Abstract
Personality traits contribute to health outcomes, in part through their association with major controllable risk factors, such as obesity. Body weight, in turn, reflects our behaviors and lifestyle and contributes to the way we perceive ourselves and others. In this study, we use data from a large (N=1,988) longitudinal study that spanned more than 50 years to examine how personality traits are associated with multiple measures of adiposity and with fluctuations in body mass index (BMI). Using 14,531 anthropometric assessments, we modeled the trajectory of BMI across adulthood and tested whether personality predicted its rate of change. Measured concurrently, participants higher on Neuroticism or Extraversion or lower on Conscientiousness had higher BMI; these associations replicated across body fat, waist, and hip circumference. The strongest association was found for the impulsivity facet: Participants who scored in the top 10% of impulsivity weighed, on average, 11Kg more than those in the bottom 10%. Longitudinally, high Neuroticism and low Conscientiousness, and the facets of these traits related to difficulty with impulse control, were associated with weight fluctuations, measured as the variability in weight over time. Finally, low Agreeableness and impulsivity-related traits predicted a greater increase in BMI across the adult lifespan. BMI was mostly unrelated to change in personality traits. Personality traits are defined by cognitive, emotional, and behavioral patterns that likely contribute to unhealthy weight and difficulties with weight management. Such associations may elucidate the role of personality traits in disease progression and may help to design more effective interventions.
Once considered a sign of affluence, obesity is now a major public health crisis across the globe, from developing nations to the industrialized world (Yach, Stuckler, & Brownell, 2006). In the United States, the behaviors conducive to obesity, including poor diet and physical inactivity, are the second leading controllable cause of death, following smoking (Mokdad, Marks, Stroup, & Gerberding, 2004). In fact, obesity contributes to disease burden at approximately the same rate as smoking (Jia & Lubetkin, 2010) and it leads to a number of comorbidities, including type 2 diabetes, cardiovascular disease, several cancers, and, ultimately, shortens life expectancy (Haslam & James, 2005). Further, as the number of smokers continues to decline, obesity may overtake smoking as the leading preventable cause of disease (Mokdad et al., 2004).
Societal shifts in food quality, quantity, and availability are certainly major contributors to this recent increase in obesity. Yet, many other factors are also implicated in weight control. In particular, personality traits are consistently associated with the controllable behaviors that lead to obesity (Provencher et al., 2008) and personality has an effect on adiposity even after controlling for known demographic and genetic influences (Terracciano et al., 2009). Most studies of personality and weight have been cross-sectional; long-term longitudinal studies are needed to test how personality is associated with weight change across the adult lifespan.
With nearly 15,000 assessments of height and weight across more than 50 years, the present study addresses the links between personality traits and body mass index (BMI) using data from the Baltimore Longitudinal Study of Aging (BLSA). We examine the concurrent relations between personality and global (BMI) and central (waist and hip circumference, body fat) measures of adiposity. We further test whether personality is associated with weight fluctuations and the rate of change in BMI and whether BMI is associated with change in personality traits across the adult lifespan.
Personality and Abnormal Weight
Body weight is a fundamental individual difference variable that has a pervasive effect on nearly every aspect of our lives. Although most commonly implicated in physical health, adiposity contributes to a variety of psychological processes, such as well-being, identity formation, and person perception. Overweight individuals are prone to depression (Luppino et al., 2010), have poor body image (Schwartz & Brownell, 2004), are evaluated negatively by others (Crandall, 1994), and are ascribed traits based on their body size (Roehling, Roehling, & Odland, 2008). In fact, just being associated with someone who is overweight can lead to negative evaluations (Hebl & Mannix, 2003). As such, body weight contributes to how we understand ourselves, how we see others, and how others see us.
Weight and weight gain are certainly multiply determined. Adiposity varies as a function of age, sex, and socioeconomic status (Ogden et al., 2006; Yach et al., 2006), and, genetically, the fat mass and obesity associated (FTO) gene has been consistently associated with BMI (Frayling et al., 2007; Scuteri et al., 2007). In addition to these demographic and genetic influences, psychological processes contribute to an individual’s waistline. Eating can be a form of emotion regulation (Evers, Stok, & de Ridder, 2010), the inability to resist cravings contributes to binge eating (Rush, Becker, & Curry, 2009), whereas self-discipline is required to exercise regularly (Hoyt, Rhodes, Hausenblas, & Giacobbi, 2009). This line of evidence suggests that weight is a physical manifestation of processes inherent to an individual’s characteristic ways of thinking, feeling, and behaving. Thus, body weight is, in part, a reflection of the processes that define common personality traits.
The traits within the Five-Factor Model (FFM) of personality, Neuroticism, Extraversion, Openness to Experience, Agreeableness, and Conscientiousness, have been linked to health behaviors and outcomes in general (Friedman, 2008; Goodwin & Friedman, 2006; Ozer & Benet-Martínez, 2006) and to abnormal weight in particular (Brummett et al., 2006; Chapman, Fiscella, Duberstein, Coletta, & Kawachi, 2009; Terracciano et al., 2009). Of the five traits, Conscientiousness is the most consistently associated with adiposity. Across different personality measures, populations, and both self-reported and clinician-assessed weight, conscientious individuals have lower adiposity (Brummett et al., 2006; Chapman et al., 2009; Roehling et al., 2008; Sullivan, Cloninger, Przybeck, & Klein, 2007; Terracciano et al., 2009). In particular, the order and self-discipline facets of Conscientiousness are strongly associated with weight (Terracciano et al., 2009). Presumably, those who score higher on Order and Self-Discipline are leaner because they are organized and stick to their diet and meal schedule. The lifestyle choices of individuals high in Conscientiousness likely contribute to their healthy weight. These individuals, for example, are physically active (Rhodes & Smith, 2006), restrain from binge eating and drinking (Rush et al., 2009), and are less likely to have disordered eating (Bogg & Roberts, 2004).
Abnormal weight has also been associated with trait Neuroticism. Individuals who are underweight tend to score higher in proneness to negative affect than those who are in the normal weight range (Kakizaki et al., 2008; Terracciano et al., 2009). Similarly, in clinical populations, underweight individuals and those with eating disorders tend to score higher in Neuroticism (Bulik et al., 2006; Cassin & Von Ranson, 2005). On the other side of the BMI continuum, overweight and obese groups tend to have a higher prevalence of psychiatric disorders (Petry, Barry, Pietrzak, & Wagner, 2008), which suggests that such groups may also score higher on Neuroticism. Neuroticism may be associated with both ends of abnormal weight for at least two reasons: There could be a curvilinear relation between weight and Neuroticism, such that both ends of the BMI continuum are associated with higher Neuroticism and/or different aspects of Neuroticism may be associated with being overweight or underweight (see below).
There is less evidence for the association between BMI and the remaining three traits. Among Japanese participants, overweight groups scored lower on Extraversion (Kakizaki et al., 2008), whereas no association was found among Italians (Terracciano et al., 2009) or Americans (Chapman et al., 2009). Some have found this negative association between Extraversion and BMI among women, but the opposite among men (Faith, Flint, Fairburn, Goodwin, & Allison, 2001). Among men, higher Agreeableness has been associated with higher BMI (Chapman et al., 2009), but others have found the opposite (Brummett et al., 2006). Studies that have included a measure of Openness have either found a negative (Brummett et al., 2006) or no (Chapman et al., 2009; Terracciano et al., 2009) relation with BMI.
These seemingly inconsistent findings may be due, in part, to the use of different personality measures that emphasize different facets of the traits. For example, scales that tap into the more impulsive aspects of Neuroticism may be more strongly related to higher BMI, whereas scales that tap into the vulnerability aspects of this trait may be related to lower BMI. Similarly, individuals who score high on scales that emphasize the activity component of Extraversion may weigh less, whereas individuals who score high on scales that emphasize the positive emotionality components of Extraversion may weigh more. As such, it is necessary to have a detailed personality assessment that measures both the broad and narrow traits to be able to identify which aspects of personality traits are associated with abnormal weight.
Personality Traits and Weight Over Time
For most people, weight is not static, but fluctuates over time. As individuals age, their metabolic needs decrease, but their energy intake typically remains constant or increases (Bosy-Westphal et al., 2003; Elia, Ritz, & Stubbs, 2000). As a result, until old age, adults tend to gradually gain weight as they age. Similar to weight at any one given point in time, there are considerable individual differences in the extent to which BMI fluctuates across the lifespan.
Longitudinal studies on FFM personality traits and weight have been relatively sparse. To date, the only longitudinal study that assessed all the FFM domains and change in BMI over a significant period of time found that participants low on Conscientiousness increased in BMI across 14 years of middle adulthood (Brummett et al., 2006). In a three-year prospective study, Terracciano and colleagues (Terracciano et al., 2009) found virtually the same pattern of associations between personality and weight in concurrent and prospective analyses. During the three-year follow-up, however, there was little change in BMI. Long-term longitudinal studies that have multiple assessments of adiposity across the lifespan are needed to identify how personality is associated with the trajectory of BMI. In addition, to date, the one longitudinal study on personality and BMI change only assessed domain-level traits. Facet-level analyses provide a richer understanding of the relation between personality traits, behaviors and life outcomes (e.g., Paunonen, Haddock, Forsterling, & Keinonen, 2003).
In addition to the general increase in weight across the lifespan, many individuals also experience fluctuations in weight. That is, regardless of whether the weight change is deliberate (e.g., dieting) or not, some people lose and gain weight more often than others. Such cycling is associated with a variety of health conditions, such as metabolic syndrome (Zhang et al., 2005) and cardiovascular disease (Diaz, Mainous, & Everett, 2005), and health outcomes, including mortality (Diaz et al., 2005; Rzehak et al., 2007; but see Field, Malspeis, & Willett, 2009).
More research has been devoted to the consequences of weight oscillation rather than its antecedents. Evidence from related literatures, however, implicates personality in such fluctuations. For example, individuals who are not able to maintain a significant weight loss tend to score lower on traits related to Conscientiousness and impulse control and higher on traits related to Neuroticism (for a review see Elfhag & Rössner, 2005). In addition, high Neuroticism and low Conscientiousness are both associated with disordered eating (Brannan & Petrie, 2008; Tasca et al., 2009), unhealthy attitudes toward eating (Podar, Hannus, & Allik, 1999; Provencher et al., 2008), and a physically inactive lifestyle (Hoyt et al., 2009; Rhodes & Smith, 2006), all of which contribute to weight instability. We are unaware, however, of any study that has directly examined how the FFM personality traits are associated with weight fluctuations over time.
