Abstract
BACKGROUND
Chances of achieving parenthood are high for couples who undergo fertility treatment. However, many choose to discontinue before conceiving. A systematic review was conducted to investigate patients' stated reasons for and predictors of discontinuation at five fertility treatment stages.
METHODS
Six databases were systematically searched. Search-terms referred to fertility treatment and discontinuation. Studies reporting on patients' stated reasons for or predictors of treatment discontinuation were included. A list of all reasons for discontinuation presented in each study was made, different categories of reasons were defined and the percentage of selections of each category was calculated. For each predictor, it was noted how many studies investigated it and how many found a positive and/or negative association with discontinuation.
RESULTS
The review included 22 studies that sampled 21 453 patients from eight countries. The most selected reasons for discontinuation were: postponement of treatment (39.18%, postponement of treatment or unknown 19.17%), physical and psychological burden (19.07%, psychological burden 14%, physical burden 6.32%), relational and personal problems (16.67%, personal reasons 9.27%, relational problems 8.83%), treatment rejection (13.23%) and organizational (11.68%) and clinic (7.71%) problems. Some reasons were common across stages (e.g. psychological burden). Others were stage-specific (e.g. treatment rejection during workup). None of the predictors reported were consistently associated with discontinuation.
CONCLUSIONS
Much longitudinal and theory led research is required to explain discontinuation. Meanwhile, treatment burden should be addressed by better care organization and support for patients. Patients should be well informed, have the opportunity to discuss values and worries about treatment and receive advice to decide about continuing treatment.
Keywords: fertility treatment, discontinuation, dropout, predictors, decisional aid
Introduction
Infertility affects 9–15% of couples of childbearing age (Boivin et al., 2007) and is defined by the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse (Zegers-Hochschild et al., 2009). About 56% of these couples will seek medical assistance to conceive (Boivin et al., 2007). Although the chances of achieving parenthood can be as high as 72% for couples undergoing treatment (Pinborg et al., 2009; Brandes et al., 2010), many choose to discontinue treatment before achieving a live birth. Discontinuation of fertility treatment refers to the decision to opt out of (further) treatment, despite a favourable prognosis and ability to cover the costs of treatment (Boivin et al., 2012). Research focusing on discontinuation started as early as 1980 (Meijer and Hamerlynck, 1980) and was motivated by the need to understand its impact on treatment efficacy (e.g. Land et al., 1997) and why some couples discontinue treatment (e.g. Callan et al., 1988). It is known that discontinuation can occur at any treatment stage, from as early as diagnostic workup (Eisenberg et al., 2010) to any stage during assisted reproductive technologies (ART; Olivious et al., 2004) and that treatment success rates are negatively affected by it (Land et al., 1997; Witsenburg et al., 2005). Why couples discontinue treatment is not entirely clear. It is known that they discontinue due to different reasons and that these vary according to treatment stage (Brandes et al., 2009). The aim of the present systematic review was to examine reasons and predictors of discontinuation from fertility treatment.
Past research has mainly identified causes for discontinuation by asking patients to state their reasons for discontinuing (hereafter ‘stated reasons’). The typical approach is to ask couples to choose from a structured list of reasons for stopping treatment, which applies to them (e.g. Akyuz and Sever, 2009; Van den Broeck et al., 2009). Reasons can be requested at different time points after treatment and lists can contain any number of reasons, but participants are typically women reporting on the couple's joint decision-making. This structured method is useful because it gives the patients' perspective on discontinuation. However, the reasons offered to patients are often general or vague (e.g. emotional distress, psychological burden, Verhagen et al., 2008; Brandes et al., 2009) or do not cover all possible causes. Further, the retrospective nature of this method makes it difficult to distinguish cause from effect, that is, whether the reason was the reason at the time of discontinuation, which could have been many years before, or whether it emerged as a consequence of the discontinuation itself. The inability to identify which factors cause discontinuation and how, makes it difficult to use the discontinuation data to profile patients at risk of discontinuation or to identify targets for interventions. Some researchers have tried to reach greater precision in the identification of causes by investigating the relationship between pretreatment variables (e.g. age at start of treatment, pretreatment depression) and the occurrence of discontinuation, aiming to identify its predictors. Most prediction studies focus on treatment variables (mostly prognosis indicators, e.g. Pearson et al., 2009) and do not differentiate between different stages in the treatment trajectory (e.g. diagnostic workup, ovulation induction; Brandes et al., 2009). Therefore information from prediction studies has yet to be translated into changes in clinical practice.
A more recent integrated approach to fertility healthcare (Boivin et al., 2012) suggests that treatment (e.g. type and effect, Verberg et al., 2008; Verhagen et al., 2008), clinic (e.g. quality of care, Van den Broeck et al., 2009) and patient factors (e.g. psychological distress, Smeenk et al., 2004) have reciprocal influences on each other and all potentially contribute to discontinuation by adding to the burden of fertility treatment. The identification of these factors is crucial to pinpoint the onerous aspects of treatment that should be minimized or even eliminated and to ensure that patient decision-making about continuing or stopping recommended treatment is made free of constraints and solely based on individual values and preferences (WHO, 2003). Because treatment success rates are influenced by patients' compliance (Land et al., 1997; Witsenburg et al., 2005), interventions targeting such burdensome aspects of treatment could eventually also result in more couples becoming parents.
The aim of the present systematic review was to describe patients' stated reasons for discontinuation from fertility treatment and to identify treatment, clinic and patient predictors of discontinuation.
Methods
Systematic search
A systematic literature search was conducted in six databases (Medline, Medline In Progress, EMBASE, BNI, PsycINFO and The Cochrane Library) from 1978 until December 2011 (inclusively). A search strategy was created using terminology from the International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART (Zegers-Hochschild et al., 2009) that was based on search terms for fertility treatment (e.g. fertility treatment, artificial insemination, assisted reproductive technology, in vitro fertilization or variations) AND discontinuation (variations of dropout or compliance or discontinuation or end or stop or termination or withdrawal or abandon or quit or stay or persist or persevere or attrition). With small adaptations, this strategy was used in all databases). MeSH terms were used in PubMed (See Table 1 of Supplementary material). No restriction was made on the type (journal, conference paper or dissertation) or language of publication. A comprehensive examination of the reference sections of all identified articles was carried to identify other relevant manuscripts. All citations were transferred to EndNote (Thomson Reuters, San Francisco, CA, USA).
Study selection
Longitudinal and/or cross-sectional studies were included if they reported on the number of patients who discontinued fertility treatment and on patients' stated reasons for discontinuation or predictors of discontinuation (assessed prior to the occurrence of discontinuation behaviour). By ‘stated reasons’, we mean the reasons endorsed by the patient on structured or unstructured surveys or interviews. By ‘predictors’, we mean factors that were measured at the start or during treatment and that were then used to predict discontinuation (whether significant or not). Reasons for discontinuation could be assessed on cross-sectional or longitudinal studies, however, to investigate predictors, only longitudinal studies were considered. Discontinuation from fertility treatment can occur at any time between the patient's first visit to the clinic and the last recorded cycle of an ART regimen. Accordingly, five stages of fertility workup and treatment were defined that correspond to critical decision points when patients decide about undergoing treatment. These were whether to: (i) initiate treatment (INITIATE), (ii) undertake first-order treatments like insemination or ovulation induction (FIRST), (iii) undergo treatment with assisted reproductive techniques (ART-START), (iv) continue after a failed ART cycle (ART-FAILED) or (v) discontinue before completion of the typical ART regimen (ART-TYPICAL). Studies differed in the number of ART cycles followed up. To control for this variability, we based our analysis for ART-TYPICAL on the first three ART cycles because this is the typical ART regimen for optimal chances of success and the usual number of cycles covered by subsidized health care provision (where it exists, e.g. National Institute for Clinical Excellence (NICE), 2004). Exceptions were allowed when there were compelling reasons to consider more than three cycles (e.g. nine subsidized cycles of modified natural IVF, Pelinck et al., 2007).
Studies were included if the reported discontinuation data could be assigned to at least one of the described treatment stages. For the analysis of patients' stated reasons for discontinuation, studies were included if the data reported could be individually assigned to at least one of the defined treatment stages. However, for the analysis of predictors of discontinuation most studies did not meet this condition. Therefore, studies where the reported data covered all ART treatment stages but could not be individually assigned to only one of these stages were also included (i.e. ART-START or ART-FAILED or ART-TYPICAL, e.g. Pelinck et al., 2007; Pearson et al., 2009; Verhagen et al., 2008).
The first author (S.G.) screened titles, abstracts and if necessary full text reports of all studies identified by the search strategy and excluded studies were classified according to reason for exclusion (see Fig. 1). A research specialist (Debbie Moss (D.M.)) crosschecked this process independently.
Figure 1.
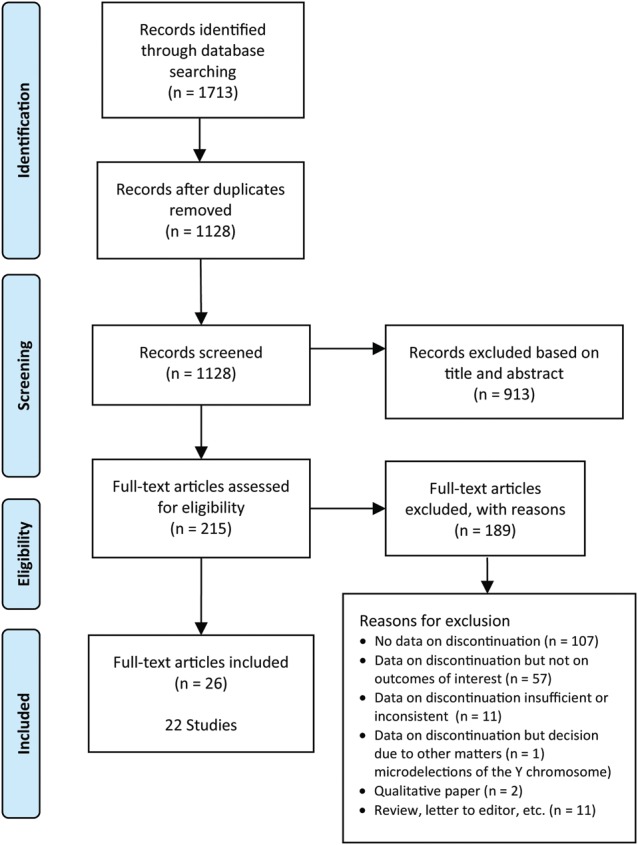
Decision flowchart for identified studies.
Duplicate or secondary publications on the same sample were excluded to avoid multiple publication bias. In these cases, priority was given to the publication that focused on discontinuation from treatment.
Data extraction
S.G. and a research specialist (D.M.) extracted data using a standardized protocol. Whenever there were missing or inconsistent data in a manuscript, these were requested from the authors. Disagreement was resolved by discussion and agreement was reached in all cases.
