Abstract
Shortly after the influenza A (H1N1) 2009 pandemic began, the U.S. government provided guidance to state and local authorities to assist decision-making for the use of nonpharmaceutical strategies to minimize influenza spread. This guidance included recommendations for flexible decision-making based on outbreak severity, and it allowed for uncertainty and course correction as the pandemic progressed. These recommendations build on a foundation of local, collaborative planning and posit a series of questions regarding epidemiology, the impact on the health-care system, and locally determined feasibility and acceptability of nonpharmaceutical strategies. This article describes -recommendations and key questions for decision makers.
In preparation for a severe influenza pandemic, the Centers for Disease Control and Prevention (CDC) issued Interim Pre-Pandemic Planning Guidance: Community Strategy for Pandemic Influenza Mitigation in the United States—Early, Targeted, Layered Use of Nonpharmaceutical Interventions in February 2007.1 This document described tiers of nonpharmaceutical measures (e.g., dismissing students from school and using facemasks) that could be used for different pandemic severity levels, but primarily focused on measures for a 1918-like severe influenza pandemic. As influenza A (H1N1)pdm09 (hereafter, pH1N1) outbreaks began in the United States in April 2009, CDC released new guidance on nonpharmaceutical measures to state and local public health agencies and communities, and updated this guidance every three to four days based on rapidly changing epidemiologic and laboratory information as well as feedback from public health and education sector partners.
By May 2009, emerging data suggested that the pH1N1 outbreak was not as severe as the 1918 pandemic. Providing advisory measures that were well matched to the severity of the pandemic in the first few weeks proved challenging for several reasons: decisions were needed before much was known about the severity of the pandemic, pre-pandemic planning did not focus sufficiently on middle-range severity pandemics or how to use nonpharmaceutical strategies in a limited fashion, and communities varied widely in their experiences with pH1N1 and, accordingly, in their willingness to implement more disruptive measures. To address these concerns, during the summer of 2009, CDC held discussions with influenza experts, the U.S. Department of Education, and state and local public health and education officials to understand their concerns and inform further guidance.
METHODS
CDC and the U.S. Department of Education hosted a meeting with 19 education sector national nongovernmental organizations, the U.S. Department of Agriculture, and the U.S. Department of Defense Education Agency in Washington, D.C., on June 29, 2009, to address recommendations on the dismissal of students from schools. On July 1 and 2, 2009, CDC and the Council of State and Territorial Epidemiologists (CSTE) held a joint meeting in Atlanta, Georgia. This meeting was followed by weekly conference calls with CSTE and the Association of State and Territorial Health Officials (ASTHO) membership. These calls were used to present draft guidance and receive CSTE and ASTHO input. Additional input was sought from and provided by federal agencies including the Environmental Protection Agency, U.S. Department of Homeland Security, U.S. Department of Labor, Administration for Children and Families Office of Head Start, U.S. Small Business Administration, and U.S. Department of Commerce. Based on this feedback, CDC released new guidance documents in August 2009 on selecting and implementing nonpharmaceutical measures for schools, colleges/universities, child care programs, and employers.2–5 These new guidance materials established a framework for flexible decision-making based on outbreak severity, allowing for the uncertainty inherent in this type of decision-making process. The centerpiece of the guidance documents was a set of key questions to determine which nonpharmaceutical strategies to use and when.
Beginning in fall 2009, CDC provided technical assistance to the Harvard School of Public Health as its staff conducted repeated polls assessing public perceptions and acceptance of community mitigation guidance.6,7 In addition, during fall 2009 and winter 2010, CDC conducted opinion leader calls and focus groups with administrators, staff, and families from K–12 schools, institutions of higher education, and early childhood programs, as well as with employers representing both large and small businesses.
CDC used the findings from these formative evaluation activities to finalize the framework presented in this article. The framework is intended for use by state and local public health officials in collaboration with appropriate stakeholders such as education officials or large local employers.
