Abstract
Background
The transcription factor NF-κB consisting of the subunits RelA/p65 and p50 is known to be quickly activated after partial hepatectomy (PH), the functional relevance of which is still a matter of debate. Current concepts suggest that activation of NF-κB is especially critical in non-parenchymal cells to produce cytokines (TNF, IL-6) to adequately prime hepatocytes to proliferate after PH, while NF-κB within hepatocytes mainly bears cytoprotective functions.
Methods
To study the role of the NF-κB pathway in different liver cell compartments, we generated conditional knockout mice in which the transactivating NF-κB subunit RelA/p65 can be inactivated specifically in hepatocytes (RelaF/FAlbCre) or both in hepatocytes plus non-parenchymal cells including Kupffer cells (RelaF/FMxCre). 2/3 and 80% PH were performed in controls (RelaF/F) and conditional knockout mice (RelaF/FAlbCre and RelaF/FMxCre) and analyzed for regeneration.
Results
Hepatocyte-specific deletion of RelA/p65 in RelaF/FAlbCre mice resulted in an accelerated cell cycle progression without altering liver mass regeneration after 2/3 PH. Surprisingly, hepatocyte apoptosis or liver damage were not enhanced in RelaF/FAlbCre mice, even when performing 80% PH. The additional inactivation of RelA/p65 in non-parenchymal cells in RelaF/FMxCre mice reversed the small proliferative advantage observed after hepatocyte-specific deletion of RelA/p65 so that RelaF/FMxCre mice displayed normal cell cycle progression, DNA-synthesis and liver mass regeneration.
Conclusion
The NF-κB subunit RelA/p65 fulfills opposite functions in different liver cell compartments in liver regeneration after PH. However, the effects observed after conditional deletion of RelA/p65 are small and do not alter liver mass regeneration after PH. We therefore do not consider RelA/p65-containing canonical NF-κB signalling to be essential for successful liver regeneration after PH.
Introduction
The liver has a unique capacity to regenerate after resection. In the mouse model of 2/3 partial hepatectomy (2/3 PH) a sequence of well orchestrated cellular events is initiated which leads to proliferation of the normally quiescent organ to ultimately restore liver function and size within 7–10 days [1]–[3]. In the mouse DNA synthesis of the remaining hepatocytes peaks at about 36–42 hours after PH. To get prepared for cell cycle entrance, multiple signalling pathways are activated within the first hours after PH, which has traditionally been denoted the “priming phase” [1], [3]. Among others the transcription factor NF-κB consisting of the subunits RelA/p65 and p50 was early identified to be quickly activated after PH within 30 minutes [4], the functional relevance of which is still a matter of debate.
In canonical NF-κB-signalling, RelA/p65-p50 is the prototypical NF-κB heterodimer to regulate transcription of genes that control inflammation, cell death, and proliferation. RelA/p65 is kept inactive in the cytoplasm bound to its inhibitor IκB, which is under the control of the IKK complex, consisting of the catalytic subunits IKKα (IKK1), IKKβ (IKK2) and the regulatory subunit IKKγ (NEMO). Upon stimulation by cytokines such as TNF, IκB is phosphorylated and degraded after ubiquitination thereby unmasking a nuclear localisation sequence (NLS) of RelA/p65 ultimately resulting in nuclear translocation and transcriptional activity of NF-κB [5], [6].
First attempts to inactivate NF-κB signalling in rodent models to unravel its function in liver regeneration suggested intact NF-κB signalling to be crucial for normal PH-induced regeneration. The adenoviral transfer of a non-degradable NF-κB superrepressor (AdIκBα) inhibiting nuclear translocation of RelA/p65 and NF-κB activation within all liver cells led to liver apoptosis and impaired hepatocyte proliferation in rat and mouse [7], [8]. In contrast, attenuation of NF-κB activity specifically in about 45% of hepatocytes by conditional expression of an IκBα superrepressor (ΔN-IκBα) under the control of the transthyretin promoter did not alter liver regeneration after PH in mice [9]. Furthermore, conditional hepatocyte-specific deletion of IKKβ in IkkβF/FAlbCre animals was reported not to alter PH-induced hepatocyte proliferation [10]. However, the same group found liver regeneration to be impaired, when Ikkβ was inactivated in all liver cells including Kupffer cells in IKKβF/FMxCre mice [11]. Taken these results together, a concept has evolved that supports NF-κB signalling to be critical especially within non-parenchymal cells to drive an adequate early cytokine response important for normal regeneration after PH. According to this concept, NF-κB signalling within hepatocytes would be irrelevant for a proper regenerative response but rather fulfill a cytoprotective role after PH [7]–[11]. However, recently it was shown that hepatocyte-specific inactivation of IKKβ in IkkβF/FAlfpCre [12] or IkkβF/FAlbCre animals [13] rather accelerates cell cycle progression while pharmacological systemic inhibition of IKKβ did not alter liver regeneration after PH [12]. From previous studies we have learned, that conditional deletion of the IKKβ subunit of the IKK complex does not completely block but rather attenuates NF-κB activation [10], [14], [15]. We therefore asked whether discrepancies in previous studies investigating NF-κB in liver regeneration could be attributed to different degrees of inhibition of the NF-κB in the models used. Therefore, we used a conditional knockout mouse model in which the transactivating NF-κB subunit RelA/p65 which is essential for canonical NF-κB activation can be inactivated either specifically in hepatocytes (RelaF/FAlbCre) or in all liver cells (RelaF/FMxCre). Here, we report that genetic inactivation of RelA/p65 within hepatocytes does not lead to enhanced liver injury or apoptosis nor alter liver mass regeneration after 2/3 or extended PH even though cell cycle progression is accelerated. Furthermore, when RelA/p65 is inactivated in all liver cells including Kupffer cells we found an altered early cytokine response after PH. However, this only equalized the accelerated cell cycle progression observed after hepatocyte-specific deletion of RelA/p65 but did not significantly impair liver mass regeneration. Taken together, our data support a concept in which canonical NF-κB-signalling serves certain modulating but opposite functions within parenchymal and non-parenchymal liver cells after PH. However, normal liver mass regeneration occurs successful in livers lacking RelA/p65.
Materials and Methods
Mice
Generation of conditional RelA/p65-knockout animals (RelaF/F) was described previously [15], [16]. Shortly, in these mice exons 7 to 10 of the Rela gene are flanked by loxP sites leading to the generation of a truncated and functionally inactive RelA/p65 protein (Δp65) that lacks the Rel Homolgy Domain (RHD) upon Cre-mediated recombination. RelaF/F animals were crossed with AlbCre or MxCre animals [17], [18] to generate RelaF/FAlbCre or RelaF/FMxCre mice as described [15]. In RelaF/FAlbCre animals Rela is inactivated specifically in hepatocytes and biliary cells but not in non-parenchymal liver cells during late embryonic development [19], [20]. In contrast, recombination of floxed alleles was achieved in RelaF/FMxCre animals by a single i.p. injection of poly(I)-poly(C) (10 µg/g body weight) which leads to inactivation of Rela in IFNα-responsive tissues most efficiently in the liver including both hepatocytes and non-parenchymal cells [11], [15], [18]. All experiments were performed according to the protocols approved by our Institutional Animal Care and veterinarian office of the State of Bavaria (Regierung von Oberbayern, approval ID: TVA 55.2-1-54-2531-55-07) according to the National Institutes of Health “Guide for the Care and Use of Laboratory Animals”.
Partial Hepatectomy
Partial hepatectomy was performed in age- (8–10 weeks) and sex-matched animals using inhalation anaesthesia with isoflurane (2% isoflurane, O2 2 l/min). For 2/3 PH the left lobe (LL), the left median lobe (LML) and right median lobe (RML) were each ligated separately and resected with taking care not to injure the gallbladder (Fig. S1). For 80% PH the lower right lobe (LRL) and one omental lobe (OL) were additionally removed. Resected lobes served as controls (PH 0h) for biochemical analysis.
