Abstract
Background & objectives:
Cervical cancer has a major impact on woman's lives worldwide and one in every five women suffering from cervical cancer belongs to India. Hence the objectives of this study were to find the knowledge of women regarding cervical cancer, to determine screening practices and determinants, and to identify factors for non screening.
Methods:
A cross-sectional study was conducted in Vypin Block of Ernakulam District, Kerala, India where four of the seven Panchayats were randomly chosen. Households were selected by systematic random sampling taking every second house in the tenth ward of the Panchayat till at least 200 women were interviewed. Thus, 809 women were interviewed from four Panchayats.
Results:
Mean age of the study population was 34.5 + 9.23 yr. Three fourths of the population (74.2%) knew that cervical cancer could be detected early by a screening test. Majority of respondents (89.2%) did not know any risk factor for cervical cancer. Of the 809 women studied, only 6.9 per cent had undergone screening. One third of the population were desirous of undergoing screening test but had not done it due to various factors. These factors related to knowledge (51.4%) such as no symptoms, not being aware of Pap test, not necessary, etc. This was followed by resource factors (15.1%) like no time, no money, etc. and psychosocial factors (10.2%) included lack of interest, fear of procedure, etc. Independent predictors for doing Pap test included age >35, having knowledge of screening for cervical cancer and Pap test (P<0.05).
Interpretation & conclusions:
Specific knowledge on cervical cancer screening is a critical element in determining whether a woman will undergo Pap test in addition to making cancer screening facilities available in the primary health centre.
Keywords: Cervical cancer, knowledge, practice, screening
Cervical cancer, the third most common cancer among women in the world, was responsible for 275,000 deaths in 2008, 88 per cent of which occurred in developing countries and 159,800 in Asia1. One in every five women in the world suffering from cervical cancer belongs to India which has the largest burden of cervical cancer patients in the world2. The disease consumes resources at a staggering rate in the way of medical, non-medical spending and lost productivity3. Although cervical cancer is the most frequent cancer diagnosed in Indian women, age-adjusted incidence rates vary from 8.8 per 100,000 women population in Thiruvananthapuram to 22.5 per 100,000 women population in Aizwal4.
It is possible to prevent deaths due to cervical cancer through various strategies that target women >30 yr for screening and treatment5. The introduction of Papanicolaou test led to significant reduction in mortality and morbidity in developed countries where proportion of women who are screened by Pap test vary from 68 to 84 per cent6–8. On the other hand, the screening coverage in Asian countries is low and varies from 50 per cent in Singapore which has an existing Cancer Screening Programme to 2.6-5 per cent in India7,9,10. Despite existence of national guidelines the screening coverage in India is appalling and is mainly attributed to inequality between infrastructure, resources and outsized population2. As a result, very often diagnosis of cervical cancer is based on opportunistic screening or after the onset of symptoms. Though data from the 20 populations based cancer registries in India indicate a steady decline in cervical cancer incidence rates over the last two decades, it still occupies number two position and the risk of disease is still high4. These registries are predominantly urban and in the rural cancer registry in Barshi the risk of cancer of cervix was considerably high compared to urban Mumbai registry and it accounted for half the cancer burden11.
Thus in India, the onus of preventing cervical cancer is on the women themselves. Therefore, it is the women's knowledge level, motivation for screening and other psychosocial factors that determine her health seeking behaviour. In India, most studies have either addressed compliance rate of attendees of specially arranged screening programmes or have been done in hospital settings. Hence, this study was aimed to determine knowledge levels of women on cancer cervix, screening practices and their determinants among women aged between 15-50 yr in a rural community in Kerala in the absence of a screening programme.
Material & Methods
The study was conducted by the Deparment of Community Medicine, Amrita Institute of Medical Sciences, Cochin, Kerala. The study was conducted in a rural area of Kerala State, India. The Vypin Block with a population of 2, 22008 (census 2001) was chosen as the study area. The study was carried out between January 2009 to August 2009. For the purpose of sample size calculation and feasibility, the study was pilot tested on 50 women from the area. At 95 per cent confidence level and relative precision of 20 per cent the required sample size was calculated on the basis of awareness, practice of previous studies and the higher sample size of 590 was taken. At a non-response rate of 20 per cent, the calculated sample size was 737. Selection of household was done by following multistage sampling (two-stage). In the first stage, four Panchayats were randomly chosen from the seven Panchayats in Vypin Block. In the second stage, the households were selected by systematic random sampling, taking every second house in the tenth ward of selected Panchayat starting from north end of each Panchayat till at least 200 women were interviewed. In a household if there were more than one woman in the 15-50 yr age group, all of them were interviewed. Thus a total of 809 women were interviewed after explaining the purpose of the study, obtaining verbal consent and assuring confidentiality. A pre-tested, semi-structured questionnaire was used. Two days forenoon session were devoted to training the field personnel on interview technique and the questionnaire.
