Abstract
Symptomatic spontaneous celiac artery dissection is a rare condition that is being detected more often with the use of advanced imaging techniques. There is no consensus as to whether surgical or endovascular treatment is more appropriate.
We describe the case of a 41-year-old hypertensive woman who presented with the sudden onset of sharp, persistent, right-upper-quadrant abdominal and epigastric pain. Magnetic resonance angiography of the abdomen revealed celiac artery dissection, with a flap compressing the lumen approximately 17 mm from the artery's origin at the aorta. Because of the patient's persistent epigastric pain, endovascular celiac artery stent implantation was performed with the use of 2 overlapping balloon-expandable stents. Twelve months after the procedure, the patient remained asymptomatic, and the stents were patent. This case and others in the medical literature suggest that endovascular treatment can be feasible in symptomatic patients with isolated spontaneous celiac artery dissection.
Key words: Aneurysm, dissecting/diagnosis/radiography/therapy; angiography/methods; anticoagulants/therapeutic use; celiac artery/injuries/pathology/radiography; rupture, spontaneous/diagnosis/therapy; stents; vascular surgical procedures
Isolated spontaneous celiac artery dissection is rare. Most reported cases have occurred in men, and the cause and natural history of the condition are not well understood. In regard to symptomatic spontaneous dissection, it is debated whether surgical or endovascular treatment is more appropriate. We describe our endovascular treatment of spontaneous celiac artery dissection in a symptomatic female patient, and we discuss our findings in the context of previously reported cases.
Case Report
A 41-year-old woman presented with the sudden onset of sharp pain in the epigastrium and the right upper quadrant of the abdomen. The pain radiated to the left breast and the back. Her medical history included hypertension and a previous hysterectomy for uterine fibroids. Physical examination revealed mild epigastric tenderness. Results of laboratory tests, including a complete blood count and basic metabolic profile, were normal except for an increased lipase level of 359 U/L (normal range, 6–51 U/L). The patient was diagnosed with pancreatitis and was admitted for observation.
Abdominal radiographs and contrast-enhanced computed tomograms of the abdomen showed nothing unusual. Ultrasonography of the abdomen revealed gallbladder sludge. The patient's lipase level returned to normal in 4 days; however, nausea and severe epigastric pain persisted. Magnetic resonance angiography of the abdomen revealed celiac artery dissection with a flap that originated approximately 17 mm from the celiac artery ostium (Fig. 1). The caliber of the true lumen appeared to be compromised. The hepatic, splenic, and gastric arteries were clearly patent.

Fig. 1 Three-dimensional magnetic resonance angiogram shows celiac artery dissection (arrow).
Because of the symptoms secondary to the dissection, selective angiography of the abdominal aorta and celiac artery was performed (Fig. 2). The true lumen of the celiac artery was entered with a 0.014-in HI-TORQUE® WHISPER® hydrophilic guidewire (Abbott Vascular, part of Abbott Laboratories; Santa Clara, Calif) inside an 8F internal mammary artery guiding catheter after heparin was given as an anticoagulant. Intravascular ultrasonography with use of a 0.014-in Eagle Eye® system (Volcano Corporation; San Diego, Calif) showed a large false lumen and a dissection that extended from the proximal to the mid celiac artery. To prevent distal dissection and to better support the endovascular procedure, the Whisper wire was exchanged for a 0.014-in nonhydrophilic HI-TORQUE® Spartacore® peripheral guidewire (Abbott Vascular) (Fig. 3). Two overlapping 6 × 18-mm Palmaz® Blue™ stents (Cordis Corporation, a Johnson & Johnson company; Bridgewater, NJ) were then placed in the celiac artery, slightly distal to that artery's origin, in order to maintain the patency of the gastric artery, which also arises from the proximal celiac artery. Angiography revealed satisfactory widening of the true lumen and minimal contrast medium in the false lumen (Fig. 4). The patient's abdominal pain disappeared immediately after the intervention. She was prescribed aspirin and clopidogrel, and a β-blocker for hypertension.
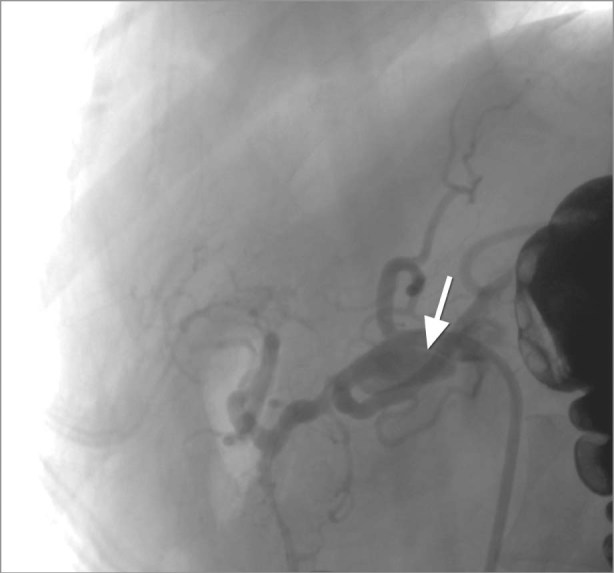
Fig. 2 Selective angiogram shows the celiac artery dissection and the proximal false lumen (arrow).