Tissue Processing and Analysis of Liver Regeneration after PH
Animals were injected i.p. with BrdU 100 µg/g BW two hours before they were sacrificed at the indicated time points after PH. Blood was withdrawn from the inferior caval vein, centrifuged, and serum was kept at −80°C until assayed. Liver tissue was processed for histology or snap-frozen and stored at −80°C. For determination of the extent of liver injury, ALT serum levels were determined by standard procedures. TNF and IL-6 serum levels were determined using a commercially available murine quantitative enzyme-linked immunosorbent assay (ELISA) kit (R&D Systems). Liver mass regeneration (%) at the respective time points after PH was determined by estimating original liver mass form the mass of the resected lobes at the time of PH. For this calculation the resected lobes were assumed to make up 67% and 78% in 2/3 PH and 80% PH respectively. These proportions had been determined in more than 20 mice of the same genetic background.
Kupffer Cell Isolation
To isolate liver Kupffer cells (KC) in order to verify efficient deletion of RelA/p65 on protein level, liver cells were isolated by retrograde Collagenase-perfusion as described previously [15]. The non-parenchymal cell fraction was pelleted by centrifugation (350 G, 10 min 4°C) and layered on top of a preformed two-step Percoll-gradient (50% and 25%). After centrifugation (800 G, 20 min, 4°C) cells in the KC-interphase were collected, pelleted, and resuspended in RPMI-1640 Medium (Sigma) at 0.5×106 cells/ml and selective adherence of KC was allowed for 15 min.
Protein Isolation and Immunoblot Analysis
For preparation of whole-cell protein extracts livers or cells were homogenized in Triton-lysis buffer (1% Triton, 20 mM Tris-HCl, 150 mM NaCl, 1 mM Na2EDTA, 1 mM EGTA, 1 mM PMSF and protease- and phosphatase-inhibitor cocktail). The lysate was sonicated and clarified by centrifugation, snap-frozen in liquid nitrogen and stored at −80°C until assayed. Protein extracts were analyzed by discontinuous SDS-PAGE as described previously [15]. Antibodies used were: rabbit anti-p65, anti-PCNA, anti-β-actin, anti-Cyclin A, anti-Cyclin D1 (all Santa Cruz), anti-JNK, anti-phospho-JNK, anti-STAT, anti-phospho-STAT (all Cell Signaling).
Histology
For histological analysis livers were fixed in 4% neutral phosphate-buffered paraformaldehyde for 20 hours, embedded in paraffin, and sectioned. Serial 3.5 µm-thick sections were stained with H&E using a standard protocol and evaluated under light microscopy. For immunohistochemical analysis tissues were processed as described previously [19] using anti-BrdU (Serotec) and goat anti-p65 (Santa Cruz). The TUNEL assay was performed using the in situ cell death detection kit POD (Roche Diagnostics Corp.) according to the manufacturer’s instructions. BrdU-uptake (%) was quantified by counting BrdU positive and negative hepatocyte nuclei in 10 random ×200-power fields in two different liver lobes.
Real-time PCR
Total RNA from livers was extracted using the RNeasy kit (Qiagen, Germany) according to the manufacturer’s instructions. RNA was transcribed into cDNA using random hexamers and the TaqMan Reverse Transcription Kit (Applied Biosystems). cDNA was further analyzed by real-time PCR as described previously [16] on an ABI 7700 Sequence Detection System (Applied Biosystems). All samples were analyzed in triplicate and data were calculated by 2-ΔΔCt method as described by the manufacturer and were expressed as fold increase over controls as indicated in the figure legends. Cyclophillin expression was used for normalization (primer sequences can be obtained by the authors upon request).
Electrophoretic mobility shift assay (EMSA)
For preparation of nuclear enriched whole-cell protein extracts snap frozen livers were homogenized in CelLytic™-Buffer and a high salt buffer (NuCLEAR™ Extraction Kit, Sigma-Aldrich). In brief, snap frozen liver samples were homogenized and lysed in isotonic buffer (10 mM Tris-HCl, pH 7.5, 2 mM MgCl2, 3 mM CaCl2, 0.5 M sucrose, 1 mM DTT, and protease inhibitor mixture) on ice for 20 min, and 0.6% IGEPAL CA-630 solution was added followed by centrifugation at 9000×g for 10 min. The nuclear pellet was resuspended in extraction buffer (20 mM HEPES, pH 7.9, 1.5 mM MgCl2, 0.42 M NaCl, 0.2 mM EDTA, 25% glycerol, 1 mM DTT, and protease inhibitor mixture) on a vortex mixer for 30 min at 4°C, sonicated on ice and centrifuged at 20000×g for 5 min. The supernatants were used as nuclear enriched whole-cell protein extracts. For EMSA 7,5 µg protein was assembled with 1 µl 10× Binding Buffer (100 mM Tris, 500 mM KCl, 10 mM DTT; pH 7.5), 2 µl of 50 mM DTT, 2.5% Tween-20, 1 µl 1% NP-40, 12 µl ddH2O, 1 µg of Poly (dI.dC) (1 µg/µl in 10 mM Tris, 1 mM EDTA; pH 7.5, Sigma-Aldrich) as nonspecific competitor and incubated with 1 µl of IRdye 700 pre-labeled NF-κB consensus oligonucleotide 50 fmol/µl (LI-COR) in dark for 30 min at room temperature. Cold competition was performed in the presence of 100-fold excess non-labeled consensus oligonucleotides respectively for 10 minutes prior to the addition of labeled oligonucleotides. The samples were loaded with 1 µl of 10X Orange Loading Dye on a 8% pre-run TBE-polyacrylamid gel and electrophoresis was continued at 80 V for 90–120 minutes. The signal was then detected and quantified with Odyssey infrared imaging system (Li-COR).
Statistics
Data are expressed as mean ± standard error (SEM). Differences between groups were analyzed by Student’s t-test where appropriate. In all cases, sample sizes (as indicated in the figures) were chosen to produce statistically unambiguous results. A P value of 0.05 or less was considered significant.
Results
Hepatocyte-specific Loss of RelA/p65 does not Result in Enhanced Liver Damage after 2/3 PH
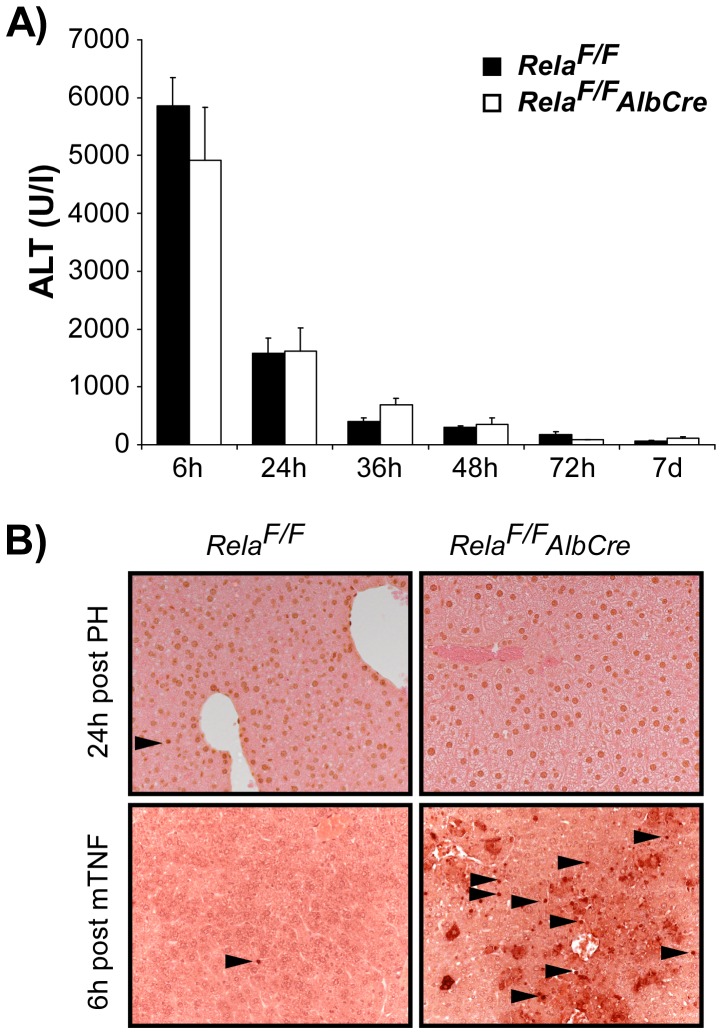
To study the functional role of the transactivating NF-κB subunit RelA/p65 in liver regeneration, RelaF/FAlbCre animals were subjected to 2/3 PH. Livers of these mice lack a functional RelA/p65 specifically in hepatocytes and loss of NF-κB binding activity upon LPS- or TNF-stimulation renders them highly sensitive to TNF-induced apoptosis [15]. Because PH is known to trigger a cytokine response with significant TNF-serum levels [21], we were curious whether the loss of RelA/p65 within hepatocytes would lead to enhanced liver injury after PH. To our surprise, we did not observe significantly different ALT levels in RelaF/FAlbCre animals as compared to control animals when followed over 7 days after 2/3 PH (Fig. 1A). Moreover, tissue integrity was not disturbed and no significant apoptotic cell death could be detected at any time point as assessed by histology and TUNEL-staining (Fig. 1B). Overall mortality after 2/3 PH did not differ significantly between groups (<5%) and could be attributed to technical complications during surgery. These results suggest that the main NF-κB subunit RelA/p65 is not essential to protect hepatocytes form cell death after 2/3 PH.