Knowledge regarding the common cancers affecting women, the screening methods of cervical cancer, screening practices were part of the interview schedule. Factors affecting non-screening were also assessed among those who were desirous of doing the screening test but had not done it till date. For assessing socio-economic status Modified Prasad's Scale based on Consumer price index for 2009 was used12.
Statistical analysis was performed using SPSS version 1113. A univariate analysis was done to identify predictors of screening and then multivariate logistic regression was done for the significant values. P<0.05 was considered significant. Aspects of knowledge such as cervical cancer being a cancer affecting women, symptoms of cervical cancer, risk factors, whether it can be detected early by screening, and tests available for screening were determined. Each of these categories were scored with a maximum of 0.5-1 awarded for each of the questions with a total of 4. A score of less than 2 was considered to be poor knowledge and more than or equal to 2 was considered to be good knowledge.
Results
The mean age of women in the study population was 34.5 ± 9.23 yr with the age range from 15-50 yr. More than half of the study population (443, 54.8%) were Hindus and a majority (521, 64.4%) had completed high/higher secondary school education. A majority of the women (740, 91.4%) were non-working and most of them (651, 80.4%) were homemakers. Married women comprised 88.4 per cent (715) and over half 60.5 per cent (490) lived in a nuclear family. Most of the women (386, 59.6%) belonged to poor socio-economic status. Different sources of information on cervical cancer were also identified. The most common and important source of information mentioned was media (452, 55.8%) followed by health workers and doctors (273, 33.74%). Family and friends was cited by 119 (14.7%).
Almost three fourths of the study population (584, 72.1%) was aware of cervical cancer as a type of cancer affecting women. Three fourth of the population (600, 74.2%) knew that it could be detected early by a screening test but only 47 (5.8%) could name the Pap test as the screening method of cervical cancer. Though 56 (6.9%) had ever done Pap test, only 5.8 per cent could recall the name of the screening test. Only about half (395, 48.8%) of the women were aware of symptoms of cervical cancer. The cardinal symptoms of cervical cancer mentioned included bleeding (289, 35.7%) and pain (70, 8.6%). Other incorrect responses included lump, stomachache, and pain in legs (9.1%). Majority of respondents (722, 89.2%) did not know any risk factor for cervical cancer and 5.3 per cent gave incorrect responses. Lack of hygiene and multiple sexual contacts were the only two risk factors cited by 3.9 per cent (32) and 1.6 per cent (13) respondents. respectively. On being asked about timing of Pap test, majority of women (726, 89.7%) did not know when it should be done, 23 (2.8%) said it should be done only when there is any problem and 60 (7.4%) said it should be done after age of 30 yr. On periodicity, 12 (1.5%) said it should be done monthly, 20 (2.5%) said 1-2 yearly and 23 (28%) every 2 to 3 years. Scoring of knowledge levels showed that 92.8 per cent had poor knowledge on the various aspects like symptoms, risk factors, screening test, etc.
Of the 809 women studied (56, 6.9%) had undergone screening at some point and about two thirds were not willing to be screened in future also (Fig.). About 30 per cent (245) women were desirous of undergoing screening test, but had not done it due to various reasons.
Fig.
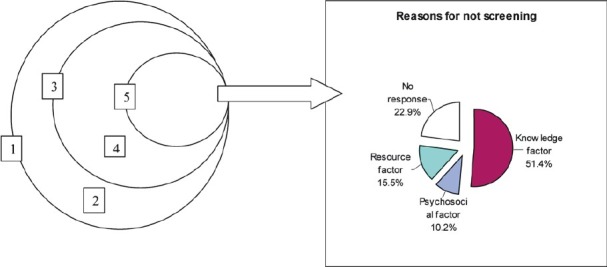
Distribution of sample population as per their screening status, willingness to undergo screening in future and reasons for not screening. 1. Sample population = 809. 2. Ever screened = 56/809 =6.9%. 3. Never screened = 753/809=93.1%. 4. Not willing to be screened in future and non responders =484/753 =64.3% and 24/753= 3.1%; total =67.1%. 5. Willing to get screened= 245/ 753 = 32.6%.