Finally, there may also be longitudinal effects in the other direction. That is, weight may contribute to personality development across adulthood. Indeed, weight has been associated with changes in a variety of psychological states. For example, obese individuals tend to be prone to subsequent depression (Luppino et al., 2010), whereas individuals who lose weight experience improved mood and quality of life (Wadden, Womble, Stunkard, & Anderson, 2002). Weight can be a very physical reminder of one’s failures at control and discipline and individuals who are unable to maintain their desired weight may come to perceive themselves as more impulsive, disorganized, and less disciplined. Similarly, individuals who suffer from anorexia tend to be highly disciplined and controlled (Claes, Vandereycken, & Vertommen, 2005). The discipline and control required to restrict eating may encourage the development of these same characteristics in the individual. To that end, we examine whether adiposity is associated with trait development across adulthood.
Current Study
To address the association between personality and weight, we take a comprehensive approach both concurrently and longitudinally. We assessed FFM personality traits at the more circumscribed facet level, as well as at the broad domain level. Recent research on facet-level analyses indicated that associations at this level do not necessarily follow their domain-level associations (Sutin, Terracciano, Deiana, Naitza et al., 2010; Sutin, Terracciano, Deiana, Uda et al., 2010). These differences reflect the heterogeneous nature of the five broad domains and speak to the importance of examining more circumscribed traits. In addition to a comprehensive approach to personality traits, we also take a comprehensive approach to adiposity. Most previous research has focused exclusively on BMI (primarily with self-reported weight), but BMI might not be the most relevant measure of adiposity to health outcomes. Therefore, in addition to BMI derived from staff-assessed weight and height, we also tested whether personality shared similar relations with three other adiposity measures: waist circumference, hip circumference, and body fat. We then move beyond concurrent associations to examine the longitudinal relations between personality and BMI in two ways. First, we used over 50 years of staff-assessed weight and height to test whether personality was associated with the rate of change of BMI across the adult lifespan. With up to 32 assessments of height and weight, data from the BLSA offer a unique opportunity to examine the trajectory of BMI across the adult lifespan and to test predictors of that trajectory. Second, because weight tends to fluctuate, we used this longitudinal data to test whether personality is associated with oscillations in weight. Fluctuations in weight and the trajectory of BMI are two different ways of quantifying weight change over time. Differential patterns of association between personality traits and these two longitudinal measures of BMI may reveal different consequences of processes inherent to the traits. Finally, we examine whether adiposity is associated with the rate of change of personality traits across the adult lifespan. With up to 16 assessments of personality, we test whether BMI predicts the trajectory of adult personality.
We hypothesized that individuals high in Neuroticism and low in Conscientiousness will have greater adiposity measured concurrently, greater fluctuations in weight over time, and larger increases in BMI across adulthood. At the facet level, we expected that participants who scored higher on impulsivity-related facets (N5: Impulsiveness, low C5: Self-Discipline, and low C6: Deliberation) will show the same pattern of associations as high Neuroticism and low Conscientiousness. In addition, because E4: Activity and C2: Order are associated with BMI concurrently (Terracciano et al., 2009), we expected active and orderly individuals to have lower adiposity, fewer weight fluctuations, and a slower rate of change. Finally, because antagonism-related traits are associated with BMI (Nabi et al., 2009) and increases in abdominal adiposity (Midei & Matthews, 2009), we expected that low Agreeableness will show a similar effect.
As noted above, average BMI has increased steadily over the past several decades (Hedley et al., 2004; Stenholm, Simonsick, & Ferrucci, 2010). That is, a 40-year-old participant who entered the BLSA in 1970 likely weighed less than a 40-year-old who entered the study in 1990. In the longitudinal models, we test and control for this potential secular trend.
Method
Participants
Community-dwelling volunteers (N = 1,988) were drawn from the BLSA, an ongoing multidisciplinary study of normal aging administered by the National Institute on Aging. The BLSA began in 1958 with a convenience sample of men, mostly college educated and predominantly White. Later recruitment has helped balance the sample by including minorities and, since 1978, women. Participants are generally healthy and highly educated (M = 16.53 years of education, SD = 2.47); the present sample is 71% White, 22% Black, and 7% other or unknown ethnicity and 50% women. Basic anthropometric measures (see below) were available on all participants since the BLSA’s inception; administration of the current personality measure (see below) started in 1989. Of participants with at least one valid assessment of personality, 89% were either active (66%) or deceased (23%). Of the remaining 11%, approximately 2% had formally withdrawn (although they are willing to participate by phone, mail, and/or home visits) and approximately 9% had dropped out, were at least one year past their due date, or were lost to follow-up.
Anthropometric assessment
Starting at the first BLSA assessment in 1958, participants’ weight and height were measured and recorded by a trained staff clinician. For participants who had at least one valid assessment of personality, there were 14,531 valid assessments of height and weight across the 50 years of the study (M assessments per participant = 7.31, SD = 5.85, range = 1 to 32). In subsequent assessments, clinicians also measured participants’ waist circumference, hip circumference, and body fat, based on skinfold thickness. In addition to examining derived BMI (calculated as kg/m2) as a continuous measure, we categorized BMI based on international standards (WHO, 2000): normal weight (BMI < 25), overweight (BMI = 25-30) and obese (BMI ≥ 30). The 17 participants who could be classified as underweight (BMI < 18.5) were grouped with the normal weight participants. In the present sample, BMI had a mean of 26.14 (SD = 4.89), waist circumference had a mean of 87.17 cm (SD = 13.32), hip circumference had a mean of 101.27 cm (SD = 8.99), and body fat had a mean of 25.63 (SD = 9.60).
Personality assessment
Personality traits were assessed with the Revised NEO Personality Inventory (NEO-PI-R), a comprehensive measure of the FFM (Costa & McCrae, 1992). The NEO-PI–R consists of 240 items answered on a 5-point Likert format ranging from strongly disagree to strongly agree. The NEO-PI–R assesses 30 facets, 6 for each dimension of the FFM. Raw scores were standardized as T-scores (M = 50, SD = 10) using combined-sex norms reported in the manual. In the current sample (on the first assessment for each participant), the internal consistencies for the five domains were .91, .87, .87, .88, and .92 for Neuroticism, Extraversion, Openness, Agreeableness, and Conscientiousness, respectively. Available longitudinal data over intervals of 10 years indicate that stability coefficients for the five factors are approximately .80 (Terracciano, Costa, & McCrae, 2006). The NEO-PI-R has a robust factor structure that has been replicated in more than 50 cultures (McCrae et al., 2005) and these traits have been associated with consequential outcomes, including income (Sutin, Costa, Miech, & Eaton, 2009), depression (Weiss et al., 2009), and indicators of physical health, such as cholesterol (Sutin, Terracciano, Deiana, Uda et al., 2010). In the current sample, the average age at which participants completed their first NEO-PI-R was 56.98 (SD = 17.02; range 19 to 96) and the average age across all NEO-PI-R assessments was 60.61 (SD = 17.26; range 20 to 96).
Statistical overview
To examine the cross-sectional associations between personality and adiposity, we selected the first personality assessment and the adiposity measures collected at that same visit. A total of 1,960 participants had anthropometric measures at the same visit as their first personality assessment. We tested for mean-level differences in personality across the three BMI categories using multivariate analysis of covariance with BMI category as the classifying variable (normal weight, overweight, obese) and controlling for sex, age, age squared, ethnicity, and education. We used post hoc tests (LSD) to contrast the normal weight group with the overweight and obese groups. We then tested whether sex and age moderated the association between personality and BMI category. In addition to categorical differences, we correlated personality with the continuous measure of BMI and three additional adiposity measures (waist and hip circumference, and body fat), controlling for the same set of covariates.
To examine whether personality is associated with weight fluctuations over time, for all participants who had at least one valid assessment of personality and two or more assessments of BMI (n = 1,779), we correlated the first assessment of personality with the standard deviation of BMI within individuals over time, controlling for sex, age, age squared, ethnicity, and education. In addition to using this simple standard deviation, we used hierarchical linear modeling (HLM; see below) to estimate the natural logarithm of the total standard deviation within each person. As with the simple standard deviation, we correlated this estimate with personality traits, controlling for the same covariates.
To test whether personality is associated with the rate of change of BMI, we used HLM (Raudenbush & Bryk, 2002; Singer & Willett, 2003) to model change in BMI across the 52 years of the longitudinal study for all participants with at least one valid personality assessment (n = 1,988). HLM is a flexible approach that can be applied to evaluate within-individual change or growth trajectories. In HLM analyses, the number and spacing of measurement observations may vary across persons, given that the time-series observations in each individual are used to estimate each individual’s trajectory (Level 1), and those individual parameters are the basis of group estimates (Level 2). Even data from individuals who were tested on only a single occasion can be used to stabilize estimates of the mean and variance. In this way, all available data can be included in the analyses. This is a major advantage of conducting analyses within the HLM framework; by contrast, missing data and varying timing pose major problems in conventional repeated measures analyses of variance (ANOVA). Furthermore, longitudinal HLM can estimate age trajectories over a broad age span with data collected in a relatively shorter time interval.
We conducted the analyses using HLM Version 6 (Raudenbush, Bryk, & Congdon, 2004). To evaluate the longitudinal trajectories, we first defined the Level 1 model and then tested possible Level 2 predictors. At Level 1, we fit a quadratic model for BMI because of the established non-linear changes in BMI across the lifespan (Drøyvold et al., 2006; Rissanen, Heliovaara, & Aromaa, 1988). At Level 2, we entered characteristics of the individual as independent variables to explain between-subjects variation in the intercept and the linear slope. Specifically, we tested sex, ethnicity, education, and the first assessment of personality as Level 2 predictors of both the intercept and linear slope. To account for secular trends, we also included the year of each participant’s first BLSA assessment, centered on the grand mean (1991), as a predictor of the intercept. Due to the number of statistical tests, we set p to .01. Finally, we centered age in decades on the grand mean (59.40 years) to minimize the correlation between the linear and quadratic terms. In the present research, the equations for the models were:
We likewise used HLM to test whether adiposity was associated with change in personality across the adult lifespan. Similar to BMI, we fit a quadratic model for personality at Level 1 because of nonlinear changes in personality across adulthood (Terracciano, McCrae, Brant, & Costa, 2005), and tested sex, ethnicity, education, and the first BMI assessment as Level 2 predictors of the linear slope. Again, to account for secular trends, we also included the year of each participant’s first personality assessment, centered on the grand mean (1995).
