Abstract
Respiratory Syncytial Virus (RSV) is a common virus that infects children and adults; however, children younger than two years of age tend to develop more serious respiratory symptoms. RSV is responsible for thousands of outpatient visits (e.g., emergency room/primary care physician), hospitalizations and can result in death. Treatment is primarily supportive care and the illness resolves without complications in most children. RSV prophylaxis with palivizumab is an option for high-risk infants and children, which can decrease hospitalization and length of stay. Immunocompromised patients are a special population of which ribavirin and palivizumab may be used for treatment. Currently, no medication or vaccine available has been able to show a reduction in mortality from RSV. Future vaccines are in the developmental stage and will hopefully decrease the symptomatic and economic burden of this disease.
Keywords: child, infant, palivizumab, ribavirin, motavizumab
INTRODUCTION
Respiratory syncytial virus (RSV) was first described as ‘acute catarrhal bronchitis’ in 1901.1 It was isolated in 1956 and today is responsible for 45%–90% of episodes of bronchiolitis, 15%–35% of pneumonia, 6%–8% of croup, and is also a cause of apnea and otitis media. More than half of all children are infected by their first birthday.2 By 2 years of age, more than 80% of children have been infected at least once, and half of these children have had RSV twice.2
In 2000, RSV was responsible for 1.7 million physician office visits, 402,000 emergency room visits, 236,000 hospital outpatient visits and 86,000 hospitalizations of children <5 years of age.3 The cost of treating RSV was found to be $394 million for hospitalizations and $258 million for other medical encounters in the US.3 Another study examining 4 years of data found the emergency room costs of RSV in the US to be approximately $202 million and total hospital charges of RSV as a primary diagnosis to be more than $2.6 billion.4
One to three of every 100 patients with RSV as the primary infection are hospitalized, mostly 2–6 month olds.1 Five percent of patients with RSV are intubated.1 A Center for Disease Control and Prevention (CDC) evaluation from 1979–1997 determined that 200–500 children die annually due to RSV-associated illnesses.5 Another study examined mortality during 1999 and found 390 infant deaths with probable association to RSV.4 Mortality is generally low (<1%) in the normal population. However, patients with chronic respiratory disease, immunodeficiency or cardiac disease have a 3%–5% mortality risk.1 A Canadian study also determined a 1% mortality rate in children hospitalized with RSV from the years 1988–1991.6 Those infants with underlying lung or cardiac disease were at a higher risk of death in this study.
RSV not only affects children, but also adults. Some studies show RSV to have an annual incidence similar to influenza A in adults.7 Each year, RSV causes infections in 3%–7% of the elderly and 4%–10% of high-risk adults. Healthy adults with RSV have basic upper respiratory symptoms including cough, rhinorrhea, and congestion. However, there are approximately 170,000 hospitalizations and 10,000 deaths in patients >65 years of age due to RSV each year.8 It has also been estimated that RSV is responsible for 17 out of 1000 deaths of nursing home residents.9 Children have primarily been the focus of RSV disease and outcomes, but studies of new medications and vaccines should also consider evaluating adults, especially the elderly population. This article will review RSV, as a disease, and focus on treatment and prevention strategies in the pediatric population.
VIRAL CHARACTERISTICS
RSV is a single-stranded enveloped RNA Paramyxovirus. It has at least 10 proteins, with 3 surface proteins: G, F and SH.1 The G protein is responsible for attachment, while the F and SH proteins penetrate the cytoplasm and fuse with the host cell. The M protein is responsible for stabilizing the envelope, which is the focus of potential future vaccines. RSV has two subtypes, A and B. Both produce clinical disease but it is thought that A is responsible for more severe disease.1
Understanding the time period of the local RSV season will assist with the optimal administration of prophylaxis and clinical diagnosis. RSV typically occurs during November through March (winter/early spring). The National Respiratory and Enteric Virus Surveillance System monitors RSV throughout regions in the US. In temperate climates, the disease peaks in the winter.10 In the southern US, there is an earlier onset but a longer duration of RSV, except for Florida.11 Florida has the longest season of all in the US, where there is an increase in July, a peak in October and then a decrease in the spring.12 The Midwest US has a later onset and a shorter duration.11
Understanding RSV transmission can decrease the spreading of the virus. RSV is transmitted by direct or close contact with contaminated secretions; usually large droplets.1 Direct contamination has a higher impact than airborne transmission. The eyes and nose are the most sensitive inoculation areas, thus proper handwashing techniques and keeping the hands away from these areas can assist in decreasing transmission. RSV survives on surfaces for several hours. It can survive on a stethoscope for 6 hours, a non-porous surface for 12 hours and the hands for over 30 minutes. The incubation period is 3–5 days and viral shedding usually occurs for 3–8 days, but could be as long as 3 weeks in younger children and those who are immunocompromised. Viral shedding in adults is shorter, 1–6 days.13
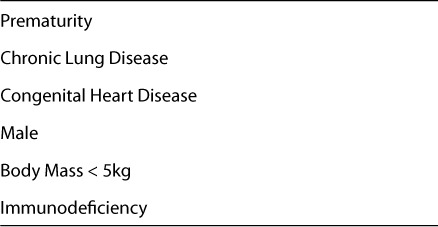
Risk factors for RSV are listed in Table 1.1,13–16 Table 2 lists factors that increase the severity of RSV.1,13,17 It is important for clinicians to interview parents in order to assess the child's risk factors for the disease, as these impact decisions regarding prophylaxis, treatment plans and monitoring.
Table 1.
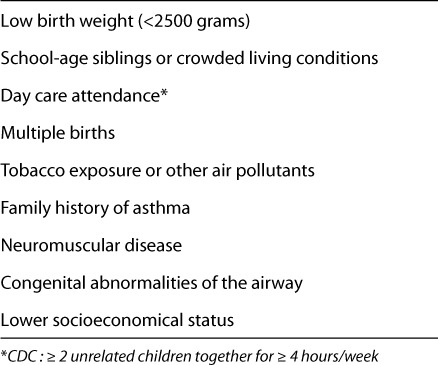
Table 2.