The factors for not screening, reported by these women (n=245) were grouped into knowledge factors 126 (51.4%), resource factors 38 (15.5%) and psychological factors 25 (10.2%). The knowledge factors included no symptoms (91, 37.1%), not being aware of the Pap test (28, 11.4%), not necessary (4, 3.1%). Resource factors included lack of time (18, 7.3%), financial reason (14, 5.7%) and lack of facility in the area (3, 1.2%). Two women said they ‘did not get a chance to do it′. Different psychosocial factors included lack of interest (3, 1.2%), fear of procedure (3, 1.2%), and embarrassment (1, 0.4%). However ,18 (7.3%) did not specify any definite reason.
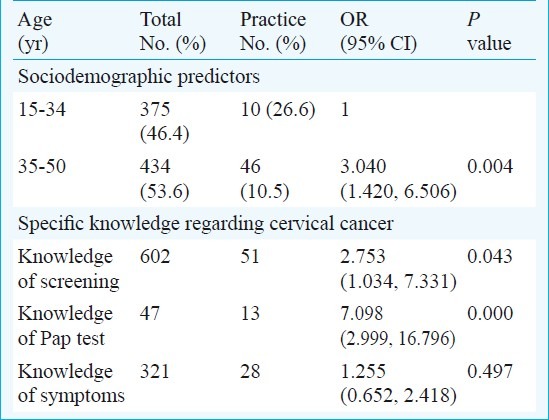
Predictors for doing Pap test were identified (Table I) and a binary logistic regression analysis showed that women, more than 35 yr of age, those who had knowledge of screening for cervical cancer, and Pap test were 3.04 times (CI 1.42-6.506), 2.75 times (CI 1.03-7.33) and 7.098 times (CI 2.999-16.796) respectively, were more likely to undergo screening as compared to their counterparts.
Table I.
Independent predictors of cervical screening practices in the study population
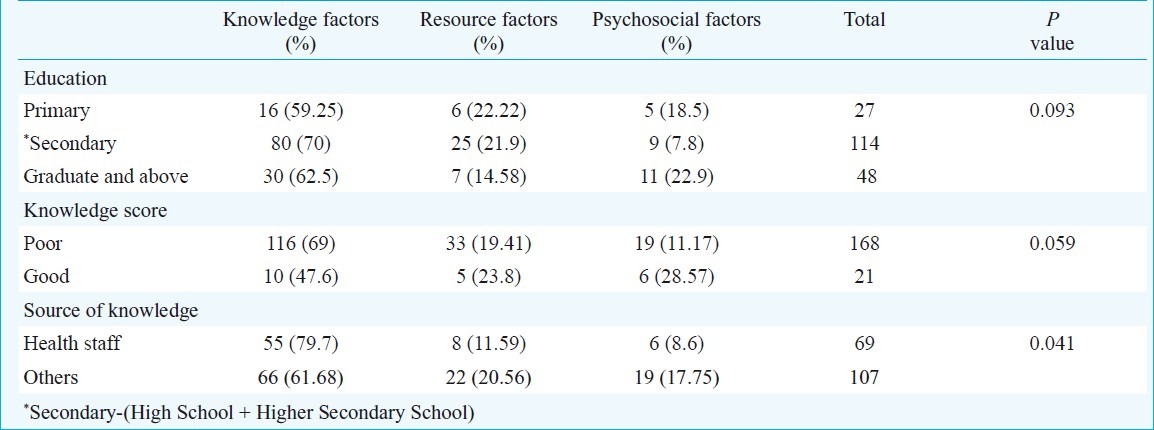
The determinants of factors affecting non screening were also studied (Table II), and 69 per cent of women with poor knowledge scores cited knowledge factors as compared to only 47.6 per cent with good knowledge score. A multinomial logistic regression confirmed that those with poor knowledge were significantly more likely to cite knowledge factors than psychosocial factors (OR=3.36, CI 1.007-11.218). Similarly those with at least a primary education were less likely to report knowledge factors compared to psychosocial factors (OR=0.347,CI 0.122, 0.198 P<0.05). Those who reported Drs/health staff as the source of information regarding cervical cancer were significantly more likely to report factors related to knowledge (OR=1.60E + 08, CI 1.5E + 07-1.7E +09, P<0.001). The other factors were not found to be significant. The good knowledge scores in the screened was 16 (28.6%), and in unscreened women was 42 (5.6%), those who were willing to be screened in future was 19 (7.8%) demonstrating the importance of specific knowledge.
