Abstract
Objective
To examine past year dental visits among underserved, Hispanic farmworker families using the Andersen Behavioral Model of Health Services Utilization (1968), which posits that predisposing, enabling, and need factors influence care-seeking behavior.
Methods
Oral health survey and clinical data were collected in 2006-7 from families in Mendota, California (Fresno County) as part of a larger, population-based study. Generalized estimating equation logit regression assessed effects of factors on having a dental visit among adults (N=326). Predisposing variables included socio-demographic characteristics, days worked in agriculture, self-rated health status, and dental beliefs. Enabling factors included resources to obtain services (dental insurance, income, acculturation level, regular dental care source). Need measures included perceived need for care and reported symptoms, along with clinically-determined untreated caries and bleeding on probing.
Results
Only 34% of adults had a past year dental visit, despite 44% reporting a regular dental care source. Most (66%) lacked dental insurance, and nearly half (46%) had untreated caries. Most (86%) perceived having current needs, and on average, reported a mean of 4.2 dental symptoms (of 12 queried).
Regression analyses indicated those with more symptoms were less likely to have a past year dental visit. Those who would ask a dentist for advice and had a regular dental care source were more likely to have a past year dental visit.
Conclusions
The final model included predisposing, enabling and need factors. Despite low utilization and prevalent symptoms, having a regular source of care helps break this pattern and should be facilitated.
Keywords: dental health services, Hispanic, agricultural workers
Introduction
One of California's largest industries is agriculture, with the state producing over 400 commodities, and about half of the country's fruits, nuts, and vegetables [1]. Yet, little research has focused on the health needs of California agricultural workers or their families. In 1999, the California Institute for Rural Studies conducted the first state-wide population-based California Agricultural Worker Health Survey (CAWHS) [2]. The CAWHS estimated there were about 700,000 agricultural workers, and that the majority were foreign-born, relatively young, male, married, and Hispanic, who neither read nor speak English, and had on average 6 years or less of formal education. The CAWHS included a dental component, and surveyed 971 agricultural workers. The report documented dental problems as the most common health complaint with over one-quarter of the survey respondents reporting, as well as very low dental utilization rates with nearly half never having been to a dentist. Studies of migrant agricultural workers in other states have reported similar oral health findings [3-7].
Agricultural workers face multiple barriers to accessing needed healthcare, including dental care [8]. The most commonly cited reasons for irregular dental care are lacking time, money, transportation, and basic oral health knowledge [5, 7, 9]. These workers are in a low paying, hazardous industry usually not providing health insurance. They are an especially vulnerable group, and access to regular care is complicated by the seasonal and sometimes migratory nature of their work. When they do need dental care, the community and migrant dental clinics that could treat them tend to have limited operating hours and be underfunded and understaffed [5].
Arcury and Quandt [9] recently summarized the multiple health care needs and common barriers to care that United States (U.S.) migrant and seasonal agricultural workers face and suggest more research is needed on their care utilization patterns. This research aims to fill this gap, and investigate factors associated with dental utilization patterns of adults in agricultural worker families in California's Central Valley.
The conceptual framework for this study is the well established Andersen and colleagues' Behavioral Model of Health Services Utilization [10, 11], which focuses on predisposing, enabling, and need characteristics as determinants of health service utilization. According to the model, whether or not an individual seeks healthcare depends on each of these domains. This model was chosen because it has the advantage of identifying factors most predictive of dental utilization. Those factors can then inform focused efforts to facilitate care for that population, as many factors are potentially amenable to change and intervention.
Predisposing factors are primarily individual demographic characteristics (such as age, sex, race), but also include beliefs about care-seeking and the healthcare system (e.g., value placed on dental visits). Enabling factors refer to the resources available to the individual to obtain services, such as income, and having dental insurance and having a dental home. The need component includes both perceived and professionally evaluated health status. Perceived need is important to assess, but can vary widely among individuals. For instance, some individuals may notice bleeding gums when brushing their teeth, and interpret it as indicative of an urgent need to see a dentist for a check-up, while the same symptom may be dismissed by others as normal. Often, perceived need is a strong predictor of, and motivator for, care-seeking.
Past studies have applied this model to examine dental utilization patterns in several different adult samples [12-19]. Despite the different study samples, collectively the literature suggests which factors may be most relevant within this framework. Race and dental care-related beliefs were the two most common important predisposing factors in dental utilization. Although based on older data, findings from the 1986 National Health Interview Survey (NHIS) indicated that Mexican Americans were the least likely to access dental services, regardless of their income or education level [12]. The payment source for dental services significantly related to past year dental visits among lower income mothers [18]. Perceived need, however, was the strongest dental care determinant in many prior studies [14, 17-19].
Agricultural workers and their families are a unique group with high documented need and low dental utilization. The current study examines a range of predisposing, enabling, and need factors associated with past year dental visits in this adult group using recent data collected from California's agricultural worker families. Reasons for their dental service utilization, or lack thereof, were also explored.
Methods
Sample
Data analyzed for this study are from a larger population-based epidemiologic study of a cohort of agricultural families conducted by researchers at the University of California (UC) Davis. The UC Davis Immigration to California: Agricultural Safety and Acculturation (MICASA) study invited the UC San Francisco Center to Address Disparities in Children's Oral Health (nicknamed CAN DO) to add a dental component to the project, which is the focus of the present study. The dental study was approved by the UC San Francisco Institutional Review Board.