Figure 1. Hepatocyte-specific inactivation of RelA/p65 in RelaF/FAlbCre animals does not lead to enhanced liver injury after 2/3 PH.
(A) RelaF/F and RelaF/FAlbCre animals were subjected to 2/3 PH and ALT serum levels were determined at the indicated time points. Data are expressed as mean ± SEM (n = 3−6 animals per time point and group). (B) No significant apoptosis was detected at any time point after PH in control or mutant mice as assessed by TUNEL-staining. Representative TUNEL stainings from control and mutant livers harvested 24 h post PH are shown in the upper row. Liver sections from TNF-injected (i.v. 10 ng/g BW) control and RelaF/FAlbCre animals which are highly sensitive to TNF-induced apoptosis served as control (lower panel, magnification ×200).
Hepatocyte-specific Inactivation of RelA/p65 Causes an Accelerated Cell Cycle Progression without Altering Liver Mass Regeneration after 2/3 PH
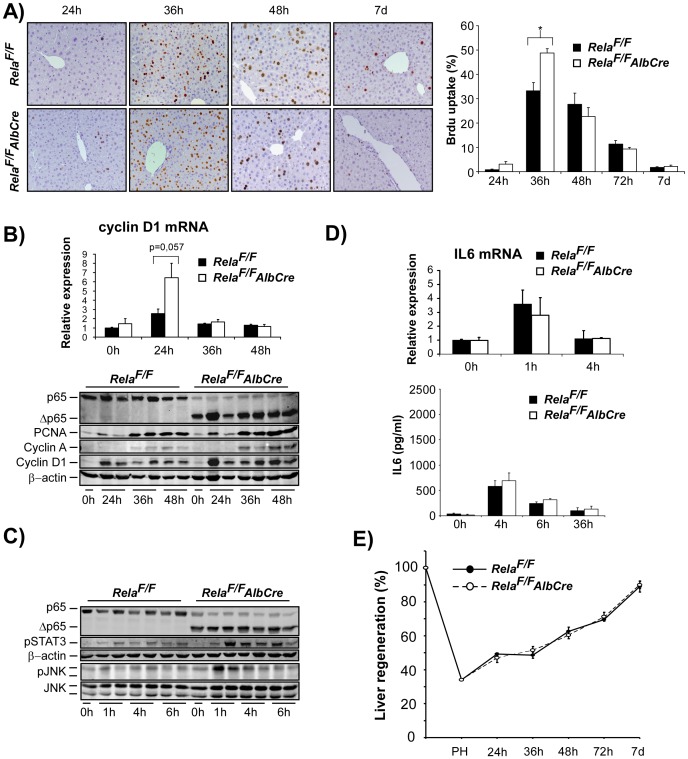
We next asked, whether the regenerative response would be altered in RelaF/FAlbCre animals after 2/3 PH as assessed by BrdU uptake as a measure for DNA-synthesis. Controls and mutant mice displayed similar kinetics of BrdU-uptake, however, the onset of BrdU uptake started earlier in RelaF/FAlbCre animals with significantly higher levels at 36 hours after PH (Fig. 2A). Consistent with histological findings, G1/S-phase-specific Cyclin D1 mRNA expression at 24 hours after PH was higher in RelaF/FAlbCre animals as was Cyclin D1 expression on protein level at 24–48 hours after PH (Fig. 2B). Moreover, WB analysis showed more pronounced PCNA and Cyclin A expression at 36 and 48 hours post PH. Theses findings suggest that hepatocyte loss of a functional RelA/p65 leads to an accelerated cell cycle progression after PH. As JNK signalling is suppressed by NF-κB signals [10], [15], [22] and Cyclin D1 expression is known to be regulated by JNK/AP1 [23], we analyzed early phosphorylation of JNK during the priming phase at 1, 4 and 6 hours after PH. While control animals did not display significant phospho-JNK levels, phosphorylation of p54-JNK was clearly induced in liver lysates from RelaF/FAlbCre after PH. Furthermore, we found enhanced levels phospho-STAT3 in livers of RelaF/FAlbCre animals as compared to controls (Fig. 2C). However, serum levels of the gp130 ligand and inducer of the JAK/STAT signalling pathway IL-6 or induction of IL-6 mRNA were not significantly different between the groups (Fig. 2D), indicating and confirming that NF-κB signals within hepatocytes negatively regulate STAT3 activation [24]. Of note, we were unable to detect any TNF-serum levels by ELISA in sera or liver lysates of control or mutant mice at 1, 4, 6 or 12 hours after PH (data not shown). mRNA expression levels of TNF were hardly detected in liver samples (CT values >31) and not different in RelaF/FAlbCre livers at 1 and 4 h after PH (data not shown).
Figure 2. Hepatocyte-specific inactivation of RelA/p65 results in accelerated cell cycle progression without altering liver mass regeneration after 2/3 PH.
(A–E) 2/3 PH was performed in RelaF/FAlbCre and RelaF/F control animals. (A) DNA synthesis was assessed by hepatocyte BrdU labelling at the indicated time points and quantified as described in Methods (representative×200 anti-BrdU stained liver sections are shown in the left panel, n = 4−8 animals per time point and group were counted for quantification, right panel). (B) Accelerated cell cycle progression in RelaF/FAlbCre mice as determined by mRNA levels of Cyclin D1 24 h post PH (upper panel) and WB analysis of cell-cycle associated proteins (PCNA, Cyclin A, Cyclin D1). Lysates were controlled for effective deletion of WT-RelA/p65 and β-actin served as loading control. Two representative lysates from each time point post PH are shown. (C) Loss of hepatocyte RelA/p65 leads to enhanced phosphorylation of STAT3 and JNK during the first hours after PH as assessed by immunoblot analysis (upper panels). (D) Liver IL-6 mRNA induction as determined by RT-PCR (upper graph) and IL-6 serum levels (ELISA, lower graph) were not different between groups. (E) Liver mass regeneration (%) determined as described in Methods did not differ between the groups. Data from BrdU-labelling, cytokine analysis, RT-PCR, and analysis of liver mass regeneration are presented as the average ± SEM for 3–6 animals per time point per group. *, p≤0.05 for mutant vs. control mice.
Despite the above findings indicating a slight but robust acceleration of cell cycle progression in RelA/p65 deficient hepatocytes, the time course of liver mass regeneration was not different between groups and all animals almost fully reached the initial liver mass within 7 days after 2/3 PH irrespective of the genotype (Fig. 2 E).