A FRAMEWORK FOR SELECTING NONPHARMACEUTICAL STRATEGIES TO USE DURING AN INFLUENZA PANDEMIC
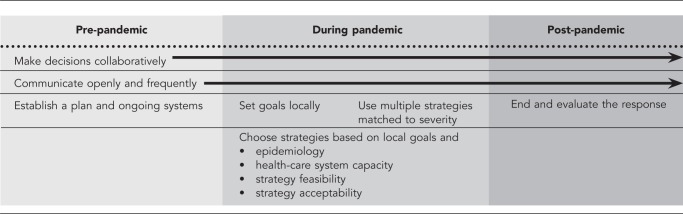
Nonpharmaceutical measures are critical components of the earliest response to a developing pandemic, prior to distribution of an effective vaccine. While they remain important after vaccine introduction to continue to assist in slowing the spread of influenza, their impact is likely to be greater when used in combination with pharmaceutical measures, such as vaccines or antiviral medications. The severity of a pandemic is unlikely to be known early in a response, and local priorities and conditions are likely to vary. To be effective in responding to a pandemic, planners must engage a variety of partners, collaborate effectively to develop a plan, make explicit the goals of their response, select strategies in a thoughtful process based on those goals and data, and evaluate the response for lessons learned (Figure). Although some aspects of this work must occur before, during, or after a pandemic, much of any response involves concurrent data collection, discussion, and iterative reassessment.
Figure.
A framework for selecting nonpharmaceutical strategies to use during an influenza pandemic
NOTE: Planners should engage a variety of partners, collaborate effectively to develop a plan, explicitly define goals, select strategies based on goals and data, and evaluate their response. Although some components occur before, during, or after a pandemic, much of the strategy involves concurrent data collection, discussion, and iterative reassessment.
Make decisions collaboratively
The key to successful implementation of a chosen course of action is that stakeholders understand and support the recommendations made. The best way to achieve stakeholder support is to include, in a collaborative decision-making process established in advance of a pandemic, representatives of groups who will implement or be affected by the course of action. State and local public health officials should collaborate with staff from other government agencies, such as education, transportation, and emergency response, to decide which strategies to implement and when, collect and share data, and disseminate emerging guidance. Neighboring states or other jurisdictions should communicate regularly to ensure that differences in response plans across jurisdictions are well understood and communicated to the public and other stakeholders. Other likely stakeholders include representatives of local businesses, health-care providers, community- and faith-based organizations, and families and representatives of targeted settings (e.g., schools, universities, child care programs, and nursing homes.) These groups bring multiple data sources, perspectives, and values; including these groups makes for a richer decision-making environment. Collaborative decision-making, based on shared values, allows for more consistent action by all stakeholders.8 The need for rapid decisions in emergencies can limit opportunities for collaborative decision-making, especially if relationships and processes are not already well-established.
Elected and appointed officials, which are a specific type of stakeholder, often feel tremendous pressure to act immediately in a crisis. This inclination runs counter to the scientist's natural preference for more data. Officials prefer to be given a single recommendation with clear outcomes; scientists may prefer to provide pros and cons of various choices. Given these competing demands, scientific decision makers should avoid promising specific outcomes. Instead, they should explain how and why decisions will be made and how further data will be used to close the gap between the recommended action and the expressed goal. Most importantly, state and local public health officials should establish trust with elected and appointed officials before a pandemic. A trusting relationship can help ensure that decisions made during a pandemic are based on the best available scientific information.
Communicate openly and frequently
Frequent, open communication with the public, other government agencies, state and local partners, and community stakeholders is essential to effective implementation. The consequences of over- or under-reacting should not be underestimated. If CDC, state, or local agencies overreact by recommending or instituting very disruptive measures, communities and families can incur great costs with only minimal benefits, and the agencies' future recommendations could be perceived as less credible. If these agencies under-react, more people might become ill, including severely ill, or die. Ultimately, the success of nonpharmaceutical strategies depends on individual and collective actions of community members. For example, employers need to understand that if their sick-leave policies align with public health policies, ill people may be more likely to stay home during a pandemic, benefiting both the business and the community. The public must understand the rationale for recommendations and be willing to accept disruption based on perceived risk.