Results
Concurrent Associations
BMI categories
We first examined mean-level differences in personality for overweight and obese participants compared to normal-weight participants, controlling for sex, age, age squared, ethnicity, and education (see Table 1). In the present sample, approximately 45% of participants were in the normal weight range (n = 885), 38% were overweight (n = 740), and 17% were obese (n = 335). Compared with normal-weight participants, overweight and obese participants scored higher on both Neuroticism and Extraversion. In addition, overweight participants scored lower on Openness and Agreeableness and obese participants scored lower on Conscientiousness, compared to their normal-weight counterparts. At the facet-level, compared to participants of normal weight, overweight and obese participants were more impulsive (N5: Impulsiveness), warm (E1: Warmth), and assertive (E3: Assertiveness), were excitement seekers (E5: Excitement-Seeking), tended to be more conservative (low O6: Values), disorganized (low O2: Order), and were more manipulative (low A2: Straightforwardness). In addition, overweight participants tended to be quick to anger (N2: Angry Hostility), preferred to be around others (E2: Gregariousness), and were less open to aesthetics (low O2: Aesthetics) and ideas (low O5: Ideas); obese participants tended to be happier (E6: Positive Emotions), concerned for others’ welfare (A3: Altruism), but less active (low E4: Activity) and less disciplined (low C5: Self-Discipline). With the exception of the difference between normal and overweight participants on E5: Excitement-Seeking, the findings did not change when we excluded underweight participants instead of including them with the normal weight participants.
Table 1.
Mean-level Differences in Adjusted Personality Traits for Normal, Overweight, and Obese Groups
| Personality | Normal (BMI < 24.99) |
Overweight (BMI 25-29.99) |
Obese (BMI ≥ 30) |
|---|---|---|---|
| Domains | |||
| Neuroticism | 47.01 (.33) | 48.16 (.35)* | 48.78 (.53)** |
| Extraversion | 50.37 (.34) | 51.74 (.37)** | 52.38 (.56)** |
| Openness | 53.46 (.34) | 51.95 (.37)** | 53.52 (.56) |
| Agreeableness | 50.64 (.32) | 49.54 (.34)* | 49.99 (.52) |
| Conscientiousness | 50.97 (.35) | 50.40 (.37) | 49.34 (.57)* |
| Facets | |||
| N1: Anxiety | 48.03 (.33) | 48.24 (.36) | 48.26 (.54) |
| N2: Angry Hostility | 48.23 (.33) | 49.37 (.35)* | 48.13 (.54) |
| N3: Depression | 47.21 (.33) | 47.97 (.35) | 48.38 (.54) |
| N4: Self-Consciousness | 48.26 (.34) | 48.23 (.36) | 49.00 (.55) |
| N5: Impulsiveness | 46.80 (.31) | 50.00 (.34)** | 53.24 (.51)** |
| N6: Vulnerability | 47.93 (.33) | 47.93 (.35) | 47.64 (.53) |
| E1: Warmth | 49.50 (.34) | 51.04 (.36)** | 52.37 (.55)** |
| E2: Gregariousness | 50.04 (.36) | 51.53 (.39)** | 51.18 (.59) |
| E3: Assertiveness | 52.17 (.34) | 53.40 (.36)* | 54.67 (.55)** |
| E4: Activity | 52.26 (.34) | 52.11 (.36) | 50.23 (.55)** |
| E5: Excitement-Seeking | 47.66 (.31) | 48.61 (.33)* | 49.58 (.50)** |
| E6: Positive Emotions | 49.99 (.35) | 50.48 (.37) | 51.73 (.56)* |
| O1: Fantasy | 51.59 (.35) | 51.21 (.37) | 52.41 (.56) |
| O2: Aesthetics | 53.97 (.33) | 52.84 (.36)* | 53.82 (.54) |
| O3: Feelings | 51.02 (.33) | 50.69 (.35) | 51.95 (.54) |
| O4: Actions | 51.40 (.36) | 51.11 (.38) | 51.62 (.58) |
| O5: Ideas | 52.52 (.34) | 51.06 (.36)** | 52.52 (.55) |
| O6: Values | 52.23 (.34) | 50.13 (.36)** | 50.60 (.55)* |
| A1: Trust | 51.91 (.32) | 51.37 (.34) | 51.80 (.52) |
| A2: Straightforwardness | 51.02 (.33) | 49.76 (.35)* | 49.31 (.53)** |
| A3: Altruism | 49.91 (.33) | 50.06 (.36) | 51.28 (.54)* |
| A4: Compliance | 50.84 (.34) | 49.90 (.36) | 50.13 (.55) |
| A5: Modesty | 48.12 (.34) | 47.34 (.37) | 47.28 (.55) |
| A6: Tender-Mindedness | 50.63 (.33) | 49.76 (.36) | 50.51 (.54) |
| C1: Competence | 52.49 (.34) | 52.58 (.37) | 53.35 (.56) |
| C2: Order | 49.16 (.36) | 47.78 (.38)** | 47.22 (.58)** |
| C3: Dutifulness | 50.88 (.32) | 50.70 (.34) | 49.94 (.52) |
| C4: Achievement Striving | 50.86 (.36) | 50.91 (.39) | 50.16 (.59) |
| C5: Self-Discipline | 48.63 (.37) | 47.96 (.39) | 46.20 (.60)** |
| C6: Deliberation | 51.73 (.34) | 51.57 (.36) | 50.48 (.55) |
Note. N = 1,960. n = 885 for normal weight, n = 740 for overweight, and n = 335 obese. Adjusted means (standard errors) computed after controlling for age, age squared, sex, ethnicity, and education. BMI = Body Mass Index.
p < .05.
p < .01.
Sex moderated very few of these associations. Obese women scored higher on Neuroticism (F(2,1957) = 3.74, p < .05) and two of its facets, N3: Depression (F(2,1957) = 3.45, p < .05) and N4: Self-Consciousness (F(2,1957) = 3.60, p < .05) than normal-weight participants; these differences did not emerge for men. Overweight men did, however, score higher on N2: Angry Hostility than normal-weight men, a difference that did not hold for women (F(2,1957) = 3.57, p < .05). Sex did not moderate any of the other personality-BMI associations. Age did not moderate the association between BMI and the five factors.
Continuous measures of adiposity
The associations between personality and weight were consistent across the different measures of adiposity (see Table 2).1 This consistency was not surprising given that the four different measures of adiposity were highly intercorrelated (median r = .87; range .78 to .94). At the broad domain level, controlling for demographic variables (sex, age, age squared, ethnicity, and education), participants higher on Neuroticism or Extraversion had greater adiposity, as assessed through either global (e.g., BMI) or central (e.g., waist circumference) measures. In addition, those higher in Conscientiousness were leaner, as assessed through either global or central measures of adiposity. Although the categorical analyses suggested that there may be a curvilinear association between personality and adiposity, we did not find such an association between BMI and any of the five traits in the continuous analyses.
Table 2.
Partial Correlations Between Personality and Continuous Measure of Adiposity, Controlling for Sex, Age, Age Squared, Ethnicity, and Education
| Personality | Adiposity Measure |
|||
|---|---|---|---|---|
| BMI | Body Fat | Waist | Hip | |
| Domains | ||||
| Neuroticism | .07** | .06** | .06** | .08** |
| Extraversion | .09** | .09** | .09** | .07** |
| Openness | .02 | .01 | .01 | .03 |
| Agreeableness | −.03 | −.03 | −.04 | −.01 |
| Conscientiousness | −.06** | −.07** | −.07** | −.07** |
| Facets | ||||
| N1: Anxiety | −.01 | .00 | .00 | .02 |
| N2: Angry Hostility | .01 | .01 | .01 | .01 |
| N3: Depression | .03 | .03 | .02 | .04 |
| N4: Self-Consciousness | .03 | .03 | .02 | .04 |
| N5: Impulsiveness | .27** | .26** | .26** | .25** |
| N6: Vulnerability | −.02 | −.02 | −.02 | .00 |
| E1: Warmth | .12** | .13** | .12** | .12** |
| E2: Gregariousness | .05* | .06** | .07** | .05* |
| E3: Assertiveness | .11** | .12** | .11** | .10** |
| E4: Activity | −.07** | −.08** | −.08** | −.07** |
| E5: Excitement-Seeking | .07** | .05* | .07** | .02 |
| E6: Positive Emotions | .08** | .07** | .07** | .07** |
| O1: Fantasy | .04 | .04 | .05* | .05* |
| O2: Aesthetics | .01 | −.01 | −.02 | .02 |
| O3: Feelings | .04 | .03 | .02 | .04 |
| O4: Actions | .01 | .00 | −.01 | .00 |
| O5: Ideas | .02 | .02 | .02 | .04 |
| O6: Values | −.04 | −.04 | −.03 | −.03 |
| A1: Trust | .01 | .04 | .02 | .03 |
| A2: Straightforwardness | −.07** | −.09** | −.09** | −.06* |
| A3: Altruism | .05* | −.05* | .05* | .05* |
| A4: Compliance | −.04 | −.03 | −.04 | −.01 |
| A5: Modesty | −.05* | −.07** | −.05* | −.05* |
| A6: Tender-Mindedness | .01 | .00 | .01 | .01 |
| C1: Competence | .05* | .05* | .05* | .04 |
| C2: Order | −.09** | −.12** | −.11** | −.10** |
| C3: Dutifulness | −.03 | −.04 | −.04 | −.03 |
| C4: Achievement Striving | −.01 | −.03 | −.03 | −.03 |
| C5: Self-Discipline | −.08** | −.10** | −.11** | −.10** |
| C6: Deliberation | −.05* | −.05* | −.04 | −.04 |
Note. N = 1,960 for BMI; n = 1852 Body Fat, n = 1868 for waist circumference, and n = 1869 for hip circumference. BMI = Body Mass Index.
p < .05.
p < .01.
The more circumscribed facet-level analyses revealed which aspects of the traits were the most strongly related to adiposity (see Table 2). Consistent with previous research (Terracciano et al., 2009), the strongest association was for N5: Impulsiveness: Those who were highly impulsive were the most likely to be overweight. Also consistent with previous research, active (E4: Activity), orderly (C2: Order), and self-disciplined (C5: Self-Discipline) participants were leaner, whereas assertive (E3: Assertiveness) participants were heavier. Finally, following the domain-level associations, participants who scored higher on the other four facets of Extraversion (E1: Warmth, E2: Gregariousness, E5: Excitement-Seeking, E6: Positive Emotions) were heavier; participants higher on A2: Straightforwardness were leaner. These associations revealed clinically-meaningful differences in weight. For example, participants who scored in the top 10% of N5: Impulsiveness weighed, on average, over 11 Kg more than those who scored in the lowest 10% of this trait. Likewise, participants who scored high on C2: Order weighed about 4.5 Kg less than those who scored low on Order.2 Additional analyses indicated a curvilinear relation between O2: Aesthetics and BMI such that those lower on this trait were more likely to be overweight than lean or obese (β = .07, p < .01) and a curvilinear relation between E3: Assertiveness and BMI such that this association was weaker among those who scored lower on this facet (β = −.04, p < .05). Finally, in all of the concurrent analyses the pattern of associations was virtually identical when we repeated the analyses using the mean across all assessments of personality and adiposity.
