Abstract
Background & objectives:
Diarrhoeal disease is the fifth leading cause of all mortality globally. To this burden, rotavirus contributes over half a million deaths annually. This pilot study was conducted to determine the economic burden of diarrhoeal episodes on families from different geographical regions accessing medical facilities in India.
Methods:
Participants were enrolled from four study sites with eight reporting hospitals, categorized as non-profit and low cost, private and government facilities between November 2008 and February 2009. Questionnaires detailing healthcare utilization, medical and non-medical expenditure and lost income were completed by families of children < 5 yr of age hospitalized for gastroenteritis. All available faecal samples were tested for rotavirus.
Results:
A total of 211 patients were enrolled. The mean total cost of a hospitalized diarrhoeal episode was  3633 (US$ 66.05) for all facilities, with a marked difference in direct costs between governmental and non-governmental facilities. Costs for rotavirus positive hospitalizations were slightly lower, at
3633 (US$ 66.05) for all facilities, with a marked difference in direct costs between governmental and non-governmental facilities. Costs for rotavirus positive hospitalizations were slightly lower, at  2956 (US$ 53.75). The median cost of a diarrhoeal episode based on annual household expenditure was 6.4 per cent for all-cause diarrhoea and 7.6 per cent for rotavirus diarrhoea. Of the 124 samples collected, 66 (53%) were positive for rotavirus.
2956 (US$ 53.75). The median cost of a diarrhoeal episode based on annual household expenditure was 6.4 per cent for all-cause diarrhoea and 7.6 per cent for rotavirus diarrhoea. Of the 124 samples collected, 66 (53%) were positive for rotavirus.
Interpretation & conclusions:
Data on direct costs alone from multiple facilities show that diarrhoeal disease constitutes a large economic burden on Indian families. Affordable, effective vaccines would greatly reduce the economic burden of severe gastroenteritis on patients, families and the government.
Keywords: Costs, diarrhoea, economic burden, India, rotavirus
Multi-cause proportionate mortality models used by the Child Health Epidemiology Reference Group of the World Health Organization to estimate deaths have recently shown that of the estimated 8.8 million deaths in children younger than 5 yr worldwide in 2008, infectious diseases caused 68 per cent, with 15 per cent due to diarrhoea1. The acute illness causes a heavy disease burden on individuals and the healthcare system, but may also have long-term consequences on the physical and mental development of children2. Hence, adequate preventive measures need to be considered to decrease disease burden and prevent subsequent disability.
Rotavirus results in about half a million deaths annually in the world3, and in India, it accounts for approximately 39 per cent of diarrhoeal admissions4, making the case for considering vaccination as a preventive strategy. However, in evaluating the possible deployment of vaccines, it is essential to consider the economic burden of the disease and the cost of vaccination. Several studies from Asia have demonstrated that rotavirus is the main cause of diarrhoeal disease in children and constitutes a considerable economic burden. A study from Vellore5 showed that 5.8 per cent of the annual household income was spent on one hospitalization of a child due to rotavirus diarrhoea. Another study6 showed that India spends  2.0-3.4 billion annually to treat rotavirus disease in children less than five years of age. This study used the costing data from two geographical regions in India and hypothetically calculated the overall burden for the whole country.
2.0-3.4 billion annually to treat rotavirus disease in children less than five years of age. This study used the costing data from two geographical regions in India and hypothetically calculated the overall burden for the whole country.
In this pilot study, we present data from a pilot project to estimate the direct costs of hospitalization due to diarrhoea in different geographical regions in India and at different types of medical facilities in the context of an ongoing surveillance network for rotavirus gastroenteritis.
Material & Methods
A multi-centre, hospital-based network with four laboratories and 10 hospitals in seven different regions of India carried out rotavirus strain surveillance from September 2005 to June 2009. At each hospital, children aged <5 yr who presented with acute gastroenteritis and required hospitalization with rehydration for at least 6 h were enrolled4. For the costing study, families of children hospitalized with acute gastroenteritis between November 2008 and February 2009 were asked for information on costs incurred due to the diarrhoeal admission. The study was approved by the institutional review boards or ethics committees of all the recruiting hospitals and a separate consent was obtained for participating in the costing study.