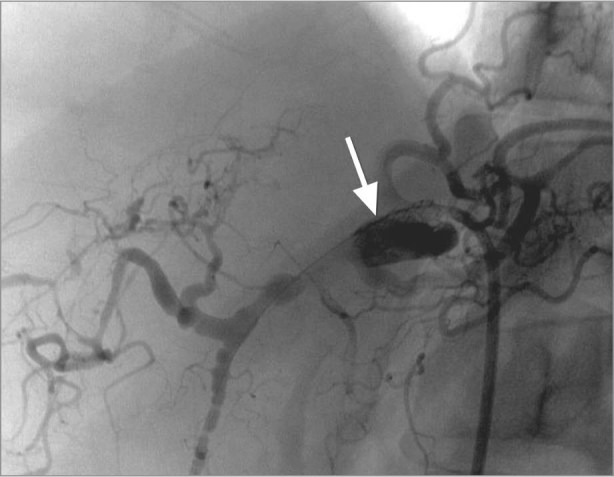
Fig. 3 Angiogram shows the celiac artery after wire insertion and before placement of the first stent (arrow).

Fig. 4 Angiogram after stent placement (arrows) shows widening of the true lumen and minimal contrast medium in the false lumen of the celiac artery.
Twelve months later, computed tomographic angiography (CTA) of the abdomen showed patency of both celiac stents with minimal contrast in the false lumen (Fig. 5), and the patient remained asymptomatic.
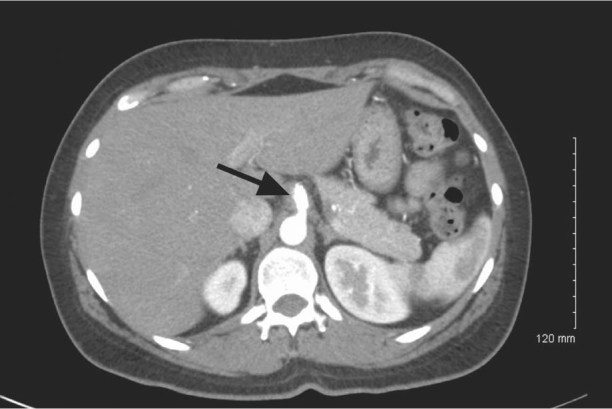
Fig. 5 After 12 months, computed tomogram shows stent patency (arrow) and substantial obliteration of the false lumen of the celiac artery.
Discussion
Isolated spontaneous celiac artery dissection is uncommon, and the diagnosis is rarely considered in patients who have acute abdominal pain. Our search of the Medline database yielded 33 reported cases.1–24 The superior mesenteric artery seems to be affected more often than the hepatic, splenic, left gastric, or celiac arteries.8 The first reported case of spontaneous celiac artery dissection was described in 1959.3 Only 13 cases were reported before 2001.8 Although the subsequent 20 cases might seem to be an unusual clustering of infrequent events, we believe that the introduction of multislice CTA for the diagnosis of abdominal pain accounts for the disparity.18 Spontaneous arterial dissection is 5 times more common in men than in women, and the average age of the patients is approximately 55 years.6 Accordingly, the spontaneous celiac artery dissection in our 41-year-old female patient is unusual. Spontaneous celiac artery dissection has typically been associated with hypertension, arteriosclerosis, degeneration of the arterial wall, trauma, pregnancy, and arteriopathy; however, no definite cause was found in many cases.1,7,8,14,19,21,24 Two patients had symptomatic dissection related to weightlifting,8,24 so microtrauma caused by a sudden increase in abdominal pressure or a significant surge in adrenergic hormones might have played a role.
