Abstract
The use of over-the-counter (OTC) cough and cold products in children has become a hot topic in the news in the past year due to the potential risk associated with using these products in children. The most recent recommendations were announced in October 2008 from The Consumer Healthcare Products Association (CHPA) which stated that OTC cough and cold medications should not be used in children less than 4 years old.1 Because of this, parents and healthcare professionals have many questions and concerns. This article will review the current data supporting the recent recommendations and provide strategies and suggestions for educating parents and caregivers when a child has complaints of cough and cold symptoms.
Keywords: adverse effects, cold, cough, FDA, OTC, over-the-counter
INTRODUCTION
The Food and Drug Administration has permitted marketing of OTC cough and cold medications in children since 1976 under the “Generally Recognized as Safe and Effective” (GRASE) classification, despite the lack of data for use in children. It was not until 2007 when the FDA started to review these products again due to recent case reports of adverse events and deaths and a citizen petition that was filed. The petition requested the FDA re-review use of these products in children and publicly state the lack of safety and efficacy data for use of OTC cough and cold medications in children < 6 years old.2 In October 2007, the FDA, the Pediatric Advisory Committee and the Non-Prescription Drug Advisory Committee convened to review the data. Around this same time, various manufacturers voluntarily withdrew all infant formulations of cough and cold medications from the market.
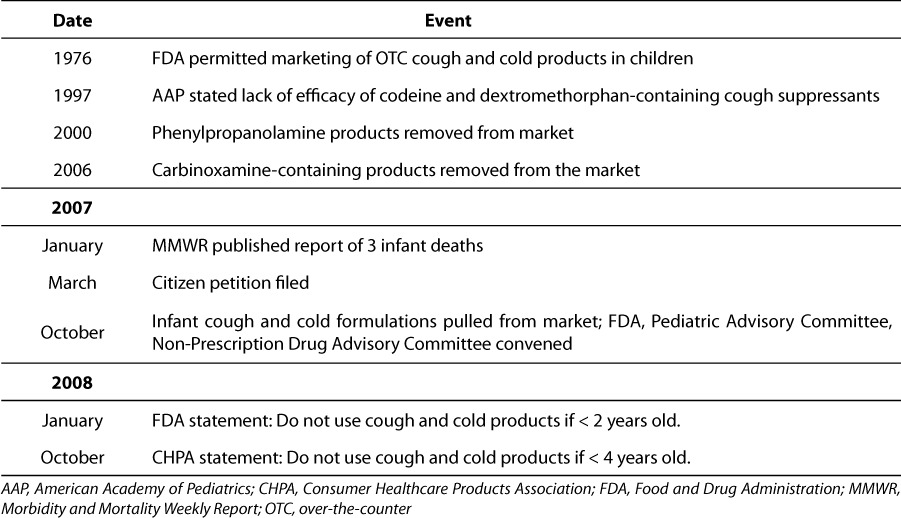
It is important to realize that there was some trail of evidence leading up to this voluntary withdrawal (Table). In 1997, the American Academy of Pediatrics (AAP) Committee on Drugs published a statement regarding the lack of efficacy of codeine and dextromethorphan-containing antitussive products in children.3 Then in 2000, phenylpropanolamine-containing products were banned because of the increased risk of stroke in women. In 2006, carbinoxamine-containing products were officially withdrawn from the market and in this same year, the American College of Chest Physicians' cough guidelines recommended against the use of OTC agents for cough because of increased morbidity and mortality reported in at least three pediatric cases.4 Finally, in January 2007, Morbidity and Mortality Weekly Report published three infant deaths that were attributed to cough and cold medication use.5 All three infants had high concentrations of pseudoephedrine postmortem and the fatalities were deemed nonintentional.
Table.
Timeline of Events Related to FDA Regulation of OTC Cold and Cough Medications
In spite of these statements and published reports, over-the-counter cough and cold product use remains very prevalent in the United States. Two surveys found that there was about a 10% prevalence of use of cough and cold medications in children in any one week.6–7 The earlier survey included 3-year-old children. Fifty-four percent of these 8000 children had received an over-the counter medication in the past thirty days. In the more recent Slone Survey, about 10% of 4267 children < 18 years old (median age 9 years) had used a cough and cold medication in the previous week. Over 50% of the products used in the Slone Survey were combination products that included an antihistamine, decongestant and antitussive medication. In another publication posted on the FDA website, BeMedWise.org, 86% of 1000 parents reported that they would use an OTC medication prior to or instead of consulting a pediatrician.8 These statistics demonstrate that OTC medication use in young children remains a widespread modality for treating the common cold, despite the lack of evidence proving efficacy and increased data supporting adverse effects.