Longitudinal Relations
We next turn to whether personality was associated with weight fluctuations and whether personality traits predicted the rate of change in BMI across the adult lifespan.
Weight fluctuations
Personality was associated with weight fluctuations over time (see Table 3). Controlling for the demographic covariates, participants with a dispositional proneness to experience negative emotions had greater fluctuations in weight. In particular, those who were highly impulsive (N5: Impulsiveness) and prone to depression (N3: Depression) had more difficulty maintaining a steady weight. By contrast, participants who scored high on Conscientiousness, and particularly the facets of C2: Order, C3: Dutifulness and C5: Self-Discipline, were able to maintain a more steady weight. Finally, highly active (E4: Activity) participants were also less prone to weight fluctuations, perhaps due, in part, to their physically active lifestyles. We found virtually identical associations between weight fluctuation and personality using either the simple standard deviation or the estimates from HLM (see Table 3). These associations between personality and BMI fluctuations remained significant after controlling for initial BMI.
Table 3.
Partial Correlations Between Personality and BMI Fluctuations, Controlling for Sex, Age, Age Squared, Ethnicity, and Education
| Personality | BMI Standard Deviation |
|
|---|---|---|
| Simple | HLM | |
| Domains | ||
| Neuroticism | .07** | .07** |
| Extraversion | −.02 | −.02 |
| Openness | −.01 | −.01 |
| Agreeableness | −.01 | −.01 |
| Conscientiousness | −.08** | −.09** |
| Facets | ||
| N1: Anxiety | .01 | .01 |
| N2: Angry Hostility | .01 | .02 |
| N3: Depression | .06** | .07** |
| N4: Self-Consciousness | .03 | .03 |
| N5: Impulsiveness | .17** | .19** |
| N6: Vulnerability | .03 | .02 |
| E1: Warmth | .04 | .03 |
| E2: Gregariousness | .01 | .00 |
| E3: Assertiveness | −.01 | −.01 |
| E4: Activity | −.12** | −.11** |
| E5: Excitement-Seeking | .00 | .01 |
| E6: Positive Emotions | −.02 | .00 |
| O1: Fantasy | .01 | .01 |
| O2: Aesthetics | −.01 | −.01 |
| O3: Feelings | −.01 | −.01 |
| O4: Actions | −.03 | −.02 |
| O5: Ideas | −.01 | −.01 |
| O6: Values | −.01 | −.02 |
| A1: Trust | .00 | −.01 |
| A2: Straightforwardness | −.04 | −.05 |
| A3: Altruism | .01 | .01 |
| A4: Compliance | .00 | .01 |
| A5: Modesty | .03 | .01 |
| A6: Tender-Mindedness | −.02 | −.01 |
| C1: Competence | −.05 | −.05 |
| C2: Order | −.07** | −.08** |
| C3: Dutifulness | −.07** | −.07** |
| C4: Achievement Striving | −.03 | −.04 |
| C5: Self-Discipline | −.09** | −.09** |
| C6: Deliberation | −.04 | −.04 |
Note. N = 1,779. BMI = Body Mass Index. HLM = Hierarchical Linear Modeling.
p < .01.
Rate of change
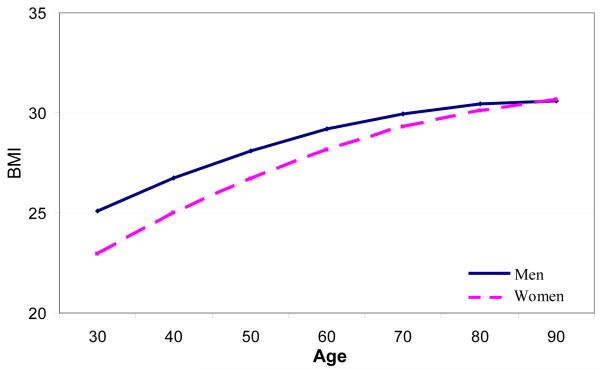
Using HLM, we estimated the rate of change in BMI for all participants who also had at least one personality assessment. In this sample, there were 14,531 valid assessments of height and weight, with an average of 7.31 assessments per participant (SD = 5.85, range = 1 to 32). Both the linear slope and the quadratic slope were significant, indicating non-linear changes in BMI across the adult lifespan (see Table 4). Specifically, BMI increases most during young and middle adulthood. The estimated trajectories of BMI, plotted separately for men and women, are shown in Figure 1. The intercept and slope were correlated .44 (p < .01), which indicates that those who weighed more around age 60 increased more on weight over time. Multi-level modeling analyses, such as HLM, control for the correlation between the intercept and the slope (Verbeke & Molenberghs, 2000).
Table 4.
HLM Coefficients and Variance Estimates of Intercept, Linear, and Quadratic Equations Predicting BMI From Age in Decades
| Component | HLM Estimates |
|---|---|
| σ2: Residual within-subject variance | 1.51 (.03)** |
| Intercept | |
| γ00: Mean | 28.07 (.74)** |
| u0: Variance | 20.92 (.10)** |
| Linear Slope | |
| γ 10: Mean | 1.33 (.25)** |
| u 1: Variance | 1.45 (.03)** |
| Quadratic Slope | |
| γ20: Mean | −.015 (.00)** |
Note. N = 1,988. Standard errors are shown in parenthesis. HLM = hierarchical linear modeling; BMI = Body Mass Index.
p < .01.
Figure 1.
Estimated trajectory of BMI from age 30 to 90, plotted separately for men and women.
Sex and ethnicity had a significant effect on both the intercept and slope (see Table 5). At the grand-mean of age (M = 59.40), men, on average, had higher BMI than women, and Black participants had higher BMI than White participants. Men and Black participants, however, had a slower rate of change than women and White participants, respectively. Also, as expected, there was evidence of secular trends, such that participants who entered the study more recently had higher BMI than participants who entered the study at an earlier point in time. Education did not have a significant effect on the intercept or slope of BMI.
Table 5.
Demographic and Personality Predictors of the Intercept and Slope of BMI
| Predictor | Intercept | Slope |
|---|---|---|
| Demographics | ||
| Sex (Males) | 1.07 (.23)** | −.04 (.02)** |
| Ethnicity (Black) | 2.04 (.29)** | −.04 (.01)** |
| Ethnicity (Other) | −.97 (.47) | −.05 (.02) |
| Education | −.11 (.04) | .00 (.00) |
| Time of measurement | .03 (.01)** | -- |
| Personality | ||
| Neuroticism | .053 (.010)**a | .003 (.002) |
| Extraversion | .068 (.009)**a | .000 (.001) |
| Openness | .041 (.009)**a | .002 (.002) |
| Agreeableness | −.046 (.010)**a | −.011 (.002)**a |
| Conscientiousness | −.025 (.009)**a | .000 (.001) |
| N1: Anxiety | .012 (.010) | −.001 (.002) |
| N2: Angry Hostility | .033 (.010)**a | .003 (.001) |
| N3: Depression | .031 (.010)** | .002 (.002) |
| N4: Self-Consciousness | .024 (.010) | .000 (.001) |
| N5: Impulsiveness | .015 (.010)**a | .007 (.002)**a |
| N6: Vulnerability | −.011 (.010) | .002 (.002) |
| E1: Warmth | .054 (.010)**a | .002 (.002) |
| E2: Gregariousness | .024 (.009)**a | .002 (.002) |
| E3: Assertiveness | .059 (.010)**a | .002 (.002) |
| E4: Activity | .012 (.010) | −.009 (.001)** |
| E5: Excitement-Seeking | .080 (.010)**a | .005 (.002)**a |
| E6: Positive Emotions | .063 (.009)**a | −.006 (.001)** |
| O1: Fantasy | .058 (.009)**a | .002 (.001) |
| O2: Aesthetics | −.007 (.010) | −.003 (.001) |
| O3: Feelings | .059 (.010)**a | .005 (.002)** |
| O4: Actions | .021 (.009) | .003 (.001) |
| O5: Ideas | .019 (.010) | .002 (.002) |
| O6: Values | .014 (.010) | −.002 (.002) |
| A1: Trust | −.034 (.010)**a | −.015 (.002)**a |
| A2: Straightforwardness | −.054 (.010)**a | −.005 (.002)** |
| A3: Altruism | .024 (.010) | −.004 (.002) |
| A4: Compliance | −.053 (.010)**a | −.007 (.002)**a |
| A5: Modesty | −.027 (.010)**a | −.003 (.001) |
| A6: Tender-mindedness | −.013 (.010) | −.006 (.002)** |
| C1: Competence | .032 (.010)**a | .003 (.002) |
| C2: Order | −.034 (.009)**a | .001 (.001) |
| C3: Dutifulness | −.040 (.010)**a | −.003 (.002) |
| C4: Achievement Striving | −.002 (.009) | −.003 (.001) |
| C5: Self-Discipline | −.030 (.009)**a | −.004 (.001)** |
| C6: Deliberation | −.028 (.010)**a | .008 (.002)** |
Note. N = 1,988. Standard errors are shown in parenthesis. Coefficients are applied to (age - mean age) in decades. Time of measurement is year of first assessment centered around the grand mean (1991). BMI = Body Mass Index.
Personality traits that replicated across the four other measurements of adiposity.
p < .01.
Turning to our analyses of interest, we tested whether personality traits had a significant effect on both the intercept and the linear slope (see Table 5). Although we focused on the effect of personality on the intercept and slope of BMI, the findings from the HLM analyses were similar across the other adiposity measures. Across these measures (BMI, hip circumference, waist circumference, and body fat), the median correlation among the estimates for the traits on the intercept was .91 (range .84 to .98) and the median correlation among the estimates for the traits on the slope was .86 (range .74 to .90). Table 5 indicates which findings were significant across all four of the adiposity measures.