To characterize the set of studies, we extracted data (where available) regarding the country, sample size, design (longitudinal or cross-sectional), population (general population that undergoes fertility treatment or selected group of patients) and fertility treatment (e.g. intrauterine insemination with or without donor insemination, in vitro fertilization) and about whether treatment was subsidized/reimbursed. In addition, it was noted whether studies made explicit reference to theoretical frameworks underlying the implemented research, defined as a set of inter-related propositions (theoretical constructs) that constitute a framework for describing, explaining and predicting the behaviour (i.e. discontinuation) under analysis (Durand et al., 2008). Data concerning discontinuation was number of patients who discontinued and continued treatment.
All but one study (Goldfarb et al., 1997) investigated reasons for discontinuation by asking patients to select one or more reasons from a structured list of possible reasons (multiple selections were permitted in some studies). For each study, the data extracted comprised all reasons on the structured list and the number of times each reason was selected. Goldfarb et al. (1997) asked patients whether they agreed, were uncertain or disagreed that each of the reasons on the structured list had been a cause for discontinuation. For the purpose of the systematic review, answers of ‘agree’ or ‘uncertain’ to each of the reasons in the structured list of this particular study were counted as selections of that reason while answers of ‘disagree’ were not. Finally, it was noted whether studies allowed patients to select only one or multiple reasons.
Data on all predictors of discontinuation investigated in each study were extracted. Data were also extracted on the statistical significance, direction and strength of associations between these predictors and discontinuation behaviour (when statistical tests were reported). The necessary sample sizes to detect medium effect sizes (power = 0.80, alpha = 0.05) in t-test, product-moment correlation and univariate analysis of variance are 65, 67 and 90, respectively. To detect small effect sizes, necessary sample sizes are 600, 620 and 790, respectively (G*Power, Faul et al., 2007). Based on these numbers and on the number of patients who discontinued and continued treatment in each study, the number of studies which had enough power to detect small and medium effect size was estimated. Finally, it was noted whether studies excluded patients who were recommended to end treatment (i.e. doctor censoring) from the analysis of predictors. In those studies that excluded doctor censored patients from the discontinuers group, decision-making can be solely attributed to the patients, however, in those studies that did not exclude doctor censored patients such an inference cannot be made (as some decisions were made by the physicians due to poor treatment prognosis).
Quality assessment
S.G., J.B., L.P. and C.M.V. assessed study quality according to Newcastle-Ottawa Quality (NOQ) assessment scale (Wells et al., 2010) adapted for the present study. The NOQ is used to appraise quality in terms of population representativeness (1 point), measurement of outcome (i.e. discontinuation, 3 points), within population comparability (2 points) and adequacy of follow-up (i.e. completion rates, 1 point, only applicable in longitudinal studies). (See Supplementary data, Table 3 for a detailed description of critical appraisal criteria.) Cross-sectional studies were assessed based on the first three criteria described and quality ratings were grouped into low (0–2), average (3–4) and high (5–6) quality studies. Longitudinal studies were assessed based on the four criteria described and quality ratings were grouped into low (0–2), average (3–5) and high (6–7) quality studies. The level of agreement between coders (S.G., J.B., L.P., C.M.V.) was calculated using the Cohen's Kappa statistic (Cohen, 1960) and disagreement was resolved with discussion.
Data synthesis
A list of all reasons presented in each study's structured list of reasons for discontinuation was made. Based on this list, different categories for reasons were defined and the level of agreement between coders (S.G., J.B., C.M.V.) was again calculated using the Cohen's Kappa statistic. Disagreement was resolved with discussion.
The chance of a specific reason to be selected was dependent on the set of choices made available to patients (i.e. number of options on the structured list) and on whether multiple selections were allowed. Because these factors varied across studies (see Supplementary data, Table 5 for detailed information), direct comparisons of the number of selections between studies were not possible. Therefore, we report how many times patients chose to select a given category whenever it was presented as a selection option. That is, for each of the defined categories, we noted the number of studies in the systematic review that investigated that category (k), the total number of selections of that category in those studies (s) and the total number of selections of all categories represented in those same studies (S) (Supplementary data, Table 7). We then calculated percentage of selections for each reason category (P = s/S) and 95% confidence intervals (CIs) (Newcombe, 1998). This was done in relation to each treatment stage and in relation to the total of all included studies (overall). In this scoring, 0 indicated that the reason category was never selected when it was made available and 100 indicated that the reason category was always selected.
For each treatment, clinic and patient predictor of discontinuation reported in the systematic review, we noted how many studies investigated it and, from these, how many found a statistically significant positive and/or negative association with discontinuation from treatment.
Results
Description of studies
The database and manual search yielded 1128 non-duplicated records that contained the relevant treatment and discontinuation terms. Figure 1 presents the study decision-flow chart whereby 22 studies were included in the systematic review. Of these, 1102 studies (97.7%) did not meet inclusion criteria and were excluded (see Figure 1 for information on reasons for exclusion and Table 2 of supplemental material for reason for exclusion per individual manuscript). S.G. and D.M. agreed on inclusion for all studies and agreed on reasons for exclusion for 91% of studies. We contacted the authors of the eleven papers with missing or inconsistent data and seven more authors of papers included to obtain other additional data (e.g. treatment coverage/reimbursement) from the manuscripts. Four authors replied stating that the requested data was not available.
The included studies sampled 21 453 patients in eight countries. The sample and design characteristics of the 22 included studies are shown in Table I. The majority of studies were longitudinal (n = 19, 86%) and about half focused on the general population that undergoes fertility treatment (n = 12, 55%) and on standard treatments (n = 11, 50%, versus specific ART treatments such as modified natural IVF or transport IVF/ICSI). Ten (45%) studies stated that treatment was subsidized or reimbursed while three (14%) specifically stated that it was not and one (5%) reported high variations in funding (36% not reported). None of the studies made explicit reference to theoretical frameworks underlying their work.
Table I.
Sample and design characteristics of the 22 included studies.
| Study and country | Sample sizea | Design | Selected population | Fertility treatment | Subsidized/reimbursed treatment | Discontinuation outcomes reported by treatment stage |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reasons |
Predictors |
||||||||||||||
| INITIATE | FIRST | ART- START | ART- FAILED | ART- TYPICAL | INITIATE | FIRST | ART- START | ART- FAILED | ART- TYPICAL | ||||||
| Brandes et al. (2009), The Netherlands | 1391 couples, DISC: 144 Initiate, 75 First, 57 ART Typical | Longitudinal | No | OI, IUI and IVF/ICSI | Yes | ✓ | ✓ | ✓ | |||||||
| Danesh-Meyer et al. (1993), New Zeeland | 261 couples, DISC: 80, CONT: 47 | Longitudinal | No | DI | NR | ✓ | ✓ | ||||||||
| De Vries et al. (1999), Belgium | 1169 women, DISC: 204 ART c1, 106 ART c2, CONT: 552 ART c1, 220 ART c2 | Longitudinal | No | IVF/ICSI | NR | ✓ | |||||||||
| Domar et al. (2010), USA | DISC: 41 women | Cross sectional | Excluded patients over 40 and using testicular biopsy | IVF/ICSI | Yes | ✓ | |||||||||
| Eisenberg et al. (2010), USA | 434 couples, DISC: 55, CONT: 379 | Longitudinal | No | NA | NR | ✓ | ✓ | ||||||||
| Goldfarb et al. (1997), USA | DISC 28 couples | Cross sectional | No | IVF/ICSI | No | ✓ | |||||||||
| Guerif et al. (2002), Italy | 588 couples, DISC: 123, CONT: 124 | Longitudinal | Severe male infertility | DI | Yes | ✓ | |||||||||
| Guerif et al. (2003), Italy | 222 couples, DISC: 56, CONT: 21 | Longitudinal | Women who had already conceived with previous AID with donor sperm | DI | Yes | ✓ | ✓ | ||||||||
| Malcom and Cumming (2004), Canada | 550 couples, DISC: 329 | Longitudinal | No | NR | No | ✓ | |||||||||
| Meijer and Hamerlynck, (1980), The Netherlands | 159 couples, DISC: 48 | Longitudinal | Fertile women, couple perceived as competent for parenthood | DI | NR | ✓ | |||||||||
| Meynol et al. (1997), France | DISC 46 women | Cross sectional | No | IVF | NR | ✓ | |||||||||
| Pearson et al. (2009), USA | 2245 women, DISC: 373 c1, 314 c2, CONT: 1186 ART c1, 579 ART c2 | Longitudinal | Excluded patients using donor gametes | IVF/ICSI | NR | ✓ | |||||||||
| Pelinck et al. (2007), CONT: 1186 ART c1, 579 ART c2 | 263 couples, DISC: 121, CONT: 21 | Longitudinal | Female age under 36, excluded patients requiring ICSI | Modified natural IVFb | Yes | ✓ | ✓ | ||||||||
| Roest et al. (1998), The Netherlands | 1211 women, DISC: 263 ART c1, 193 ART c2, CONT: 624 ART c1, 280 ART c2 | Longitudinal | No | Transport IVF/ICSIc | Yes | ✓ | |||||||||
| Rufat et al. (1994), France | 8362 couples, DISC: 2894 c1, 1335 c2, CONT: 3940 ART c1, 1938 ART c2 | Longitudinal | No | IVF | NR | ✓ | |||||||||
| Schover et al. (1992) (and 1994) USA | 52 couples, DISC: 13, CONT: 19 | Longitudinal | No | DI | No | ✓ | |||||||||
| Sharma et al. (2002), UK | 2056 women, DISC: 888 ART c1, CONT: 496 ART c1 | Longitudinal | Excluded patients requiring ICSI | IVF excluding ICSI | Wide variations | ✓ | |||||||||
| Smeenk et al. (2004), The Netherlands | 380 women, DISC: 51 ART c1, 40 ART c2, CONT: 237 ART c1, 135 ART c2 | Longitudinal | No | IVF/ICSI | Yes | ✓ | ✓ | ✓ | |||||||
| Steures et al. (2007), The Netherlands | 349 couples, DISC: 97, CONT: 252 | Longitudinal | No | IUI | Yes | ✓ | |||||||||
| Van Dongen et al. (2010), The Netherlands | 674 women, DISC: 86 | Longitudinal | Excluded patients using donor gametes or starting IVF for preimplantation genetic diagnosis and surgical sperm aspiration | NA | NR | ✓ | |||||||||
| Verberg et al. (2008), The Netherlands | 384 couples, DISC: 65, CONT: NR | Longitudinal | Excluded patients with previous IVF treatment or a healthy born child after a previous IVF treatment | Mild and conventional IVF/ICSI | Yes | ✓ | ✓ | ||||||||
| Verhagen et al. (2008), The Netherlands | 588 couples, DISC: 108, CONT: 480 | Longitudinal | Excluded patients starting IVF for preimplantation genetic diagnosis, surgical sperm aspiration or using donor gametes | IVF/ICSI | Yes | ✓ | ✓ | ||||||||
INITIATE = during diagnosis, before initiation of treatment; FIRST = during first-order treatments like insemination or ovulation induction; ART-START = on the waiting list to start assisted reproductive techniques; ART-FAILED = after the first failed ART cycle; ART-TYPICAL = before completion of the typical ART regimen.
c1, after first ART cycle; c2, after second ART cycle; NA, not applicable; NR, not reported; OI, ovulation induction; IVF, In vitro fertilization; ICSI, Intracytoplasmatic sperm injection; DI, intrauterine insemination with donor sperm; IUI, intrauterine insemination.
aFor studies focusing on patients' stated reasons for discontinuation sample size and the number of patients who discontinued treatment (DISC) is presented, for studies focusing on predictors of discontinuation the number of patients who continued treatment (CONT) is also presented.
bFollicle that spontaneously develops to dominance is used for IVF.
cAssessment, drug therapy, monitoring and egg retrieval takes place at the transport centre but the embryology and embryo replacement takes place at the clinic.