PATHOGENESIS
RSV is typically confined to the respiratory tract and lymphocytic peribronchiolar infiltration is noted.13 RSV replicates in the nasopharynx and then binds to the bronchiolar epithelium causing necrosis of the cell. Hypersecretion of mucous occurs and round cells infiltrate causing edema in the surrounding submucosa. Thus, the lumina of the small airways become obstructed. Hyperinflation results from air trapping in the peripheral areas and atelectasis occurs when the trapped air is absorbed. Interleukins, chemokines, and leukotrienes are released and cause inflammation and tissue damage during and after the infection. Recovery of the epithelium starts the first week of the illness but the ciliated cells do not recover until several weeks later.
CLINICAL MANIFESTATIONS
The preterm infant with RSV may present with poor feeding, apnea, irritability or lethargy. Apnea is associated with up to 20% of hospitalizations in RSV-positive infants, mostly pre-term and young neonates.18,19 Infants present with constant clear rhinorrhea, cough, sneezing, fever, shortness of breath, wheezing, pharyngitis or respiratory distress. Cough and wheezing occur in 50% of infected children.1 Older children and adults present with typical cold symptoms such as congestion, cough and fever. The American Academy of Pediatrics (AAP) defines severe disease in any child as “signs and symptoms associated with poor feeding and respiratory distress characterized by tachypnea, nasal flaring and hypoxemia.”20 Wheezing and rhinorrhea are commonly seen in adults with RSV.8
RSV symptoms peak around day 5 of the illness and often improve at 7–10 days.1 However, the cough may linger for about 4 weeks due to the slow recovery of the ciliated cells. Fifty percent of patients may have a prolonged wheeze after an RSV illness;13 however, it is debated if it is due to the RSV or from a prior undiagnosed host reactive airway disease. IgE is theorized to play the role in wheezing. The more IgE found during the infection, the more wheezing in the child. The Tucson Children's Respiratory Study enrolled more than 1200 children from 1980–1984, with more than 900 children being followed for 13 years.21 They found that lower respiratory tract infections increased the risk of wheezing in those up to 6 years of age. After 6 years of age, the incidence decreased and there was no difference found at age 13 years. Children who do not clinically improve as expected should be evaluated for other diagnoses such as vascular ring, heart failure, or foreign body. In adults, RSV was found to alter the airway reactivity for 8 weeks after infection, but returned to normal function at 4 months.
DIAGNOSIS
AAP recommends using clinical judgment as a reasonable way to diagnose RSV.20 Diagnostic tests can be helpful but rarely alter treatment. Nasopharyngeal washes or tracheal secretions are better specimens for confirming RSV than nasal swabs;1 however, nasal swabs are most commonly performed due to ease. Enzyme immunoassay (EIA) is the most common rapid detection test utilized due to the result time (~ 30 minutes), low cost and objective end point.13 EIA has a 90%–95% specificity, when RSV is in the community, but only a 50%–90% sensitivity range. Therefore, a negative result should not rule out RSV if clinical symptoms are present. Direct and indirect immunofluorescent assays are available but require skilled personnel and several hours for results. Another diagnostic test includes RSV cultures, but expense, time and variable laboratory technique limit its use. Washes and aspirates are more likely to grow in culture but require 4 days to 2 weeks for a result. By this time, the child should be improving or clinically recovered from the infection. Chest radiographs are not diagnostic but can show hyperinflation, peribronchial thickening or atelectasis.
TREATMENT
Supportive Care
Supportive care is the mainstay of treatment for RSV bronchiolitis. Most infants can be managed at home, but those who are ill appearing, dehydrated, have poor feeding, apnea, develop respiratory distress or require supplemental oxygen should be considered for hospitalization. The typical length of stay in the hospital ranges from 3–7 days.13
Supportive care includes hydration (i.e., oral or intravenous), clearing nasal obstruction with saline nose drops, nasal bulb suction or deep suctioning in the hospital and nutrition for the patient. Oral feedings should be encouraged. Temporary feeding tubes (e.g., nasogastric) may be required in rare situations. Oxygen may be needed in those struggling to keep their oxygen saturation >90% and it is recommended for patients whose saturations are consistently <90%.20 Mechanical ventilation is considered in those with respiratory failure and/or severe apnea. This encompasses about 5% of healthy infants hospitalized with RSV and 20% of infants with underlying chronic lung disease, congenital heart disease or immunosuppression. Chest physiotherapy is not recommended as no benefits have been identified in clinical trials.22 Contact precautions and playroom/toy restrictions should be required for all patients with RSV to decrease transmission.
Bronchodilators
Treatment of RSV with inhaled bronchodilators such as albuterol and epinephrine is debatable. Clinical trials vary in response. Large, randomized trials, meta-analysis, and systemic reviews do not support the use of bronchodilators in infants with RSV.23 In addition, long-term outcomes studies have found no difference in such drugs versus placebo. One analysis of bronchodilators (not epinephrine) versus placebo found no difference in clinical score improvement, oxygen utilization, hospitalization rate or duration in 8 clinical trials.23 Nebulized albuterol (0.1 mg/kg) has shown short-term clinical improvement (2 treatments at 30 minute intervals) in the ED in one trial.24 No long term (60 minutes–2 hours) improvement or change in clinical illness or hospitalization in several trials of nebulized or inhaled (meter dose inhaler) albuterol or salbutamol.23,25–27 Oral dosage forms are not recommended.28 A comparison of nebulized albuterol (0.15 mg/kg), nebulized saline, oral albuterol (0.15 mg/kg) and oral placebo found no difference in heart or respiratory rate, oxygenation, or the infant's clinical state between groups when comparing two nebulizations 30 minutes apart or one oral dose.29 Another study found no difference in oxygenation with albuterol nebulization (1.25 mg for <10 kg and 2.5 mg for others) versus placebo in infants with moderate symptoms when evaluating at baseline, 24 hours or time at maximum oxygenation during a hospitalization stay.30 A recent study of oral salbutamol (0.1 mg/kg) three times a day for 7 days or until symptom resolutions showed no difference from placebo when evaluating duration of symptoms, duration of resolution, hospitalization rates or adverse effects in infants with mild bronchiolitis.31 Dosing recommendations for albuterol specifically in RSV infections is not available; however, most clinical studies dosed 0.1–0.15 mg/kg with a common maximum of 2.5 mg per nebulization treatment.