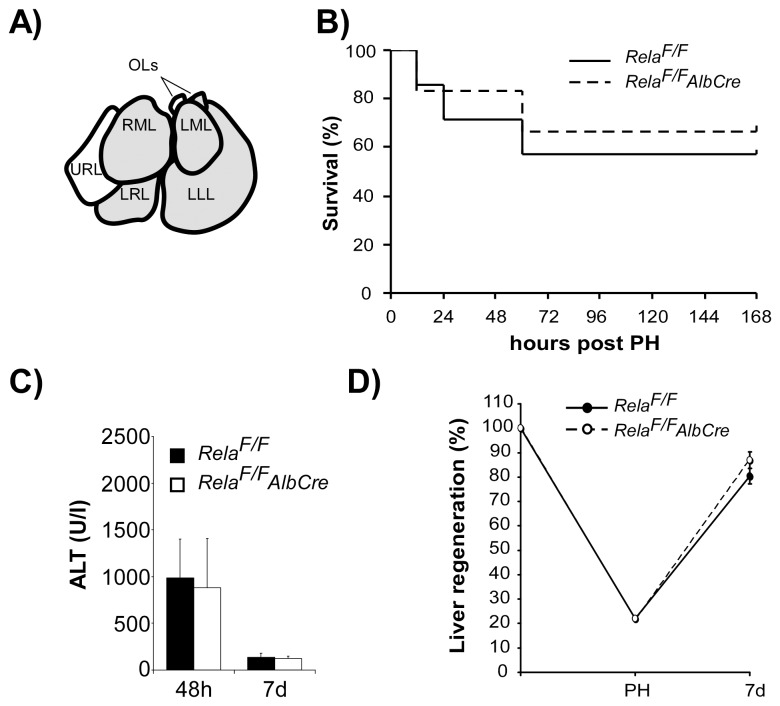
Extended Liver Mass Resection (80% PH) does not Lead to Impaired Regeneration or Increased Liver Cell Damage after Hepatocyte-specific Inactivation of RelA/p65
Our results are unexpected insofar as the main NF-κB subunit RelA/p65 is not fundamentally essential within hepatocytes to preserve liver cell integrity after 2/3 PH. To test whether this holds true also for extended liver mass resection, controls and RelaF/FAlbCre animals were subjected to extended partial hepatectomy. Additionally to the left and median lobes, the lower right lobe and the ventral omental lobe were resected resulting in about 80% PH (Fig. 3A) which is reported to be lethal to mice in 60–70% [25]. Under these conditions however, survival of control (4/6) and RelaF/FAlbCre mice (4/7) after 80% PH (Fig. 3B) and ALT levels of surviving animals at 48 hours and 7 d after extended PH were not significantly different (Fig. 3C). Livers of those animals not surviving all died within 60 hours after extended PH and displayed extensive centrilobular necrosis lacking significant apoptosis irrespective of genotype investigated (data not shown). Finally, liver mass regeneration of surviving animals at 7 days expressed in %-regeneration (Fig. 3D) or in liver weight/body weight (%) (RelaF/F 3,4±0,2%; RelaF/FAlbCre 3,5±0,1%) did not differ significantly between genotypes.
Figure 3. Extended liver mass resection of 80% does not lead to impaired regeneration or increased liver cell damage after hepatocyte-specific inactivation of RelA/p65.
(A) For extended (80%) PH the lower right lobe (LRL) and one omental lobe (OL) were additionally resected to standard 2/3 PH in control and RelaF/FAlbCre animals. (B) Survival of control and mutant animals did not differ between groups and was 4/6 in RelaF/F and 4/7 in RelaF/FAlbCre animals. ALT levels determined at 48 hours (C) and liver mass regeneration at 7 days post 80% PH (D).
Our results from 2/3 and 80% PH support the concept that genetic loss of intact NF-κB signalling within in the parenchymal cellular compartment of the liver does not particularly sensitize this organ to enhanced cell death after liver resection but rather leads to a certain proliferation advantage that however does not significantly alter overall restoration of the total number and mass of hepatocytes.
Genetic Inactivation of RelA/p65 in Both Parenchymal and Non-parenchymal Cells Neutralizes the Proliferative Advantage Seen after Hepatocyte-specific Deletion of RelA/p65 and Leads to a Normal Regenerative Response after PH
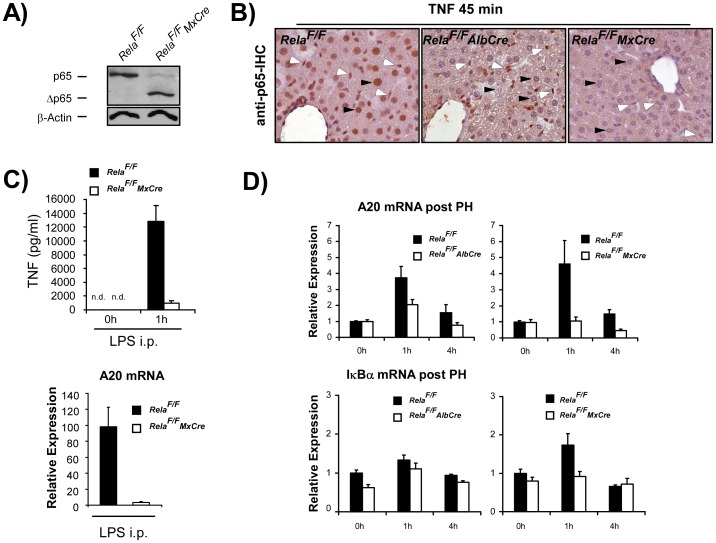
In contrast to previous reports that attribute PH-induced NF-κB-activation to parenchymal cells [7], [26], a more recent concept proposes that Kupffer cells are the main source of NF-κB-activation that also orchestrate the early cytokine response after PH [8], [9], [11]. Therefore, to additionally inactivate canonical NF-κB signalling in Kupffer cells, we used RelaF/FMxCre animals to study liver regeneration after PH. Effective deletion of wildtype RelA/p65 was confirmed by WB analysis of lysates from Kupffer cells isolated form control and RelaF/FMxCre animals 7 days after i.p. injection with polyIC (Fig. 4A). To verify that nuclear translocation of RelA/p65 as a prerequisite for NF-κB activation does not occur in both parenchymal and non-parenchymal cellular compartments in the livers of RelaF/FMxCre animals, RelaF/FMxCre and control animals were challenged with an i.p. injection of TNF (25 ng/g BW) and subjected to anti-p65-IHC analysis. TNF is a strong inducer of NF-κB and consequently, at 45 min after TNF-injection RelA/p65 translocation can be observed in hepatocytes and non-parenchymal cells in control animals (Fig. 4B, left). In RelaF/FAlbCre animals nuclear staining of RelA/p65 is restricted to non-parenchymal cells while nuclear staining of RelA/p65 is virtually absent in all cells in the livers of TNF-treated RelaF/FMxCre animals (Fig. 4B, middle and right panel respectively). Consequently and as previously reported, RelaF/FMxCre mice display a blunted LPS-induced TNF-response because nuclear translocation of RelA/p65 in Kupffer cells as the main source of LPS-induced NF-κB-dependent TNF-production is inhibited (Fig. 4C, left panel). Accordingly, stimulation of the NF-κB target gene A20 after LPS-challenge was abolished in RelaF/FMxCre mice (Fig. 4C, right panel). PH-induced induction of A20 was only attenuated in RelaF/FAlbCre mice but abolished in RelaF/FMxCre animals (Fig. 4D). However, PH-induced A20-mRNA induction in control animals (4-fold) was very low when compared to LPS injection (100-fold), suggesting that liver NF-κB activation is very weak after PH. Similarly, the magnitude of PH-induced induction of the NF-κB target gene IκBα in controls was mild, but completely inhibited in RelaF/FMxCre mice (Fig. 4D). The assumption that NF-κB activation was only mild after PH under our experimental conditions was confirmed by anti-p65-IHC where nuclear staining was only occasionally observed mainly in non-parenchymal cells of control animals when analyzed at 1 h and 4 h post PH (Fig. S2). Furthermore EMSA analysis for NF-κB binding activity at 1 h post PH did not give a robust signal in either genotype analyzed (Fig. S2).
Figure 4. Genetic deletion of WT RelA/p65 in all liver cells including Kupffer cells impairs NF-κB dependent cytokine response and activation of NF-κB target genes in RelaF/FMxCre animals.