Data concerning patients' stated reasons for discontinuation could be extracted in seven (32%) of the studies included, data concerning predictors of discontinuation could be extracted in eight (36%) of the studies and data concerning both could be extracted in seven (32%) of the studies.
Quality assessment
NOQ ratings indicated 1 low-quality study (4.5%), eleven average studies (50%) and 10 high-quality studies (45.4%), with substantial inter-rater agreement (Cohen's κ ranging from 0.70 to 0.86). See Supplementary data, Table 3 for details on quality assessment.
Patients' stated reasons for discontinuation
A total of 14 studies investigated reasons for discontinuation of fertility treatment.
The list of all reasons presented to participants in each study's structured list of reasons for discontinuation contained 117 different reasons descriptors. These descriptors were matched to one of 24 defined categories. Table II presents the 24 defined categories of reasons and the reasons descriptors included in each category. Inter-coder agreement ranged between 0.82 and 0.88 (see Supplementary data, Table 5 for details on classification numbers of selections of reasons, and Tables 6 and 7 for details on the number of selections per treatment stage and overall).
Table II.
Categories and descriptors from each of the 14 studies citing reasons.
| Category | Study descriptors |
|---|---|
| A. Psychological burden of treatment | Can not stand it; emotional distress; emotional stress; psychological; psychological burden; psychological reasons; too anxious or depressed to continue; too much stress |
| B. Physical burden of treatment | Could not stand all the injections; could not stand side effects of medication; physical burden; physical discomfort; poor tolerance to physical side of treatment; retrieval too painful; side effects from treatment; treatment too aggressive for partner |
| C. Physical and Psychological burden of treatment | Both psychological and physical burden stress; physical or psychological burden of treatment; psychological stress or physical burden |
| D. Clinic related issues | Clinic reason; insufficient or poorly formulated explanations about healthcare or fertility problem; poor management of psychological aspects |
| E. Organizational problems | Language problems; therapeutic programme difficult to integrate with work |
| F. Relational problems | Divorce; infertility taking too much of a toll on our relationship; marital problems subsequent to start of treatment; relational problems; relational problems/divorce; relationship; separated; separated/divorced; separation of couple |
| G. Marital or personal problems | Marital or personal problems |
| H. Rejection of treatment | Ethical objections to ICSI treatment after failed IVF treatment; fear of abnormal child; fear of complications; getting nervous about possible long-term effects of treatment; not interested in treatment; reject treatment in general; rejected IVF treatment |
| I. No faith in treatment success | Already given IVF my best chance; just gave up; no faith in treatment; not meant to be |
| J. Poor prognosis | Age (women); medical futility; poor prognosis; problem with semen quality; problem with the menstrual cycle; too old |
| K. Logistic/practical reasons | Distance to clinic; it was too difficult to get to IVF centre so often; move; moved; moved away; moved out of state; moved to another district; partner away at present; problem with sperm donor |
| L. Personal reasons | Identifiable social reasons; personal; personal; personal life circumstances (i.e. moving, death in family, return to school) |
| M. Adoption | Adopted; adoption; decided to pursue adoption or third-party conception; planned to adopt |
| N. Other parenting options | Pursuing alternative therapy; trying on own |
| O. Abandonment of childwish | Abandoned child wish; change in priorities; do not want children anymore; partner abandoned child wish |
| P. Postponement of treatment | Decision to postpone further treatment; needing to take a break from treatment |
| Q. Postponement of treatment or unknown | Postponement or unknown |
| R. Doctor censoring | Active censuring; active censuring (failure to correct overweight status); active censuring (failure to correct underweight status); active censuring (medical reasons); active censuring (medical); active censuring (poor embryo quality); active censuring (poor response, poor fertilization, poor response with poor fertilization, overweight with BMI > 30 kg/m2, hypertension or improved semen quality not requiring ICSI any more); active censuring (poor response/signs of ovarian aging); advised by their physician to stop; no potential treatment; physician reason; poor prognosis (doctor's refusal) |
| S. Financial issues | Financial; financial concern; financial concerns; financial problems; lost insurance coverage; other (subjects listed cost of medication and donor sperm) |
| T. Health problems | Additional health problems; health problems (one of the partners); illness or operation needed; partner deceased |
| U. Other medical treatment | ART (going to IVF); ART (IVF performed); other medical treatment; other treatment; went to different IVF program |
| V. Went to other clinics | Changed IVF centres; changed medical teams to other clinic (in other city or private care); continuation of treatment elsewhere; referred to other provider; treatment elsewhere |
| W. Other/unknown/not reported | Gave no reason; loss to follow-up; lost to follow-up; no specific reason; other reasons; patients not contacted; unknown; unknown reasons |
| X. Non-classifiable | Decided to stop treatment; medical reasons; need for using sperm donor |
From the defined categories, three captured reasons for discontinuation that could be attributed to the treatment (e.g. physical burden of treatment, psychological burden of treatment), two reasons could be attributed to the clinic (i.e. clinic-related reasons, organizational problems) and 12 could be attributed to the patient (e.g. relational problems, rejection of treatment). Four categories captured reasons related to external constraints to decision-making (e.g. doctor censoring, financial issues) and three captured non-interpretable information (i.e. other/unknown/not reported, non-classifiable, went to other clinics). The ‘went to other clinics’ was grouped with non-interpretable because it was unclear whether the change in clinics was due to dissatisfaction with clinic, move of residence, personal preference or other reasons. In addition, three of the above categories captured reason descriptors that referred to more than one cause for discontinuation at the same time (i.e. physical and psychological burden of treatment, marital or personal problems, postponement of treatment or unknown). For instance, physical and psychological burden of treatment grouped the following reason descriptors: ‘psychological stress or physical burden’, ‘physical or psychological burden of treatment’ and ‘both psychological and physical burden’.
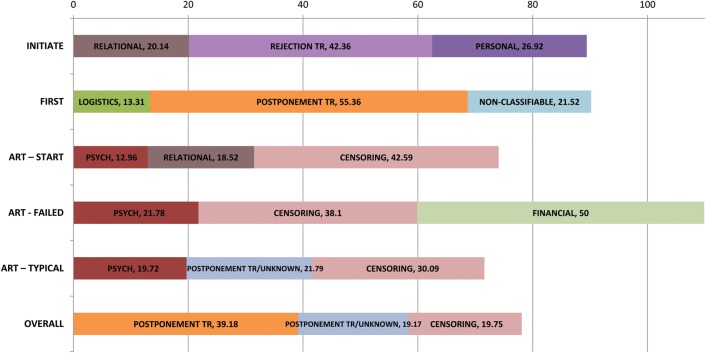
Table III shows the percentage of selections (and 95% CIs) of all the categories of reasons overall and according to each treatment stage. Figure 2 summarizes the percentage of the three most selected reason categories overall and according to each treatment stage. Two studies focused on the period before initiation of fertility treatment (Brandes et al., 2009; Eisenberg et al., 2010). Results show that the five most selected categories were rejection of treatment, personal reasons, relational problems, financial issues and psychological burden of treatment. Five studies focused on first-order treatments (Meijer and Hamerlynck, 1980; Danesh-Meyer et al., 1993; Guerif et al., 2003; Malcolm and Cumming, 2004; Brandes et al., 2009). It was noted that numerous people in the study by Malcom and colleagues (2004) reported to have stopped treatment because they ‘moved away’ (n = 97, 34% of total). If these answers were not considered, the proportion of selections of logistical/practical reasons would be 13.31% (95% CI 9.9–17.62) during first-order treatments and 11.82% (95% 8.92–15.46) overall. Taking this into consideration, results show that discontinuation during this period was mostly due to postponement of treatment, non-classifiable reasons, logistic/practical reasons, doctor censoring and adoption. Only one study focused on the period prior to initiation of ART (van Dongen et al., 2010). The most selected categories in this study were doctor censoring, relational problems, psychological burden of treatment, personal reasons and organizational problems. Three studies focused on discontinuation after the first failed ART cycle (Goldfarb et al., 1997; Meynol et al., 1997; Smeenk et al., 2004). The most selected categories were financial issues, doctor censoring, psychological burden of treatment followed by physical burden of treatment and clinic-related reasons. Finally, six studies focused on typical ART treatment (Smeenk et al., 2004; Pelinck et al., 2007; Verberg et al., 2008; Verhagen et al., 2008; Brandes et al., 2009; Domar et al., 2010). Results show that the most selected categories were doctor censoring, postponement of treatment or unknown, psychological burden of treatment, physical and psychological burden of treatment, postponement of treatment and marital and personal problems. Overall, postponement of treatment, doctor censoring, postponement of treatment or unknown, physical and psychological burden of treatment, marital and personal problems, psychological burden of treatment and rejection of treatment were the most commonly cited reasons for discontinuation.
Table III.