Epinephrine has also been evaluated with mixed results. Studies vary for epinephrine, as some used racemic epinephrine and others utilized l-epinephrine. L-epinephrine is dosed at half of the racemic dose. Nebulized epinephrine was compared to placebo in 5 different inpatient studies and 3 outpatient studies, of which change in clinical score was significant at 60 minutes.32 Change in oxygen saturation, respiratory rate improved at 30 minutes, and ‘improvement’ was seen with epinephrine versus placebo in the outpatient studies.32 Pulse was higher in the epinephrine group and admission rates did not vary per group.32
Four inpatient studies compared nebulized epinephrine and salbutamol, of which epinephrine resulted in an improved respiratory rate at 30 minutes.32 Four outpatient studies found epinephrine to improve oxygen saturation and respiratory rate at 60 minutes.32 A study in the ED found no difference in clinical score or respiratory rate between three doses of nebulized epinephrine (0.9 mg/kg/dose) and albuterol (0.15 mg/kg/dose) for bronchiolitis at 0, 30 and 60 minutes.33 Most clinical studies of nebulized epinephrine in RSV found early benefit in symptoms but long-term outcomes were not significant.
The AAP recommends bronchodilators should not be used routinely, but may be considered for a trial use and continued if there is an objective response.20 Bronchodilators may be tried in patients if the patient has bronchospasms or a family history of asthma. They tend not to be effective in younger infants due to poor penetration into the peripheral airways.34
Corticosteroids
Corticosteroids of all forms (oral, inhaled, intravenous, intramuscular) are not recommended for routine use in children for RSV.20,35 Most studies fail to show clinical benefit, a reduction in hospitalization rates or duration, a decrease in the use of mechanical ventilation or repeat admissions. However, a meta-analysis of steroids (i.e., PO, IM, or IV dexamethasone, PO prednisolone, IM methylprednisolone and IV hydrocortisone) use in RSV found a shorter length of stay and duration of symptoms in children less than 2 years of age (p = 0.03).36 An oral steroid burst may be warranted if the infant or child responds to albuterol or epinephrine and an underlying asthma or reactive airway disease component in the child is considered.
Antibiotics
Antibiotics are not recommended as RSV is a viral infection.37 Secondary bacterial infections are rare (<1%), thus antibiotics should only be prescribed after certain diagnosis.20
Ribavirin
Ribavirin (Virazole, Valeant Pharmaceuticals International, Aliso Viejo, California) is the only drug approved by the Food and Drug Administration (FDA) for treatment of RSV. It inhibits the replication of DNA and RNA viruses. Clinically this agent is not utilized due to several factors. Placebo controlled studies fail to show a decrease in mechanical ventilation, length of stay in the intensive care unit or hospital, or a decrease in mortality.38–42 However, some studies have shown a small benefit in subjective outcomes and a possible decrease in long-term wheezing.26 The AAP recommends the use of ribavirin to be based on clinical circumstances, patient factors and risks, and used in those ‘with severe disease or those at risk for severe disease, such as immunocom-promised and/or hemodynamically significant cardiopulmonary disease. 20 It may also be used in the immunocompromised/transplant high-risk groups with or without RSV-IGIV/palivizumab.
Ribavirin is very expensive and is a known teratogen in rodents, thus it is contraindicated in pregnancy, pregnancy category X. It is an aerosolized agent that is used for 8–24 hours for 3–5 days. It can only be used with a certain device, the small particle aerosol generator model-2 (SPAG-2). It may be delivered via oxyhood or tent.43 Adverse effects can be seen in healthcare workers who administer the medication or take care of the patient as well as the family members who are near the patient when the medication is administered, even when precautions are taken. Headaches are the most common adverse effect. Nausea can occur as well. The aerosolized therapy can also worsen bronchospasms but it is rare.43 There are a few ways to decrease exposure to the drug. Administering in a negative pressure room or turning off the SPAG for about 5 minutes prior to lifting the tent or hood can decrease the spread of particles.43 However, surgical masks do not filter out the drug from inhalation.43
Others
RSV-IGIV, RSV immunoglobulin, has been evaluated for treatment of RSV but showed no benefit.44 Palivizumab (Synagis, MedImmune, Inc, Gaithersburg, Maryland) a monoclonal antibody, has been evaluated for safety and kinetics for treatment of RSV in previously healthy children but the study could not detect clinical outcome differences due to small sample size.45 However, a retrospective review found decreased mortality when IV palivizumab (mean dose: 14.9 mg/kg) was used with (80%) or without ribavirin (primarily aerosolized) in 31 children who were immunocompromised (n = 18), premature (n = 5), had congenital heart issues (n = 4), or had other issues (n = 4).46 Twenty-nine patients survived with treatment and no adverse effects were reported. A phase 1 study found IV palivizumab (15 mg/kg/dose) prevented lower respiratory tract disease in 3 hematopoietic stem cell transplant patients with an RSV upper respiratory tract infection.47 It also showed an 83% survival rate in 12 transplant patients with RSV interstitial pneumonia for a 28 day study period. No adverse effects were reported in this study as well. These studies may lead to additional research with palivizumab and ribavirin for treatment in immunocompromised patients.
Heliox, an inhaled mixture of helium and oxygen, has been studied in small trials with mixed results.48,49 It was shown to provide turbulence and resistance versus oxygen, thus improving ventilation and decrease work of breathing. Inhaled nitric oxide was evaluated in 12 infants with RSV bronchiolitis and did not show benefit over salbutamol.50 However, a case report stated benefit of nitric oxide with high frequency ventilator use in a 7 month old with RSV.51 Extracorporeal membrane oxygenation has also been used in patients with RSV. One study found success with this in premature infants who were ventilated after birth or had bronchopulmonary dysplasia.52 Additional clinical trials are needed prior to recommending routine use of these agents in RSV patients.