(A) WT RelA/p65 is deleted in Kupffer cells isolated from RelaF/FMxCre animals 7 days after one single i.p. injection of poly-IC (10 µg/g BW) as assessed be immunoblot analysis with anti-p65. β-actin served as loading control. (B) 45 min after i.p. TNF (25 ng/g BW) nuclear translocation of RelA/p65 is seen in hepatocytes (black arrowheads) and non-parenchymal cells (white arrowheads) in RelaF/F controls, confined to non-parenchymal cells in RelaF/FAlbCre animals and virtually absent in all liver cells in RelaF/FMxCre animals (magnification×200). (C) LPS (2 mg/kg) -induced TNF-response in mouse serum (left panel) and LPS-induced induction of the NF-κB target gene Tfnaip3 encoding A20 in the liver (right panel) is abolished in RelaF/FMxCre animals as assessed by ELISA and RT-PCR respectively. (D) A20 mRNA and IκBα mRNA expression as assessed by RT-PCR analysis at the indicated times post PH is inhibited in RelaF/FAlbCre animals but abolished in RelaF/FMxCre animals. Data from cytokine analysis and RT-PCR are presented as the average ± SEM for 3–6 animals per time point per group.
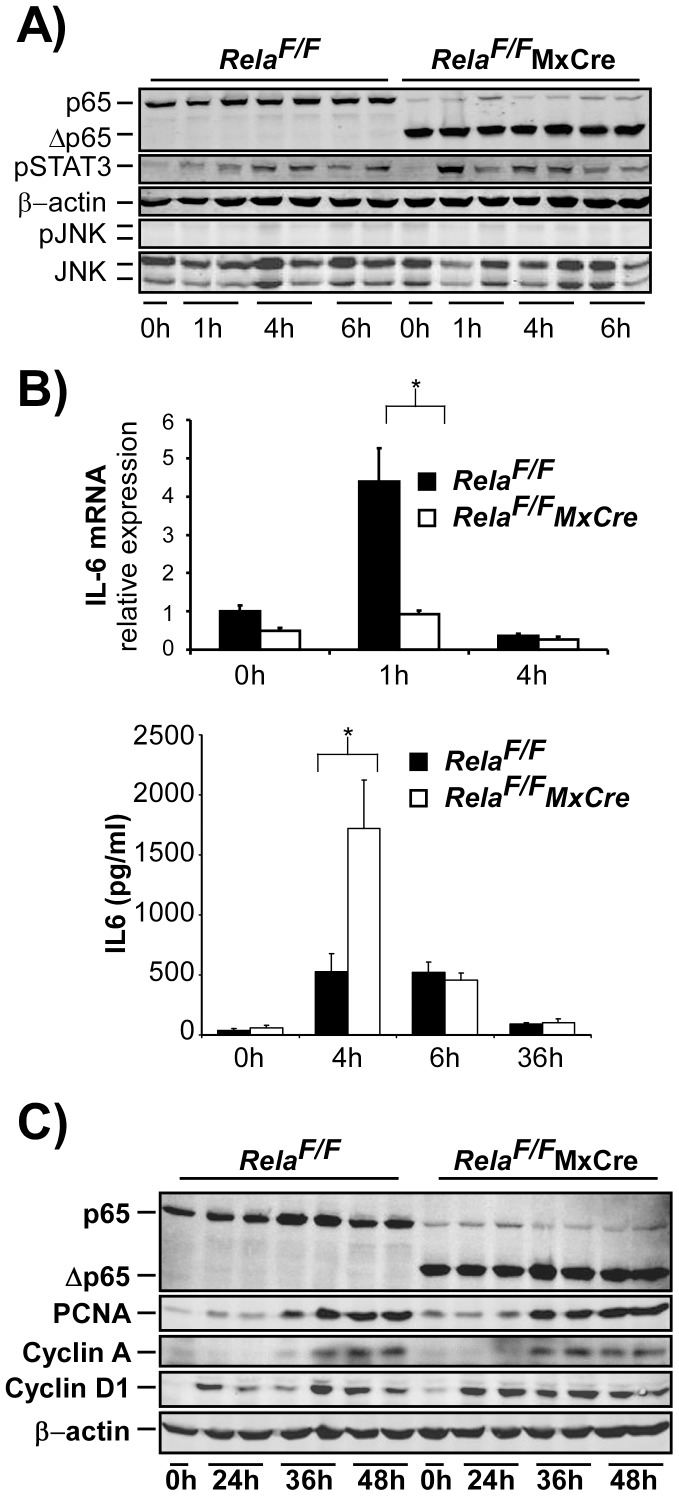
To determine the impact of the additional loss of RelA/p65 in the non-parenchymal cellular compartment to the cytokine and regenerative response after PH, RelaF/FMxCre animals and controls were subjected to 2/3 PH. Phospho-STAT3 levels at 1 h, 4 h and 6 h after PH were not significantly different between the strains (Fig. 5A, upper and middle panel). Furthermore, phospho-JNK levels were hardly detected in either group (Fig. 5A), suggesting that the additional deletion of RelA/p65 in non-parenchymal cells has a mitigating effect on enhanced STAT3- and JNK-phosphorylation seen after hepatocyte-specific deletion of RelA/65 in RelaF/FAlbCre animals. Because deletion of RelA/p65 occurs equally efficient in hepatocytes of both RelaF/FAlbCre and RelaF/FMxCre livers, we presume that NF-κB-dependent signals from non-parenchymal cells that would initiate STAT- and JNK-signalling are lost in RelaF/FMxCre animals.
Figure 5. Additional genetic deletion of RelA/p65 in all liver cells in RelaF/FMxCre alters the cytokine response without significantly altering cell cycle progression after 2/3 PH.
(A–C) 2/3 PH was performed on RelaF/F and RelaF/FMxCre animals and analyzed as indicated. (A) Levels of phospho-STAT3 in control and RelaF/FMxCre animals were not different while phosphorylation of JNK was barely detected in either group as assessed be immunoblot analysis. (B) Induction of liver IL-6 mRNA was inhibited in RelaF/FMxCre animals as determined by RT-PCR (upper image), however, IL-6 serum levels were significantly elevated in livers of RelaF/FMxCre mice at 4 h post PH (lower image). (C) Immunoblot analysis of cell cycle associated proteins was performed as described in Fig. 2. Data from cytokine analysis and RT-PCR are presented as the average ± SEM for 3–6 animals per time point per group. *, p≤0.05 for mutant vs. control mice.
As expected, IL-6 mRNA induction within the liver was clearly inhibited in RelaF/FMxCre animals as compared to Cre-negative litters at 1 h after PH (Fig. 5B, upper graph). Paradoxically, serum levels of IL-6 were significantly higher in RelaF/FMxCre animals at 4 hours after PH, suggesting that extrahepatic cells are the source of systemic IL-6 levels (Fig. 5B, lower graph). Again, TNF-serum levels could not be detected at any time point after PH (data not shown).
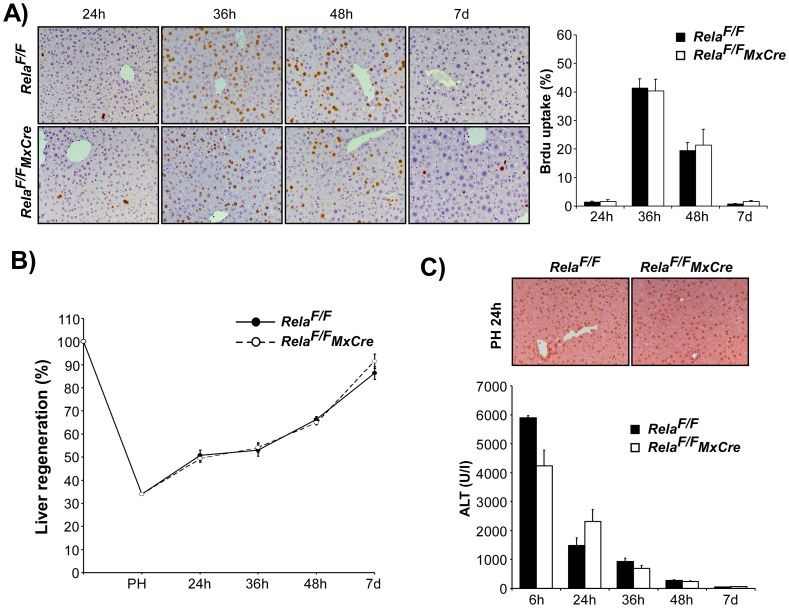
Cell cycle progression was not grossly altered as assessed by immunoblot analysis of cell cycle proteins Cyclin D1, PCNA and Cyclin A in liver lysates from control and RelaF/FMxCre animals after PH (Fig. 5C). This supports the view that the additional deletion of RelA/p65 in the non-parenchymal liver cell compartment reverses the slight proliferation advantage observed after hepatocyte-specific loss of RelA/p65. Congruently, BrdU-uptake of hepatocytes was not different in RelaF/FMxCre animals (Fig. 6A) and liver mass regeneration occurred normally (Fig. 6B). No enhanced liver damage was detected in RelaF/FMxCre animals at any time after PH as determined by ALT levels and TUNEL staining (Fig. 6C).