Percentage of selections (%) and lower and upper limits of 95% confidence intervals (LL 95% CI – UP 95% CI) for reasons for treatment discontinuation, per treatment stage and overall.
| Categories of reasons for discontinuation | INITIATE |
FIRST |
ART-START |
ART - FAILED |
ART – TYPICAL |
OVERALL |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | LL 95% CI | UL 95% CI | % | LL 95% CI | UL 95% CI | % | LL 95% CI | UL 95% CI | % | LL 95% CI | UL 95% CI | % | LL 95% CI | UL 95% CI | % | LL 95% CI | UL 95% CI | |
| Treatment | ||||||||||||||||||
| Physical burden of treatments | 0.7 | 0.12 | 2.79 | 17.49 | 12.44 | 23.95 | 3.36 | 1.24 | 8.07 | 6.32 | 4.59 | 8.61 | ||||||
| Psychological burden of treatments | 10.34 | 6.82 | 15.32 | 7.84 | 5.5 | 11 | 12.96 | 5.8 | 25.51 | 21.78 | 16.69 | 27.86 | 19.72 | 15.35 | 24.93 | 14 | 12.11 | 16.13 |
| Physical and psychological burden of treatment | 19.07 | 14.18 | 25.1 | 19.07 | 14.18 | 25.1 | ||||||||||||
| Clinic | ||||||||||||||||||
| Clinic related reasons | 2.81 | 1.31 | 5.67 | 17.48 | 11.84 | 24.92 | 7.71 | 5.44 | 10.76 | |||||||||
| Organizational problems | 5.56 | 1.45 | 16.35 | 13.99 | 8.96 | 21.02 | 11.68 | 7.7 | 17.2 | |||||||||
| Patient | ||||||||||||||||||
| Relational problems | 20.14 | 14.11 | 27.43 | 4.79 | 3.21 | 7.03 | 18.52 | 9.7 | 31.87 | 11.19 | 6.73 | 17.81 | 7.75 | 4.98 | 11.77 | 8.83 | 7.29 | 10.65 |
| Marital and personal problems | 16.67 | 7.51 | 31.96 | 16.67 | 7.51 | 31.96 | ||||||||||||
| Rejection of treatment | 42.36 | 34.26 | 50.87 | 8.89 | 6.25 | 12.44 | 5.95 | 3.16 | 10.67 | 7.88 | 4.94 | 12.22 | 13.23 | 11.15 | 15.62 | |||
| No Faith in treatment success | 2.78 | 0.89 | 7.4 | 2.78 | 1.42 | 5.22 | 5.1 | 1.89 | 12.06 | 3.16 | 1.97 | 4.98 | ||||||
| Perception of poor prognosis | 8.11 | 5.01 | 12.72 | 8.09 | 5.72 | 11.28 | 2.02 | 0.35 | 7.81 | 7.27 | 5.54 | 9.46 | ||||||
| Logistics/practical reasons | 33.33 | 28.88 | 38.09 | 6.02 | 2.24 | 14.11 | 28.83 | 24.95 | 33.04 | |||||||||
| Personal reasons | 26.92 | 17.79 | 38.35 | 5.22 | 3.26 | 8.17 | 11.11 | 4.6 | 23.31 | 9.27 | 6.93 | 12.26 | ||||||
| Adoption | 8.97 | 6.61 | 12.02 | 2.08 | 0.01 | 7.45 | 7.38 | 5.67 | 9.54 | |||||||||
| Other parenting options | 1.05 | 0.27 | 3.3 | 6.76 | 3.47 | 12.41 | 1.05 | 0.27 | 0.33 | |||||||||
| Abandonment of childwish | 2.4 | 1.12 | 4.86 | 4.9 | 2.16 | 10.21 | 3.15 | 1.84 | 5.26 | |||||||||
| Postponement of treatment | 55.36 | 41.56 | 68.43 | 17.07 | 7.69 | 32.64 | 39.18 | 29.58 | 49.65 | |||||||||
| Postponement of treatment or unknown | 14.29 | 5.95 | 29.24 | 21.79 | 13.55 | 32.85 | 19.17 | 12.78 | 27.58 | |||||||||
| External constraints | ||||||||||||||||||
| Doctor censoring | 6.94 | 3.56 | 12.7 | 11.64 | 8.94 | 15 | 42.59 | 29.5 | 56.73 | 38.1 | 23.99 | 54.35 | 30.09 | 25.38 | 35.25 | 19.75 | 17.41 | 22.31 |
| Financial issues | 15.32 | 10.98 | 20.89 | 3.89 | 2.23 | 6.59 | 3.7 | 0.64 | 13.83 | 50 | 34.06 | 65.94 | 3.57 | 1.32 | 8.56 | 9.19 | 7.34 | 11.43 |
| Health problems | 7.64 | 4.07 | 13.58 | 0.65 | 0.03 | 4.11 | 3.38 | 1.49 | 7.13 | 3.76 | 2.34 | 5.92 | ||||||
| Other medical treatment | 3.00 | 1.53 | 5.62 | 3.66 | 0.95 | 11.06 | 8.97 | 3.99 | 18.17 | 4.06 | 2.56 | 6.31 | ||||||
| Non-interpretable | ||||||||||||||||||
| Went to other clinics | 1.05 | 0.27 | 3.3 | 3.7 | 0.64 | 13.83 | 8.39 | 4.61 | 14.51 | 11.41 | 6.98 | 17.9 | 5.39 | 3.82 | 7.53 | |||
| Other/unknown/not reported | 7.64 | 4.07 | 13.58 | 10.68 | 8.27 | 13.66 | 1.85 | 0.1 | 11.18 | 17.57 | 13.61 | 22.34 | 11.86 | 10 | 14 | |||
| Non-classifiable | 21.52 | 13.38 | 32.48 | 2.8 | 0.01 | 7.45 | 9.46 | 6.09 | 14.29 | |||||||||
Note: Blank cells mean that the corresponding reason category was not investigated for the corresponding treatment stage in any study.
INITIATE, during diagnosis, before initiation of treatment; FIRST, during first-order treatments like insemination or ovulation induction; ART-START, on the waiting list to start assisted reproductive techniques; ART-FAILED, after the first failed ART cycle; ART-TYPICAL, before completion of the typical ART regimen.
Figure 2.
Percentage (%) of the three most selected categories of reasons for discontinuation overall and according to each treatment stage. INITIATE = during diagnosis, before initiation of treatment; FIRST = during first-order treatments like insemination or ovulation induction; ART-START = on the waiting list to start assisted reproductive techniques; ART-FAILED = after the first failed ART cycle; ART-TYPICAL = before completion of the typical ART regimen. Relational = relational problems; Rejection tr = rejection of treatment; Personal, personal reasons; Logistics = logistics/practical reasons; Postponement tr = postponement of treatment; Psych = psychological burden of treatment; Censoring = doctor censoring; Financial = financial issues; Postponement tr/unknown = postponement of treatment or unknown.
Treatment, clinic and patient predictors of discontinuation
A total of 14 studies investigated treatment-related predictors of discontinuation. These referred to the patients' infertility history (e.g. infertility duration, previous fertility treatment) and to the fertility treatment being implemented (e.g. hormonal stimulation dosage). No study focused on clinic predictors of discontinuation and 14 studies investigated patient predictors of discontinuation, which could be socio-demographic (e.g. age, education) and/or psychosocial (e.g. anxiety).
Studies varied considerably on the methodology used to investigate predictors. Most studies either investigated group mean or frequency differences between discontinuers and continuers (e.g. t-test, multivariate analysis of variance, χ2 test) and/or tested predictive models of discontinuation (e.g. Pearson-r, linear, Cox or logistic regressions). Studies also varied on the level of detail of results reported, with some only referring to the direction and statistical significance of associations found and others reporting on all statistical tests made. Significant associations found are reported in the text as they were reported in the original publication.
None of the studies reported a priori power in the statistical analysis. Out of 22 studies, 20 had enough power to detect medium effect sizes in mean group differences and correlations (one study did not had enough power and another did not report on the number of continuers, Guerif et al., 2003; Verberg et al., 2008), but only 3 out of 22 studies had enough power to detect small effect sizes (Rufat et al., 1994; Sharma et al., 2002; Pearson et al., 2009).
Tables IV and V summarize associations found between treatment and patient predictors investigated in the included studies and discontinuation, according to different stages of fertility treatment. For each predictor the tables show if associations investigated in each study were statistically significant (or not, NS) and, if so, whether the predictor was associated with higher (+) or lower discontinuation (−). Summaries of the number of studies that investigated each specific predictor and that found that the predictor was associated with higher and lower discontinuation were presented on the right side of the tables. Only statistically significant results found are reported in the text (See Tables 8 and 9 of supplementary material for non statistically significant results).
Table IV.
Treatment predictors of discontinuation.
| INITIATE | FIRST |
ART- FAILED | ART-FAILED and TYPICAL |
ART ALL | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Eisenberg 2010 | Danesh- Meyer 1993 | Guerif 2002 | Guerif 2003 | Steures 2007 | Sharma 2002 | De Vries 1999 | Pearson 2009 | Pelinck 2007 | Roest 1998 | Rufat 1994 | Smeenk 2004 | Verberg 2008 | Verhagen 2008 |
 Nr studies investigating predictor Nr studies investigating predictor |
|
 Nr studies associating predictor with higher discontinuation Nr studies associating predictor with higher discontinuation | |||||||||||||||
 Nr studies associating predictor with lower discontinuation Nr studies associating predictor with lower discontinuation | |||||||||||||||
| Doctor censored patients excluded from analysis | No | No | Yes | Yes | No | No | No | No | No | No | No | Yes | No | No | |
| Predictors | |||||||||||||||
| Infertility history | 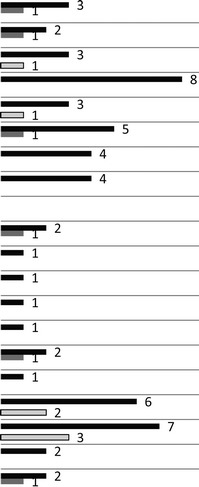 |
||||||||||||||
| Parity | NS | + | NS | ||||||||||||
| Pregnancies prior IVF | + | NS | |||||||||||||
| Previous fertility treatment | − | NS | NS | ||||||||||||
| Infertility duration | NS | NS | NS | NS | NS | NS | NS | NS | |||||||
| Primary infertility | − | NS | NS | ||||||||||||
| Male factor | NS | NS | NS | + | NS | ||||||||||
| Female factor | NS | NS | NS | NS | |||||||||||
| Unexplained/no diagnosis | NS | NS | NS | NS | |||||||||||
| Treatment | |||||||||||||||
| Time to treatment | + | NS | |||||||||||||
| Type of treatment | NS | ||||||||||||||
| Duration of treatment | NS | ||||||||||||||
| Nr visits to physician | NS | ||||||||||||||
| A priory estimated pregnancy rate | NS | ||||||||||||||
| Stimulation dosage | NS | + | |||||||||||||
| Cancelled cycle | NS | ||||||||||||||
| Oocytes retrievals | − | NS | NS | − | NS | NS | |||||||||
| Embryo fertilization, transfers & quality | − | NS | NS | − | NS | − | − | ||||||||
| Use frozen embryos | NS | NS | |||||||||||||
| Pregnancy lost/other comp | +a | NS | |||||||||||||
Note: Blank cells mean that the corresponding predictor was not investigated in the corresponding study; NS = non-significant statistical test; + = predictor associated with higher discontinuation; − = predictor associated with lower discontinuation; amoderation effect of treatment cycle between pregnancy lost/other complications and discontinuation, chemical pregnancy only (versus failed embryo implantation), cycle 1: 1.51 (95% CI 1.04–2.17), P = 0.03, cycle 2: 1.09 (95% CI 0.67–1.76), P = 0.74 and clinical pregnancy loss (versus failed embryo implantation), cycle 1: OR 1.88 (95% CI 1.22–2.90), P < 0.01, cycle 2: 0.95 (95% CI 0.52–1.72), P = 0.86.