The questionnaires for estimating costs were based on the WHO guidelines7 for estimating the economic burden of diarrhoeal disease. The questionnaires assessed direct medical costs, non-medical indirect costs and lost wages (indirect costs), which were calculated for pre-visit and inpatient costs for all hospitalizations. Monthly estimated expenditures for food, education, rent, household items and medical care were multiplied by 12 to obtain annual household expenditure. The sample size was determined based on the WHO guidelines7, using an estimate of at least 500 patients having been treated at each facility in the past year, with a coefficient of variation of 0.5 and a precision of 15 per cent, which would require 41 patients at each facility. However, because feasibility and resources did not permit sampling for one whole year, the size was increased to 50 at each site, even though the study was carried out during the winter when disease burden in northern India is known to be greater4. Since this was a pilot study nested within a strain surveillance study, sample size calculation and analysis were not adjusted for design effect or clustering.
Participants were enrolled from four study sites with eight reporting hospitals, categorized as non-profit referral and non-profit concessional, private and government facilities. The study site from the southern region, Christian Medical College (CMC), Vellore, was represented by the main hospital which operates as a no-profit, no-loss basis referral hospital for general patients and the Community Health and Development Hospital (CHAD), which is a low cost unit offering concessional care to the community. At CMC, patients pay for all direct costs incurred including for admission, diagnostic tests and drugs and these are calculated for the general ward on a no-profit, no-loss basis. At CHAD, the patients pay for all direct costs incurred including for admission, diagnostic tests and drugs, but the facilities provided are basic, with less nursing and diagnostic support and costs are calculated at a concessional rate that is approximately two-thirds of actual health care facility costs. The King Edward Memorial Hospital (KEM), Shaishav Children's Hospital and Bharati Hospital, all non-governmental private institutions, were the reporting hospitals for the National Institute of Virology (NIV) at Pune, representing the western region, and patients pay for all direct costs incurred including for admission, diagnostic tests and drugs as calculated by the respective hospital management. The B.C. Roy Memorial Government Hospital (BCH) and ID & B General Government Hospital (ID & BG) were under the National Institute of Cholera and Enteric Diseases (NICED), Kolkata, in the eastern region and patients pay no cost for admission, but may have to pay for drugs not available in the Hospital Pharmacy. The All India Institute of Medical Sciences (AIIMS), New Delhi, was the study site for the northern region, where patients pay a standard fee at attendance, but do not pay for admission, diagnostic tests or drugs. At all sites, costs related to travel, stay, food, etc., are borne by patients and their families.
Faecal samples collected from children were tested for rotavirus by an enzyme-linked immunosorbent assay4.
Results
Initially, each centre was expected to enroll 50 patients during the study period. The centres from Vellore and Delhi could enroll 50 patients each, while the centre at Kolkata could enroll only 25 patients, and the centre from Pune, with three private hospitals, enrolled 86 patients. Hence it was decided to retain all 211 participants with complete data. The enrollment was as follows, 22 from CHAD hospital, 28 from CMC, 75 from government hospitals (AIIMS-50 and NICED-25) and 86 from private institutions (KEM-10, Shaishav Children's Hospital - 39 and Bharathi Hospital- 37) . The mean age of enrolled children was 14 months (inter-quartile range, IQR 1-58 months), with 71 (34%) females and 139 (66%) males. On an average, the children had traveled 62 min (IQR 5 to 240 min) to reach the facilities. The median hospital stay was three days (IQR 2 -5 days). Overall, 164 samples were collected from 211 patients, of which, 124 samples were adequate for testing. Reasons for non-collection of samples were that the child either passed stool at night or did not pass a stool after admission. Of the 124 samples tested, 66 (53%) had rotavirus identified in stool.