Table II.
Independent determinants of reasons for not screening (n=189)
Discussion
Only half of the study population was aware of symptoms and the majority (89.2%) were unaware of the risk factors for cervical cancer. Media has a major share (55.8%) in disseminating information to the women. Here, the high literacy levels which is about 90 per cent among women had an enabling role. Though three fourths of the population knew that cervical cancer could be detected early by a screening test, only 6.9 per cent had ever done the Pap test. This was slightly higher than the rest of India9,10 probably due to higher literacy levels and greater awareness. In two studies conducted on screening for cervical cancer in Dindigul, Tamil Nadu, and Osmanabad, Maharashtra, two of 80269 women and eight of the 131746 women aged 30-59 yr had undergone previous cervical cancer screening, respectively14,15. The screening coverage in the age group of 18-69 yr among Indian women was 2.6 per cent (4.9% among urban and 2.3% among rural)9, and was found to vary between 4-6 per cent in poor and rich women in India10.
Several factors may affect a woman's ability and desire to participate in cervical cancer prevention programs16. In this study the reasons for not getting the screening test done in spite of a desire to do so were mainly no awareness, no disease or symptoms, do not know where to go, no one is doing it and never thought of it. Thus, knowledge factors accounted for 50 per cent of the self reported factors. Lack of knowledge about the disease, absence of the concept of preventive behaviour appear to be important factors. Therefore, in the context of implementing a successful programme it is essential to identify the reasons that prevent a woman from using the services16.
Similar findings were reported in the Kolkota study where most of the women did not appreciate the importance of preventive health check up in the absence of symptoms17. Among African American and Hispanic women, absence of symptoms and perception of vulnerability determined Pap smear testing18. Not knowing where to go was also found to be a significant barrier among Hispanic women19. The most frequently reported obstacles to screening in Kolkata included not knowing where to obtain a Pap test; the test is painful, anxiety about results and cost. Some other determinants included being scared of the tests, feeling shy, etc17. In our study these factors were categorized as psychosocial factors. These included lack of interest, pain, fear of pain and embarrassment. Fear of discomfort and embarrassment were most important barriers for women in Singapore having an organized screening programme20. Some respondents could not specify a reason and some did not answer for the desire to go for Pap test. Screening is considered a preventive service which is not a priority for asymptomatic persons who are struggling to cope with more acute day to day problems21. The International Agency for Research on Cancer (IARC) supports these findings in that women fail to be screened due to insufficient resources, lack of knowledge, inability to access the health care delivery system, individual psychosocial and cultural contexts, fear or limited family support and community participation22.
Our study showed that women more than 35 yr of age, having knowledge of screening for cervical cancer and Pap test were significantly more likely to undergo the Pap test. The reason could be that these women approach a health facility for different types of reproductive morbidity when an opportunistic screening is also done. Another study also reported that contact with the health care system is associated with an increased use of screening services23. Many other studies have identified knowledge, increasing age and marital status as significant positive predictors of ever performed Pap test24–26,17. Similar findings regarding marital status was found in a randomized clinical trial (RCT) conducted in Barshi, Maharashtra, though attendance for screening was higher among young women26. Evidence based studies have found that the optimal age for cervical cancer screening to achieve greatest public health impact is between 30-39 yr. A single visit or two visits can reduce the lifetime risk of cervical cancer by 25 and 35 per cent, respectively28. Specific health education exercises can motivate women to go for Pap test. These exercises should involve community leaders and also the males in the family. It should not just provide information but should involve a process of reconstructing concepts in the context of women's lives29. In our study, educational status of the woman was not found to be a factor affecting whether a woman had done Pap test or not. This might be because the differential in educational levels was quite low and there were no illiterates. Moreover, research on relation between socio-economic factors and the use of health services has shown that education influences screening behaviour through its effects on income and through its association with individual knowledge on cancer screening30. Higher levels of education did not seem to have an influence on reducing knowledge factors as compared to psychosocial factors.
The primary health care facilities where cervical screening should be available are limited, under- resourced and over-burdened in most developing countries21. There is evidence that visual screening can lead to a significant reduction in disease and can be used readily in all health care setting31. Cytology can be provided in rural areas for approximately  392 per women and can achieve higher detection rates than visual inspection with acetic acid (VIA), though VIA is 34 per cent cheaper32.