INITIATE = during diagnosis, before initiation of treatment; FIRST = during first-order treatments like insemination or ovulation induction; ART-START = on the waiting list to start assisted reproductive techniques; ART-FAILED = after the first failed ART cycle; ART-TYPICAL = before completion of the typical ART regimen.
Table V.
Patient predictors of discontinuation.
| INITIATE | FIRST |
ART-FAILED | ART-FAILED and TYPICAL |
ART ALL | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Eisenberg 2010 | Danesh- Meyer 1993 | Guerif 2002 | Guerif 2003 | Schover 1992 | Sharma 2002 | De Vries 1999 | Pearson 2009 | Pelinck 2007 | Roest 1998 | Rufat 1994 | Smeenk 2004 | Verberg 2008 | Verhagen 2008 |
 Nr studies investigating predictor Nr studies investigating predictor |
|
 Nr studies associating predictor with higher discontinuation Nr studies associating predictor with higher discontinuation | |||||||||||||||
 Nr studies associating predictor with lower discontinuation Nr studies associating predictor with lower discontinuation | |||||||||||||||
| Doctor censored patients excluded from analysis | No | No | Yes | Yes | No | No | No | No | No | No | No | Yes | No | No | |
| Predictors | |||||||||||||||
| Socio-demographic |  |
||||||||||||||
| Age women | + | NS | NS | NS | + | + | + | NS | NS | NS | + | NS | NS | NS | |
| Age men | NS | NS | NS | ||||||||||||
| Education women | − | NS | NS | ||||||||||||
| Education men | NS | NS | |||||||||||||
| Financial issues | NS | NS | NS | NS | |||||||||||
| Distance of residence to clinic | NS | ||||||||||||||
| Ethnicity | NS | ||||||||||||||
| Religion | NS | NS | |||||||||||||
| Psychosocial | |||||||||||||||
| Anxiety women | NS | +a | NSb | ||||||||||||
| Depression women | + | +c | NS | ||||||||||||
| Distress women | NS | ||||||||||||||
| Distress men | NS | ||||||||||||||
| Relational/sexual adjustment woman | − | NS | |||||||||||||
| Relational/sexual adjustment man | NS | ||||||||||||||
Note: Blank cells mean that the corresponding predictor was not investigated in the corresponding study; NS = non-significant statistical test; + = predictor associated with higher discontinuation; − = predictor associated with lower discontinuation; amoderation effect of treatment cycle (first, second) on relationship between pre treatment state anxiety and discontinuation, first cycle: discontinuers: 42.5 ± 14.3, continuers: 36.3 ± 10.0. P < 0.05, second cycle: discontinuers: 38.0 ± 12.4, continuers: 38.6 ± 10.3, NS; bmoderation effect of stimulation dosage on relationship between anxiety and discontinuation: 1.38 conventional, 1.16 mild [relative reduction in hazard 0.84 (95% CI 0.72–0.99)]; cmoderation effect of treatment cycle (first, second) on relationship between pre treatment depression score and discontinuation, first cycle: discontinuers: 9.5 ± 8.7, continuers: 5.8 ± 5.3. P < 0.05, second cycle: discontinuers: 5.3 ± 5.6, continuers: 6.9 ± 6.0, NS.
INITIATE = during diagnosis, before initiation of treatment; FIRST = during first-order treatments like insemination or ovulation induction; ART-START = on the waiting list to start assisted reproductive techniques; ART-FAILED = after the first failed ART cycle; ART-TYPICAL = before completion of the typical ART regimen.
Treatment predictors of discontinuation
Infertility history predictors
Parity was defined as a dichotomous variable (no children or children). From three studies investigating parity, one found that patients with children were more likely to discontinue treatment after the first and second ART-failed cycles than patients without children [OR 1.58 (95% CI 1.18–2.10), P < 0.01 and OR 1.66 (95% CI 1.16–2.37), P < 0.01, Pearson et al., 2009].
From two studies investigating the number of pregnancies prior to treatment, one reported that it was associated with higher discontinuation during typical ART treatment (P < 0.05; De Vries et al., 1999).
Three studies investigated previous fertility treatment and Guerif et al. (2002) found that the mean number of previous first-order cycles done, was associated with lower discontinuation from donor insemination treatment (5.9 ± 3.4 versus 8.0 ± 3.1, P < 0.05).
Three studies investigated primary infertility (versus secondary) and De Vries et al. (1999) found that it was associated with lower discontinuation (P < 0.05).
Finally, five studies investigated if different causes of infertility (e.g. endometriosis, anovulation) predicted discontinuation and one found that severe male infertility (treated with ICSI) was associated with higher discontinuation during typical ART treatment [HR 4.81 (95% CI 1.63–14.14), P= 0.004, Verberg et al., 2008].
Fertility treatment predictors
Two studies investigated time to treatment and Guerif et al. (2003) found that the time interval (in months) between a first and second donor insemination treatment course in patients returning to treatment after successful treatment, was longer for patients who discontinued than for patients who did not (39 ± 18 versus 30 ± 12, P < 0.05).
Two studies investigated hormonal stimulation dosage and one found that patients using a mild stimulation dosage protocol were less likely to discontinue typical ART treatment than patients using a standard stimulation protocol [HR 0.55 (95% CI 0.31–0.96), P = 0.034, Verberg et al., 2008].
Six studies investigated oocyte retrieval, which was assessed according to the number of oocytes available for retrieval (Verberg et al., 2008), number of oocytes retrieved (De Vries et al., 1998; Roest et al., 1998; Sharma et al., 2002), number of retrievals performed (Pelinck et al., 2007), cancelled (De Vries et al., 1998) or successful (Pelinck et al., 2007) and whether retrieval was performed (Pearson et al., 2009). It was found that a smaller number of oocytes retrieved (12.52 ± 11.07 versus 12.99 ± 8.11, P = 0.02, Sharma et al., 2002) and a lower number of retrievals performed (P < 0.05, Pelinck et al., 2007) were reported for discontinuers than for continuers.
Seven studies investigated embryo fertilization, quality and transfer using different assessments. These could be the availability of embryos to transfer (Verberg et al., 2008), the number of embryos transferred (De Vries et al., 1998; Roest et al., 1998; Sharma et al., 2002; Pelinck et al., 2007), fertilization (De Vries et al., 1998; Roest et al., 1998; Sharma et al., 2002; Pelinck et al., 2007) or cleavage rates (Sharma et al., 2002), the quality of the embryos transferred (De Vries et al., 1998) or the failure of fertilization (Pearson et al., 2009) or embryo transfers (Rufat et al., 1994). One study showed that the absence of embryo transfers was positively associated with discontinuation after a first (discontinuers: 34%, continuers: 26%, P < 0.05) and second ART-failed cycle (33% discontinuers, 24% continuers, P< 0.04, Rufat et al., 1994). Another study reported that patients who transferred more than two embryos were less likely to discontinue after the first ART cycle (71 continuers versus 52 discontinuers, P < 0.0001, Sharma et al., 2002). Two other studies reported that the availability of an embryo for transfer [OR 0.41 (95% CI 0.24–0.72), P = 0.002,Verhagen et al., 2008] and the percentage of embryo transfers per cycle (P < 0.05) and of fertilizations per successful oocyte retrieval (P < 0.05, Pelinck et al., 2007) were negatively associated with discontinuation from typical ART.
Finally, two studies investigated pregnancy losses and other complications and one reported that patients who experienced a chemical and clinical pregnancy loss (versus failed embryo implantation) were more likely to discontinue after a first failed ART cycle [OR 1.51 (95% CI 1.04–2.17), P = 0.03 and OR 1.88 (95% CI 1.22–2.90), P < 0.01, Pearson et al., 2009].
Patient predictors of discontinuation
Socio-demographic predictors
Age of women was positively associated with discontinuation in a total of 5 studies out of 14. These five studies referred to discontinuation before initiation of treatment [OR 1.77 (95% CI 1.11–2.82), P = 0.02, Eisenberg et al., 2010], during first-order treatment [discontinuers: 34, continuers: 29, t(50) = −3.18, P < 0.003, Schover et al., 1992] and during typical ART treatment (cycle 1: discontinuers: 32.0 ± 5.5, continuers: 31.0 ± 4.3, P < 0.05, cycle 2: discontinuers: 32.0 ± 4.7, continuers: 31.6 ± 4.3, P > 0.05, De Vries et al., 1999, cycle 1: discontinuers: 33.2 ± 4.9, continuers: 32.5 ± 4.6, t= 6.4, P < 0.001, cycle 2: discontinuers: 33.5 ± 4.8, continuers: 32.9 ± 4.4, t = 3.9, P < 0.05, Rufat et al., 1994, discontinuers: 32.91 ± 4.84, continuers: 32.31 ± 4.04, P = 0.017, Sharma et al., 2002).
Three studies investigated the women's education level and one found that it was negatively associated with discontinuation before the initiation of treatment [some college education versus college degree, OR 0.21 (95% CI 0.10–0.45), P < 0.001, Eisenberg et al., 2010].
Psychosocial predictors
Three studies investigated anxiety and depression in women. In one study anxiety and depression were assessed prior to the start of an ART cycle with the State-Trait Anxiety Inventory (Spielberger et al., 1970) and the Beck Depression Inventory (Beck and Beamesderfer, 1976) and were found to be associated with higher discontinuation after the first failed ART cycle (discontinuers: 42.5 ± 14.3, continuers: 36.3 ± 10.0, P < 0.05, Smeenk et al., 2004). Another study found that depression, assessed with the Center for Epidemological Studies Depression Scale (Radloff, 1977), was associated with higher discontinuation before the initiation of fertility treatment (Eisenberg et al., 2010).
Finally, two studies investigated relational and sexual adjustment in women and one found that women with higher marital adjustment before starting first-order treatments, assessed with the dyadic adjustment scale (Spanier, 1976), were less likely to discontinue [t(49) = −2.72, P < 0.01, Schover et al., 1992].
Discussion
Postponement of treatment, physical and psychological burden and relational and personal problems were the most frequently selected reasons for discontinuing treatment, followed by clinic/organizational problems, rejection of treatment and logistical and practical reasons. Reasons varied across the stages of treatment. Some reasons were common across stages [e.g. psychological burden, postponement of treatment (when assessed), doctor censoring] whilst others were dominant to a particular stage (e.g. rejection of treatment at initiation; financial issues and relational problems at treatment initiation and after a failed ART cycle). None of the predictors (treatment, clinic, patient) explained discontinuation in longitudinal research. This may be because the predictors investigated generally did not measure the factors patients identified as most important for their decision about discontinuation and reflects that our knowledge about causes of discontinuation from fertility treatment is still limited. Much research is required to explain discontinuation and this could be achieved by conducting theory led research with longitudinal designs that allow causal inferences to be made.