The mean total cost of hospitalization for one diarrhoeal episode was  3633 (US$ 66.05, 1 US$=55
3633 (US$ 66.05, 1 US$=55  for any-cause diarrhoea and that for children admitted with rotavirus diarrhoea was
for any-cause diarrhoea and that for children admitted with rotavirus diarrhoea was  2,956 (US$ 53.75) across all facilities. The mean expenditure for one diarrhoeal episode for non-profit referral hospital and private hospitals were
2,956 (US$ 53.75) across all facilities. The mean expenditure for one diarrhoeal episode for non-profit referral hospital and private hospitals were  6634 and 6071, respectively. For non-profit low-cost/concessional hospital and government hospitals it was
6634 and 6071, respectively. For non-profit low-cost/concessional hospital and government hospitals it was  1869 and 233, respectively (Table).
1869 and 233, respectively (Table).
Table.
Mean and inter-quartile range of costs in Indian Rupees ( ) per diarrhoeal episode at different study sites and for rotavirus positive diarrhoea
) per diarrhoeal episode at different study sites and for rotavirus positive diarrhoea
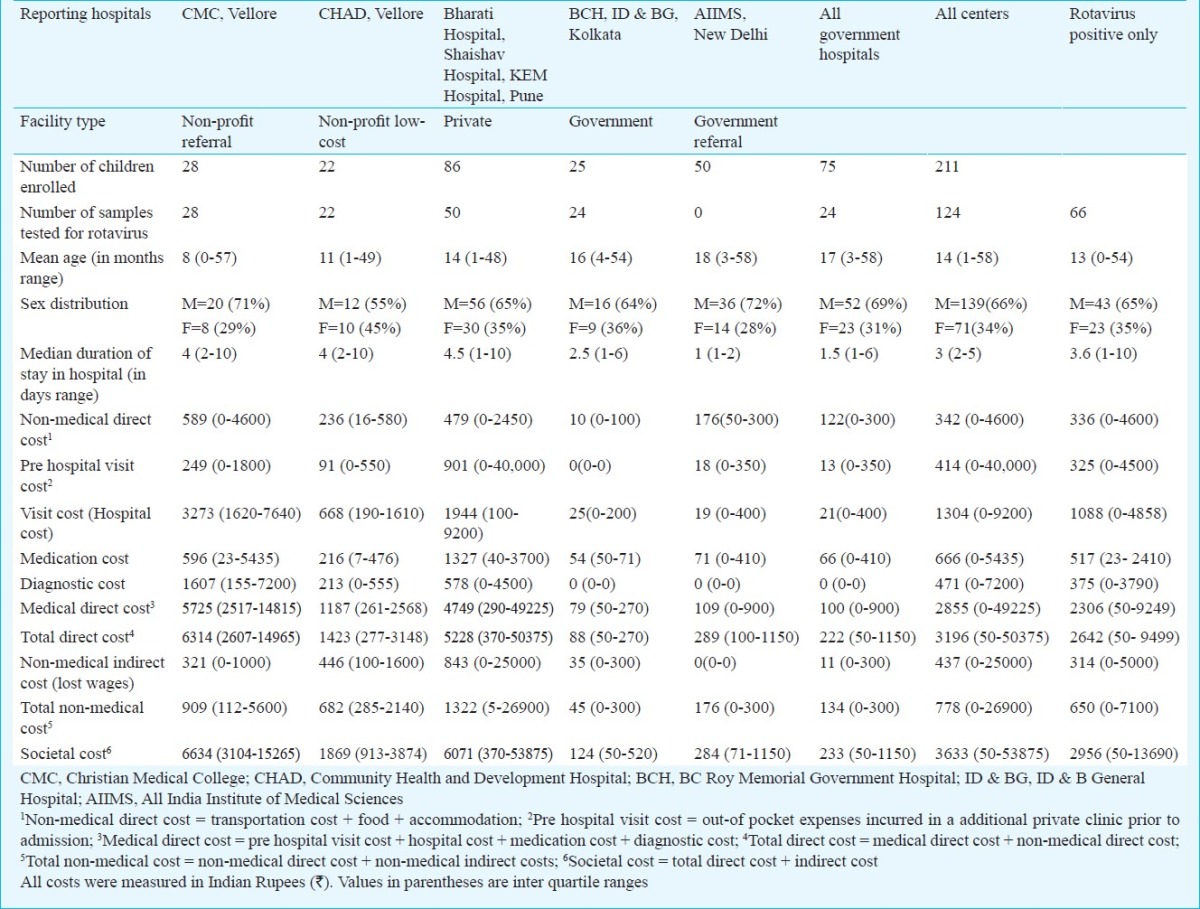
During one diarrhoeal admission, on an average, 36 per cent of the expenses were on the hospital visit/admission costs followed by 18 per cent medication costs, 13 per cent diagnostic costs and 11 per cent prehospital visit costs. Non-medical costs accounted for 21 per cent of the overall expenses.