Surfactants are theorized to possibly be beneficial as it is believed severe bronchiolitis results in surfactant deficiency. Small clinical trials of ventilated patients show a decrease in mechanical ventilation use and ICU stay;53 however, more data is required prior to recommendation for such treatment. Nebulized recombinant human DNase (2.5 mg) was no better than placebo in reducing hospital length of stay or days of oxygen use in 225 oxygen-dependent infants with RSV.54 Case reports have shown benefit55 and a trial in hospitalized infants resulted in an improved chest x-ray findings versus placebo, but failed to show a difference in respiratory rate, wheezing or retractions with recombinant human deoxyribonuclease I.56
PREVENTION
Non-pharmacological methods of preventing the spread of RSV are important. Practitioners, parents, and those in close contact with a child with RSV should practice good hand washing technique and repetitive hand washing. Patient isolation of those with RSV in a hospital environment, infection control measures, and cleaning of toys and other objects contaminated with RSV will also aid in decreasing viral transmission. Two prophylaxis products are recommended for use in high-risk patients to prevent RSV infections, respiratory syncytial virus immune globulin intravenous (RSV-IGIV, RespiGam, MedImmune, Inc, Gaithersburg, Maryland) and palivizumab. Only palivizumab is currently available in the U.S. but both are discussed.
RSV-IGIV
RSV-IGIV is made from donors with high RSV neutralizing antibody titers. It is administered as a 4 hour infusion once a month during the RSV season (starting one month prior to season) and is dosed as 750 mg/kg/month. Two clinical trials evaluated RSV-IGIV efficacy in RSV infants, the PREVENT study group (Reduction of respiratory syncytial virus hospitalization among premature infants and infants with bronchopulmonary dysplasia using respiratory syncytial virus immune globulin prophylaxis) and NIAID (National Institute of Allergy and Infectious Disease) trials.57,58 There was a statistically significant decrease in rate of hospitalizations in both studies (41%57 and 63%58) and a decrease in length of stay (53%57 and 63%58). There was a trend for decreasing intensive care unit (ICU) admissions and mechanical ventilation. In the PREVENT trial, RSV-IGIV also decreased the hospitalization incidence and hospital days of those with any viral respiratory infections.57 Patients experienced adverse effects such as a mild decrease in oxygen saturation, fever, and mild fluid overload from RSV-IGIV.57,58 Those patients in the congenital heart disease group were found to have an increase in mortality, which lead to concerns in this patient population.58 Today, RSV-IGIV is contraindicated in patients with hemodynamically significant heart disease. If RSV-IGIV is administered to a child, live vaccines, such as varicella and measles, mumps, rubella must be deferred for 9 months after the last RSV-IGIV dose.
Palivizumab
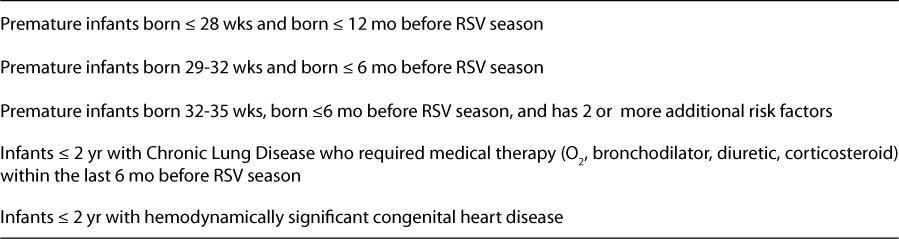
In 1998, palivizumab was approved for use of preventing RSV infections in specific patient populations (Table 3).59 Palivizumab is a humanized mouse monoclonal antibody that attaches to the F protein to neutralize and prevent fusion of the virus with the epithelial cell. It is 50 times more potent than RSV-IGIV and administered as a 15 mg/kg intramuscular injection once monthly, starting one month prior to RSV season. Five doses are typically provided to the patient. Dose volumes over 1 mL must be administered in divided doses. Palivizumab must be stored in the refrigerator and open vials should be utilized within 6 hours. Palivizumab should be continued throughout the season, even if the patient contracts RSV or outgrows the indication during the season. The Palivizumab Outcomes Registry monitors the passive vaccines and post-licensure data that further confirm the clinical trials. Currently, no palivizumab resistant RSV strains have been identified.
Table 3.
Palivizumab FDA Indications for Use59
The IMpact-RSV trial evaluated palivizumab in 1,502 infants.60 Children <24 months with bronchopulmonary dysplasia or children who were premature (<35 weeks) and ≤6 months of age at study entry were included. Hospitalizations were reduced from 10.6% in the placebo group to 4.8% in the palivizumab group (p < 0.001). ICU admissions were reduced by 57% (p = 0.026). Hospital length of stay and days on oxygen were also decreased, 42% and 40%, respectively (both p < 0.001). The ICU length of stay, mechanical ventilation and incidence of otitis media were not altered with palivizumab. It is important to note that the incidence of mortality did not change with palivizumab. Adverse reactions reported in the clinical trials included injection site reactions, rash, and increased liver function tests. Also, post-marketing reports describe severe thrombocytopenia in <1 person per 100,000.59
Palivizumab was then studied over 4 RSV seasons in 1,287 patients that were ≤ 24 months of age with hemodynamically significant congenital heart disease.61 Hospitalizations were decreased from 9.7% in the placebo group to 5.3% in the palivizumab group (p < 0.003). Length of stay was decreased 56% (p < 0.014). There was no change in ICU admissions, mechanical ventilation or mortality. Adverse effects included fever, injection site reactions and cyanosis (3.6% vs. 2.2%).
Because of these trials, palivizumab is FDA indicated in those children listed in Table 3 and this serves as the AAP recommended criteria for use.59,62 In addition, it may be considered in infants ≤ 2 years of age with serious conditions that compromise pulmonary or immune function, such as immunocompromised or transplant patients. Cystic fibrosis patients may be administered palivizumab to prevent RSV infections;63,64 however, no clinical trials are available at this time. It is also important to consider the patient's insurance prior to administering the medication. Each state's Medicaid program, as well as private insurance plans, differ on coverage criteria/risk factors for reimbursement of palivizumab prophylaxis.