392 per women and can achieve higher detection rates than visual inspection with acetic acid (VIA), though VIA is 34 per cent cheaper32.
Though, cervical cancer is the second leading site of cancer among women in Thiruvananthapuram registry33; women in the community are ignorant about the risks, risk factors, symptoms of this particular cancer. Specific knowledge on cervical cancer is thus a critical element in determining whether a woman will undergo Pap test or not. The limitation of this study was that it was a quantitative study and hence psycho-socio-cultural reasons for not undertaking the screening test could not be explored in depth. Qualititative research may add to understanding the factors affecting those who have not gone for screening the test, and to help unravel the silence of the non-responders.
Acknowledgment
The authors acknowledge the support of Shri K. Kumarankutty, Ms. R. Radhikadas, Ms. K. Devaki, Shri T.S. Anish, Ms. Binobha in the field and Shri Reneej T., Ms Rajasree for assistance in data entry. The authors thank Dr K.R. Sundaram, Professor & Head, Department of Biostatistics, Amrita Institute of Medical Sciences, Kochi.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of Cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Government of India - World Health Organization Collaboration Programme 2004-2005. Guidelines for cervical cancer screening programme. 2006 [Google Scholar]
- 3.Breakway: The global burden of cancer - Challenges and opportunities. A report from the Economist Intelligence Unit. 2009 [Google Scholar]
- 4.Three year report of population based cancer registries 2006-2008. New Delhi: ICMR; 2010. National Cancer Registry Programme. [Google Scholar]
- 5.Goldie SJ, Gaffikin L, Goldhaber-Fiebert JD, Gordillo-Tobar A, Levin C, Mahe C, et al. Alliance for Cervical Cancer Prevention Cost Working Group. Cost-effectiveness of cervical cancer screening in five developing countries. N Engl J Med. 2005;353:2158–68. doi: 10.1056/NEJMsa044278. [DOI] [PubMed] [Google Scholar]
- 6.Harry TK, Felicia MS, Ngugen S. A needs assessment of barriers to cervical cancer screening in Vietnamese American Health Care Providers. Californian J Health Promotion. 2006;4:146–56. [Google Scholar]
- 7.Nor HO, Matejka R. Challenges to cervical cancer screening in a developing country: The case of Malaysia. Asia Pacific J Cancer Prev. 2009;10:747–52. [PubMed] [Google Scholar]
- 8.Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States.Results from the 2000 National Health Interview Survey. Cancer. 2003;97:1528–40. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- 9.World Health Survey. Geneva: WHO; 2003. WHO. [Google Scholar]
- 10.Gakidou E, Nordhagen S, Obermeyer Z. Coverage of cervical cancer screening in 57 countries: low average levels and large inequalities. PloS Med. 2008;5:e132. doi: 10.1371/journal.pmed.0050132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kasturi J, Bhagwan MN, Rajendra AB, Nandkumar SP, Ranjit VT, Feroz YK. Rural Cancer Registry at Barshi, Maharashtra and its impact on cancer control. Natl Med India. 2010;23:274–7. [PubMed] [Google Scholar]
- 12.Agarwal AK. Social classification: The need to update in present scenario. Indian J Commun Med. 2008;33:50–1. doi: 10.4103/0970-0218.39245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Basant KP. SP SS in practice. 2nd ed. London: Arnold; 2002. [Google Scholar]
- 14.Sankaranarayanan R, Nene BM, Shastri SS, Jayant K, Muwonge R, Budukh AM, et al. HPV screening for cervical cancer screening in rural India. N Engl J Med. 2009;360:1385–94. doi: 10.1056/NEJMoa0808516. [DOI] [PubMed] [Google Scholar]
- 15.Sankaranarayanan R, Esmy PO, Rajkumar R, Muwonge R, Swaminathan R, Santhakumari S, et al. Effect of visual screening on cervical cancer incidence and mortality in Tamil Nadu, India: a cluster randomized trial. Lancet. 2007;370:398–406. doi: 10.1016/S0140-6736(07)61195-7. [DOI] [PubMed] [Google Scholar]
- 16.Allison B, Amie B, Patricia C, Jennifer W, Janet B, Ilana D. Factors affecting preventive services in low resources settings. Salud Publica de Mexico. 2003;45:S408–15. doi: 10.1590/s0036-36342003000900015. [DOI] [PubMed] [Google Scholar]
