Abstract
In selected patients, transcatheter closure of atrial septal defects with the AMPLATZER Septal Occluder has yielded excellent results. However, there is a slight risk of device embolization after deployment. We report the case of a 26-year-old woman in whom an embolized AMPLATZER device was retrieved percutaneously from the right pulmonary artery. We also discuss important technical principles for managing this uncommon but potentially severe complication.
Key words: Device removal/methods; embolization, therapeutic/instrumentation; heart catheterization/instrumentation; heart septal defects, atrial/ultrasonography; patient selection; prosthesis implantation/adverse effects; prostheses and implants; septal occluder device/adverse effects; treatment outcome
Transcatheter closure of atrial septal defects (ASDs) with use of the AMPLATZER® Septal Occluder (St. Jude Medical, Inc.; St. Paul, Minn) has yielded excellent results in properly selected patients.1,2 The major advantage of the AMPLATZER occluder is its easy retrieval at all stages of deployment before its final release from the delivery cable. Although embolization of AMPLATZER ASD occluders is rare, it can occur even when interventional cardiologists are experienced. Despite an earlier belief that the transcatheter retrieval of embolized AMPLATZER devices would be difficult, success rates from 50% to 75% have been reported.3,4 We describe the retrieval of an embolized AMPLATZER device in a young woman. In addition, we present some technical principles with which operators practicing device closure should be familiar.
Case Report
A 26-year-old woman presented with a 5-year history of shortness of breath and palpitations. Clinical examination revealed features that suggested a large ASD, and 2-dimensional echocardiography showed a 19-mm secundum ASD with an estimated right ventricular systolic pressure of 45 mmHg. Transesophageal echocardiography revealed adequacy of the caval and aortic rims of the defect. The patient was taken to the catheterization laboratory for transcatheter closure of the ASD, to be performed under fluoroscopic and echocardiographic guidance.
Balloon sizing of the defect was performed with use of a Meditech® sizing balloon (Boston Scientific Corporation; Natick, Mass). The stretched diameter of the defect was 20 mm. A 22-mm AMPLATZER Septal Occluder was chosen for defect closure. In accordance with protocol, the defect was crossed with use of a multipurpose catheter and with a 0.035-in Amplatz™ exchange guidewire (Boston Scientific) that was placed in the patient's right middle pulmonary vein. The AMPLATZER device was loaded onto the delivery system and introduced into a 10F long sheath that had already been placed over the exchange wire. After the device was advanced into the left atrium (LA), the long sheath was withdrawn into the right atrium (RA) until the LA disc opened and aligned itself with the interatrial septum. When continuous echocardiography confirmed adequate device positioning, the RA disc was opened, and the “Minnesota wiggle” maneuver5 was performed on the delivery cable to ensure satisfactory device positioning. It was noted at this time that the LA disc was seated somewhat obliquely across the interatrial septum (Fig. 1A); however, in view of the complete obliteration of color flow across the defect on echocardiography, and the seemingly stable position, we decided to leave the device in its current position.