Cost analyses have been conducted on both products. RSV-IGIV cost more than $53,000 to prevent 1 hospitalization due to RSV bronchiolitis.65 Palivizumab costs approximately $6,000 per patient per season. Most cost-effective analyses do not show benefit as costs range from $39,000–$420,000 to prevent 1 hospitalization.66 Cost savings have been seen more in the earlier preterm infant versus other groups. In those ≤ 32 weeks (who required ≥ 28 days of oxygen and were discharged Sept–Nov), the number needed to treat to avoid one hospitalization was 7.4. In the other neonatal intensive care patients, the number needed to treat ranged from 15–152.
There are no comparative clinical trials between RSV-IGIV and palivizumab. Although palivizumab is the only product available today, if both were on the market, palivizumab typically would be favored based upon ease of administration, less adverse effects and lack of interference with live vaccines.
NEW VACCINES/BIOLOGICS
Currently no vaccine is available to prevent RSV. Previous versions, such as a formalin-inactivated vaccine, only led to more severe diseases in those exposed to natural disease.1 An intravenous live vaccine did not demonstrate efficacy and an attenuated vaccine showed no response or caused symptomatic disease.1 A cold-adapted live vaccine is currently being evaluated, as well as a recombinant adenovirus base vaccine which expressed the G protein. Potential future vaccines may consider other surface proteins for mechanisms of prevention.
Motavizumab (Numax, MedImmune, Inc, Gaithersburg, Maryland) is a second generation monoclonal antibody derived from palivizumab. It is more potent due to enhanced binding, 70-fold increased binding to F protein than palivizumab.67,68 A phase 3 study on motavizumab as prophylaxis for RSV evaluated 6,635 pre-term infants and found motavizumab decreased hospitalizations by 26% compared to palivizumab (p < 0.01 for non-inferiority).69 There was also a 50% reduction (4% vs 2%) of RSV-specific medically attended outpatient lower respiratory tract infections (p < 0.01). No difference was seen in mortality rates.
In an additional phase 3 trial, in 1,410 full term Native American infants < 6 months of age, motavizumab decreased hospitalization by 83% (1.4 motavizumab vs. 8.3 placebo, p < 0.001).67 It also decreased outpatient visits (2.8% motavizumab vs. 9.5% placebo) for RSV lower respiratory tract infections (p < 0.001). Mortality rates did not differ. The biological licensure application was submitted to the FDA in January of 2008 and the company is awaiting response. Motavizumab is also in phase 2 studies for treatment of RSV. A third generation antibody is already in development, Numax-YTE, which has an extended serum half-life.67 It has a 4 fold half-life in the Rhesus monkey and a 4 fold bioavailability in the lung.
Many questions remain regarding these newer agents and full release of data will assist with providing clinical efficacy information (motavizumab vs. palivizumab or placebo) and evaluation of cost-effectiveness of the available agents as they come on the market.
CONCLUSION
RSV is a disease that impacts millions of children each year. Supportive care including nutrition, hydration, clearing of nasal secretions, and oxygen, if needed, remains the mainstay therapy for patients. Good handwashing techniques and contact isolation should be conducted to prevent RSV transmission. Those with risk factors, who meet inclusion criteria, should be administered palivizumab to prevent RSV infections. Ribavirin and palivizumab may be utilized for treatment in immunocompromised patients. Future vaccines could potentially decrease the economic burden of RSV in the healthcare setting.
ABBREVIATIONS
- AAP
American Academy of Pediatrics
- CDC
Centers for Disease Control and Prevention
- EIA
enzyme immunoassay
- ED
emergency department
- FDA
Food and Drug Administration
- ICU
intensive care unit
- RSV
respiratory syncytial virus
- RSV-IGIV
respiratory syncytial virus immune globulin intravenous
- SPAG-2
small particle aerosol generator model-2
- US
United States
Footnotes
DISCLOSURE The author declares no conflicts or financial interest in any product or service mentioned in the manuscript, including grants, equipment, medications, employment, gifts, and honoraria.
REFERENCES
- 1.Tristram DA, Welliver RC. Respiratory Syncytial Virus. In: Long SS, Pickering LK, Prober CG, editors. Principles and Practice of Pediatric Infectious Diseases. 2nd ed. New York, NY: Churchill Livingstone; 2003. pp. 213–218. [Google Scholar]
- 2.Glezen WP, Taber LH, Frank AL. Risk of primary infection and reinfection with respiratory syncytial virus. Am J Dis Child. 1986;140:543–546. doi: 10.1001/archpedi.1986.02140200053026. et al. [DOI] [PubMed] [Google Scholar]
- 3.Paramore LC, Ciuryla V, Ciesla G. Economic impact of respiratory syncytial virus-related illness in the US: an analysis of national databases. Pharmacoeconomics. 2004;22:275–284. doi: 10.2165/00019053-200422050-00001. et al. [DOI] [PubMed] [Google Scholar]
- 4.Leader S, Kohlhase K. Recent trends in severe respiratory syncytial virus (RSV) among US infants, 1997 to 2000. J Pediatr. 2003;143:S127–132. doi: 10.1067/s0022-3476(03)00510-9. [DOI] [PubMed] [Google Scholar]