The most common presenting symptom is the sudden onset of severe epigastric or hypochondrial pain. Most patients' physical examinations have yielded normal results except for epigastric tenderness. We found one report similar to ours: spontaneous celiac artery dissection with associated pancreatitis that was secondary to some degree of pancreatic ischemia.1
Magnetic resonance imaging, ultrasonography, and conventional angiography have been used in the diagnosis of splanchnic artery dissections; however, CTA is considered to be the imaging technique of choice.6,8 This method yields details of the mesenteric vasculature regardless of a patient's body mass or anatomic variants. In addition, CTA can display luminal borders and extraluminal disease in 3 dimensions.25
The natural progression of spontaneous celiac artery dissection is not fully understood. Severe sequelae include splenic infarction, intraperitoneal hemorrhage, and intestinal ischemia.6,8,12 It is debated whether surgical or endovascular treatment is better for uncomplicated but symptomatic spontaneous dissection. Patients with an incidentally detected celiac artery dissection should undergo CTA monitoring on a regular basis if medical therapy rather than corrective action is preferred.1,6,10,18,25
Surgery—once the treatment of choice when medical therapy failed5—has progressively given way to endovascular treatment.1 No published data support the superiority of either treatment. Conservative medical management might be appropriate for asymptomatic patients in whom there are no signs of ruptured celiac artery branches or bowel ischemia1,6,14,18,19 secondary to compression of the true lumen.25
Medical management consists of anticoagulative therapy. Continuous heparin administration is recommended while the patient is fasting or until the abdominal pain abates.1,6,14,18,19 Therapy can later be changed to oral warfarin until improvement is evident.11 If the need for anticoagulative therapy exceeds 6 months, we recommend that an invasive strategy be considered, because lifelong warfarin therapy has no proven benefit in patients with celiac artery dissection.
Some authors have advocated antiplatelet therapy during the acute stage of spontaneous dissection,1,13,24 because subendothelial injury can trigger thrombosis. Strict blood pressure control might prevent propagation of the dissection.13
A goal of optimal long-term conservative management is to identify a trigger, such as malperfusion or rupture, that would indicate the need for operative or endovascular intervention before adverse sequelae occur.18 Persistent or recurrent symptoms should raise suspicion of an undetected propagation of the dissection, expansion of the false lumen, or ischemia.
Endovascular intervention has been successful in treating spontaneous dissection of the superior mesenteric artery.9 We found 3 instances in which stenting was used to treat celiac artery dissection. Intervention respectively involved the use of a self-expanding stent (WALLSTENT®; Boston Scientific Corporation; Natick, Mass),18 a balloon-expandable bare-metal stent (Genesis®, Cordis),18 and a covered stent for a possible contained rupture.1 There are also reports of balloon fenestration17 and transcatheter embolization with coils.20 As with our patient, all the patients who underwent endovascular stenting had minimal sequelae, a complete resolution of symptoms, and no reported stenosis or progression of the dissection upon follow-up examination. However, the reported cases are too few and the follow-up periods too brief to yield definitive conclusions.
Potential advantages of stenting versus surgery include shorter hospital stays, less need for anticoagulation, and reduced radiation exposure from serial imaging. Potential disadvantages include stent thrombosis, restenosis, and procedure-related sequelae such as access-site complications. We would reserve surgical intervention for lesions that are inaccessible through an endovascular approach or for patients in whom angiography is contraindicated. Otherwise, stenting appears to be feasible as a primary treatment in patients with uncomplicated spontaneous celiac artery dissection.
Acknowledgment
Stephen N. Palmer, PhD, ELS, contributed to the editing of the manuscript.
Footnotes
Address for reprints: Neil E. Strickman, MD, 6624 Fannin St., Suite 2480, Houston, TX 77030
E-mail: NStrickman@hgcardio.com
References
- 1.Amabile P, Ouaissi M, Cohen S, Piquet P. Conservative treatment of spontaneous and isolated dissection of mesenteric arteries. Ann Vasc Surg 2009;23(6):738–44. [DOI] [PubMed]