The literature review showed that although there is more than 20 years of research on discontinuation from fertility treatment, many studies did not address why patients discontinued treatment (<60% of papers investigating discontinuation, see Fig. 1). The few that did focus on the ‘why’ ignored the available compliance and decision-making theories that could provide a theoretical framework for their work (e.g. WHO, 2003; Durand et al., 2008). Instead, researchers have been basing their studies on an arbitrary set of reason descriptors (see Table II) that do not seem to have been validated in prior qualitative or modelling research (Campbell et al., 2000) and/or do not match theoretical constructs that are known to be associated with decision-making (e.g. attitudes towards the behaviour, Ajzen and Fishbein, 1980). As a result the descriptors presented in the studies were vague (e.g. ‘psychological reasons’), ambiguous (e.g. ‘personal’) and/or had substantial conceptual overlap (e.g. ‘psychological and physical burden’, ‘postponement or unknown’) that could cause confusion in interpretation. In addition, descriptors did not seem to capture all possible reasons for discontinuation, as categories allowing for idiosyncratic reasons (i.e. ‘personal reasons’, ‘other/unknown/not reported’) were frequently selected. This atheoretical approach was also reflected in the longitudinal research on predictors of discontinuation. The majority of studies adopted a medical perspective of discontinuation exploring predictors such as infertility duration (8 studies), age (15 studies) or poor prognosis indicators (e.g. embryo fertilization outcomes, 7 studies). In contrast, causes stated by patients, such as psychological distress, were much less frequently investigated (e.g. anxiety, three studies) as predictors. Similarly, clinic predictors were never considered despite studies showing that clinic related reasons (17.48%) and organizational problems (13.99%) were some of the most selected reasons for discontinuation after the first failed ART cycle. The lack of concordance observed between research focusing on reasons and that focusing on predictors suggests a need for greater coherence (and consensus) in the field about how to address discontinuation. It is important to recognize that compliance (as opposed to discontinuation) is the single most important modifiable factor that compromises treatment outcome in many health contexts (WHO, 2003), yet fundamental knowledge about compliance with fertility treatment is still lacking.
In an integrated approach to fertility care, Boivin et al. (2012) proposed that discontinuation in ART can only be fully addressed if fertility clinics tackle its causes where and when they arise: patients, clinics and/or in the treatment domain at any stage of the treatment trajectory. In the present study it was shown that barriers to uptake of [further] treatment differed across these domains and also treatment stages. Some barriers were common to all stages of treatment (from diagnostic evaluation to ART) whilst others were stage-specific.
Psychological burden of treatment was a main reason for discontinuing treatment at all stages, especially during ART. Psychological distress is known to vary according to the demands of infertility and its treatment (physical, logistic, financial, etc.) as well as according to cognitions and personal beliefs regarding parenthood and childlessness (Verhaak et al., 2007; Moura-Ramos et al., 2011), two factors that become more prominent as patients progress through treatment stages, undergo more demanding medical procedures and increasingly face the possibility of definitive treatment failure. It is assumed that the patient has to adapt to treatment and not the opposite. Thus, there is a vast literature on interventions to help couples cope with the psychological burden of ART treatment (cf. Boivin, 2003; Hämmerli et al., 2009) and much less on interventions to diminish burden, which need to be developed and validated (Boivin et al., 2012). Patients report that the shock of treatment failure demands some processing time before they feel able to discuss further uptake of treatment (Peddie et al., 2005), which is consistent with results of quantitative studies that show that the aftermath of treatment failure is marked by intense depressive emotions (Verhaak et al., 2005). Further, the necessity to decide about whether to undergo more treatment is in itself distressing for couples (Peddie et al., 2005) and better decisional support should be provided. Indeed, quantitative and qualitative research has shown that few patients are given the opportunity to discuss the advantages and disadvantages of ending treatment (24 and 18%, respectively, Peddie et al., 2004), that patients report a sense of being ill-prepared for deciding about treatment uptake and feel that an appointment to discuss this issue would be useful (Peddie et al., 2005; Boden, 2007). Nonetheless, only 22% of patients found that counsellors were helpful when they were deciding whether to stop treatment (Hammarberg et al., 2001). The emotional distress caused by the treatment failure and the necessity to choose about future treatment can also explain why patients report postponement of treatment as the most frequent reason for discontinuation. Indeed, more than delaying their decision, patients may be avoiding it to manage or prevent negative emotional reactions (Anderson, 2003). If indeed discontinuation were a reflection of decision avoidance, it would be helpful if fertility staff could contact couples after an adequate period of time with the aim of prompting patients for decision-making regarding compliance. Such contact should also serve the goal of empowering patients to make the decision through the provision of adequate information and decisional support (Spranca, 2001). The high number of people using other methods to achieve parenthood (e.g. adoption) also suggests the need to discuss these alternative paths. Clinics could also offer brochures with typical issues and decisions that couples are likely to face during their treatment pathway.
Physical burden of treatment was negligible during first-order treatments but was the second most frequent reason for discontinuation after the first failed ART cycle. Its relative importance to explain discontinuation in the midst of the typical ART regimen (i.e. within first three cycles) is difficult to assess because many studies did not differentiate it from the psychological burden of treatment. Data from this systematic review suggests that patients attribute more weight to the psychologically onerous aspects of treatment than the physical aspects, a result that is consistent with past prospective research showing that anxiety (i.e. feeling tense, nervous, anxious, worried) was significantly higher during the last 7 days of the waiting period that during the preceding last 7 days of stimulation (Boivin and Lancastle, 2010). Nevertheless, how the psychological and physical onerous aspects of treatment affect discontinuation needs to be better clarified through a clear differentiation between the two. A detailed inspection of the reason descriptors under the ‘physical burden’ category showed that patients cited oocyte retrieval being too painful followed by the side effects from medication and/or treatment as reasons for discontinuation (Table II). Qualitative research has also shown that patients consider that adequate pain medication during oocyte retrieval can increase their physical comfort (Dancet et al., 2011).
Relational problems seem to interfere more with uptake of new types of treatments than with continued uptake of the same treatment (Table III). Such moments, when the two members of the couple consider treatment in light of their individual values, interests and preferences, may trigger intra-couple strain and exacerbate coping gender differences, as women are known to worry more about treatment, to plan more in advance in case of failure, and to be generally more proactive and willing to undergo treatment than men (Jordan and Revenson, 1999; Merari et al., 2002). The descriptors under the ‘relational problems’ and ‘marital and personal problems’ categories are too vague to inform possible compliance interventions and more work is needed in this area. Meanwhile, for those couples requesting decisional aid, the support provided should integrate life and relationship values clarification techniques. These would meet patients' expressed desire for clinics to fully involve their partner in the treatment process (Dancet et al., 2010) and could be helpful for couples to identify shared values and discuss perceived barriers to action, such as fear of partner rejection and relational insecurities (Peterson et al., 2009). For instance, a study showed that couples who felt their relationship could be threatened by a lack of children were more likely to continue with treatment (Strauss et al., 1998).
Personal reasons were also highly cited by patients, especially at the start of treatment, pointing for idiosyncratic reasons for discontinuation (i.e. moving, death in family, return to school). However, the only study that considered this category at this stage (Eisenberg et al., 2010) did not include patient related reasons other than poor prognosis, so selections may reflect a wide range of motives. Because the only study that assesses personal reasons during typical ART (Pelinck et al., 2007) does not differentiate them from marital problems (‘marital and personal problems’ category), it remains unclear to what degree idiosyncratic motives interfere with compliance. In general, such idiosyncratic reasons are not the subject of clinical interference of discussion. What is important is that researchers are able to offer a clear and exhaustive description of all reasons behind discontinuation that should indeed be the target of clinic interventions.
Results suggest that patients who choose not to undertake any fertility treatment tend to do so because of moral/ethical objections and/or fear of negative health effects of treatment. If people reject treatment for moral or ethical reasons, then this is a value-based decision that should be respected. However, if rejection is based on fears that are not justified (e.g. health of the baby), then misconceptions need to be addressed prior to the start of treatment so that couples can make well informed decisions (Boivin et al., 2012). Additionally, at this moment couples could also be provided with precise descriptions of what treatment procedures entail (e.g. number and schedule of visits to the clinic), so that they could organize their routines in advance to minimize the impact of treatment on their personal, professional and social lives. For instance, undergoing a single IVF cycle can force women to be absent from work from 24 to 75 h on average, depending on how distant the fertility clinic is (Kelly et al., 2006). Providing preparatory information implies extra organizational efforts from the clinics but could help decrease discontinuation due to organizational problems and logistical and practical reasons, which were also common reasons for discontinuation. Previous research has already demonstrated that preparatory information contributes to decreased fertility-related concerns and increases compliance with clinic appointments during workup (e.g. Pook and Krause, 2005).
Financial issues were only reported in studies from Canada and North America (Goldfarb et al., 1997; Malcolm and Cumming, 2004; Eisenberg et al., 2010) where fertility care is not (or was not) covered by the National Health Systems. These results indicate that financial issues can be an important barrier to compliance decision-making in fertility treatment and that there is still worldwide inequality in the costs of fertility treatment (Nachtigall, 2006).
Data on treatment, clinic and patient predictors of discontinuation are mainly inconclusive. Although multiple studies report on significant associations between a few predictors (e.g. age, oocytes retrieval, embryo fertilization, transfers and quality) and discontinuation that consistently show the same direction of association, these represent less than half of the studies investigating each particular predictor. Possible reasons for inconsistency in results are: low power to detect significant associations, differences in the study populations and in the definition of the discontinuers group. Sample size in most studies only allowed for the detection of medium effect sizes, which means that weak associations between the predictors investigated and discontinuation may not have been detected (Cohen, 1992). Considering that the majority of the studies investigated treatment predictors of discontinuation, the heterogeneity in study population and discontinuers definition, and thus in the prognosis status of different patients groups, may have contributed to inconsistency. However, a closer analysis of results, considering only studies that focused on the general population that undergoes fertility treatment and excluding doctor censored patients from the discontinuers group, did not provide a clearer picture. It may also be that some predictors only operate in an additive way. For instance, Peronace et al. (2006) showed that discontinuers from ART treatment were characterized by having both less previous experience with first-order treatments (e.g. intrauterine insemination) and high social network antipathy to treatment, which could make them more wary to engage in IVF.