Broadly consistent with the concurrent analyses, higher scores on Neuroticism, Extraversion, and Openness were associated with being heavier, whereas higher scores on Agreeableness and Conscientiousness were associated with being leaner. Most of the facets that had a significant effect on the intercept followed their domain-level associations. There were, however, a few notable exceptions. Although N2: Hostility, N3: Depression, and N5: Impulsiveness were associated with higher BMI, N6: Vulnerability was not related to BMI. In addition, participants higher on C1: Competence had higher BMI, whereas most of the other facets within Conscientiousness were associated with lower BMI. Of note, with the exception of E4: Activity, all of the associations between personality and the intercept of BMI replicated the concurrent analyses.
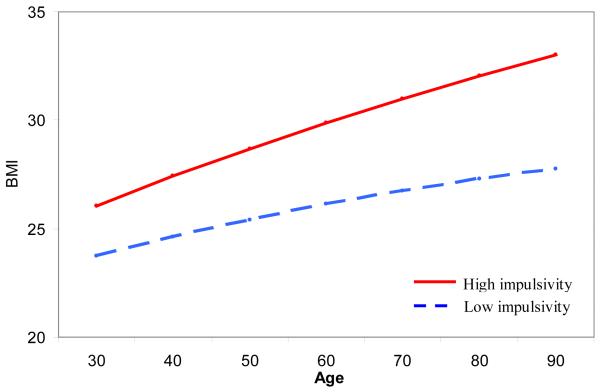
At the domain level, Agreeableness was associated with the rate of change of BMI across the adult lifespan: Individuals high in antagonism (low Agreeableness; see Figure 2) increased more in BMI over time. In particular, the BMI of participants who were cynical (low A1: Trust), aggressive (low A4: Compliance), and arrogant (low A5: Modesty) increased more in adiposity. In addition, the emotional aspects of impulsivity (N5: Impulsiveness and E5: Excitement-Seeking) were also associated with greater increases in adiposity. For example, on average, at age 30, those who score one standard deviation above the mean on impulsivity had a BMI that was approximately 2.30 points higher than those who scored one standard deviation below the mean on this trait. By age 90, this gap increased to a 5.22 BMI point difference (see Figure 3).
Figure 2.
Estimated trajectory of BMI for participants 1 SD above and below the mean on Agreeableness. In plotting the trajectory, we accounted for the normative increase in Agreeableness across the adult lifespan (approximately 1 T-score point per decade; Terracciano, McCrae, Brant, & Costa, 2005).
Figure 3.
Estimated trajectory of BMI for participants 1 SD above and below the mean on N5: Impulsiveness. In plotting the trajectory, we accounted for the normative decline in N5: Impulsiveness across the adult lifespan (approximately 1 T-score point per decade; Terracciano, McCrae, Brant, & Costa, 2005).
Finally, we tested whether BMI was associated with change in personality. Detailed information about normative changes in personality across the adult lifespan in the BLSA can be found in Terracciano and colleagues (2005). Using HLM, we estimated the rate of change in personality and then tested whether BMI was associated with this trajectory.3 There were 6,824 valid assessments of personality, with an average of 3.42 assessments per participant (SD = 2.47, range = 1 to 16). Adiposity was primarily unrelated to change in personality: BMI was not associated with the slope of any of the five broad domains. The other three measures of adiposity were also unrelated to change in the five factors. At the facet level, higher BMI was associated with decreases in N5: Impulsiveness (b = −.08 [SE = .02], p < .01). This effect replicated across waist circumference, hip circumference, and body fat. BMI was unrelated to change in any of the other facets. Sex did not moderate the association between BMI and the trajectory of personality.
Discussion
Using data from a longitudinal study of aging that spanned more than 50 years, we examined the associations between a comprehensive measure of FFM personality traits and multiple anthropometric measures. In both the continuous and categorical classification of BMI, and three additional measures of adiposity, participants high on Neuroticism or Extraversion weighed more, whereas conscientious participants were leaner. High Neuroticism and low Conscientiousness were also associated with more weight fluctuations and, across the adult lifespan, low Agreeableness and the emotional aspects of trait impulsivity were associated with greater increases in BMI. BMI was primarily unrelated to changes in personality traits.
Concurrent Associations between Personality and Weight
Individuals high in Neuroticism or low in Conscientiousness are vulnerable to being overweight or obese. In particular, the facets of these traits related to impulsivity – N5: Impulsiveness and (low) C5: Self-Discipline – were consistently associated with greater adiposity. Individuals with this constellation of traits tend to give in to temptation and lack the discipline to stay on task amid difficulties or frustration (Costa & McCrae, 1992). To maintain a healthy weight it is typically necessary to have a healthy diet and a sustained program of physical activity, both of which require commitment and restraint. Such control may be difficult for highly impulsive individuals. In addition to these impulsivity-related traits, across both the concurrent and longitudinal analyses, C2: Order was also consistently associated with adiposity. Such individuals may be leaner because they are organized and stick to a regular diet and meal schedule, which minimize the intake of extra calories.
Neuroticism and Conscientiousness are both associated with the health-risk behaviors that contribute to abnormal weight. Individuals high in Neuroticism and low in Conscientiousness are more likely to smoke (Terracciano & Costa, 2004), abuse drugs (Terracciano, Löckenhoff, Crum, Bienvenu, & Costa, 2008), be physically inactive (Rhodes & Smith, 2006), and binge eat and drink (Rush et al., 2009). Consistent with these more recent studies, a meta-analysis found that Conscientiousness correlated negatively with health behaviors that are among the leading behavioral contributors to mortality, including disordered eating, physical inactivity, alcohol and drug use, and smoking (Bogg & Roberts, 2004). Individuals high in Neuroticism, in addition to their other health-risk behaviors, tend to be overly concerned with their shape and weight and, despite their attempts at restraint, tend to lose control over their food intake (Provencher et al., 2008). One outcome of these maladaptive cognitive and behavioral patterns is difficulty with weight regulation.
The physiological consequences to this type of lifestyle do not end with obesity. Individuals high on Neuroticism, in particular the impulsiveness facet, and low on Conscientiousness have elevated triglycerides (Sutin, Terracciano, Deiana, Uda et al., 2010), hypertension (Goodwin, Cox, & Clara, 2006; Goodwin & Friedman, 2006), and clinically-elevated levels of inflammation (Sutin, Terracciano, Deiana, Naitza et al., 2010), even after controlling for differences in adiposity. Abnormal weight may be one mechanism that partially mediates the relation between personality and these health outcomes. For example, individuals high in Neuroticism or low in Conscientiousness weigh more, which, in turn, contributes to their chronic inflammation (Sutin, Terracciano, Deiana, Naitza et al., 2010).
Although we found that higher Neuroticism scores were consistently associated with greater weight, both across different ways of measuring adiposity and longitudinally as well as in the cross-sectional analyses, other studies have found the opposite relation (Bulik et al., 2006; Kakizaki et al., 2008). There may be at least two reasons for this discrepancy. First, there could be a curvilinear association between Neuroticism and weight; those high on Neuroticism may be particularly susceptible to abnormal weight, on either side of the BMI continuum. In the current research we did not find such a curvilinear effect, but we did not have enough underweight participants to sufficiently test this hypothesis. Second, different aspects of Neuroticism may share opposite relations with BMI. For example, impulsive individuals have a hard time controlling their urges, including the urge for extra helpings of food. In contrast, individuals high on self-consciousness or vulnerability may be much more sensitive about their weight (Swami, Hadji-Michael, & Furnham, 2008) and more restrictive in their eating (Heaven, Mulligan, Merrilees, Woods, & Fairooz, 2001). As such, the different emotional aspects of Neuroticism may have different outcomes with regard to weight. These potential differences point to the importance of examining personality traits at a more specific level of analysis in addition to the five broad domains.
At this more circumscribed facet-level, the cross-sectional findings in the current study were similar to those from a large sample from Sardinia, Italy (Terracciano et al., 2009). Specifically, the strongest positive association with weight in both studies was with N5: Impulsiveness, whereas the strongest negative association in both studies was with C2: Order: Those who are unable to resist temptation and have a difficult time following regular meal rhythms may find it more difficult to maintain a healthy weight. In addition, other facets of personality most consistently related to different measures of adiposity in the Sardinian sample were also apparent in the current sample, including E3: Assertiveness, E4: Activity, and C5: Self-Discipline. This consistency across studies is remarkable, given the cultural and demographic differences between participants in the two samples: the Sardinian sample is drawn from a rural population with relatively lower education, whereas participants from the BLSA sample are from a major urban center and are generally well-educated. This consistency suggests that many associations between personality and adiposity transcend sample and cultural differences.
The positive association between adiposity and Extraversion was unexpected. Previous research has found no association (Chapman et al., 2009; Terracciano et al., 2009), a negative association (Kakizaki et al., 2008), or sex-specific associations (Brummett et al., 2006; Faith et al., 2001) between adiposity and Extraversion at the domain level. In the present study, this association was consistent across different ways of measuring adiposity in the cross-sectional analyses and over time in the longitudinal analyses. At the facet-level, although some of the associations were expected based on previous research (i.e., E3: Assertiveness and E4: Activity), the consistent association between adiposity and the emotional aspects of this trait was not. Overall, it is difficult to draw any conclusions about Extraversion, given the inconsistent findings across studies.
Personality and Longitudinal Changes in Weight
Although weight tends to increase gradually across the lifespan, there are considerable individual differences in the rate and magnitude of change. After accounting for demographic differences, in the present study, impulsive individuals, in particular those who are unable to resist temptation (N5: Impulsiveness) and those who enjoy taking risks (E5: Excitement-Seeking) and individuals who are antagonistic, in particular those who are cynical (low A1: Trust), competitive and aggressive (low A4: Compliance), gained more weight. In addition to weight gain over time, the analyses of weight fluctuations revealed a pattern of associations between personality and adiposity over time not captured by the HLM analyses. As described below, the differences between the HLM and the fluctuation analyses suggest that processes inherent to traits may have different implications for weight across the adult lifespan.
In the HLM analyses, the emotional aspects of impulsivity – N5: Impulsiveness and E5: Excitement-Seeking – were consistently associated with greater weight gain over time across the four measures of adiposity. Such individuals give in to temptation and seek out highly stimulating environments; food and alcohol may be one form of stimulation. And, in fact, sensation seeking has been linked with binge drinking (McAdams & Donnellan, 2009) and overeating (Davis et al., 2007). Such behavior may, over time, contribute to weight gain.
