery dissection: presenting findings and predictors of outcome. Stroke 2006;37(10):2499–503. [DOI] [PubMed]