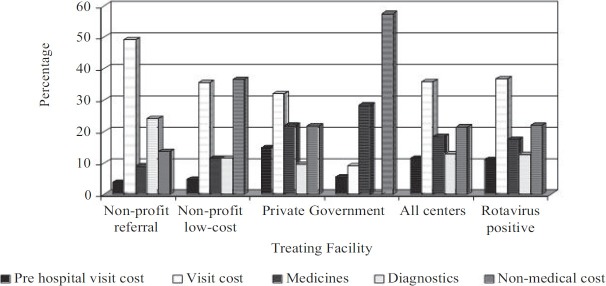
The Fig. shows the proportion of expenditure on cost heads for the different treating facilities. In the private, non-profit referral and non-profit low cost/concessional hospital, or all categories of non-governmental hospitals, the largest proportion of expenditure was on hospital visit costs. In the government hospitals, the largest proportion of the expenditure was towards non-medical expenses. Among the 86 patients admitted to private hospitals, 55 (64%) had sought treatment from other medical facilities prior to admission.
Fig. 1.
Proportion of costs for different treating facilities and rotavirus positive cases.
Of the 211 patients enrolled, 136 (64%) sought treatment from non-governmental facilities and 82 of 136 (60.2%) borrowed money to pay for the diarrhoeal admission. The median annual household income across all the facilities was  34,800 (US$ 773), with 6.4 per cent of annual income spent on one diarrhoeal episode. In rotavirus positive children, the income and proportional expenditure were
34,800 (US$ 773), with 6.4 per cent of annual income spent on one diarrhoeal episode. In rotavirus positive children, the income and proportional expenditure were  20,340 (US$ 452) and 7.6 per cent, respectively.
20,340 (US$ 452) and 7.6 per cent, respectively.
Discussion
Rotavirus infection occurs universally in developed and developing countries. Though rotavirus is spread mainly through the faeco-oral route, improvement in hygiene does not reduce the disease prevalence. Infection with mild to moderate dehydration can be treated with oral rehydration, while severe infections need specialized care, which may not always be available in developing countries. Hence, implementation of affordable and effective vaccines to prevent morbidity and mortality associated with rotavirus diarrhoea is needed. In order to evaluate cost-effectiveness of vaccines in the public health system, the economic burden of rotavirus diarrhoea must be estimated to carry out relevant analyses. In our study, the overall mean cost for treating one episode of rotavirus diarrhoea across the country was  2,956 (US$ 53.75). The estimates from India fall within the range of cost estimates for diarrhoeal hospitalizations available from Vietnam (US$ 36), Ghana (US$ 65.14-133.86) and Kenya (US$ 100)8–10. Since healthcare costs in most middle-income and developed countries are higher, estimates of the costs of hospitalization are also high, up to US$ 3135 in privately insured US children hospitalized for rotavirus gastroenteritis11.
2,956 (US$ 53.75). The estimates from India fall within the range of cost estimates for diarrhoeal hospitalizations available from Vietnam (US$ 36), Ghana (US$ 65.14-133.86) and Kenya (US$ 100)8–10. Since healthcare costs in most middle-income and developed countries are higher, estimates of the costs of hospitalization are also high, up to US$ 3135 in privately insured US children hospitalized for rotavirus gastroenteritis11.