Evidence is growing for the role of antagonism-related traits in weight gain across the lifespan. Highly antagonistic individuals, starting in adolescence, gain weight quicker than less antagonistic individuals (Midei & Matthews, 2009), a pattern that continues through old age (Räikkönen, Matthews, Kuller, Reiber, & Bunker, 1999). This weight gain may be due, in part, to their behavioral patterns. For example, hostile individuals tend to continue eating, even after they feel satiated (Van Den Bree, Przybeck, & Cloninger, 2006). The cumulative effect over the lifetime may end in the cardiovascular problems that are more common to individuals scoring high on measures of antagonism (Siegman, Townsend, Cahid Civelek, & Blumenthal, 2000; Smith & Ruiz, 2002; Tindle et al., 2009).
The pathway from personality traits to weight gain is likely complex and mediated by physiological mechanisms, as well as behavioral ones. In particular, greater physiological reactivity to stress may also contribute to increases in adiposity. Neuroticism-related traits are associated with greater cortisol reactivity (Mangold & Wand, 2006; Tyrka et al., 2008), and such reactivity may lead to weight gain (Vicennati, Pasqui, Cavazza, Pagotto, & Pasquali, 2009). Likewise, antagonistic individuals have a reactive and sustained physiological response to acute stress. Following an acute stressor, for example, antagonistic individuals show a sharp increase in blood pressure and circulating interleukin-6 (a marker of inflammation), which remain elevated long after the stressor has been removed (Brydon et al., 2010). Such inflammatory stress responses may be implicated in weight gain (Engström et al., 2003).
To the best of our knowledge, we are the first to examine whether personality is associated with fluctuations in weight over time. Interestingly, our pattern of associations fits nicely with the characteristics of these traits. As discussed above, both Neuroticism and (low) Conscientiousness are associated with unhealthy eating patterns (Provencher et al., 2008; Tasca et al., 2009). Individuals who have difficulty managing their weight often attempt to reduce their weight through diet and other lifestyle changes. Despite weight loss accomplishments, however, relapses are common. Our data suggest that those scoring high on Neuroticism and low on Conscientiousness are more likely to go through such cycles of weight gain and loss. At the more specific facet level, both impulsivity and depression were associated with greater weight fluctuations. Impulsive individuals often alternate between restricting their food intake and periods of uninhibited eating (Jansen et al., 2009) and changes in appetite are one of the core characteristics of depression (American Psychiatric Association, 1994). Thus, it is not surprising that those who give in to temptation and those with a predisposition to experience depression cannot maintain a steady weight. Finally, of the 30 facets, E4: Activity and C5: Self-Discipline have the strongest associations with exercise behavior (Hoyt et al., 2009) and these two facets shared the strongest negative associations with weight fluctuations: Active and disciplined individuals maintain a more steady weight as they age. Both weight fluctuations and personality have been implicated in the same health outcomes, such as metabolic syndrome and mortality; such fluctuations may be one mediator between traits and these outcomes.
These two different ways to assess how adiposity changes over time highlights differences between traits that are conceptually and empirically related. For example, trait anxiety and trait depression are highly correlated (r = .66 in the current sample), but anxiety and depression are distinguishable constructs that have unique correlates (Watson et al., 1995). And, indeed, depression and anxiety had different longitudinal associations with BMI: Depression was associated with weight fluctuations, anxiety was not. Interestingly, the depression facet of Neuroticism measures the susceptibility to negative mood, not the physical symptoms of depressed mood (e.g., changes in appetite). Yet, this trait had the expected relation with weight fluctuations, but was unrelated to a systematic increase in weight. In contrast, the physical manifestations of anxiety do not include changes in appetite, and this trait was not associated with weight fluctuations or systematic increases in weight over time.
In addition, our analysis of weight fluctuations informs the association between antagonism and weight gain. As noted above, consistent with previous research on anger-related traits, antagonism was associated with weight gain across adulthood. The fluctuation analyses, however, indicated that antagonism was unrelated to deviations in weight. Taken together, these two sets of analyses suggest that antagonistic individuals gradually gain weight over time rather than gaining and losing, as is the case with other traits.
Finally, we found little evidence that weight contributes to changes in personality across adulthood. BMI was unrelated to change in the five broad traits over time and only one effect emerged at the facet level: Participants with higher BMI declined more on N5: Impulsiveness over time. This association likely reflects regression to the mean in that the heaviest participants were also the most impulsive. Thus, over time, these participants’ impulsivity scores declined the most. The lack of significant effect of weight on personality change may be due to the high level of trait stability in this adult sample, with intra-individual variability accounting for less than 15% of the variance (Terracciano et al., 2005). Further, after accounting for transient error (Chmielewski & Watson, 2009), there may be little remaining variance to be explained by other factors. Research on adolescents and young adults, a time when personality is less stable, may be more fruitful for testing how weight may shape personality traits over time.
Implications, Strengths, Limitations, and Future Directions
A myriad of health consequences are associated with abnormal weight. Weight, however, is not only important for physical health, but can also have psychological consequences with implications for mental health as well. For example, an individual’s weight, either actual or perceived, has an effect on well-being and other personality processes, such as self-esteem, with increasing weight associated with lower self-esteem (Miller & Downey, 1999). Further, obesity is associated with subsequent depression (Luppino et al., 2010), whereas weight loss is associated with improved mood and quality of life (Wadden, Womble, Stunkard, & Anderson, 2002). As such, individual differences in weight are one characteristic of the person that has implications not just for physical health outcomes, but for how individuals understand and feel about themselves.
In addition to self-perception, body weight and fat distribution may bias person perception. Body weight is a highly visible individual difference variable that plays a role in how we perceive other people. This perception is not limited to physical size, but expands to other characteristics about the person, such as social economic status and personality. Ascribing traits to others based on their body size is not a new concept. Earlier in our history when food was scarcer, excess weight was considered a symbol of affluence, whereas today, in most western societies, obesity is more prevalent among the less affluent. More relevant to this study, personality traits are often ascribed to individuals based on their weight. As with other stereotypes (Terracciano, Abdel-Khalak, Ádám, Adamovová, Ahn, Ahn, et al., 2005), these stereotypes are often highly exaggerated or inaccurate, but have significant consequences. Overweight and obese individuals, for example, earn lower wages, face prejudice and unsatisfactory treatment from health care providers, and are portrayed negatively in the media (see Puhl & Heuer, 2009 for a comprehensive review). The present research gives a point of reference for assessing such stereotypes.
Identifying the trait profile associated with abnormal weight may help to inform future intervention research. Although personality traits are considered basic tendencies that are resistant to change, the expression of these traits, or their characteristic adaptations, is modifiable. As such, interventions that aim to modify characteristic adaptations may be the most effective. For example, individuals high on impulsivity and low on Conscientiousness may benefit most from interventions that stress menu planning and regular meal schedules. In addition, knowing an individual’s full trait profile will help with differential treatment planning. Interventions that take into account individual differences in preferences for exercise setting, motives, and potential barriers to success may achieve better treatment outcomes. For example, lifestyle and exercise interventions that are done in a group setting may be more effective for extroverts than for introverts.
This study has several strengths. With a large sample size and clinician-assessed anthropometric measurements spanning more than 50 years, we examined the longitudinal associations between a comprehensive set of FFM personality traits and BMI across the adult lifespan. In addition to BMI, we replicated the associations with three additional measures of adiposity. Our findings were robust in that personality shared the same relations with adiposity across four different ways of measuring it.
Despite these strengths, the current research had some limitations. One major concern is that our educated sample is not representative and thus the findings may not be generalizable. As noted above, however, many of the findings were consistent with findings from very different, more diverse populations. Another potential limitation is that with a comprehensive FFM measure of personality traits and multiple anthropometric measures, we necessarily conducted a large number of statistical tests, increasing the possibility of Type 1 errors. Although certainly a legitimate concern, several factors help to alleviate this limitation. The findings were largely consistent with our hypotheses derived from the literature on personality and weight. Further, we found a similar pattern of associations both across the four different measures of adiposity in cross-sectional analyses and longitudinal analyses. We also focused primarily on the findings that were consistent across methods and with previous research.
A final limitation is that we did not examine whether deliberate changes in weight have an effect on personality development. Gains and losses in weight have an impact on perceptions of the self (Blaine, Rodman, & Newman, 2007; Burgmer et al., 2007), as well as perceptions of body image (Foster, Wadden, & Vogt, 1997; Walker, Gately, Bewick, & Hill, 2003). Whether these weight changes would also have a significant effect on the individual’s personality traits is yet unknown. For example, obesity may increase proneness to anxiety, depression, and self-consciousness, whereas healthy weight loss may reduce these tendencies. Future research would benefit from testing whether substantial gains or losses in weight have a significant effect on one’s personality traits, especially during adolescence and young adulthood.
Obesity is a major public health crisis that has multiple antecedents. Certainly many factors, other than psychological, have contributed to the recent societal increase in weight. Yet, even after controlling for major demographic and genetic risk factors, personality traits remain significant predictors of adiposity (Chapman et al., 2009; Terracciano et al., 2009). In fact, personality has an effect on BMI that is of similar or greater magnitude than that of socio-economic status (Chapman et al., 2009) or the FTO-variant (Terracciano et al., 2009). The cognitive, emotional, and behavioral patterns associated with personality traits likely contribute to unhealthy weight and difficulties with weight management. Identifying the personality traits associated with obesity may help to elucidate the role of personality traits in disease progression.
Acknowledgement
This research was supported entirely by the Intramural Research Program of the NIH, National Institute on Aging.
Footnotes
With the exception of Neuroticism, the pattern of correlations was similar for waist-to-hip ratio as the other measures of adiposity.
We compared the mean weight of participants in the top and bottom 10% of the distribution on these two traits, controlling for sex, age, age squared, ethnicity, education, and height.
As an alternative longitudinal approach, we used cross-lagged models (Ferrer & McArdle, 2003; Jöreskog, 1979) to test whether personality and adiposity mutually influenced each other over time. Due to complexities in the BLSA data (i.e., data were not collected in waves and there is unequal spacing over time and unequal assessments across participants), we used the first and last assessment of personality and adiposity (N = 1,413), controlling for interval length (M = 10.05, SD = 4.80; range = 1.01-19.87), as well as the covariates included in all other analyses (sex, age, ethnicity, education). Consistent with the HLM analyses, BMI was unrelated to change in the five factors across the first and last assessments. Also consistent with the HLM analyses, we confirmed that individuals who scored low in Agreeableness gained more weight over time (γ = −.03, p < .05). In addition, we found that Neuroticism predicted an increase in BMI between the two assessments (γ = .03, p < .05). Results from analyses limited to assessments that ranged between six and 10 years apart (N = 806) were essentially the same as from the analyses on the first and last assessments of personality.