Figure 6. Genetic deletion of WT RelA/p65 in all liver cells in RelaF/FMxCre animals does not alter DNA-synthesis or liver mass regeneration after 2/3 PH.
(A) DNA-synthesis as determined by BrdU-uptake and (B) liver mass regeneration was not different in control and mutant animals. (C) Representative TUNEL staining at 24 h and ALT levels did not reveal significant apoptosis or altered liver damage in RelaF/F and RelaF/FMxCre animals. Data are presented as the average ± SEM for 3–6 animals per time point per group.
Discussion
The most important finding in our study is that liver regeneration after PH occurs perfectly fine when the transactivating NF-κB subunit RelA/p65 is inactivated, either in hepatocytes alone or in all liver cells. Initial studies investigating the role of NF-κB signalling in liver regeneration pointed to an essential role of NF-κB to prevent apoptotic cell death and drive proliferation after PH [7]. Harmonizing with initial studies obtained from IL-6- or TNFR1-deficient mice that were reported to display impaired liver regeneration [21], [27] an attractive model was coined where NF-κB not only serves cytoprotective functions within hepatocytes but also routes an adequate cytokine response primarily within Kupffer cells to prime hepatocytes for mitogenic stimuli to proliferate [28].
There is the current conception, that the degree of NF-κB inhibition determines the sensitivity of hepatocytes to apoptotic cell death [29], [30]. This view has been deduced from genetic studies investigating hepatocytes deficient for the IKKβ-subunit of the IKK-complex that are still capable to display residual NF-κB activity and show only mild TNF-induced cell death [10], [14], [15]. In contrast, in hepatocytes lacking the IKK-subunit IKKγ- or the NF-κB-subunit RelA/p65, TNF-induced NF-κB-activation is completely abolished rendering these cells highly sensitive to minute amounts of TNF [14], [15]. Conditional hepatocyte-specific deletion of IKKβ rather accelerates regeneration after 2/3 PH [11], [12], however, massive apoptosis and strongly impaired regeneration associated with high mortality is observed after PH in mice after hepatocyte-specific inactivation of IKKγ [31]. With respect to this latter congress report our results are unexpected insofar as we did not find any significant apoptosis after 2/3 PH suggesting that TNF levels after PH do not suffice to trigger cell death even when canonical NF-κB signalling is shut down in hepatocytes. Because RelA/p65- and IKKγ-deficient hepatocytes are highly sensitive to TNF-induced apoptosis [15], [32] but regeneration after PH is obviously different, it seems that the IKK-complex preserves cell integrity also by regulating pathways independent of canonical NF-κB signalling [33]. However, we cannot rule out that NF-κB dimers lacking RelA/p65 at later time points during liver regeneration not analyzed for NF-κB activation may be capable to induce survival signals in RelaF/FAlbCre animals. Furthermore, as pointed out below, different surgical PH-techniques may lead to different cytokine levels that might account for the differences.
Livers from RelaF/FAlbCre showed an earlier onset of cell cycle progression and a higher maximum of DNA-synthesis after PH. This was preceded be enhanced JNK-activation known to be important to drive transition from G0 to G1 as a possible mechanism for the accelerated cell cycle progression. Our findings are in agreement with results obtained from IKKβF/FAlfpCre [12] and IKKβF/FAlbCre [13] animals and suggest that the loss of NF-κB signals within hepatocytes goes along with a proliferation advantage after PH possibly due to an altered acute phase response or differential NF-κB-dependent control of STAT3 activity [24] Enhanced proliferation observed in RelaF/FAlbCre animals was robust but rather small and liver mass regeneration was not altered in RelaF/FAlbCre animals. So, we are reluctant to over-interpret its functional meaning in liver regeneration after PH and our results rather underscore the view that classical canonical NF-κB signalling containing RelA/p65 within hepatocytes is dispensable for liver regeneration after PH.
The small proliferation advantage of RelA/p65-deficient hepatocytes after PH was lost when RelA/p65 was inactivated in all liver cells in RelaF/FMxCre mice consistent with the popular view that NF-κB-dependent signals from non-parenchymal cells that promote regeneration are lost [1], [3]. However, considering the decisive role that is attributed to canonical NF-κB signalling in non-parenchymal liver cells in liver regeneration after PH, it is stunning that regeneration in RelaF/FMxCre animals occurs perfectly fine. We are well aware that the MxCre-mouse line has limitations because MxCre-induced deletion is not restricted to liver cells but also occurs in the spleen and other IFN-sensitive tissues [18]. Deletion of IKKβ or RelA/p65 using MxCre mice has been reported to alter cytokine processing in myeloid cells [34]. In this context it is possible that even though liver IL-6 mRNA is suppressed in RelaF/FMxCre animals after PH, enhanced IL-6 production from extrahepatic tissues as observed in our study might compensate for reduced IL-6 production in RelA/p65-deficient Kupffer cells. Nevertheless, Maeda et al. reported a strongly reduced regenerative response in IKKβF/FMxCre animals [11] while systemic pharmacological inhibition of IKKβ was not found to alter liver regeneration after PH by others [12].
It is conspicuous that studies investigating the role of NF-κB signalling and cytokines in mouse liver regeneration after PH often produce conflicting results: Significant NF-κB activation in response to 2/3 PH is not found by all investigators [25] and the time point when maximal NF-κB activation is observed after PH varies from 30 minutes [4] to 12 hours after PH [8]. In our hands, the magnitude of NF-κB activation in control animals was too low to be detected using NF-κB-binding assays, and we only observed sparse nuclear translocation of RelA/p65 mainly in non-parenchymal cells with immunohistochemistry at 1 h post PH (Fig. S2). Furthermore, TNF-serum levels are only infrequently detected by different research groups and the effect of genetic deletion or inhibition of TNF or its receptor TNFR1 has produced clearly different results ranging from “grossly impaired liver regeneration and high lethality” to “no functional relevance” after PH [21], [35], [36]. Also, while initial studies in Il-6 null mice suggested IL-6 to be essential for both proliferation and survival [27], subsequent studies in Il-6 null mice or in mice with ablation of the IL-6 downstream signalling molecule gp130 showed essentially normal regeneration and clearly relativized the importance of IL-6 in regeneration after PH [37], [38]. Remarkably, also genetic deletion of the TLR-adaptor protein MYD88 has revealed conflicting results by different groups [39], [40]. Though both groups reported a blunted IL-6 and TNF-response in Myd88 null mice, only one group found liver regeneration to be impaired [39]. Furthermore, in a recent study a dramatic influence of different puncture sites for blood sampling on IL-6 levels was pointed out. In that study, even an anti-proliferative effect of IL-6 on liver regeneration after PH was suggested [41]. It is unlikely that all these contradictory findings from many different laboratories can all be attributed to differences in genetic background or breeding conditions of the animals.