In this study, the patients were seen in several parts of the country and in different kinds of facilities, providing a wide range of costs that made it possible to estimate cost components for almost all kinds of facilities. As expected, direct costs were higher for non-governmental facilities, because treatment at the government hospitals is provided at a subsidized rate and, therefore, the bulk of the direct expenditure was on food, accommodation and transport rather than the real costs of provision of health care. Additionally, in government facilities, the average number of days of admission was lower, resulting in lower costs. In this study, higher costs were reported from non-governmental health care facilities, with private and the non-profit referral hospital having almost similar overall costs. However, as might be expected laboratory or diagnostic costs formed a significant proportion of the expenditure at the referral hospitals, but medication costs were higher at the private hospitals.
Previously, the rates of rotavirus positivity in India have been shown to be between 35 to 53 per cent and 6 to 45 per cent at different kinds of facilities12,13. In this study, 53 per cent of the tested samples were positive for rotavirus. There was little difference in the proportion of expenditure spent on different cost categories between all-cause diarrhoea and rotavirus positive diarrhoea.
Hospitalization for a single diarrhoeal episode consumed a median of 6.4 per cent of annual income. This is consistent with previous studies conducted in India at Vellore where hospitalization for diarrhoea required a median expenditure of 5.8 per cent of annual income5. This was a significant burden on individual households as approximately 70 per cent of expenditure on health care is estimated to be borne by households in India14.
For decreasing the burden of diarrhoeal disease, several interventions and treatments are available. Interventions that prevent diarrhoea include improvements in water supplies, sanitation and hygiene, the promotion of breastfeeding, vitamin A supplementation, and vaccination against rotavirus, while treatment for diarrhoea include oral rehydration salts, zinc supplementation, and antibiotics for dysentery15. Of the vaccines available, the two currently widely available rotavirus vaccines cost between  2200 and 2700 per course. An analysis based on available data indicates that a universal rotavirus vaccine programme for India could be cost-effective based on a decision rule whereby an intervention that averts one disability-adjusted life-year for less than India's GDP per capita (US$ 1017 in 2008) is considered to be a highly cost-effective intervention16. However, if in the future, local manufacturers make available the vaccine at a much lower price per dose, rotavirus vaccine may offer an important option for the Government of India to help reach the Millenium Development Goal 4 target17.
2200 and 2700 per course. An analysis based on available data indicates that a universal rotavirus vaccine programme for India could be cost-effective based on a decision rule whereby an intervention that averts one disability-adjusted life-year for less than India's GDP per capita (US$ 1017 in 2008) is considered to be a highly cost-effective intervention16. However, if in the future, local manufacturers make available the vaccine at a much lower price per dose, rotavirus vaccine may offer an important option for the Government of India to help reach the Millenium Development Goal 4 target17.
This pilot study did not take into account several factors, including the severity of disease, the availability of other systems of medicine, healthcare utilization patterns and the actual costs to the healthcare system, all of which can play an important role in determining the treatment required and the economic burden of diarrhoeal disease on society. However, the data obtained from direct costs alone by sampling multiple facilities have shown that diarrhoeal disease constitutes a large economic burden on Indian families. Preventive strategies are needed to reduce mortality, morbidity and the economic burden due to diarrhoeal disease.
Acknowledgment
This study was supported by the Indian Council of Medical Research, New Delhi.