In January 2008 a report was published from the National Electronic Injury Surveillance System-Cooperative Adverse Event Surveillance project analyzing about 160,000 patients ≤ 18 years of age treated in an emergency department for an adverse drug event (ADE).9–10 This voluntary survey included 63 US hospitals, which was a nationally representative sample, with a minimum of 6 beds and having a 24-hour adult and/or pediatric emergency department. The most common reason for the ADEs was reported to be unintentional overdose and this was most commonly encountered in children ages 1 to 4 years old.9–10 An annual estimate of 5.2% of ADEs was reported to be caused by cough and cold product combinations. When reviewing the cough and cold product combinations reported to cause the ADEs, most of the events were due to unsupervised ingestion, which was defined as cases where the child obtained the medication without adult supervision. Most of these cases were in children ≤ 5 years of age.9
This report along with other reviews prompted the FDA warnings in January 2008. The public health advisory recommended against OTC cough and cold product use in children < 2 years old and gave specific advice to help guide care-givers and healthcare professionals. However, the question remains whether these products are safe or effective for the common cold and cough.
Decongestants are known to cause vasoconstriction and tachycardia, and some patients may experience tachypnea.11 These agents can also have central nervous system (CNS) effects. In March 2006, the Combat Methamphetamine Epidemic Act was passed, restricting the sale of OTC pseudoephedrine without proper identification and review by a pharmacist due to the potential for abuse.12
Typically, antihistamines are considered CNS depressants, causing drowsiness. In young children, however, a paradoxical effect, usually excitability, can be observed.11 For the common cold and cough, antihistamines are used for their anticholinergic effects (i.e., drying up secretions), but in some patients, these anticholinergic effects can manifest as tachycardia, agitation and blurry vision. Besides the known pharmacological effects of these medications, published clinical experience does not support efficacy.
REVIEW OF LITERATURE
Hutton and colleagues studied the efficacy of a combination antihistamine-decongestant product versus placebo versus no medication for the common cold.13 The combination product used was brompheniramine maleate with pseudoephedrine hydrochloride. This study investigated the parents beliefs about medication needed for treatment, the effectiveness of the combination product, and if parents who wanted and received medication for their child noted an improvement after 48 hours. Patients were recruited from a primary care walk-in clinic at Johns Hopkins Hospital during the winter season. Ninety-six children whose mean age was 25 ± 15.7 months (range, 6 months to 5 years) were evaluated over a two-day period. About 50% of the population was girls, primarily black, living in an inner city. Randomization was completed with 36 children in the medication group, 27 children in the placebo group and 33 children in the no medication group.
In speaking to the parents via phone, about two-thirds believed medication was necessary for treatment of the common cold.13 Cold symptoms (i.e., congestion, rhinorrhea, fever, or sleep) improved in 67% of those receiving an antihistamine-decongestant product, 71% given placebo and 57% who received no medication. The authors concluded that there was no difference in the relief of cold symptoms when placebo and medication were compared. However, improvement of symptoms was greater in children of parents who initially desired to use medications compared to those whose parents did not want to use medications.
Another study evaluated the effect of cough suppressants in 49 children.14 Children with a significant night cough for < 14 days and who were between the ages of 18 months and 12 years were followed for three days. The mean age was 4.7 ± 2.3 years with the majority of the patients being white and about 50% female. Codeine plus guaifenesin or dextromethorphan hydrobromide plus guaifenesin were compared to placebo. Randomization resulted in 17 children receiving codeine, 19 children receiving dextromethorphan and 13 children receiving placebo.
Parents were given a questionnaire at baseline and on the morning following each day of the study to evaluate the amount of coughing and loss of sleep and any posttussive emesis. There was no significant difference between groups (p>0.5), and neither codeine nor dextromethorphan were found to be significantly better than placebo (p=0.7 and 0.41, respectively). Interestingly, regardless of treatment group, all patients started to improve on day 3.14
Clemens et al. assessed the effect of a combined antihistamine/decongestant (brompheniramine maleate with phenylpropanolamine hydrochloride) compared to placebo for an upper respiratory tract infection that had been evident for less than 7 days.15 Fifty-nine children (6 months to 5 years old) were included in this two day study. Fifty percent were female, and the mean age was 23.7 months for the medication group and 30.1 months for the placebo group. The duration of upper respiratory tract symptoms was about 3 ± 1.4 days for each group. Up to four doses of medication were allowed per patient, administered no more often than every 4 hours.