- 5.Shay DK, Holman RC, Roosevelt GE. Bronchiolitis-associated mortality and estimates of respiratory syncytial virus-associated deaths among US children, 1979–1997. J Infect Dis. 2001;183:16–22. doi: 10.1086/317655. et al. Epub 2000 Nov 10. [DOI] [PubMed] [Google Scholar]
- 6.Navas L, Wang E, de Carvalho V. Improved outcome of respiratory syncytial virus infection in a high-risk hospitalized population of Canadian children. Pediatric Investigators Collaborative Network on Infections in Canada. J Pediatr. 1992;121:348–354. doi: 10.1016/s0022-3476(05)90000-0. et al. [DOI] [PubMed] [Google Scholar]
- 7.Falsey AR, Hennessey PA, Formica MA. Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med. 2005;352:1749–1759. doi: 10.1056/NEJMoa043951. et al. [DOI] [PubMed] [Google Scholar]
- 8.Murata Y, Falsey AR. Respiratory syncytial virus infection in adults. Antivir Ther. 2007;12:659–670. [PubMed] [Google Scholar]
- 9.Ellis SE, Coffey CS, Mitchel EF Jr. Influenza- and respiratory syncytial virus-associated morbidity and mortality in the nursing home population. J Am Geriatr Soc. 2003;51:761–767. doi: 10.1046/j.1365-2389.2003.51254.x. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) Brief report: respiratory syncytial virus activity–United States, July 2006–November 2007. MMWR Morb Mortal Wkly Rep. 2007;56:1263–1265. [PubMed] [Google Scholar]
- 11.Panozzo CA, Fowlkes AL, Anderson LJ. Variation in timing of respiratory syncytial virus outbreaks: lessons from national surveillance. Pediatr Infect Dis J. 2007;26:S41–S45. doi: 10.1097/INF.0b013e318157da82. [DOI] [PubMed] [Google Scholar]
- 12.Light M. Respiratory syncytial virus seasonality in southeast Florida: results from three area hospitals caring for children. Pediatr Infect Dis J. 2007;26:S55–S59. doi: 10.1097/INF.0b013e318157dac1. [DOI] [PubMed] [Google Scholar]
- 13.Hall CB, McCarthy CA. Respiratory syncytial virus. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas and Bennett's principles and practice of infectious diseases. 5th ed. Philadelphia: Churchill Livingston; 2000. pp. 1782–1801. [Google Scholar]
- 14.Panitch HB. Viral respiratory infections in children with technology dependence and neuromuscular disorders. Pediatr Infect Dis J. 2004;23:S222–S227. doi: 10.1097/01.inf.0000144670.78558.c7. [DOI] [PubMed] [Google Scholar]
- 15.Arnold SR, Wang EE, Law BJ. Variable morbidity of respiratory syncytial virus infection in patients with underlying disease: a review of the PICNIC RSV database. Pediatr Infect Dis J. 1999;18:866–869. doi: 10.1097/00006454-199910000-00006. et al. [DOI] [PubMed] [Google Scholar]
- 16.Lanari M, Giovannini M, Giuffre L. Prevalence of respiratory syncytial virus infection in Italian infants hospitalized for acute lower respiratory tract infections, and association between respiratory syncytial virus infection risk factors and disease severity. Pediatr Pulmonol. 2002;33:458–465. doi: 10.1002/ppul.10047. et al. [DOI] [PubMed] [Google Scholar]
- 17.American Academy of Pediatrics. Respiratory Syncytial Virus. In: Pickering LK, Baker CJ, Long SS, McMillan JA, editors. Red Book: 2006 Report of the Committee on Infectious Diseases. 27th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2006. pp. 560–566. [Google Scholar]
- 18.Church NR, Anas NG, Hall CB. Respiratory syncytial virus-related apnea in infants. Demographics and outcome. Am J Dis Child. 1984;138:247–250. doi: 10.1001/archpedi.1984.02140410027010. et al. [DOI] [PubMed] [Google Scholar]
- 19.Bruhn FW, Mokrohisky ST, McIntosh K. Apnea associated with respiratory syncytial virus infection in young infants. J Pediatr. 1977;90:382–386. doi: 10.1016/s0022-3476(77)80697-5. [DOI] [PubMed] [Google Scholar]
- 20.American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis. Diagnosis and management of bronchiolitis. Pediatrics. 2006;118:1774–1793. doi: 10.1542/peds.2006-2223. [DOI] [PubMed] [Google Scholar]
- 21.Stein RT, Sherrill D, Morgan WJ. Respiratory syncytial virus in early life and risk of wheeze and allergy by age 13 years. Lancet. 1999;354:541–545. doi: 10.1016/S0140-6736(98)10321-5. et al. [DOI] [PubMed] [Google Scholar]
- 22.Perrotta C, Ortiz Z, Roque M. Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old. Cochrane Database of Systematic Reviews. 2007. Art. No.: CD004873. DOI: 10.1002/14651858.CD004873.pub3. [DOI] [PubMed]
- 23.Gadomski AM, Bhasale AL. Bronchodilators for bronchiolitis. Cochrane Database of Systematic Reviews. 2006. Art. No.: CD001266. DOI: 10.1002/14651858.CD001266.pub2. [DOI] [PubMed]
- 24.Klassen TP, Rowe PC, Sutcliffe T. Randomized trial of salbutamol in acute bronchiolitis. J Pediatr. 1991;118:807–811. doi: 10.1016/s0022-3476(05)80051-4. et al. [DOI] [PubMed] [Google Scholar]
- 25.Ho L, Collis G, Landau LI. Effect of salbutamol on oxygen saturation in bronchiolitis. Arch Dis Child. 1991;66:1061–1064. doi: 10.1136/adc.66.9.1061. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hammer J, Numa A, Newth CJ. Albuterol responsiveness in infants with respiratory failure caused by respiratory syncytial virus infection. J Pediatr. 1995;127:485–490. doi: 10.1016/s0022-3476(95)70088-9. [DOI] [PubMed] [Google Scholar]
- 27.Torres A, Jr, Anders M, Anderson P. Efficacy of metered-dose inhaler administration of albuterol in intubated infants. Chest. 1997;112:484–490. doi: 10.1378/chest.112.2.484. et al. [DOI] [PubMed] [Google Scholar]