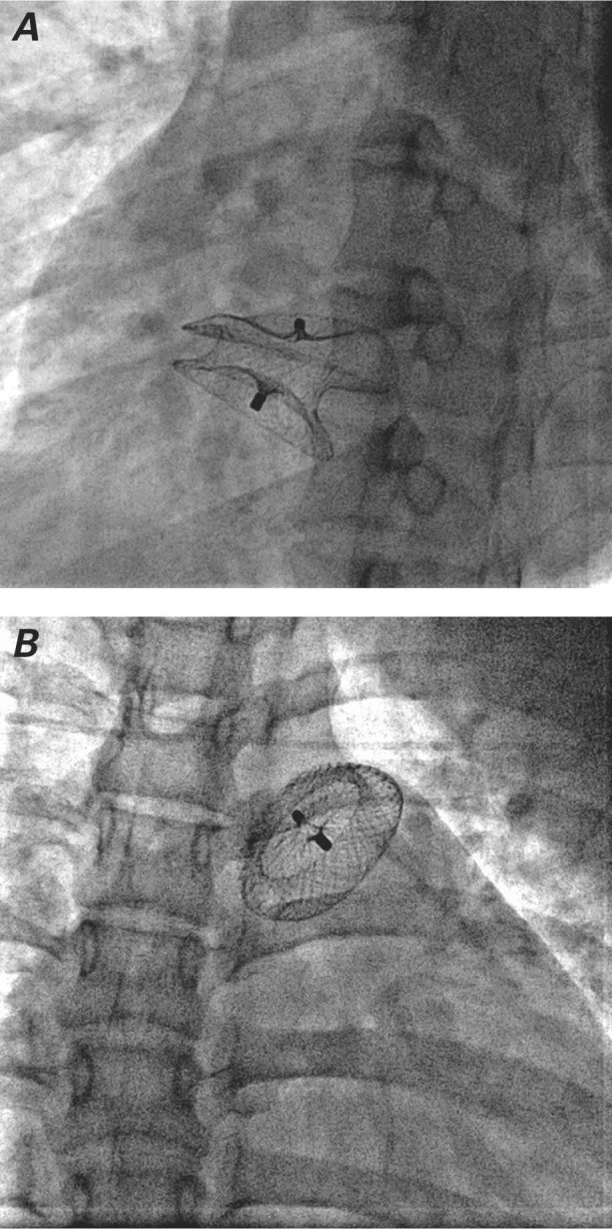
Fig. 1 Fluoroscopy shows A) the left atrial disc seated somewhat obliquely across the intra-atrial septum, and B) embolization of the occluder to the proximal right pulmonary artery.
A few minutes after deployment, the device embolized to the proximal right pulmonary artery (RPA) (Fig. 1B). The cardiac surgeons were alerted, but all operating rooms were occupied, and surgery was not expected to be an option within the next 2 hours. We decided to attempt percutaneous retrieval of the device while waiting, and to refer the patient for surgery if we were unsuccessful.
Percutaneous Retrieval
A 15-mm Amplatz GooseNeck® Snare (eV3 Endovascular, Inc.; part of Covidien; Plymouth, Minn) was introduced from the right femoral vein through a 12F sheath along with the 0.038-in tracker catheter provided with the snare. We then passed a 0.035-in guidewire from the left femoral vein into the RA and then into the RPA. We tried to position the wire close to the embolized device, and we manipulated the wire in an attempt to orient the screw on the RA disc toward the mouth of the snare to facilitate retrieval. Because stabilizing the device before retrieval is very important, we replaced the left femoral guidewire with a 6F pigtail catheter, which we placed across the RPA near the device. After the pigtail catheter had stabilized the device, the screw on the RA disc was snared successfully, despite its being centered slightly away from the mouth of the snare (Fig. 2A). With continuous gentle tension on the pigtail catheter and an increasingly intense pull on the snare, the RA disc was slenderized and retrieved into the long sheath. The entire device was then easily pulled into the sheath and successfully retrieved (Fig. 2B).
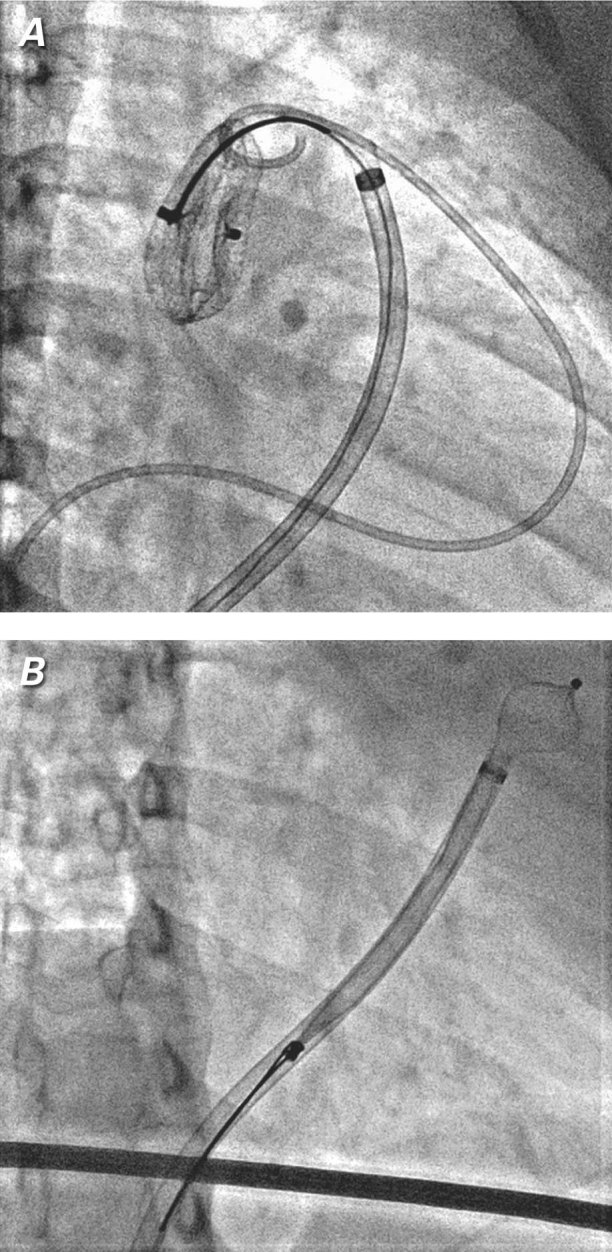
Fig. 2 Fluoroscopy shows A) successful snaring of the screw on the right atrial disc and B) subsequent slenderization of the right atrial disc and retrieval of the entire device into the long sheath.