References
- 1.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 2.Parashar UD, Burton A, Lanata C, Boschi-Pinto C, Shibuya K, Steele D, et al. Global mortality associated with rotavirus disease among children in 2004. J Infect Dis. 2009;200(Suppl 1):S9–S15. doi: 10.1086/605025. [DOI] [PubMed] [Google Scholar]
- 3.Guerrant RL KM, Moore S, Lorntz B, Brantley R, Lima AA. Magnitude and impact of diarrhoeal disease. Arch Med Res. 2002;33:351–5. doi: 10.1016/s0188-4409(02)00379-x. [DOI] [PubMed] [Google Scholar]
- 4.Kang G, Arora R, Chitambar SD, Deshpande JM, Gupte MD, Kulkarni M, et al. Multicenter, hospital-based surveillance of rotavirus disease and strains among Indian children aged <5 years. J Infect Dis. 2009;200(Suppl 1):S147–53. doi: 10.1086/605031. [DOI] [PubMed] [Google Scholar]
- 5.Mendelsohn AS, Asirvatham JR, Mkaya Mwamburi D, Sowmyanarayanan TV, Malik V, Muliyil J, et al. Estimates of the economic burden of rotavirus-associated and all-cause diarrhoea in Vellore, India. Trop Med Int Health. 2008;13:934–42. doi: 10.1111/j.1365-3156.2008.02094.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tate JE, Chitambar S, Esposito DH, Sarkar R, Gladstone B, Ramani S, et al. Disease and economic burden of rotavirus diarrhoea in India. Vaccine. 2009;27(Suppl 5):F18–24. doi: 10.1016/j.vaccine.2009.08.098. [DOI] [PubMed] [Google Scholar]
- 7.Guidelines for estimating the economic burden of diarrhoeal disease with focus on assessing the costs of rotavirus diarrhoea. WHO/IVB/05.10. Geneva: WHO; 2005. World Health Organization. [Google Scholar]
- 8.Fischer TK, Anh DD, Antil L, Cat ND, Kilgore PE, Thiem VD, et al. Health care costs of diarrheal disease and estimates of the cost-effectiveness of rotavirus vaccination in Vietnam. J Infect Dis. 2005;192:1720–6. doi: 10.1086/497339. [DOI] [PubMed] [Google Scholar]
- 9.Osano BO, Wang’ombe JK, Kamenwa RW, Wamalwa D. Cost analysis of care for children admitted to kenyatta national hospital with rotavirus gastroenteritis. Vaccine. 2011;29:4019–24. doi: 10.1016/j.vaccine.2011.03.053. [DOI] [PubMed] [Google Scholar]
- 10.Aikins M, Armah G, Akazili J, Hodgson A. Hospital health care cost of diarrheal disease in Northern Ghana. J Infect Dis. 2010;202(Suppl):S126–30. doi: 10.1086/653573. [DOI] [PubMed] [Google Scholar]
- 11.Cortes JE, Curns AT, Tate JE, Parashar UD. Trends in healthcare utilization for diarrhea and rotavirus disease in privately insured US children <5 years of age, 2001-2006. Pediatr Infect Dis J. 2009;28:874–8. doi: 10.1097/INF.0b013e3181a653cd. [DOI] [PubMed] [Google Scholar]
- 12.Tate JE, Chitambar S, Esposito DH, Sarkar R, Gladstone B, Ramani S, et al. Disease and economic burden of rotavirus diarrhoea in India. Vaccine. 2009;27(Suppl 5):F18–24. doi: 10.1016/j.vaccine.2009.08.098. [DOI] [PubMed] [Google Scholar]
- 13.Ramani S, Kang G. Burden of disease and molecular epidemiology of group A rotavirus infections in India. Indian J Med Res. 2007;125:619–32. [PMC free article] [PubMed] [Google Scholar]
- 14.Rao KS. Report of the National Commission on Macroeconomic and Health. New Delhi: Ministry of Health and Family Welfare. Government of India; 2005. Section IV. Financing of health in India. [Google Scholar]
- 15.Fischer Walker CL, Friberg IK, Binkin N, Young M, Walker N, Fontaine O, et al. Scaling up diarrhea prevention and treatment interventions: a Lives Saved Tool analysis. PLoS Med. 2011;8:e1000428. doi: 10.1371/journal.pmed.1000428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Esposito DH, Tate JE, Kang G, Parashar UD. Projected impact and cost-effectiveness of a rotavirus vaccination program in India, 2008. Clin Infect Dis. 2011;52:171–7. doi: 10.1093/cid/ciq094. [DOI] [PubMed] [Google Scholar]
- 17.Nelson EA, Walker DG. Reaching MDG 4 in India: a role for rotavirus vaccine? Clin Infect Dis. 2011;52:178–9. doi: 10.1093/cid/ciq095. [DOI] [PubMed] [Google Scholar]