In the future, researchers should strive to reach greater precision in the identification of barriers to compliance decision-making. In order to do so, researchers need to ground their studies on decision-making and compliance theory and conduct longitudinal research that attributes equal emphasis to the investigation of treatment, clinic and patient predictors of discontinuation, as proposed in the integrated approach to fertility care (Boivin et al., 2012). There is already a vast literature about compliance in medical health settings that could be helpful to advance research in the fertility specific context (WHO, 2003). In addition, there are many decision-making theories that could be used to frame research. For instance, the Theory of Planned Behaviour (Ajzen and Fishbein, 1980) would be useful to understand how patients attitudes, perceptions of significant others or barriers (e.g. costs) affect their compliance behaviour. The Conflict Model of Decision-Making (Janis and Mann, 1977), which predicts that decisions often entail conflict between the desire to act in order to avoid immediate distress (e.g. current emotional demands of treatment) and the worry that hasty decisions will result in regret (e.g. ‘what if’ next treatment was successful), would help us to understand the decision-making process in itself and to differentiate between desired and undesired discontinuation, that is, between those discontinuation decisions that are value-based and satisfying for patients and those that are not. This information is crucial to ensure that compliance interventions are useful and decisions are indeed made free of barriers. The Rational–Emotional Theory of decisional avoidance may explain why some people intend to undergo [further] treatment but never do (Anderson, 2003). Finally, consensus must be reached about what is discontinuation (e.g. doctored censored patients should not be considered discontinuers) and how does it differ from other phenomenon, such as clinic surfing, that reflect different problems in fertility care that also need further investigation.
Strengths and limitations
This is the first systematic review to synthesize more than 20 years of research on discontinuation. Seven databases were searched yielding 22 papers from eight countries representing the discontinuation decisions of 21 453 patients. Data were independently extracted and quality evaluations were made in accordance with standard protocols for all studies. Data on reasons and predictors of discontinuation were organized according to treatment stages, when patients make important decisions about opting in or out of (further) fertility treatment. Reason descriptors presented in the studies were independently matched to different categories with high agreement between coders. The research on what the systematic review was based on was of average to high quality. Despite these strengths, several limitations of the reviewed literature exist: reason descriptors were vague and insufficient to capture all reasons for discontinuation, research on predictors of discontinuation was of low power and neglected patient and clinic predictors and studies varied on how they defined the group of patients considered to have discontinued treatment. Although these limitations need to be acknowledged, the results presented are in line with the only longitudinal cohort study that investigated reasons at different treatment stages taking into consideration these issues (Brandes et al., 2009), thus reinforcing that this systematic review presents a reliable overview of the current best available evidence about discontinuation from fertility treatment.
Conclusions
Discontinuation is a primary determinant of the effectiveness of treatment because it attenuates optimum clinical benefit (WHO, 2003). The NICE guidelines in the UK recommended that compliance should be monitored for audit purposes and to provide recommendations for care implementation (National Institute for Clinical Excellence (NICE), 2004). This review documents more than 20 years of research on discontinuation from fertility treatment. It shows that patients discontinue treatment because they choose to postpone it, due to its physical and psychological burden, to relational and personal problems, to moral/ethical objections and/or fear of negative health effects of treatment and organizational and clinic problems. For maximum impact, interventions to reduce burden should be directed at discontinuation causes that are common across treatment stages and/or are stage unique but endorsed by many people. Clinics could organize treatments so that burden is diminished as much as possible and ensure that patients receive support to meet the demands of treatment. Clinics could also ensure that couples receive all the necessary treatment-related information and that they have the opportunity to discuss their values, express their concerns and have their treatment misconceptions addressed. Finally, clinics need to ensure that all patients recommended to do (more) treatment receive the adequate decisional support to decide about whether to follow or not medical recommendations. Much research is required to explain discontinuation and this could be achieved by conducting theory led research with designs that allow causal inferences to be made and by attributing equal emphasis to treatment, clinic- and patient-related factors.
Supplementary data
Supplementary data are available at http://humupd.oxfordjournals.org/.
Authors' roles
S.G. did data extraction, critical appraisal, data analysis and interpretation and writing of the report. J.B., L.P. and C.M.V. did critical appraisal, data interpretation and writing of the report. All authors approved the final version for submission.
Funding
S.G. holds a postdoctoral fellowship from the Portuguese Foundation for Science and Technology (FCT-SFRH/BPD/63063/2009). Merck Serono SA, Switzerland sponsored the systematic literature search that was performed by Sure Support Unit for Research Evidence, Cardiff University and the second coding of articles that was performed by Debbie Moss (DM), Caudex Medical. Merck Serono SA performed a scientific review of the publication but the views and opinions described in the publication do not necessarily reflect those of Merck Serono SA.
Conflict of interest
L.P. currently works for Merck Serono, the company that partially funded this systematic review.
Supplementary Material
References
- Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behaviour. Englewood Cliffs, NJ: Prentice-Hall; 1980. doi:10.1111/j.1365-2044.1949.tb05837.x. [Google Scholar]
- Akyuz A, Sever N. Reasons for infertile couples to discontinue in vitro fertilization (IVF) treatment. J Reprod Infant Psychol. 2009;27:258–268. doi:10.1056/NEJM197710202971601. [Google Scholar]
- Anderson CJ. The psychology of doing nothing: forms of decision avoidance results from reason and emotion. Psychol Bull. 2003;129:139–167. doi: 10.1037/0033-2909.129.1.139. doi:10.1213/01/ane.0000309024.28586.70. [DOI] [PubMed] [Google Scholar]
- Beck AT, Beamesderfer A. Assessment of depression: the depression inventory. Pharmacopsychiatria. 1976;7:151–169. doi: 10.1159/000395074. doi:10.1378/chest.104.3.701. [DOI] [PubMed] [Google Scholar]
- Boden J. When IVF treatment fails. Hum Fertil. 2007;10:93–98. doi: 10.1080/14647270601142614. [DOI] [PubMed] [Google Scholar]
- Boivin J. A review of psychosocial interventions in infertility. Soc Sci Med. 2003;57:2325–2341. doi: 10.1016/s0277-9536(03)00138-2. doi:10.1097/SLA.0b013e3181cf811d. [DOI] [PubMed] [Google Scholar]
- Boivin J, Lancastle D. Medical waiting periods: imminence, emotions and coping. Womens Health. 2010;6:59–69. doi: 10.2217/whe.09.79. doi:10.1002/bjs.5734. [DOI] [PubMed] [Google Scholar]
- Boivin J, Bunting L, Collins JA, Nygren KG. International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod. 2007;22:1506–1512. doi: 10.1093/humrep/dem046. doi:10.1111/j.1365-2044.2009.06063.x. [DOI] [PubMed] [Google Scholar]
- Boivin J, Domar AD, Shapiro DB, Wischmann T, Fauser BC, Verhaak CM. Tackling burden in ART: an integrated approach for medical staff. Hum Reprod. 2012;27:941–950. doi: 10.1093/humrep/der467. doi:10.1093/bja/aeq128. [DOI] [PubMed] [Google Scholar]
- Brandes M, van der Steen JOM, Bokdam SB, Hamilton CJCM, de Bruin JP, Nelen WLDM, Kremer JAM. When and why do subfertile couples discontinue their fertility care? A longitudinal cohort study in a secondary care subfertility population. Hum Reprod. 2009;24:3127–3134. doi: 10.1093/humrep/dep340. [DOI] [PubMed] [Google Scholar]
- Brandes M, Hamilton CJCM, De Bruin JP, Nelen WLDM, Kremer JAM. The relative contribution of IVF to the total ongoing pregnancy rate in a subfertile cohort. Hum Reprod. 2010;25:118–126. doi: 10.1093/humrep/dep341. [DOI] [PubMed] [Google Scholar]
- Callan VJ, Kloske B, Kashima Y, Hennessey JF. Toward understanding women's decisions to continue or stop in vitro fertilization: The role of social, psychological, and background factors. J Vitro Fert Embryo Transf. 1988;5:363–369. doi: 10.1007/BF01129572. [DOI] [PubMed] [Google Scholar]
- Campbell M, Firtzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, Tyrer P. Framework for design and evaluation of complex interventions to improve health. Br Med J. 2000;321:694–696. doi: 10.1136/bmj.321.7262.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. doi:10.1111/j.0006-341X.2000.00256.x. [DOI] [PubMed] [Google Scholar]
- Dancet EAF, Nelen WLDM, Sermeus W, De Leeuw L, Kremer JAM, D'Hooghe TM. The patients' perspective on fertility care: a systematic review. Hum Reprod Update. 2010;16:467–487. doi: 10.1093/humupd/dmq004. doi:10.1214/ss/1009212519. [DOI] [PubMed] [Google Scholar]
- Dancet EAF, van Empel IWH, Rober P, Nelen WLDM, Kremer JAM, D'Hooghe T. Patient-centred infertility care: a qualitative study to listen to the patient's voice. Hum Reprod. 2011;26:827–833. doi: 10.1093/humrep/der022. doi:10.1111/1467-9876.00082. [DOI] [PubMed] [Google Scholar]
- Danesh-Meyer HV, Gillett WR, Daniels KR. Withdrawal from a donor insemination programme. Aust N Z J Obstet Gynaecol. 1993;33:187–190. doi: 10.1111/j.1479-828x.1993.tb02390.x. [DOI] [PubMed] [Google Scholar]
- De Vries MJ, De Sutter P, Dhont M. Prognostic factors in patients continuing IVF treatment and dropouts. Hum Reprod. 1998;13:S54. doi: 10.1016/s0015-0282(99)00334-9. doi:10.2307/2983440. [DOI] [PubMed] [Google Scholar]
- De Vries MJ, De Sutter P, Dhont M. Prognostic factors in patients continuing in vitro fertilization or intracytoplasmic sperm injection treatment and dropouts. Fertil Steril. 1999;72:674–678. doi: 10.1016/s0015-0282(99)00334-9. [DOI] [PubMed] [Google Scholar]