References
- American Psychiatric Association, A. P. Diagnostic and statistical manual of mental disorders. 4th ed American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Blaine BE, Rodman J, Newman JM. Weight loss treatment and psychological well-being: A review and meta-analysis. Journal of Health Psychology. 2007;12:66–82. doi: 10.1177/1359105307071741. [DOI] [PubMed] [Google Scholar]
- Bogg T, Roberts BW. Conscientiousness and health-related behaviors: A meta-analysis of the leading behavioral contributors to mortality. Psychological Bulletin. 2004;130:887–919. doi: 10.1037/0033-2909.130.6.887. [DOI] [PubMed] [Google Scholar]
- Bosy-Westphal A, Eichhorn C, Kutzner D, Illner K, Heller M, Müller MJ. The age-related decline in resting energy expenditure in humans is due to the loss of fat-free mass and to alterations in its metabolically active components. Journal of Nutrition. 2003;133:2356–2362. doi: 10.1093/jn/133.7.2356. [DOI] [PubMed] [Google Scholar]
- Brannan ME, Petrie TA. Moderators of the body dissatisfaction-eating disorder symptomatology relationship: Replication and extension. Journal of Counseling Psychology. 2008;55:263–275. [Google Scholar]
- Brummett BH, Babyak MA, Williams RB, Barefoot JC, Costa PT, Siegler IC. NEO personality domains and gender predict levels and trends in body mass index over 14 years during midlife. Journal of Research in Personality. 2006;40:222–236. [Google Scholar]
- Brydon L, Strike PC, Bhattacharyya MR, Whitehead DL, McEwan J, Zachary I, et al. Hostility and physiological responses to laboratory stress in acute coronary syndrome patients. Journal of Psychosomatic Research. 2010;68:109–116. doi: 10.1016/j.jpsychores.2009.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulik CM, Sullivan PF, Tozzi F, Furberg H, Lichtenstein P, Pedersen NL. Prevalence, heritability, and prospective risk factors for anorexia nervosa. Archives of General Psychiatry. 2006;63:305–312. doi: 10.1001/archpsyc.63.3.305. [DOI] [PubMed] [Google Scholar]
- Burgmer R, Petersen I, Burgmer M, De Zwaan M, Wolf AM, Herpertz S. Psychological outcome two years after restrictive bariatric surgery. Obesity Surgery. 2007;17:785–791. doi: 10.1007/s11695-007-9144-9. [DOI] [PubMed] [Google Scholar]
- Cassin SE, Von Ranson KM. Personality and eating disorders: A decade in review. Clinical Psychology Review. 2005;25:895–916. doi: 10.1016/j.cpr.2005.04.012. [DOI] [PubMed] [Google Scholar]
- Chapman BP, Fiscella K, Duberstein P, Coletta M, Kawachi I. Can the influence of childhood socioeconomic status on men’s and women’s adult body mass be explained by adult socioeconomic status or personality? Findings from a national sample. Health Psychology. 2009;28:419–427. doi: 10.1037/a0015212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chmielewski M, Watson D. What is being assessed and why it matters: The impact of transient error on trait research. Journal of Personality and Social Psychology. 2009;97:186–202. doi: 10.1037/a0015618. [DOI] [PubMed] [Google Scholar]
- Claes L, Vandereycken W, Luyten P, Soenens B, Pieters G, Vertommen H. Personality prototypes in eating disorders based on the big five model. Journal of Personality Disorders. 2006;20:401–416. doi: 10.1521/pedi.2006.20.4.401. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr., McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and the NEO Five-Factor Inventory (NEO-FFI) professional manual. Psychological Assessment Resources; Odessa, FL: 1992. [Google Scholar]
- Crandall CS. Prejudice against fat people: Ideology and self-interest. Journal of Personality and Social Psychology. 1994;66:882–894. doi: 10.1037//0022-3514.66.5.882. [DOI] [PubMed] [Google Scholar]
- Davis C, Patte K, Levitan R, Reid C, Tweed S, Curtis C. From motivation to behaviour: A model of reward sensitivity, overeating, and food preferences in the risk profile for obesity. Appetite. 2007;48:12–19. doi: 10.1016/j.appet.2006.05.016. [DOI] [PubMed] [Google Scholar]
- Diaz VA, Mainous AG, Iii, Everett CJ. The association between weight fluctuation and mortality: Results from a population-based cohort study. Journal of Community Health. 2005;30:153–165. doi: 10.1007/s10900-004-1955-1. [DOI] [PubMed] [Google Scholar]
- Drøyvold WB, Nilsen TIL, Krüger Ø, Holmen TL, Krokstad S, Midthjell K, et al. Change in height, weight and body mass index: Longitudinal data from the HUNT Study in Norway. International Journal of Obesity. 2006;30:935–939. doi: 10.1038/sj.ijo.0803178. [DOI] [PubMed] [Google Scholar]
- Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obesity Reviews. 2005;6:67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- Elia M, Ritz P, Stubbs RJ. Total energy expenditure in the elderly. European Journal of Clinical Nutrition. 2000;54:S92–S103. doi: 10.1038/sj.ejcn.1601030. [DOI] [PubMed] [Google Scholar]
- Engström G, Hedblad B, Stavenow L, Lind P, Janzon L, Lindgärde F. Inflammation-sensitive plasma proteins are associated with future weight gain. Diabetes. 2003;52:2097–2101. doi: 10.2337/diabetes.52.8.2097. [DOI] [PubMed] [Google Scholar]
- Evers C, Stok F, de Ridder DTD. Feeding your feelings: Emotion regulation strategies and emotional eating. Personality and Social Psychology Bulletin. 2010;36:792–804. doi: 10.1177/0146167210371383. [DOI] [PubMed] [Google Scholar]
- Faith MS, Flint J, Fairburn CG, Goodwin GM, Allison DB. Gender differences in the relationship between personality dimensions and relative body weight. Obesity Research. 2001;9:647–650. doi: 10.1038/oby.2001.86. [DOI] [PubMed] [Google Scholar]
- Ferrer E, McArdle JJ. Alternative structural models for multivariate longitudinal data analysis. Structural Equation Modeling. 2003;10:493–524. [Google Scholar]
- Field AE, Malspeis S, Willett WC. Weight cycling and mortality among middle-aged or older women. Archives of Internal Medicine. 2009;169:881–886. doi: 10.1001/archinternmed.2009.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster GD, Wadden TA, Vogt RA. Body image in obese women before, during, and after weight loss treatment. Health Psychology. 1997;16:226–229. doi: 10.1037//0278-6133.16.3.226. [DOI] [PubMed] [Google Scholar]
- Frayling TM, Timpson NJ, Weedon MN, Zeggini E, Freathy RM, Lindgren CM, et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science. 2007;316:889–894. doi: 10.1126/science.1141634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman HS. The multiple linkages of personality and disease. Brain, Behavior, and Immunity. 2008;22:668–675. doi: 10.1016/j.bbi.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin RD, Cox BJ, Clara I. Neuroticism and physical disorders among adults in the community: Results from the national comorbidity survey. Journal of Behavioral Medicine. 2006;29:229–238. doi: 10.1007/s10865-006-9048-5. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Friedman HS. Health status and the five-factor personality traits in a nationally representative sample. Journal of Health Psychology. 2006;11:643–654. doi: 10.1177/1359105306066610. [DOI] [PubMed] [Google Scholar]
- Haslam DW, James WPT. Obesity. Lancet. 2005;366:1197–1209. doi: 10.1016/S0140-6736(05)67483-1. [DOI] [PubMed] [Google Scholar]
- Heaven PCL, Mulligan K, Merrilees R, Woods T, Fairooz Y. Neuroticism and conscientiousness as predictors of emotional, external, and restrained eating behaviors. International Journal of Eating Disorders. 2001;30:161–166. doi: 10.1002/eat.1068. [DOI] [PubMed] [Google Scholar]
- Hebl MR, Mannix LM. The weight of obesity in evaluating others: A mere proximity effect. Personality and Social Psychology Bulletin. 2003;29:28–38. doi: 10.1177/0146167202238369. [DOI] [PubMed] [Google Scholar]
- Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. Journal of the American Medical Association. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- Hoyt AL, Rhodes RE, Hausenblas HA, Giacobbi PR., Jr Integrating five-factor model facet-level traits with the theory of planned behavior and exercise. Psychology of Sport and Exercise. 2009;10:565–572. [Google Scholar]
- Jansen A, Nederkoorn C, van Baak L, Keirse C, Guerrieri R, Havermans R. High-restrained eaters only overeat when they are also impulsive. Behaviour Research and Therapy. 2009;47:105–110. doi: 10.1016/j.brat.2008.10.016. [DOI] [PubMed] [Google Scholar]
- Jia H, Lubetkin EI. Trends in quality-adjusted life-years lost contributed by smoking and obesity. American Journal of Preventive Medicine. 2010;38:138–144. doi: 10.1016/j.amepre.2009.09.043. [DOI] [PubMed] [Google Scholar]
- Jöreskog KG, Sörbom D. Advances in factor analysis and structural equation models. Abt Books; Cambridge, MA: 1979. [Google Scholar]
- Kakizaki M, Kuriyama S, Sato Y, Shimazu T, Matsuda-Ohmori K, Nakaya N, et al. Personality and body mass index: A cross-sectional analysis from the Miyagi Cohort Study. Journal of Psychosomatic Research. 2008;64:71–80. doi: 10.1016/j.jpsychores.2007.07.008. [DOI] [PubMed] [Google Scholar]
- Luppino FS, De Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BWJH, et al. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Archives of General Psychiatry. 2010;67(3):220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- Mangold DL, Wand GS. Cortisol and adrenocorticotropic hormone responses to naloxone in subjects with high and low neuroticism. Biological Psychiatry. 2006;60:850–855. doi: 10.1016/j.biopsych.2006.03.049. [DOI] [PubMed] [Google Scholar]
- McAdams KK, Donnellan MB. Facets of personality and drinking in first-year college students. Personality and Individual Differences. 2009;46:207–212. [Google Scholar]
- McCrae RR, Terracciano A, Project M. o. t. P. P. o. C. Universal features of personality traits from the observer’s perspective: Data from 50 cultures. Journal of Personality and Social Psychology. 2005;88(3):547–561. doi: 10.1037/0022-3514.88.3.547. [DOI] [PubMed] [Google Scholar]