Relationships with local media should be established before a pandemic. During a pandemic, state and local public health officials should work with media and trusted sources in communities to (1) describe the nonpharmaceutical strategies being implemented and dispel rumors, (2) clarify goals and rationale, (3) inform the public when and why response strategies change, (4) disseminate clear information about what the public should and should not do, and (5) communicate uncertainty as well as the likelihood for changing course as new information emerges.
Establish a plan and ongoing systems before a pandemic
Decisions about nonpharmaceutical strategies to use during a pandemic should be based on an existing plan and within the context of a standard emergency response framework, such as the Incident Command System.9 Given inevitable uncertainty, it is critical that plans avoid a locked-in fixed response and be flexible enough to respond to uncertainty and, ultimately, to evolving pandemic scenarios of different severities. Planning assumptions in underlying scenarios must be explicit so that they can be evaluated against the reality of an emerging event. Plans should frequently be reviewed, tested, and revised (as needed) in collaboration with partners and stakeholders and as part of ongoing emergency preparedness activities. Plans should address legal authorities and policies, including which agencies or officials are authorized to implement measures such as closing schools, and which decision makers need to be involved in planning and implementation. Plans also should describe the methods that will be used to evaluate whether selected measures meet the goals set by the state or community.
A strong, ongoing influenza surveillance system, capable of providing timely data for a range of age groups, is critical for decision-making during a pandemic but must be established in advance. Information on seasonal influenza-related illness, doctor's office visits, hospitalizations, emergency department visits, intensive care unit (ICU) admissions, workplace and school absenteeism, and deaths can greatly help the state or community determine the impact of the pandemic over and above seasonal influenza.
Set goals locally
CDC will monitor an evolving pandemic, look for changes in illness severity and the virus itself, and share what is learned with state and local agencies and the public. However, communities are likely to be affected differently and at different times. Communities also may set different prevention and mitigation goals. Feasibility and acceptability of intervention strategies will vary across communities as well. Therefore, local decisions should be based on local circumstances and not national data alone.
Decision makers should explicitly set, prioritize, and communicate the goals they hope to achieve by implementing nonpharmaceutical strategies whether that be reducing overall transmission of the influenza virus or reducing transmission in certain settings. For example, depending on illness severity and the age groups most affected, a community might place a higher priority on implementing strategies in schools or nursing homes. Decision makers likely will need to decide which population groups most need protection. They could select strategies likely to reduce overall transmission or place a higher priority on those at increased risk for serious complications from influenza (e.g., people with chronic medical conditions). Decision makers must balance the risk of influenza transmission, impact of disease, and community functioning. They should consider how much the pandemic is disrupting community functioning and the health outcomes of those who become ill and examine whether (further) disruption is necessary and tolerable when selecting measures.
Use multiple strategies matched to outbreak severity
Decision makers should understand the types of nonpharmaceutical strategies available to them and consult the best available implementation, policy analysis, and evaluation science. Using multiple strategies early and in a coordinated fashion may be more effective in reducing transmission than using a single strategy.10,11 Specific strategies are designed to affect influenza transmission at different times in the transmission process and in a pandemic. For example, social distancing measures (e.g., school dismissals) are intended for preemptive use and must be applied early and comprehensively throughout a community to be most effective.12 Once disease is in a community, aggressive monitoring of symptoms and swift isolation at the beginning of symptoms, as well as antiviral prophylaxis for household members might delay community transmission.13–15 Hand hygiene and cough etiquette may reduce the likelihood of transmission from an infected person to someone else. The availability of pharmaceutical strategies such as vaccines and antiviral medications will influence which nonpharmaceutical strategies to implement as well. Because each strategy works in a different way, the effectiveness of the overall response would be expected to be greater when multiple strategies are simultaneously used. Appropriate matching of the intensity and type of intervention to the severity of a pandemic is important to maximize the public health benefit that may result from using these measures while minimizing untoward secondary effects. Decision makers should answer the following questions to help set goals locally and make collaborative decisions about the best strategies to use.
Examine the epidemiology.