2/3 PH is considered the golden standard to study liver regeneration in mice. The more it is surprising that the surgical procedure to perform PH has not been standardized. The original mass ligation of the median and the left liver lobe as originally described for the rat by Higgins and Anderson back in 1931 [42] has been adopted by multiple laboratories to study liver regeneration in the mouse though it has early been recognized that distinct anatomical differences such as the presence of a gallbladder in the mouse may lead to considerable mortality and less reproducible results [43]–[45]. Only infrequently separate ligation and separate resection of the liver lobes (either with or without resection of the gallbladder) have been applied in mouse studies investigating liver regeneration after 2/3 PH and only recently efforts were undertaken by researchers to provide a standard for the surgical procedure in the mouse [46]–[48]. It has been pointed out that selective ligation and resection of each liver lobe is crucial to avoid venous obstruction and consecutive necrosis that interferes with liver regeneration as sometimes observed after mass ligation [47]. Several studies suggest that the surgical technique in fact may have a strong impact on liver regeneration after PH. For instance, lethality of Il-6 null animals was initially found to be very high [27], [49] but was absent when the lobes were resected separately and the gallbladder was left undisrupted [37]. Another striking example for the significance of the surgical procedure comes from one group that earlier found 80% lethality in hepatocyte-specific knockout mice for the HGF-receptor c-Met using the method of Higgins & Anderson [50]. However, lethality was absent when the gallbladder was left intact and the liver lobes were ligated separately [51]. It may well be the case that i.e. the magnitude of endotoxin translocation from the gut or the release from other factors that regulate the cytokine and acute phase responses as well as the magnitude of NF-κB activation are influenced by a variable extent of tissue damage caused by different surgical techniques. In initial experiments we found considerable lethality and impaired liver DNA-synthesis in RelaF/FMxCre animals when using mass ligation including cholecystectomy. This would support the notion that NF-κB dependent signals or pathways in fact may be vital to face an enhanced acute phase response and enable liver regeneration when less gentle surgical techniques are applied. However, using the surgical technique as described, we show that the transactivating NF-κB subunit RelA/p65 fulfils rather minor albeit opposite functions in parenchymal and non-parenchymal liver cells. We conclude that classical canonical NF-κB signalling containing RelA/p65 within liver cells is of minor importance for successful liver regeneration after PH. One has to be cautious regarding potential side effects of NF-κB inhibitors in the setting of inflammation. However, translating our findings to the clinical situation, it may be save to perform liver resection even in the setting of systemic (i.e. pharmacological) NF-κB inhibition.
Supporting Information
Surgical procedure for 2/3 PH. (A) For 2/3 PH the left lower lobe (LLL), the left median and the right median lobe (LML and RML) are removed. (B) Each lobe is separately ligated (a-c) with taking special care not to disrupt the gallbladder (d).
(TIF)
NF-κB activation after 2/3 PH. (A) NF-κB activation in livers of indicated genotypes as assessed by anti-p65 IHC at 1 h and 4 h post PH. Nuclear staining is occasionally observed in non-parenchymal cells (white arrowheads) only in control and RelaF/FAlbCre animals at 1 h and to a lesser extent at 4 h post PH. Nuclear staining for p65 is almost never detected in hepatocytes of either genotype (black arrowhead marks a positive hepatocyte in a control animal). Nuclear staining was nearly completely absent in RelaF/FMxCre animals both in hepatocytes and non-parenchymal cells (magnification×200). (B) No robust NF-κB binding activity could be detected by EMSA analysis 1 h post PH in livers of indicated genotypes. Liver lysates from LPS-treated animals served as positive control (LPS 2 mg/kg i.p.).
(TIF)
Acknowledgments
The authors thank Silvia Krutsch for excellent laboratory assistance.
Funding Statement
This work has been supported by a grant from the Else Kröner-Fresenius-Stiftung (EKFS, grant P10/07 to F.G. and R.M.S.). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Fausto N, Campbell JS, Riehle KJ (2006) Liver regeneration. Hepatology 43: S45–53. [DOI] [PubMed] [Google Scholar]
- 2. Taub R (2004) Liver regeneration: from myth to mechanism. Nat Rev Mol Cell Biol 5: 836–847. [DOI] [PubMed] [Google Scholar]
- 3. Michalopoulos GK (2007) Liver regeneration. J Cell Physiol 213: 286–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cressman DE, Greenbaum LE, Haber BA, Taub R (1994) Rapid activation of post-hepatectomy factor/nuclear factor kappa B in hepatocytes, a primary response in the regenerating liver. J Biol Chem 269: 30429–30435. [PubMed] [Google Scholar]
- 5. Chen LF, Greene WC (2004) Shaping the nuclear action of NF-kappaB. Nat Rev Mol Cell Biol 5: 392–401. [DOI] [PubMed] [Google Scholar]
- 6. Hayden MS, Ghosh S (2004) Signaling to NF-kappaB. Genes Dev 18: 2195–2224. [DOI] [PubMed] [Google Scholar]
- 7. Iimuro Y, Nishiura T, Hellerbrand C, Behrns KE, Schoonhoven R, et al. (1998) NFkappaB prevents apoptosis and liver dysfunction during liver regeneration. J Clin Invest 101: 802–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yang L, Magness ST, Bataller R, Rippe RA, Brenner DA (2005) NF-kappaB activation in Kupffer cells after partial hepatectomy. Am J Physiol Gastrointest Liver Physiol 289: G530–538. [DOI] [PubMed] [Google Scholar]
- 9. Chaisson ML, Brooling JT, Ladiges W, Tsai S, Fausto N (2002) Hepatocyte-specific inhibition of NF-kappaB leads to apoptosis after TNF treatment, but not after partial hepatectomy. J Clin Invest 110: 193–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Maeda S, Chang L, Li ZW, Luo JL, Leffert H, et al. (2003) IKKbeta is required for prevention of apoptosis mediated by cell-bound but not by circulating TNFalpha. Immunity 19: 725–737. [DOI] [PubMed] [Google Scholar]
- 11. Maeda S, Kamata H, Luo JL, Leffert H, Karin M (2005) IKKbeta couples hepatocyte death to cytokine-driven compensatory proliferation that promotes chemical hepatocarcinogenesis. Cell 121: 977–990. [DOI] [PubMed] [Google Scholar]
- 12. Malato Y, Sander LE, Liedtke C, Al-Masaoudi M, Tacke F, et al. (2008) Hepatocyte-specific inhibitor-of-kappaB-kinase deletion triggers the innate immune response and promotes earlier cell proliferation during liver regeneration. Hepatology 47: 2036–2050. [DOI] [PubMed] [Google Scholar]
- 13. Koch KS, Maeda S, He G, Karin M, Leffert HL (2009) Targeted deletion of hepatocyte Ikkbeta confers growth advantages. Biochem Biophys Res Commun 380: 349–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Luedde T, Assmus U, Wustefeld T, Meyer zu Vilsendorf A, Roskams T, et al. (2005) Deletion of IKK2 in hepatocytes does not sensitize these cells to TNF-induced apoptosis but protects from ischemia/reperfusion injury. J Clin Invest 115: 849–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Geisler F, Algul H, Paxian S, Schmid RM (2007) Genetic inactivation of RelA/p65 sensitizes adult mouse hepatocytes to TNF-induced apoptosis in vivo and in vitro. Gastroenterology 132: 2489–2503. [DOI] [PubMed] [Google Scholar]
- 16. Algul H, Treiber M, Lesina M, Nakhai H, Saur D, et al. (2007) Pancreas-specific RelA/p65 truncation increases susceptibility of acini to inflammation-associated cell death following cerulein pancreatitis. J Clin Invest 117: 1490–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Postic C, Magnuson MA (2000) DNA excision in liver by an albumin-Cre transgene occurs progressively with age. Genesis 26: 149–150. [DOI] [PubMed] [Google Scholar]
- 18. Kuhn R, Schwenk F, Aguet M, Rajewsky K (1995) Inducible gene targeting in mice. Science 269: 1427–1429. [DOI] [PubMed] [Google Scholar]