Real-time motion images are available at www.texasheart.org/journal.
Subsequently, the same 22-mm AMPLATZER occluder was carefully deployed across the defect without any complications (Fig. 3). The patient was discharged from the hospital after 48 hours, after the device was echocardiographically confirmed to be properly placed.
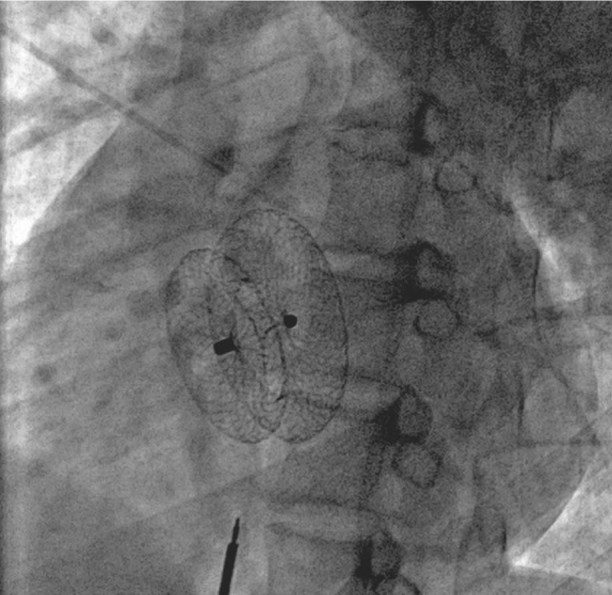
Fig. 3 Fluoroscopy shows final successful placement of the atrial septal occluder.
Discussion
After deployment of an ASD septal occluder, device embolization is known to occur in up to 0.5% of cases, even when the interventionalist is experienced.3,4 Using detailed echocardiography to evaluate the adequacy of the defect's rims is crucial in all patients in whom device closure is contemplated. By far, the most common cause of embolization is the use of an undersized device. Careful attention to technical details—such as noting the alignment of the discs across the interatrial septum, avoiding excessive tension on the delivery cable, or performing an excessive wiggle procedure—also helps to reduce the risk of embolization.
We think that imperfect alignment of the device across the interatrial septum was the cause of embolization in our patient. Although this misalignment was noted on fluoroscopy after the LA disc was deployed, we decided to deploy the device, because of the complete obliteration of color flow across the defect on echocardiography and the device's seemingly stable position.
Previously, clinicians thought that the transcatheter retrieval of embolized AMPLATZER devices would be difficult, and this prompted the use of surgical retrieval methods.4 However, a few cases of successful percutaneous retrieval were subsequently reported (overall success rates, 50%–75%), and our report adds to the literature.3,6–9 Embolized devices generally need to be completely retrieved; however, one can pull the RA disc back into the RA with a snare and reposition the same device across the ASD.10
Recommendations for Retrieval
Before retrieval, the embolized device should be stabilized. This has been achieved by either passing a stiff guidewire10 or using a bioptome to hold the LA disc while the RA disc is being snared.3,8,9 We used the 0.35-in guidewire to orient the screw on the RA disc to be coaxial with the snare and thus facilitate retrieval. After this, we chose a 6F pigtail catheter to stabilize the device while it was being snared at the RA disc end.