- 28.Patel H, Gouin S, Platt RW. Randomized, double-blind, placebo-controlled trial of oral albuterol in infants with mild-to-moderate acute viral bronchiolitis. J Pediatr. 2003;142:509–514. doi: 10.1067/mpd.2003.196. [DOI] [PubMed] [Google Scholar]
- 29.Gadomski AM, Lichenstein R, Horton L. Efficacy of albuterol in the management of bronchiolitis. Pediatrics. 1994;93:907–912. et al. [PubMed] [Google Scholar]
- 30.Dobson JV, Stephens-Groff SM, McMahon SR. The use of albuterol in hospitalized infants with bronchiolitis. Pediatrics. 1998;101:361–368. doi: 10.1542/peds.101.3.361. et al. [DOI] [PubMed] [Google Scholar]
- 31.Gupta P, Aggarwal A, Gupta P. Oral salbutamol for symptomatic relief in mild bronchiolitis a double blind randomized placebo controlled trial. Indian Pediatrics. 2008;45:547–553. et al. [PubMed] [Google Scholar]
- 32.Hartling L, Wiebe N, Russell K. Epinephrine for bronchiolitis. Cochrane Database of Systematic Reviews. 2004;(Issue 1) doi: 10.1002/14651858.CD003123.pub2. et al. Art. No.: CD003123. DOI: 10.1002/14651858.CD003123.pub2. [DOI] [PubMed] [Google Scholar]
- 33.Mull CC, Scarfone RJ, Ferri LR. A randomized trial of nebulized epinephrine vs albuterol in the emergency department treatment of bronchiolitis. Arch Pediatr Adolesc Med. 2004;158:113–118. doi: 10.1001/archpedi.158.2.113. et al. [DOI] [PubMed] [Google Scholar]
- 34.Amirav I, Balanov I, Gorenberg M. ß-agonist aerosol distribution in respiratory syncytial virus bronchiolitis in infants. J Nucl Med. 2002;43:487–491. et al. [PubMed] [Google Scholar]
- 35.Blom D, Ermers M, Bont L. Inhaled corticosteroids during acute bronchiolitis in the prevention of post-bronchiolitic wheezing. Cochrane Database of Systematic Reviews. 2007;(Issue 1) doi: 10.1002/14651858.CD004881.pub2. et al. Art. No.: CD004881. DOI: 10.1002/14651858.CD004881.pub2. [DOI] [PubMed] [Google Scholar]
- 36.Garrison MM, Christakis DA, Harvey E. Systemic corticosteroids in infant bronchiolitis: A meta-analysis. Pediatrics. 2000;105:E44. doi: 10.1542/peds.105.4.e44. et al. [DOI] [PubMed] [Google Scholar]
- 37.Spurling GK, Fonseka K, Doust J, Del Mar C. Antibiotics for bronchiolitis in children. Cochrane Database of Systematic Reviews. 2007;(Issue 1) doi: 10.1002/14651858.CD005189.pub2. Art. No.: CD005189. DOI: 10.1002/14651858.CD005189.pub2. [DOI] [PubMed] [Google Scholar]
- 38.Guerguerian AM, Gauthier M, Lebel MH. Ribavirin in ventilated respiratory syncytial virus bronchiolitis. A randomized, placebo-controlled trial. Am J Respir Crit Care Med. 1999;160:829–834. doi: 10.1164/ajrccm.160.3.9810013. et al. [DOI] [PubMed] [Google Scholar]
- 39.Law BJ, Wang EE, MacDonald N. Does ribavirin impact on the hospital course of children with respiratory syncytial virus (RSV) infection? An analysis using the pediatric investigators collaborative network on infections in Canada (PICNIC) RSV database. Pediatrics. 1997;99:E7. doi: 10.1542/peds.99.3.e7. et al. [DOI] [PubMed] [Google Scholar]
- 40.Moler FW, Steinhart CM, Ohmit SE. Effectiveness of ribavirin in otherwise well infants with respiratory syncytial virus-associated respiratory failure. Pediatric Critical Study Group. J Pediatr. 1996;128:422–428. doi: 10.1016/s0022-3476(96)70294-9. et al. [DOI] [PubMed] [Google Scholar]
- 41.Meert KL, Sarnaik AP, Gelmini MJ. Aerosolized ribavirin in mechanically ventilated children with respiratory syncytial virus lower respiratory tract disease: a prospective, double-blind, randomized trial. Crit Care Med. 1994;22:566–572. doi: 10.1097/00003246-199404000-00010. et al. [DOI] [PubMed] [Google Scholar]
- 42.Ventre K, Randolph AG. Ribavirin for respiratory syncytial virus infection of the lower respiratory tract in infants and young children. Cochrane Database Syst Rev. 2007;(1):CD000181. doi: 10.1002/14651858.CD000181.pub3. [DOI] [PubMed] [Google Scholar]
- 43.Krilov LR. Safety issues related to the administration of ribavirin. Pediatr Infect Dis J. 2002;21:479–481. doi: 10.1097/00006454-200205000-00037. [DOI] [PubMed] [Google Scholar]
- 44.Rodriguez WJ, Gruber WC, Groothuis JR. Respiratory syncytial virus immune globulin treatment of RSV lower respiratory tract infection in previously healthy children. Pediatrics. 1997;100:937–942. doi: 10.1542/peds.100.6.937. et al. [DOI] [PubMed] [Google Scholar]
- 45.Sáez-Llorens X, Moreno MT, Ramilo O. Safety and pharmacokinetics of palivizumab therapy in children hospitalized with respiratory syncytial virus infection. Pediatr Infect Dis J. 2004;23:707–712. doi: 10.1097/01.inf.0000133165.85909.08. et al. [DOI] [PubMed] [Google Scholar]
- 46.Chávez-Bueno S, Mejías A, Merryman RA. Intravenous palivizumab and ribavirin combination for respiratory syncytial virus disease in high-risk pediatric patients. Pediatr Infect Dis J. 2007;26:1089–1093. doi: 10.1097/INF.0b013e3181343b7e. et al. [DOI] [PubMed] [Google Scholar]
- 47.Boeckh M, Berrey MM, Bowden RA. Phase 1 evaluation of the respiratory syncytial virus-specific monoclonal antibody palivizumab in recipients of hematopoietic stem cell transplants. J Infect Dis. 2001;184:350–354. doi: 10.1086/322043. et al. [DOI] [PubMed] [Google Scholar]
- 48.Martinón-Torres F, Rodríguez-Núñez A, Martinón-Sánchez JM. Heliox therapy in infants with acute bronchiolitis. Pediatrics. 2002;109:68–73. doi: 10.1542/peds.109.1.68. [DOI] [PubMed] [Google Scholar]