- 17.Roy B, Tricia ST. Cervical cancer screening in Kokata, India: Beliefs and predictors of cervical cancer screening among women attending a women's Health Clinic in Kolkata. J Cancer Educ. 2008;23:253–9. doi: 10.1080/08858190802189105. [DOI] [PubMed] [Google Scholar]
- 18.Kelly A, Kimberlee G. Factors influencing cancer screening practices of underserved women. J Am Acad Nurse Pract. 2007;19:591–601. doi: 10.1111/j.1745-7599.2007.00268.x. [DOI] [PubMed] [Google Scholar]
- 19.Byrd TL, Petterson SK, Chavez R, Heckert A. Cervical cancer screening beliefs among young Hispanic women. Prev Med. 2004;38:192–7. doi: 10.1016/j.ypmed.2003.09.017. [DOI] [PubMed] [Google Scholar]
- 20.Seow A, Wong ML, Smith WCS, Lee HP. Beliefs and attitudes as determinants of cervical cancer screening: A community based study in Singapore. Prev Med. 1995;24:134–41. doi: 10.1006/pmed.1995.1026. [DOI] [PubMed] [Google Scholar]
- 21.Tsu VD, Pollach AE. Preventing cervical cancer in low resource settings: How far have we come and what does the future hold? Int J Gynaecol Obstet. 2005;89:S55–9. doi: 10.1016/j.ijgo.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 22.Handbook of cancer prevention. Cervix cancer screening. Vol. 10. Lyon, France: IARC; 2005. International Agency for Research on Cancer (IARC) [Google Scholar]
- 23.Lantz PM, Weigner ME, House JS. Education & immuno differentials in breast & cervical cancer screening: Policy implication for rural women. Med Care. 1997;35:219–36. doi: 10.1097/00005650-199703000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Coffey P, Arrossi S, Bradley J, Dzuba I, White S ACCP Community Involvement Affinity Group. Seattle WA: Alliance for Cervical Cancer Prevention; 2004. [January 21, 2011]. Improving screening coverage rates of cervical cancer prevention programs: a focus on communities (Issues in Depth No: 4) Available from: http://www.path.org/files/RH_accp_improve_screening.pdf . [Google Scholar]
- 25.Juon HS, Seung-Lee C, Klassen AC. Predictors of regular Pap smears among Korean- American women. Prev Med. 2003;37:585–92. doi: 10.1016/j.ypmed.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 26.Risendal B, Dezapien J, Fowler B, Papenfuss M, Giuliano A. Pap smear screening among urban Southwestern American Indian women. Prev Med. 1999;29:510–8. doi: 10.1006/pmed.1999.0565. [DOI] [PubMed] [Google Scholar]
- 27.Bhagwan N, Kasturi J, Silvina A, Surendra S, Atul B, Sanjay H, et al. Determinants of women's participation in cervical cancer screening trial, Maharashtra, India. Bull World Health Organ. 2007;85:264–72. doi: 10.2471/BLT.06.031195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jacqueline S, Scott W, Amy K, John S, Silvana L, Rengaswamy S, et al. Evidence based, alternative cervical cancer screening approaches in low resource settings. Int Perspect Sexual Reprod Health. 2009;35:1–14. doi: 10.1363/ifpp.35.147.09. [DOI] [PubMed] [Google Scholar]
- 29.Bradley J, Risi L, Denny L. Widening the cervical cancer screening net in a South African township: who are the underserved? Health Care Women Int. 2004;25:227–41. doi: 10.1080/07399330490272732. [DOI] [PubMed] [Google Scholar]
- 30.Sankaranarayanan R, Rajkumar R, Arossi S, Theresa R, Esmy PO, Mahe C, et al. Determinants of participation of women in a cervical cancer visual screening trial in rural south India. Cancer Detect Prev. 2003;27:457–65. doi: 10.1016/j.cdp.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 31.Sankaranarayanan R. Screening for cervical and oral cancers in India is feasible & effective. Nat Med India. 2005;18:281–4. [PubMed] [Google Scholar]
- 32.Legood R, Alastair MG, Cedirie M, Jane W, Kasturi J, Bhagwan MN, et al. Screening for cervical cancer in India: How much will it cost? A trial based analysis of the cost per case detected. Int J Cancer. 2005;117:981–7. doi: 10.1002/ijc.21220. [DOI] [PubMed] [Google Scholar]
- 33.Nandakumar A, Ramnath T, Meesha C. The magnitude of cancer cervix in India. Indian J Med Res. 2009;130:219–21. [PubMed] [Google Scholar]