Federal, state, and local data can be used in combination to generate an epidemiologic picture of a pandemic and its likely local effects. It is unlikely that most states or cities will be able to answer all of the questions listed subsequently. Additionally, data on outbreaks that begin outside the U.S. might be contradictory, difficult to interpret, or of questionable validity for the U.S. context. The following are questions for state and local health officials to consider:
What is the extent of the spread of influenza-related illness? Regional? National? Global?
Who is most affected? Consider age groups, regions, and vulnerable populations.
What is the course of the disease? Do people become severely ill soon after symptoms arise?
What is the number/rate of outpatient visits for influenza-like illness? What proportion of those visits is due to confirmed influenza?
What percentage of people with influenza-like illness are hospitalized?
What percentage of hospitalized patients need ICU, advanced care, or respirators?
How many deaths are occurring and among which groups?
How are populations at increased risk for serious complications from influenza distributed within the jurisdiction? What is the likely effect on these populations?
Health officials are not the only potential sources of useful information to assess the extent of the pandemic. Education agencies, child care licensing offices, universities, pharmacies, businesses, and chambers of commerce also are potential sources of valuable data. For example, education agencies might be able to share their student and staff absenteeism rates, school health office visits, and numbers of students and staff with influenza-like symptoms leaving during the school day. Large local employers may be able to report trends in employee absenteeism.
Consider health care.
A pandemic can overburden the health-care system. This occurs when there are not enough health-care providers, hospital beds, emergency room capacity, ICU spaces, ventilators, or medicines available to provide adequate care for influenza- and non-influenza-related medical conditions. During a severe pandemic, ill people, as well as people who are not ill but worried, may be more likely to seek medical care. When health-care systems cannot provide adequate care, mortality and costs are likely to increase. The impact of influenza on the health-care system will influence decisions about the types, numbers, and timing of nonpharmaceutical strategies. Questions to consider include the following:
Are health-care providers and hospitals able to accommodate the increase in influenza-related visits they are receiving or may receive?
Are there enough resources such as staffed hospital beds, medications, and ventilators?
Is there enough capacity in emergency departments and ICUs to accommodate an increased demand?
Is absenteeism increasing among health-care workers due to influenza-like illness in themselves or their family members?
Is there enough antiviral medicine to treat people at increased risk for influenza-related complications or who have more severe illness?
Are effective vaccines available? If not, when will they be available in the state or locality and how will they be distributed?
Determine feasibility.
Decision makers need to consider implementation-related issues that can limit their available strategy options. Balancing information on severity, spread, affected populations, and local goals with a critical examination of the feasibility of each strategy option requires asking questions such as the following:
Do strategies need to be implemented in a particular order? If so, what should be done first?
Are changes to legal authority or policy needed? If so, how feasible are these changes?
How long will specific strategies take to get started? For how long can they be sustained?
What resources (e.g., funds, personnel, equipment, and space) are needed and available to implement the strategies?
What obstacles could decrease the effectiveness of the strategies?
What can be done to improve adherence to nonpharmaceutical strategy recommendations?
Determine acceptability.
Community support is critical to strategy implementation. Although the most disruptive nonpharmaceutical strategies (e.g., prolonged school dismissals or child care facility closures) are unlikely to be used in less severe pandemics, several strategies can have negative secondary effects, disrupting families and communities.
Strategies are more likely to be implemented fully and effectively if the public is prepared, if they perceive the same level of severity of influenza-related illness as decision makers, or if they believe that the strategy will be effective. Risk perceptions can vary across time and place and be influenced by media attention.16 Polling might be an effective tool for gathering information about risk perceptions and strategy acceptability in a time frame that is useful for decision-making.6,7 The following questions can guide analyses of strategy acceptability and methods for increasing acceptability:
What are public concerns about the influenza pandemic? Do people believe they are likely to be infected? Do they believe many people could become seriously ill or die?
Do social norms and public opinion support or reject specific strategies under consideration?
What communication efforts can be used to explain the need for the strategies to the public? What can be used to minimize or dispel rumors and misinformation and spread correct information? Who should be the spokesperson to communicate with the public?
How should guidance be adapted for use with multiple audiences?
How can expected benefits be measured and shared with the public?
What negative effects (e.g., detrimental effects on child nutrition, job security, financial support, or educational progress) could occur? How could negative effects be reduced?