- Midei AJ, Matthews KA. Social relationships and negative emotional traits are associated with central adiposity and arterial stiffness in healthy adolescents. Health Psychology. 2009;28:347–353. doi: 10.1037/a0014214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. Journal of the American Medical Association. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Nabi H, Kivimaki M, Sabia S, Dugravot A, Lajnef M, Marmot MG, et al. Hostility and trajectories of body mass index over 19 years: The Whitehall II study. American Journal of Epidemiology. 2009;169:347–354. doi: 10.1093/aje/kwn333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. Journal of the American Medical Association. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Ozer DJ, Benet-Martínez V. Personality and the prediction of consequential outcomes. Annual Review of Psychology. 2006;57:401–421. doi: 10.1146/annurev.psych.57.102904.190127. [DOI] [PubMed] [Google Scholar]
- Paunonen SV, Haddock G, Forsterling F, Keinonen M. Broad versus narrow personality measures and the prediction of behaviour across cultures. European Journal of Personality. 2003;17:413–433. [Google Scholar]
- Petry NM, Barry D, Pietrzak RH, Wagner JA. Overweight and obesity are associated with psychiatric disorders: Results from the national epidemiologic survey on alcohol and related conditions. Psychosomatic Medicine. 2008;70:288–297. doi: 10.1097/PSY.0b013e3181651651. [DOI] [PubMed] [Google Scholar]
- Podar I, Hannus A, Allik J. Personality and affectivity characteristics associated with eating disorders: A comparison of eating disordered, weight-preoccupied, and normal samples. Journal of Personality Assessment. 1999;73:133–147. doi: 10.1207/S15327752JPA730109. [DOI] [PubMed] [Google Scholar]
- Provencher V, Bégin C, Gagnon-Girouard MP, Tremblay A, Boivin S, Lemieux S. Personality traits in overweight and obese women: Associations with BMI and eating behaviors. Eating Behaviors. 2008;9:294–302. doi: 10.1016/j.eatbeh.2007.10.004. [DOI] [PubMed] [Google Scholar]
- Räikkönen K, Matthews KA, Kuller LH, Reiber C, Bunker CH. Anger, hostility, and visceral adipose tissue in healthy postmenopausal women. Metabolism: Clinical and Experimental. 1999;48:1146–1151. doi: 10.1016/s0026-0495(99)90129-4. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd ed Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- Raudenbush SW, Bryk AS, Congdon R. HLM. Version 6 Scientific Software International; Lincolnwood, IL: 2004. [Google Scholar]
- Rhodes RE, Smith NEI. Personality correlates of physical activity: A review and meta-analysis. British Journal of Sports Medicine. 2006;40:958–965. doi: 10.1136/bjsm.2006.028860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rissanen A, Heliovaara M, Aromaa A. Overweight and anthropometric changes in adulthood: A prospective study of 17 000 Finns. International Journal of Obesity. 1988;12:391–401. [PubMed] [Google Scholar]
- Roehling MV, Roehling PV, Odland LM. Investigating the validity of stereotypes about overweight employees: The relationship between body weight and normal personality traits. Group and Organization Management. 2008;33:392–424. [Google Scholar]
- Rush CC, Becker SJ, Curry JF. Personality factors and styles among college students who binge eat and drink. Psychology of Addictive Behaviors. 2009;23:140–145. doi: 10.1037/a0013167. [DOI] [PubMed] [Google Scholar]
- Rzehak P, Meisinger C, Woelke G, Brasche S, Strube G, Heinrich J. Weight change, weight cycling and mortality in the ERFORT Male Cohort Study. European Journal of Epidemiology. 2007;22:665–673. doi: 10.1007/s10654-007-9167-5. [DOI] [PubMed] [Google Scholar]
- Schwartz MB, Brownell KD. Obesity and body image. Body Image. 2004;1:43–56. doi: 10.1016/S1740-1445(03)00007-X. [DOI] [PubMed] [Google Scholar]
- Scuteri A, Sanna S, Chen WM, Uda M, Albai G, Strait J, et al. Genome-wide association scan shows genetic variants in the FTO gene are associated with obesity-related traits. PLoS Genetics. 2007;3 doi: 10.1371/journal.pgen.0030115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegman AW, Townsend ST, Civelek A. Cahid, Blumenthal RS. Antagonistic behavior, dominance, hostility, and coronary heart disease. Psychosomatic Medicine. 2000;62:248–257. doi: 10.1097/00006842-200003000-00017. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford University Press; New York: 2003. [Google Scholar]
- Smith TW, Ruiz JM. Psychosocial influences on the development and course of coronary heart disease: Current status and implications for research and practice. Journal of Consulting and Clinical Psychology. 2002;70:548–568. doi: 10.1037//0022-006x.70.3.548. [DOI] [PubMed] [Google Scholar]
- Stenholm S, Simonsick EM, Ferrucci L. Secular trends in body weight in older men born between 1877 and 1941: the Baltimore Longitudinal Study of Aging. The journals of gerontology. Series A, Biological sciences and medical sciences. 2010;65:105–110. doi: 10.1093/gerona/glp178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan S, Cloninger CR, Przybeck TR, Klein S. Personality characteristics in obesity and relationship with successful weight loss. International Journal of Obesity. 2007;31:669–674. doi: 10.1038/sj.ijo.0803464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin AR, Costa PT, Jr, Miech R, Eaton WW. Personality and career success: Concurrent and longitudinal relations. European Journal of Personality. 2009;23:71–84. doi: 10.1002/per.704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin AR, Terracciano A, Deiana B, Naitza S, Ferrucci L, Uda M, et al. High neuroticism and low conscientiousness are associated with interleukin-6. Psychological Medicine. 2010;40:1485–1493. doi: 10.1017/S0033291709992029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin AR, Terracciano A, Deiana B, Uda M, Schlessinger D, Lakatta E, et al. Cholesterol, triglycerides, and the Five-Factor Model of personality. Biological Psychology. 2010;40:1485–1493. doi: 10.1016/j.biopsycho.2010.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swami V, Hadji-Michael M, Furnham A. Personality and individual difference correlates of positive body image. Body Image. 2008;5:322–325. doi: 10.1016/j.bodyim.2008.03.007. [DOI] [PubMed] [Google Scholar]
- Tasca GA, Demidenko N, Krysanski V, Bissada H, Illing V, Gick M, et al. Personality dimensions among women with an eating disorder: Towards reconceptualizing DSM. European Eating Disorders Review. 2009;17:281–289. doi: 10.1002/erv.938. [DOI] [PubMed] [Google Scholar]
- Terracciano A, Costa PT., Jr Smoking and the Five-Factor Model of personality. Addiction. 2004;99:472–481. doi: 10.1111/j.1360-0443.2004.00687.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Costa PTJ, McCrae RR. Personality plasticity after age 30. Personality and Social Psychology Bulletin. 2006;32:999–1009. doi: 10.1177/0146167206288599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Löckenhoff CE, Crum RM, Bienvenu OJ, Costa PT., Jr Five-factor model personality profiles of drug users. BMC Psychiatry. 2008;8:22. doi: 10.1186/1471-244X-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, McCrae RR, Brant LJ, Costa PT., Jr Hierarchical linear modeling analyses of the NEO-PI-R scales in the Baltimore Longitudinal Study of Aging. Psychology and Aging. 2005;20:493–506. doi: 10.1037/0882-7974.20.3.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Sutin AR, McCrae RR, Deiana B, Ferrucci L, Schlessinger D, et al. Facets of personality linked to underweight and overweight. Psychosomatic Medicine. 2009;71:682–689. doi: 10.1097/PSY.0b013e3181a2925b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tindle HA, Chang YF, Kuller LH, Manson JE, Robinson JG, Rosal MC, et al. Optimism, cynical hostility, and incident coronary heart disease and mortality in the women’s health initiative. Circulation. 2009;120:656–662. doi: 10.1161/CIRCULATIONAHA.108.827642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrka AR, Wier LM, Price LH, Rikhye K, Ross NS, Anderson GM, et al. Cortisol and ACTH responses to the Dex/CRH Test: Influence of temperament. Hormones and Behavior. 2008;53:518–525. doi: 10.1016/j.yhbeh.2007.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Den Bree MBM, Przybeck TR, Cloninger RC. Diet and personality: Associations in a population-based sample. Appetite. 2006;46:177–188. doi: 10.1016/j.appet.2005.12.004. [DOI] [PubMed] [Google Scholar]
- Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. Springer-Verlag; New York: 2000. [Google Scholar]
- Vicennati V, Pasqui F, Cavazza C, Pagotto U, Pasquali R. Stress-related development of obesity and cortisol in women. Obesity. 2009;17:1678–1683. doi: 10.1038/oby.2009.76. [DOI] [PubMed] [Google Scholar]
- Wadden, Womble, Stunkard, Anderson . Psychosocial consequences of obesity and weight loss. In: Waden TA, Stunkard AJ, editors. Handbook of Obesity Treatment. Guilford Press; New York: 2002. pp. 144–169. [Google Scholar]
- Walker LLM, Gately PJ, Bewick BM, Hill AJ. Children’s weight-loss camps: Psychological benefit or jeopardy? International Journal of Obesity. 2003;27:748–754. doi: 10.1038/sj.ijo.0802290. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Weber K, Assenheimer JS, Strauss ME, McCormick RA. Testing a tripartite model: II. Exploring the symptom structure of anxiety and depression in student, adult, and patient samples. Journal of Abnormal Psychology. 1995;104:15–25. doi: 10.1037//0021-843x.104.1.15. [DOI] [PubMed] [Google Scholar]
- Weiss A, Sutin AR, Duberstein PR, Friedman B, Bagby RM, Costa PT. The personality domains and styles of the Five-Factor Model are related to incident depression in Medicare recipients aged 65 to 100. American Journal of Geriatric Psychiatry. 2009;17:591–601. doi: 10.1097/jgp.0b013e31819d859d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . Obesity: preventing and managing the global epidemic. World Health Organizationo; Geneva: 2000. Document Number) [PubMed] [Google Scholar]
- Yach D, Stuckler D, Brownell KD. Epidemiologic and economic consequences of the global epidemics of obesity and diabetes. Nature Medicine. 2006;12:62–66. doi: 10.1038/nm0106-62. [DOI] [PubMed] [Google Scholar]
- Zhang H, Tamakoshi K, Yatsuya H, Murata C, Wada K, Otsuka R, et al. Long-term body weight fluctuation is associated with metabolic syndrome independent of current body mass index among Japanese men. Circulation. 2005;69:13–18. doi: 10.1253/circj.69.13. [DOI] [PubMed] [Google Scholar]