It has been suggested that firmly holding the device at both ends (by the LA and RA discs) facilitates slenderizing the embolized device into the sheath. Although, as mentioned above, operators have used a bioptome to secure the LA disc, we think that the force exerted by the bioptome is generally not strong enough to catch the RA disc screw lead and pull the device back into a sheath. In our patient, we could grip the RA screw with the snare while the pigtail catheter helped to stabilize the device. Nevertheless, we agree that if the device does not withdraw easily while pulling at only one end with the snare, it may be wise to secure and hold both ends of the device, to avoid device slippage or kinking of the sheath.
Retrieval should not be attempted by trying to snare the screw on the LA disk. All efforts must be made to snare the RA disc—and, before that, to orient the RA disc so that it is easily accessible and can be snared around the base of its screw.
Our use of a larger 12F sheath during retrieval (rather than the 10F sheath used for device deployment) enabled easier entry of the device into the sheath after the RA disc was snared. When the screw at the RA disc has been snared and an effort is made to slenderize the device, the device might get stuck in the sheath if it is even slightly noncoaxial. Therefore, one should use a slightly larger sheath than the one with the best fit. Apart from using oversized sheaths, other pertinent technical recommendations include using stiffer sheaths that are less likely to kink, and beveling one end of the sheath to facilitate easier entry of the screw into the sheath after snaring.
Footnotes
Address for reprints: Pravin K. Goel, DM, FACC, Department of Cardiology, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow 226014, India
E-mail: golf_pgi@yahoo.co.in
References
- 1.Du ZD, Hijazi ZM, Kleinman CS, Silverman NH, Larntz K; Amplatzer Investigators. Comparison between transcatheter and surgical closure of secundum atrial septal defect in children and adults: results of a multicenter nonrandomized trial. J Am Coll Cardiol 2002;39(11):1836–44. [DOI] [PubMed]
- 2.Majunke N, Bialkowski J, Wilson N, Szkutnik M, Kusa J, Baranowski A, et al. Closure of atrial septal defect with the Amplatzer septal occluder in adults. Am J Cardiol 2009;103(4):550–4. [DOI] [PubMed]
- 3.Levi DS, Moore JW. Embolization and retrieval of the Amplatzer septal occluder. Catheter Cardiovasc Interv 2004;61 (4):543–7. [DOI] [PubMed]
- 4.Chessa M, Carminati M, Butera G, Bini RM, Drago M, Rosti L, et al. Early and late complications associated with transcatheter occlusion of secundum atrial septal defect. J Am Coll Cardiol 2002;39(6):1061–5. [DOI] [PubMed]
- 5.Hernandez F, Garcia-Tejada J, Velazquez M, Albarran A, Andreu J, Tascon J. Intracardiac echocardiography and percutaneous closure of atrial septal defects in adults [in Spanish]. Rev Esp Cardiol 2008;61(5):465–70 [PubMed]
- 6.Wilkinson JL, Goh TH. Early clinical experience with use of the “Amplatzer Septal Occluder” device for atrial septal defect. Cardiol Young 1998;8(3):295–302. [DOI] [PubMed]
- 7.Balbi M, Pongiglione G, Bezante GP. Percutaneous rescue of left ventricular embolized Amplatzer septal occluder device. Catheter Cardiovasc Interv 2008;72(4):559–62. [DOI] [PubMed]
- 8.Shirodkar S, Patil S, Pinto R, Dalvi B. Successful retrieval of migrated Amplatzer septal occluder. Ann Pediatr Cardiol 2010;3(1):83–6. [DOI] [PMC free article] [PubMed]
- 9.Chan KT, Cheng BC. Retrieval of an embolized Amplatzer septal occluder. Catheter Cardiovasc Interv 2010;75(3):465–8. [DOI] [PubMed]
- 10.Peuster M, Boekenkamp R, Kaulitz R, Fink C, Hausdorf G. Transcatheter retrieval and repositioning of an Amplatzer device embolized into the left atrium. Catheter Cardiovasc Interv 2000;51(3):297–300. [DOI] [PubMed]