What can be done to increase community buy-in and support?
What can be done to increase the public's self-efficacy for implementing protective actions?
End and evaluate the response
Careful monitoring of the evolution of a pandemic allows for detection of changes in severity or waning of the outbreak. Knowing when and how decisions will be made about stopping strategies is as important as knowing when to start them. Planning for ending and evaluating a response should happen early in the response process, engaging the same stakeholders in a collaborative decision-making process. Discussions should encompass criteria for removing nonpharmaceutical strategies and returning to normal operations, and should take into account how difficult it will be to stop each implemented measure. Plans should address whether some strategies should be continued for a longer period of time.
Evaluation activities, for example, after-action reviews, should address both processes (i.e., how well strategies were implemented) and outcomes (i.e., how effective they were in achieving the goals). Evaluation should not be an academic exercise: care should be taken to determine how lessons learned will be applied to future planning.
CONCLUSIONS
It is impossible to predict when the next influenza pandemic will occur or what its severity will be. Decision makers must be flexible and willing to change course based on information about the virus, epidemiology, and the acceptability of responses as new information becomes available. Decision-making in a pandemic is an ongoing process—not a one-time activity. Current plans should be reviewed and revised based on lessons learned during the pH1N1 pandemic.6,7,17–22 However, as that experience illustrated, we can never conceive of all possible scenarios ahead of time, will always want additional information, and need a flexible framework for making and communicating decisions. Despite advances in vaccine production and distribution, it is unlikely that a well-matched vaccine will be available at the onset of the next pandemic. Nonpharmaceutical strategies will be needed to help slow the spread of influenza in conjunction with other measures; the judicious use of these measures may yield the best results. Using a standard framework, such as the one described in this article, can provide a structure for making decisions.
Acknowledgments
The authors acknowledge Amanda McWhorter, Stephanie Zaza, Francisco Alvarado-Ramy, Francisco Averhoff, Clive Brown, and Carolyn Bridges for their contributions to the 2009 H1N1 nonpharmaceutical strategies guidance and the decision-making framework.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) Atlanta: CDC; 2007. [cited 2012 Mar 8]. Interim pre-pandemic planning guidance: community strategy for pandemic influenza mitigation in the United States—early, targeted, layered use of nonpharmaceutical interventions. Also available from: URL: http://www.flu.gov/planning-preparedness/community/community_mitigation.pdf. [Google Scholar]
- 2.CDC (US) Atlanta: CDC; 2009. [cited 2012 Apr 11]. CDC guidance for state and local public health officials and school administrators for school (K-12) responses to influenza during the 2009-2010 school year. Also available from: URL: http://www.cdc.gov/h1n1flu/schools/schoolguidance.htm. [Google Scholar]
- 3.CDC (US) Atlanta: CDC; 2009. [cited 2012 Apr 11]. CDC guidance for responses to influenza for institutions of higher education during the 2009-2010 academic year. Also available from: URL: http://www.cdc.gov/h1n1flu/institutions/guidance. [Google Scholar]
- 4.CDC (US) Atlanta: CDC; 2009. [cited 2012 Apr 11]. CDC guidance on helping child care and early childhood programs respond to influenza during the 2009-2010 influenza season. Also available from: URL: http://www.cdc.gov/h1n1flu/childcare/guidance.htm. [Google Scholar]
- 5.CDC (US) Atlanta: CDC; 2009. [cited 2012 Apr 11]. Guidance for businesses and employers to plan and respond to the 2009-2010 influenza season. Also available from: URL: http://www.cdc.gov/h1n1flu/business/guidance. [Google Scholar]