- 49.Cambonie G, Milési C, Fournier-Favre S. Clinical effects of heliox administration for acute bronchiolitis in young infants. Chest. 2006;129:676–682. doi: 10.1378/chest.129.3.676. et al. [DOI] [PubMed] [Google Scholar]
- 50.Patel NR, Hammer J, Nichani S. Effect of inhaled nitric oxide on respiratory mechanics in ventilated infants with RSV bronchiolitis. Intensive Care Med. 1999;25:81–87. doi: 10.1007/s001340050791. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hoehn T, Krause M, Krueger M. Treatment of respiratory failure with inhaled nitric oxide and high- frequency ventilation in an infant with respiratory syncytial virus pneumonia and bronchopulmonary dysplasia. Respiration. 1998;65:477–480. doi: 10.1159/000029317. et al. [DOI] [PubMed] [Google Scholar]
- 52.Khan JY, Kerr SJ, Tometzki A. Role of ECMO in the treatment of respiratory syncytial virus bronchiolitis: a collaborative report. Arch Dis Child Fetal Neonatal Ed. 1995;73:F91–F94. doi: 10.1136/fn.73.2.f91. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ventre K, Haroon M, Davison C. Surfactant therapy for bronchiolitis in critically ill infants. Cochrane Database of Systematic Reviews. 2006;(Issue 3) doi: 10.1002/14651858.CD005150.pub2. Art. No.: CD005150. DOI: 10.1002/14651858.CD005150.pub2. [DOI] [PubMed] [Google Scholar]
- 54.Boogaard R, Hulsmann AR, van Veen L. Recombinant human deoxyribonuclease in infants with respiratory syncytial virus bronchiolitis. Chest. 2007;131:788–795. doi: 10.1378/chest.06-2282. et al. [DOI] [PubMed] [Google Scholar]
- 55.Merkus PJ, de Hoog M, van Gent R. DNase treatment for atelectasis in infants with severe respiratory syncytial virus bronchiolitis. Eur Respir J. 2001;18:734–737. et al. [PubMed] [Google Scholar]
- 56.Nasr SZ, Strouse PJ, Soskolne E. Efficacy of recombinant human deoxyribonuclease I in the hospital management of respiratory syncytial virus bronchiolitis. Chest. 2001;120:203–208. doi: 10.1378/chest.120.1.203. et al. [DOI] [PubMed] [Google Scholar]
- 57.Reduction of respiratory syncytial virus hospitalization among premature infants and infants with bronchopulmonary dysplasia using respiratory syncytial virus immune globulin prophylaxis. The PREVENT Study Group. Pediatrics. 1997;99:93–99. doi: 10.1542/peds.99.1.93. [DOI] [PubMed] [Google Scholar]
- 58.Groothuis JR, Simoes EA, Levin MJ. Prophylactic administration of respiratory syncytial virus immune globulin to high-risk infants and young children. The Respiratory Syncytial Virus Immune Globulin Study Group. N Engl J Med. 1993;329:1524–1530. doi: 10.1056/NEJM199311183292102. et al. [DOI] [PubMed] [Google Scholar]
- 59.Product Information. Synagis (palivizumab) Gaithersburg, MD: MedImmune; October 2007. [Google Scholar]
- 60.Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. The IMpact-RSV Study Group. Pediatrics. 1998;102:531–537. [PubMed] [Google Scholar]
- 61.Feltes TF, Cabalka AK, Meissner HC. Cardiac Synagis Study Group. Palivizumab prophylaxis reduces hospitalization due to respiratory syncytial virus in young children with hemodynamically significant congenital heart disease. J Pediatr. 2003;143:532–540. doi: 10.1067/s0022-3476(03)00454-2. et al. [DOI] [PubMed] [Google Scholar]
- 62.American Academy of Pediatrics Committee on Infectious Diseases and Committee on Fetus and Newborn. Revised indications for the use of palivizumab and respiratory syncytial virus immune globulin intravenous for the prevention of respiratory syncytial virus infections. Pediatrics. 2003;112:1442–1446. [PubMed] [Google Scholar]
- 63.Speer ME, Fernandes CJ, Boron M. Use of Palivizumab for prevention of hospitalization as a result of respiratory syncytial virus in infants with cystic fibrosis. Pediatr Infect Dis J. 2008;27:559–561. doi: 10.1097/INF.0b013e3181673c15. et al. [DOI] [PubMed] [Google Scholar]
- 64.Giebels K, Marcotte JE, Podoba J. Prophylaxis against respiratory syncytial virus in young children with cystic fibrosis. Pediatr Pulmonol. 2008;43:169–174. doi: 10.1002/ppul.20751. et al. [DOI] [PubMed] [Google Scholar]
- 65.Barton LL, Grant KL, Lemen RJ. Respiratory syncytial virus immune globulin: decisions and costs. Pediatr Pulmonol. 2001;32:20–28. doi: 10.1002/ppul.1084. [DOI] [PubMed] [Google Scholar]
- 66.Joffe S, Ray GT, Escobar GJ. Cost-effectiveness of respiratory syncytial virus prophylaxis among preterm infants. Pediatrics. 1999;104:419–427. doi: 10.1542/peds.104.3.419. et al. [DOI] [PubMed] [Google Scholar]
- 67.Wu H, Pfarr DS, Losonsky GA. Immunoprophylaxis of RSV infection: advancing from RSV-IGIV to palivizumab and motavizumab. Curr Top Microbiol Immunol. 2008;317:103–123. doi: 10.1007/978-3-540-72146-8_4. et al. [DOI] [PubMed] [Google Scholar]
- 68.Wu H, Pfarr DS, Johnson S. Development of motavizumab, an ultra-potent antibody for the prevention of respiratory syncytial virus infection in the upper and lower respiratory tract. J Mol Biol. 2007;368:652–665. doi: 10.1016/j.jmb.2007.02.024. et al. [DOI] [PubMed] [Google Scholar]
- 69.MedImmune [homepage on the internet]. Gaithersburg: Press Releases. [updated 2008; cited 29 Sept 2008] Available from: http://phx.corporate-ir.net/phoenix.zhtml?c=83037&p=irol-investornewsArticle&ID=1043517&highlight=