Two hours after administration of each dose of medication or placebo, a parent evaluated the child's response.15 Parents were instructed to evaluate rhinorrhea, congestion and cough on a 7-point Likert scale ranging from ‘much worse' to ‘much better'. Overall, no difference was observed in symptoms (p>0.5 for rhinorrhea, nasal congestion and cough). However, patients who received the combination antihistamine/ decongestant product were more likely to be asleep 2 hours after administration of medication (p<0.01).
One final double-blind, randomized study reviewed whether there was any improvement in nocturnal cough secondary to an upper respiratory tract infection and sleep quality in patients receiving either diphenhydramine hydrochloride or dextromethorphan hydrobromide, compared to placebo.16 The average duration of illness was 4.21 ± 1.57 days. One hundred children, 2 to 18 years of age, were included in this one-night study. The median age was 4.5 years, more than 75% were white and 58% were female. Thirty-three patients received diphenhydramine, 33 were administered dextromethorphan, and 34 patients received placebo. A 7-point Likert scale was given to parents to assess cough and sleep the night before study enrollment and for the subsequent night when either medication or placebo was administered.
No significant difference was observed in cough reduction (p=0.56), or child (p=0.28) or parent (p=0.85) sleep quality. There was a slight trend toward improved sleep quality in the children administered the diphenhydramine hydrochloride. As in a previous study, symptoms started to improve on the second night, regardless of intervention.
PROPOSED STRATEGIES
This lack of evidence demonstrating efficacy, combined with data supporting increasing adverse effects with over-the-counter cough and cold product use in children, require that parents/caregivers and healthcare professionals implement strategies to avoid or reduce adverse events.5 Parents and caregivers must read carefully the product labels for information related to appropriate use (i.e., Drug Facts and the active ingredient). This is intended to help guide correct use of the product and to prevent duplicate medications from being administered. At this time, it is extremely important as there will be a transition period in the implementation of the recent CHPA recommendations. This may result in different product labeling from one product to another. For example, some products will state “do not use” for children < 4 years old and others will still state “do not use” for children < 2 years old. Reviewing the product's instructions for use and using the provided measuring device is also important for minimizing or, hopefully, preventing dosing errors. If no administration device is provided with the product, the health-care professionals must provide the family with an appropriate labeled measuring device (i.e., an oral syringe) to decrease dose measuring errors. Also, the parent/caregiver must receive education that these medications are intended only for symptomatic relief and will not treat the common cold or cough. These products should never be used for their side effects (i.e., to help the child fall asleep). Finally, in order to prevent accidental exposure, these products, as with all medications, should be stored out of sight and reach from children.
Some other strategies for health care professionals to recommend to parents/caregivers include proper advice about fever and pain relief (i.e., recommending acetaminophen or ibuprofen as single-ingredient agents for these indications). Educate families regarding proper disposal of medications and posting of the poison control center telephone number (i.e., on the telephone or refrigerator). Finally, emphasize the nonpharmacological options for symptomatic relief of the common cold/cough in children. Adequate hydration, cool mist humidification and saline nose drops are inexpensive and easy strategies to implement.
CONCLUSION AND SUMMARY
As of October 2008, CHPA has recommended that OTC cough and cold products not be used in children < 4 years old. The FDA supports this statement and manufacturers have started to voluntarily change labeling to reflect this recommendation. Even though this new recommendation is fairly clear, there are still some concerns. Parents/ caregivers may intentionally or mistakenly use adult-based preparations for children, stockpile medications in the home or demand prescription medications. Parents/caregivers may also start to use herbal and alternative therapies.
Despite the recent warnings of adverse events, over-the-counter cough and cold product use in children remains prevalent. Pharmacists need to be aware of the potential risk involved with using these medications and provide strategies to not only prevent adverse events but also to educate caregivers regarding alternative options. The nonpharmacological suggestions given within this article are safe and may offer some symptomatic benefit. Pharmacists should also educate caregivers and healthcare providers about the facts of the typical cough and cold, remembering that these symptoms usually are due to a viral infection that continues for 10 to 14 days, but does improve with time. Children with a cough or fever that lasts for more than 10 to 14 days or are < 3 months old with these symptoms, should see a physician. Finally, pharmacists need to always secure a complete medication history, including not only prescription medication, but also over-the-counter medication use and dietary and herbal supplement use.