- 2.Batsis JA, Arora AS. Celiac artery dissection: an uncommon cause of abdominal pain and weight loss. Clin Gastroenterol Hepatol 2005;3(10):A30. [DOI] [PubMed]
- 3.Foord AG, Lewis RD. Primary dissecting aneurysms of peripheral and pulmonary arteries: dissecting hemorrhage of media. Arch Pathol 1959;68:553–77. [PubMed]
- 4.Chaillou P, Moussu P, Noel SF, Sagan C, Pistorius MA, Langlard JM, Patra P. Spontaneous dissection of the celiac artery. Ann Vasc Surg 1997;11(4):413–5. [DOI] [PubMed]
- 5.Cormier F, Ferry J, Artru B, Wechsler B, Cormier JM. Dissecting aneurysms of the main trunk of the superior mesenteric artery. J Vasc Surg 1992;15(2):424–30. [PubMed]
- 6.D'Ambrosio N, Friedman B, Siegel D, Katz D, Newatia A, Hines J. Spontaneous isolated dissection of the celiac artery: CT findings in adults. AJR Am J Roentgenol 2007;188(6): W506–11. [DOI] [PubMed]
- 7.Fenoglio L, Allione A, Scalabrino E, Alberto G, Benedetti V, Pomero F, et al. Spontaneous dissection of the celiac artery: a pitfall in the diagnosis of acute abdominal pain. Presentation of two cases. Dig Dis Sci 2004;49(7–8):1223–7. [DOI] [PubMed]
- 8.Glehen O, Feugier P, Aleksic Y, Delannoy P, Chevalier JM. Spontaneous dissection of the celiac artery. Ann Vasc Surg 2001;15(6):687–92. [DOI] [PubMed]
- 9.Gobble RM, Brill ER, Rockman CB, Hecht EM, Lamparello PJ, Jacobowitz GR, Maldonado TS. Endovascular treatment of spontaneous dissections of the superior mesenteric artery. J Vasc Surg 2009;50(6):1326–32. [DOI] [PubMed]
- 10.Kang TL, Teich DL, McGillicuddy DC. Isolated, spontaneous superior mesenteric and celiac artery dissection: case report and review of literature. J Emerg Med 2011;40(2):e21–5. [DOI] [PubMed]
- 11.Nagai T, Torishima R, Uchida A, Nakashima H, Takahashi K, Okawara H, et al. Spontaneous dissection of the superior mesenteric artery in four cases treated with anticoagulation therapy. Intern Med 2004;43(6):473–8. [DOI] [PubMed]
- 12.Nordanstig J, Gerdes H, Kocys E. Spontaneous isolated dissection of the celiac trunk with rupture of the proximal splenic artery: a case report. Eur J Vasc Endovasc Surg 2009;37(2):194–7. [DOI] [PubMed]
- 13.Ozaki N, Wakita N, Yamada A, Tanaka Y. Spontaneous dissection of the splanchnic arteries. Interact Cardiovasc Thorac Surg 2010;10(4):656–8. [DOI] [PubMed]
- 14.Poylin V, Hile C, Campbell D. Medical management of spontaneous celiac artery dissection: case report and literature review. Vasc Endovascular Surg 2008;42(1):62–4. [DOI] [PubMed]
- 15.Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med 2001;344(12):898–906. [DOI] [PubMed]
- 16.Sheldon PJ, Esther JB, Sheldon EL, Sparks SR, Brophy DP, Oglevie SB. Spontaneous dissection of the superior mesenteric artery. Cardiovasc Intervent Radiol 2001;24(5):329–31. [DOI] [PubMed]
- 17.So YH, Chung JW, Park JH. Balloon fenestration of iatrogenic celiac artery dissection. J Vasc Interv Radiol 2003;14(4):493–6. [DOI] [PubMed]
- 18.Takach TJ, Madjarov JM, Holleman JH, Robicsek F, Roush TS. Spontaneous splanchnic dissection: application and timing of therapeutic options. J Vasc Surg 2009;50(3):557–63. [DOI] [PubMed]
- 19.Takayama T, Miyata T, Shirakawa M, Nagawa H. Isolated spontaneous dissection of the splanchnic arteries. J Vasc Surg 2008;48(2):329–33. [DOI] [PubMed]
- 20.Takeda H, Matsunaga N, Sakamoto I, Obata S, Nakamura S, Hayashi K. Spontaneous dissection of the celiac and hepatic arteries treated by transcatheter embolization. AJR Am J Roentgenol 1995;165(5):1288–9. [DOI] [PubMed]
- 21.Woolard JD, Ammar AD. Spontaneous dissection of the celiac artery: a case report. J Vasc Surg 2007;45(6):1256–8. [DOI] [PubMed]
- 22.Zainoun B, Geffroy Y, Weber-Donat G, Chavihot C, Teriitehau C, Minvielle F, Baccialone J. A rare cause of epigastric pain: isolated spontaneous dissection of the celiac artery, a case report [in French]. J Mal Vasc 2009;34(4):275–8. [DOI] [PubMed]
- 23.Zeina AR, Nachtigal A, Troitsa A, Admon G, Avshovich N. Isolated spontaneous dissection of the celiac trunk in a patient with bicuspid aortic valve. Vasc Health Risk Manag 2010;6:383–6. [DOI] [PMC free article] [PubMed]
- 24.Zhang WW, Killeen JD, Chiriano J, Bianchi C, Teruya TH, Abou-Zamzam AM. Management of symptomatic spontaneous isolated visceral artery dissection: is emergent intervention mandatory? Ann Vasc Surg 2009;23(1):90–4. [DOI] [PubMed]
- 25.Subhas G, Gupta A, Nawalany M, Oppat WF. Spontaneous isolated superior mesenteric artery dissection: a case report and literature review with management algorithm. Ann Vasc Surg 2009;23(6):788–98. [DOI] [PubMed]