- 19. Geisler F, Nagl F, Mazur PK, Lee M, Zimber-Strobl U, et al. (2008) Liver-specific inactivation of Notch2, but not Notch1, compromises intrahepatic bile duct development in mice. Hepatology 48: 607–616. [DOI] [PubMed] [Google Scholar]
- 20. Weisend CM, Kundert JA, Suvorova ES, Prigge JR, Schmidt EE (2009) Cre activity in fetal albCre mouse hepatocytes: Utility for developmental studies. Genesis 47: 789–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Yamada Y, Kirillova I, Peschon JJ, Fausto N (1997) Initiation of liver growth by tumor necrosis factor: deficient liver regeneration in mice lacking type I tumor necrosis factor receptor. Proc Natl Acad Sci U S A 94: 1441–1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liu H, Lo CR, Czaja MJ (2002) NF-kappaB inhibition sensitizes hepatocytes to TNF-induced apoptosis through a sustained activation of JNK and c-Jun. Hepatology 35: 772–778. [DOI] [PubMed] [Google Scholar]
- 23. Schwabe RF, Bradham CA, Uehara T, Hatano E, Bennett BL, et al. (2003) c-Jun-N-terminal kinase drives cyclin D1 expression and proliferation during liver regeneration. Hepatology 37: 824–832. [DOI] [PubMed] [Google Scholar]
- 24. He G, Yu GY, Temkin V, Ogata H, Kuntzen C, et al. (2010) Hepatocyte IKKbeta/NF-kappaB inhibits tumor promotion and progression by preventing oxidative stress-driven STAT3 activation. Cancer Cell 17: 286–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cataldegirmen G, Zeng S, Feirt N, Ippagunta N, Dun H, et al. (2005) RAGE limits regeneration after massive liver injury by coordinated suppression of TNF-alpha and NF-kappaB. J Exp Med 201: 473–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Trautwein C, Rakemann T, Niehof M, Rose-John S, Manns MP (1996) Acute-phase response factor, increased binding, and target gene transcription during liver regeneration. Gastroenterology 110: 1854–1862. [DOI] [PubMed] [Google Scholar]
- 27. Cressman DE, Greenbaum LE, DeAngelis RA, Ciliberto G, Furth EE, et al. (1996) Liver failure and defective hepatocyte regeneration in interleukin-6-deficient mice. Science 274: 1379–1383. [DOI] [PubMed] [Google Scholar]
- 28. Fausto N (2000) Liver regeneration. J Hepatol 32: 19–31. [DOI] [PubMed] [Google Scholar]
- 29. Chakraborty JB, Mann DA (2010) NF-kappaB signalling: embracing complexity to achieve translation. J Hepatol 52: 285–291. [DOI] [PubMed] [Google Scholar]
- 30. Pasparakis M (2009) Regulation of tissue homeostasis by NF-kappaB signalling: implications for inflammatory diseases. Nat Rev Immunol 9: 778–788. [DOI] [PubMed] [Google Scholar]
- 31. Malato Y, Beraza N, Gassler N, Al-Masaoudi M, Liedtke C, et al. (2009) Activation of Progenitor Cells Triggers the Repopulation of Conditional Nemo Ko Livers during Liver Regeneration in Mice. Journal of Hepatology 50: S310–S310. [Google Scholar]
- 32. Beraza N, Ludde T, Assmus U, Roskams T, Vander Borght S, et al. (2007) Hepatocyte-specific IKK gamma/NEMO expression determines the degree of liver injury. Gastroenterology 132: 2504–2517. [DOI] [PubMed] [Google Scholar]
- 33. Bettermann K, Vucur M, Haybaeck J, Koppe C, Janssen J, et al. TAK1 suppresses a NEMO-dependent but NF-kappaB-independent pathway to liver cancer. Cancer Cell 17: 481–496. [DOI] [PubMed] [Google Scholar]
- 34. Greten FR, Arkan MC, Bollrath J, Hsu LC, Goode J, et al. (2007) NF-kappaB is a negative regulator of IL-1beta secretion as revealed by genetic and pharmacological inhibition of IKKbeta. Cell 130: 918–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fujita J, Marino MW, Wada H, Jungbluth AA, Mackrell PJ, et al. (2001) Effect of TNF gene depletion on liver regeneration after partial hepatectomy in mice. Surgery 129: 48–54. [DOI] [PubMed] [Google Scholar]
- 36. Hayashi H, Nagaki M, Imose M, Osawa Y, Kimura K, et al. (2005) Normal liver regeneration and liver cell apoptosis after partial hepatectomy in tumor necrosis factor-alpha-deficient mice. Liver Int 25: 162–170. [DOI] [PubMed] [Google Scholar]
- 37. Sakamoto T, Liu Z, Murase N, Ezure T, Yokomuro S, et al. (1999) Mitosis and apoptosis in the liver of interleukin-6-deficient mice after partial hepatectomy. Hepatology 29: 403–411. [DOI] [PubMed] [Google Scholar]
- 38. Wuestefeld T, Klein C, Streetz KL, Betz U, Lauber J, et al. (2003) Interleukin-6/glycoprotein 130-dependent pathways are protective during liver regeneration. J Biol Chem 278: 11281–11288. [DOI] [PubMed] [Google Scholar]
- 39. Seki E, Tsutsui H, Iimuro Y, Naka T, Son G, et al. (2005) Contribution of Toll-like receptor/myeloid differentiation factor 88 signaling to murine liver regeneration. Hepatology 41: 443–450. [DOI] [PubMed] [Google Scholar]
- 40. Campbell JS, Riehle KJ, Brooling JT, Bauer RL, Mitchell C, et al. (2006) Proinflammatory cytokine production in liver regeneration is Myd88-dependent, but independent of Cd14, Tlr2, and Tlr4. J Immunol 176: 2522–2528. [DOI] [PubMed] [Google Scholar]
- 41. Vaquero J, Campbell JS, Haque J, McMahan RS, Riehle KJ, et al. (2011) Toll-like receptor 4 and myeloid differentiation factor 88 provide mechanistic insights into the cause and effects of interleukin-6 activation in mouse liver regeneration. Hepatology 54: 597–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Higgins GM, Anderson RM (1931) Experimental pathology of the liver I. Restoration of the liver of the white rat following partial surgical removal. Arch Pathol 12: 186–202. [Google Scholar]
- 43. Yokoyama HO, Wilson ME, Tsuboi KK, Stowell RE (1953) Regeneration of mouse liver after partial hepatectomy. Cancer Res 13: 80–85. [PubMed] [Google Scholar]
- 44. Doerr RJ, Castillo MH, Luchette FA, Caruna J (1990) Partial Hepatectomy in the Mouse. Clinical Anatomy 3: 279–286. [Google Scholar]
- 45. Paulsen JE (1990) Variations in regenerative growth of mouse liver following partial hepatectomy. In Vivo 4: 235–238. [PubMed] [Google Scholar]
- 46. Greene AK, Puder M (2003) Partial hepatectomy in the mouse: technique and perioperative management. J Invest Surg 16: 99–102. [PubMed] [Google Scholar]
- 47. Mitchell C, Willenbring H (2008) A reproducible and well-tolerated method for 2/3 partial hepatectomy in mice. Nat Protoc 3: 1167–1170. [DOI] [PubMed] [Google Scholar]
- 48. Boyce S, Harrison D (2008) A detailed methodology of partial hepatectomy in the mouse. Lab Anim (NY) 37: 529–532. [DOI] [PubMed] [Google Scholar]
- 49. Blindenbacher A, Wang X, Langer I, Savino R, Terracciano L, et al. (2003) Interleukin 6 is important for survival after partial hepatectomy in mice. Hepatology 38: 674–682. [DOI] [PubMed] [Google Scholar]
- 50. Huh CG, Factor VM, Sanchez A, Uchida K, Conner EA, et al. (2004) Hepatocyte growth factor/c-met signaling pathway is required for efficient liver regeneration and repair. Proc Natl Acad Sci U S A 101: 4477–4482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Factor VM, Seo D, Ishikawa T, Kaposi-Novak P, Marquardt JU, et al. (2010) Loss of c-Met disrupts gene expression program required for G2/M progression during liver regeneration in mice. PLoS One 5: e12739. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical procedure for 2/3 PH. (A) For 2/3 PH the left lower lobe (LLL), the left median and the right median lobe (LML and RML) are removed. (B) Each lobe is separately ligated (a-c) with taking special care not to disrupt the gallbladder (d).
(TIF)
NF-κB activation after 2/3 PH. (A) NF-κB activation in livers of indicated genotypes as assessed by anti-p65 IHC at 1 h and 4 h post PH. Nuclear staining is occasionally observed in non-parenchymal cells (white arrowheads) only in control and RelaF/FAlbCre animals at 1 h and to a lesser extent at 4 h post PH. Nuclear staining for p65 is almost never detected in hepatocytes of either genotype (black arrowhead marks a positive hepatocyte in a control animal). Nuclear staining was nearly completely absent in RelaF/FMxCre animals both in hepatocytes and non-parenchymal cells (magnification×200). (B) No robust NF-κB binding activity could be detected by EMSA analysis 1 h post PH in livers of indicated genotypes. Liver lysates from LPS-treated animals served as positive control (LPS 2 mg/kg i.p.).
(TIF)