ABBREVIATIONS
- ADE
adverse drug event
- AAP
American Academy of Pediatrics
- CNS
central nervous system
- FDA
Food and Drug Administration
- GRASE
Generally Recognized as Safe and Effective
- OTC
over-the-counter
- CHPA
Consumer Healthcare Products Association
Footnotes
see Editorial page 124
AAP, American Academy of Pediatrics; CHPA, Consumer Healthcare Products Association; FDA, Food and Drug Administration; MMWR, Morbidity and Mortality Weekly Report; OTC, over-the-counter
REFERENCES
- 1.Consumer Healthcare Products Association. Available at: http://www.chpa-info.org. Accessed April 23, 2009.
- 2.Food and Drug Administration. Available at: http://www.fda.gov. Accessed April 17, 2009.
- 3.American Academy of Pediatrics. Committee on Drugs. Use of codeine- and dextromethorphan-containing cough remedies in children. Pediatrics. 1997;99:918–920. doi: 10.1542/peds.99.6.918. [DOI] [PubMed] [Google Scholar]
- 4.American College of Chest Physicians. Diagnosis and management of cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl):1S–292S. doi: 10.1378/chest.129.1_suppl.287S. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Infant deaths associated with cough and cold medications—two states, 2005. MMWR Morb Mortal Wkly Rep. 2007;56:1–4. [PubMed] [Google Scholar]
- 6.Vernacchio L, Kelly JP, Kaufman DW. Cough and cold medication use by US children, 1999–2006: Results from the Slone survey. Pediatrics. 2008;122:e323–e329. doi: 10.1542/peds.2008-0498. et al. [DOI] [PubMed] [Google Scholar]
- 7.Kogan MD, Pappas G, Yu SM. Over-the-counter medication use among US pre-school-age children. JAMA. 1994;272:1025–1030. et al. [PubMed] [Google Scholar]
- 8.Be MedWise (a campaign of the National Council on Patient Information and Education) Available at: http://www.bemedwise.org. Accessed April 22, 2009.
- 9.Schaefer MK, Shehab N, Cohen AL. Adverse events from cough and cold medications in children. Pediatrics. 2008;121:783–787. doi: 10.1542/peds.2007-3638. et al. [DOI] [PubMed] [Google Scholar]
- 10.Cohen AL, Budnitz DS, Weidenbach KN. National surveillance of emergency department visits for outpatient adverse drug events in children and adolescents. J Pediatr. 2008;152:416–421. doi: 10.1016/j.jpeds.2007.07.041. et al. [DOI] [PubMed] [Google Scholar]
- 11.Gunn VL, Taha SH, Liebelt EL. Toxicity of over-the-counter cough and cold medications. Pediatrics. 2001;108:e52. doi: 10.1542/peds.108.3.e52. et al. [DOI] [PubMed] [Google Scholar]
- 12.United States Department of Justice Drug Enforcement Administration. Office of Diversion Control. Combat Methamphetamine Epidemic Act 2005. Available at: http://www.deadiversion.usdoj.gov/meth. Accessed June 19, 2009.
- 13.Hutton N, Wilson MH, Mellits D. Effectiveness of an antihistamine-decongestant combination for young children with the common cold: a randomized, controlled trial. J Pediatr. 1991;118:125–130. doi: 10.1016/s0022-3476(05)81865-7. et al. [DOI] [PubMed] [Google Scholar]
- 14.Taylor JA, Novack AH, Almquist JR. Efficacy of cough suppressants in children. J Pediatr. 1993;122:799–802. doi: 10.1016/s0022-3476(06)80031-4. et al. [DOI] [PubMed] [Google Scholar]
- 15.Clemens CJ, Taylor JA, Almquist JR. Is an antihistamine-decongestant combination effective in temporarily relieving symptoms of the common cold in preschool children? J Pediatr. 1997;130:463–466. doi: 10.1016/s0022-3476(97)70211-7. et al. [DOI] [PubMed] [Google Scholar]
- 16.Paul IM, Yoder KE, Crowell KR. Effect of dextromethorphan, diphenhydramine, and placebo on nocturnal cough and sleep quality for coughing children and their parents. Pediatrics. 2004;114:e85–90. doi: 10.1542/peds.114.1.e85. et al. [DOI] [PubMed] [Google Scholar]