- 6.SteelFisher GK, Blendon RJ, Bekheit MM, Lubell K. The public's response to the 2009 H1N1 influenza pandemic. N Engl J Med. 2010;362:e65. doi: 10.1056/NEJMp1005102. [DOI] [PubMed] [Google Scholar]
- 7.Parental attitudes and experiences during school dismissals related to 2009 influenza A (H1N1)—United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(35):1131–4. [PubMed] [Google Scholar]
- 8.Snowden DJ. The paradox of story: simplicity and complexity in strategy. Scenario and Strategy Planning. 1999;1:16–20. [Google Scholar]
- 9.Federal Emergency Management Agency (US) Washington: FEMA; 2008. [cited 2010 Dec 1]. Incident Command System review material. Also available from: URL: http://www.training.fema.gov/EMIWeb/IS/ICSResource/assets/reviewMaterials.pdf. [Google Scholar]
- 10.Markel H, Lipman HB, Navarro JA, Sloan A, Michalsen JR, Stern AM, et al. Nonpharmaceutical interventions implemented by US cities during the 1918-1919 influenza pandemic [published erratum appears in JAMA 2007;298:2264] JAMA. 2007;298:644–54. doi: 10.1001/jama.298.6.644. [DOI] [PubMed] [Google Scholar]
- 11.Halloran ME, Ferguson NM, Eubank S, Longini IM, Jr, Cummings DA, Lewis B, et al. Modeling targeted layered containment of an influenza pandemic in the United States. Proc Natl Acad Sci. 2008;105:4639–44. doi: 10.1073/pnas.0706849105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davey VJ, Glass RJ, Min HJ, Beyeler WE, Glass LM. Effective, robust design of community mitigation for pandemic influenza: a systematic examination of proposed US guidance. PLoS One. 2008;3:e2606. doi: 10.1371/journal.pone.0002606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bell DM, World Health Organization Working Group on Prevention of International and Community Transmission of SARS Public health interventions and SARS spread, 2003. Emerg Infect Dis. 2004;10:1900–6. doi: 10.3201/eid1011.040729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van Gemert C, Hellard M, McBryde ES, Fielding J, Spelman T, Higgins N, et al. Intrahousehold transmission of pandemic (H1N1) 2009 virus, Victoria, Australia. Emerg Infect Dis. 2011;17:1599–607. doi: 10.3201/eid1709.101948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pang X, Yang P, Li S, Zhang L, Tian L, Li Y, et al. Pandemic (H1N1) 2009 among quarantined close contacts, Beijing, People's Republic of China. Emerg Infect Dis. 2011;17:1824–30. doi: 10.3201/eid1710.101344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ibuka Y, Chapman GB, Meyers LA, Li M, Galvani AP. The dynamics of risk perceptions and precautionary behavior in response to 2009 (H1N1) pandemic influenza. BMC Infect Dis. 2010;10:296. doi: 10.1186/1471-2334-10-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nicoll A, Coulombier D. Europe's initial experience with pandemic (H1N1) 2009—mitigation and delaying policies and practices. Euro Surveill. 2009;14:19279. doi: 10.2807/ese.14.29.19279-en. pii. [DOI] [PubMed] [Google Scholar]
- 18.Chao DL, Halloran ME, Longini IM., Jr School opening dates predict pandemic influenza A (H1N1) outbreaks in the United States. J Infect Dis. 2010;202:877–80. doi: 10.1086/655810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chu CY, Li CY, Zhang H, Wang Y, Huo D, Wen L, et al. Quarantine methods and prevention of secondary outbreak of pandemic (H1N1) 2009. Emerg Infect Dis. 2010;16:1300–2. doi: 10.3201/eid1608.091787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.De Serres G, Rouleau I, Hamelin ME, Quach C, Skowronski D, Flamand L, et al. Contagious period for pandemic (H1N1) 2009. Emerg Infect Dis. 2010;16:783–8. doi: 10.3201/eid1605.091894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gift TL, Palekar RS, Sodha SV, Kent CK, Fagan RP, Archer WR, et al. Household effects of school closure during pandemic (H1N1) 2009, Pennsylvania, USA. Emerg Infect Dis. 2010;16:1315–7. doi: 10.3201/eid1608.091827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu JT, Cowling BJ, Lau EH, Ip DK, Ho LM, Tsang T, et al. School closure and mitigation of pandemic (H1N1) 2009, Hong Kong. Emerg Infect Dis. 2010;16:538–41. doi: 10.3201/eid1603.091216. [DOI] [PMC free article] [PubMed] [Google Scholar]