- Domar AD, Smith K, Conboy L, Iannone M, Alper M. A prospective investigation into the reasons why insured United States patients drop out of in vitro fertilization treatment. Fertil Steril. 2010;94:1457–1459. doi: 10.1016/j.fertnstert.2009.06.020. [DOI] [PubMed] [Google Scholar]
- Durand M-A, Stiel M, Boivin J, Elwyn G. Where is the theory? Evaluating the theoretical frameworks described in decision support technologies. Patient Educ Couns. 2008;71:125–135. doi: 10.1016/j.pec.2007.12.004. doi:10.1214/aos/1176344136. [DOI] [PubMed] [Google Scholar]
- Eisenberg ML, Smith JF, Millstein SG, Nachtigall RD, Adler NE, Pasch LA, Katz PP. Predictors of not pursuing infertility treatment after an infertility diagnosis: examination of a prospective U.S. cohort. Fertil Steril. 2010;94:2369–2371. doi: 10.1016/j.fertnstert.2010.03.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. doi:10.1056/NEJMcp002842. [DOI] [PubMed] [Google Scholar]
- Goldfarb J, Austin C, Lisbona H, Loret de Mola R, Peskin B, Stewart S. Factors influencing patients' decision not to repeat IVF. J Assist Reprod Genet. 1997;14:381–384. doi: 10.1007/BF02766144. doi:10.1378/chest.104.3.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerif F, Fourquet F, Marret H, Saussereau M-H, Barthelemy C, Lecomte C, Lecomte P, Lansac J, Royere D. Cohort follow-up of couples with primary infertiilty in an ART programme using frozen donor semen. Hum Reprod. 2002;17:1525–1531. doi: 10.1093/humrep/17.6.1525. [DOI] [PubMed] [Google Scholar]
- Guerif F, Saussereau M-H, Barthelemy C, Lanoue M, Lecomte C, Ract V, Lansac J, Royere D. Achievement of second parenthood in an ART programme using frozen donor semen: cohort follow-up. Hum Reprod. 2003;18:1853–1857. doi: 10.1093/humrep/deg380. doi:10.1093/bja/aeq207. [DOI] [PubMed] [Google Scholar]
- Hammarberg K, Astbury J, Baker HWG. Women's experience of IVF: a follow-up study. Hum Reprod. 2001;16:374–383. doi: 10.1093/humrep/16.2.374. [DOI] [PubMed] [Google Scholar]
- Hämmerli K, Znoj H, Barth J. The efficacy of psychological interventions for infertile patients: a meta-analysis examining mental health and pregnancy rate. Hum Reprod Update. 2009;15:279–295. doi: 10.1093/humupd/dmp002. [DOI] [PubMed] [Google Scholar]
- Janis IL, Mann L. Decision-Making: A Psychological Analysis of Conflict, Choice and Commitment. New York: Free Press; 1977. [Google Scholar]
- Jordan C, Revenson TA. Gender differences in coping with infertility: a meta analysis. J Behav Med. 1999;22:341–358. doi: 10.1023/a:1018774019232. [DOI] [PubMed] [Google Scholar]
- Kelly J, Hughes C, Harrison RF. The hidden costs of IVF. Ir Med J. 2006;99:142–143. [PubMed] [Google Scholar]
- Land JA, Courtar DA, Evers JL. Patients dropout in an assisted reproductive technology program: implications for pregnancy rates. Fertil Steril. 1997;68:278–281. doi: 10.1016/s0015-0282(97)81515-4. [DOI] [PubMed] [Google Scholar]
- Malcolm CE, Cumming DC. Follow-up of infertile couples who dropped out of a specialist fertiliy clinic. Fertil Steril. 2004;81:269–270. doi: 10.1016/j.fertnstert.2003.03.003. [DOI] [PubMed] [Google Scholar]
- Meijer AM, Hamerlynck JVTH. De behandelingsresultaten van donorinseminatie. Ned T Geneesk. 1980;124:587–592. [PubMed] [Google Scholar]
- Merari D, Chetrit A, Modan B. Emotional reactions and attitudes prior to In Vitro Fertilization: an inter-spouse study. Psychol Health. 2002;17:629–640. [Google Scholar]
- Meynol F, Bongain A, Isnard V, Gillet J-Y. Abandon de la FIV après une seule tentative. J Gynecol Obstet Biol Reprod. 1997;26:136–138. [PubMed] [Google Scholar]
- Moura-Ramos M, Gameiro S, Canavarro MC, Soares I. Assessing infertility stress: re-examining the factor structure of the Fertility Problem Inventory. Hum Reprod. 2011;27:496–505. doi: 10.1093/humrep/der388. [DOI] [PubMed] [Google Scholar]
- Nachtigall RD. International disparities in access to infertility services. Fertil Steril. 2006;85:871–875. doi: 10.1016/j.fertnstert.2005.08.066. [DOI] [PubMed] [Google Scholar]
- National Institute for Clinical Excellence (NICE) Fertility: Assessment and Treatment for People with Fertility Problems. London: NICE; 2004. [Google Scholar]
- Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 1998;17:857–872. doi: 10.1002/(sici)1097-0258(19980430)17:8<857::aid-sim777>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- Olivious C, Friden B, Borg G, Bergh C. Why do couples discontinue in vitro fertilization treatment? A cohort study. Fertil Steril. 2004;81:258–260. doi: 10.1016/j.fertnstert.2003.06.029. [DOI] [PubMed] [Google Scholar]
- Pearson KR, Hauser R, Cramer DW, Missmer SA. Point of failure as a predictor of in vitro fertilization treatment discontinuation. Fertil Steril. 2009;91:1483–1485. doi: 10.1016/j.fertnstert.2008.07.1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peddie VL, van Teijlingen E, Bhattacharya S. Ending in-vitro fertilization: women's perception's of decision making. Hum Fertil. 2004;7:31–37. doi: 10.1080/1464727042000198069. [DOI] [PubMed] [Google Scholar]
- Peddie VL, van Teijlingen E, Bhattacharya S. A qualitative study of women's decision-making at the end of IVF treatment. Hum Reprod. 2005;20:1944–1951. doi: 10.1093/humrep/deh857. [DOI] [PubMed] [Google Scholar]
- Pelinck MJ, Vogel NEA, Arts EGJM, Simons AHM, Heineman MJ, Hoek A. Cumulative pregnancy rates after a maximum of nine cycles of modified natural cycle IVF and analysis of patient drop-out: a cohort study. Hum Reprod. 2007;22:2463–2470. doi: 10.1093/humrep/dem164. [DOI] [PubMed] [Google Scholar]
- Peronace LA, Boivin J, Schmidt L. Psychological predictors of treatment dropout at five years follow-up. Fertil Steril. 2006;86:S176–S277. [Google Scholar]
- Peterson BD, Eifert GH, Feingold T, Davidson S. Using acceptance and commitment therapy to treat distressed couples: a case study with two couples. Cogn Behav Practive. 2009;16:430–442. [Google Scholar]
- Pinborg A, Hougaard CO, Andersen AN, Molbo D, Schmidt L. Prospective longitudinal cohort study on comulative 5-year delivery and adoption rates among 1338 couples initiating infertility treatment. Hum Reprod. 2009;24:991–999. doi: 10.1093/humrep/den463. [DOI] [PubMed] [Google Scholar]
- Pook M, Krause W. Stress reduction in male infertility patients: a randomized, controlled trial. Fertil Steril. 2005;83:68–73. doi: 10.1016/j.fertnstert.2004.06.053. [DOI] [PubMed] [Google Scholar]
- Radloff L. The CED-D scale: a self report depression scale for research in general population. Appl Psychol Measure. 1977;1:385–401. [Google Scholar]
- Roest J, van Heusden AM, Zeilmaker GH, Verhoeff A. Cumulative pregnancy rates and selective drop-out of patients in in-vitro fertilization treatment. Hum Reprod. 1998;13:339–341. doi: 10.1093/humrep/13.2.339. [DOI] [PubMed] [Google Scholar]
- Rufat P, Roulier R, Belaisch-Allart J, Bachelot A, de Mouzon J. Évolutions des critères pronostiques de fécondation in vitro selon le rang de la tentative. Contracept Fertil Sex. 1994;22:282–286. [PubMed] [Google Scholar]
- Schover LR, Collins RL, Richards S. Psychological aspects of donor insemination: evaliation and follow up of recipient couples. Fertil Steril, 1992;57:583–590. doi: 10.1016/s0015-0282(16)54904-8. [DOI] [PubMed] [Google Scholar]
- Sharma V, Allgar V, Rajkhowa M. Factors influencing the cumulative conception rate and discontinuation of in vitro fertilization treatment for infertility. Fertil Steril. 2002;78:40–46. doi: 10.1016/s0015-0282(02)03160-6. [DOI] [PubMed] [Google Scholar]
- Smeenk JM, Verhaak CM, Stolwijk AM, Kremer JM, Braat DM. Reasons for dropout in an in vitro fertilization/intracytoplasmic sperm injection program. Fertil Steril. 2004;81:262–268. doi: 10.1016/j.fertnstert.2003.09.027. [DOI] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and other dyads. J Marriage Family. 1976;38:15–28. [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. Test Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- Spranca MD. Designing websites to empower health care consumers. In: Weber E, Baron J, Loomes G, editors. Conflict and Tradeoffs in Decision Making. New York: Cambridge University Press; 2001. [Google Scholar]
- Steures P, Custers IM, van der Steeg JW, Tonch N, van Wely M, van der Veen F, Mol BWJ. Is the a priori prognosis from couples dropping out of an IUI programme different from couples continuing IUI? Hum Reprod. 2007;22:366. [Google Scholar]
- Strauss B, Hepp U, Staeding G, Mettler L. Psychological characeristics of infertile couples: Can they predict pregnancy and treatment persistence? J Commun Appl Soc Psychol. 1998;8:289–301. [Google Scholar]
- Van den Broeck U, Holvoet L, Enzlin P, Bakelants E, Demyttenaere K, D'Hooghe T. Reasons for dropout in infertility treatment. Gynecol Obstet Invest. 2009;68:58–64. doi: 10.1159/000214839. [DOI] [PubMed] [Google Scholar]
- van Dongen AJCN, Verhagen TEM, Dumoulin JCM, Land JA, Evers JLH. Reasons for dropping out from a waiting list for in vitro fertilization. Fertil Steril. 2010;94:1713–1716. doi: 10.1016/j.fertnstert.2009.08.066. [DOI] [PubMed] [Google Scholar]
- Verberg MFG, Eijkemans MJC, Heijnen EMEW, Broekmans FJ, de Klerk C, Fauser BCJM, Macklon NS. Why do couples drop-out from IVF treatment? A prospective cohort study. Hum Reprod. 2008;23:2050–2055. doi: 10.1093/humrep/den219. [DOI] [PubMed] [Google Scholar]
- Verhaak CM, Smeenk JM, van Minnen A, Kremer JM, Kraaimaat FW. Predicting emotional response to unsucessful fertility treatment: a prospective study. J Behav Med. 2005;28:181–190. doi: 10.1007/s10865-005-3667-0. [DOI] [PubMed] [Google Scholar]
- Verhaak CM, Smeenk JM, Evers AWM, Kremer JM, Kraaimaat FW, Braat DM. Women's emotional adjustment to IVF: A systematic review of 25 years of research. Hum Reprod Update. 2007;13:27–36. doi: 10.1093/humupd/dml040. [DOI] [PubMed] [Google Scholar]
- Verhagen TEM, Dumoulin JCM, Evers JLH, Land JA. What is the most accurate estimate of pregnancy rates in IVF dropouts? Hum Reprod. 2008;23:1793–1799. doi: 10.1093/humrep/den209. [DOI] [PubMed] [Google Scholar]
- Wells G, Shea B, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analyses. Ottawa, Canada: The Ottawa Health Research Institute; 2010. [Google Scholar]
- WHO. Adherence to Long-Term Therapies: Evidence for Action. Geneva, Switzerland: World Health Organization; 2003. [Google Scholar]
- Witsenburg C, Dieben S, Van der Westerlaken L, BVerburg H, Naaktgeboren N. Cumulative live birth rates in cohorts of patients treated with in vitro fertilization or intracytoplasmic sperm injection. Fertil Steril. 2005;84:99–107. doi: 10.1016/j.fertnstert.2005.02.013. [DOI] [PubMed] [Google Scholar]
- Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, Sullivan E, Vanderpoel S. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92:1520–1524. doi: 10.1016/j.fertnstert.2009.09.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.