UC Davis employed a two-stage sampling process, stratifying on the two census tracts in Mendota, California (a small rural community in the central San Joaquin Valley in Fresno County) and a door-to-door enumeration to identify eligible participants. To be eligible for MICASA, at least one adult household member had to be between 18-55 years old, self-identified as Hispanic, engaged in farmwork in the U.S. for at least 30 days in the prior year, and a Mendota resident at the time of the interview. A random, community-based sample of 335 farmworker families in Mendota, was selected as the final MICASA study cohort. Families eligible for the dental study were determined from 445 MICASA households with at least one child under age 18. Data were collected on 213 families (representing 64% of the 335 eligible), These families were invited to participate in the dental component. Local bilingual interviewers contacted the family, and obtained additional informed consent for the dental component.
Data collection
Dental exams were conducted at the study field office by one trained, experienced dental examiner using portable equipment following universal infection control guidelines and National Health and Nutrition Examination Survey (NHANES) criteria [20]. A bilingual assistant entered the clinical data electronically into a secure computer. The interviews were conducted mostly in the family's home (or the field office, as preferred) by local, trained bilingual interviewers familiar with the local culture and institutions. All data were collected during 2006-7. Each adult was interviewed separately, in Spanish, in a face-to-face format. All self-reported variables were collected during face-to-face interviews and data were entered by the interviewer into a database (Microsoft Access, Redmond, WA). Families received a $15 gift certificate and toothbrushes for each participant as an honorarium for their time and inconvenience.
Measures
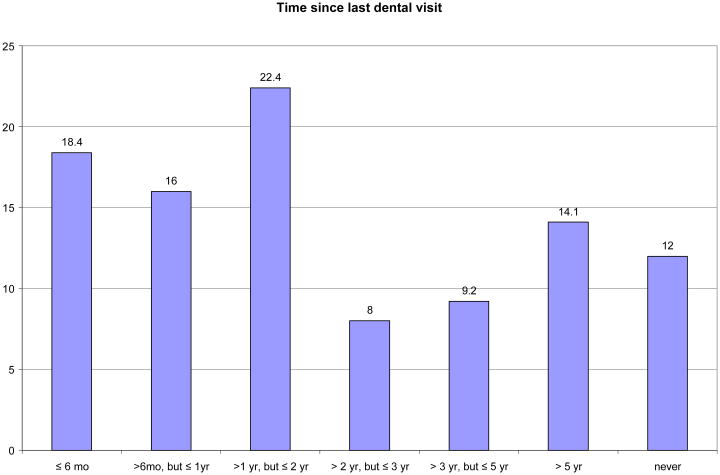
The dependent variable in this study was self-report of past dental utilization, recoded into a dichotomy for a dental visit in the past year. This cut-point differentiates dental visits that were either regular preventive care or restorative care for a recent ailment versus those visits that were irregular, neglected, or postponed (see Figure 1). Ordinal time since last visit was also examined. Additional descriptive information about reasons for not getting dental care when needed as well as reasons for ever visiting a dentist were examined.
Figure 1.
The independent variables were selected following the Behavioral Model of Health Services Utilization. Predisposing factors included the following individual socio-demographic characteristics: age (continuous), sex (male or female), marital status (married or not), and the number of days worked in farming prior year (continuous). The individual's self-rated general health status (recoded as fair/poor or good/very good/excellent) and whether or not s/he would ask a dentist for advice if s/he had a dental problem/concern were also predisposing variables.
Enabling factors included the following resources that may be available to help successfully access care: highest grade level of education completed (continuous), annual household income (recoded as <$10,000, $10-$19,999, or ≥$20,000- a 3-level measure of poverty: below poverty level, within poverty level, and above poverty level. The federal poverty threshold for a family of four in 2006-7 was about $20,000.), household size (numeric), dental insurance status (insured or not), acculturation level (the validated reliable Acculturation Rating Scale for Mexican Americans-II, ARSMA-II) [21] (numeric), and reporting a regular source of dental care. The ARSMA-II scale is the average of 12 items assessing how often individuals think, read, write, speak, and watch television in English versus Spanish on a 5 point Likert scale as reported during interviews.
Need factors included two clinical and two self-reported measures of need. Dichotomous clinical variables for any untreated carious, decayed surfaces (defined as DS>0) and any bleeding of gums in either of the two quadrants probed were derived from the dental exams. Perceiving a dental need and a count of dental symptoms experienced at the time of the interview out of twelve queried (numeric) were included as well. The dental symptom list was adapted from Gilbert and colleagues [22], including items from mild (e.g., food catching in teeth often, bad breath, dry mouth, sensitivity) to more severe (e.g., toothaches, abscesses, loose teeth, broken teeth).
Data Analysis
Adults were included in this analysis if they self-reported Hispanic ethnicity (N=326). Measures had few missing items (less than 10% for any single variable). To use all available data and maintain the maximum sample size, the few missing items were imputed using the SAS-callable IVEware [23] multiple imputation procedure before scales were constructed or any analyses were conducted. All variables in the models except for marital status and gender had some missing items that were imputed for analysis. The distributions of all variables were explored. Descriptive statistics and bivariable associations between each variable of interest and the dependent variable were analyzed.
Generalized estimating equation (GEE) logit regression analyses assessed the effects of predisposing, enabling, and need factors on the likelihood of a dental visit in the prior year among adults, using SAS version 9 PROC GENMOD to account for clustering of adults within households [24]. Model 1 included only predisposing factors, Model 2 included predisposing and enabling factors, and Model 3 included predisposing, enabling and need factors together. The tolerances (equivalent to the reciprocal of variance inflation factors) of variables in each model were examined to check for potential multicollinearity issues, and none were found. A Box-Tidwell method was applied to the need factor of the number of dental symptoms to test the assumption of linearity.
Results
Table 1 describes the study sample characteristics. The average age of adults was about 37 years old, most were female and married, and worked in agriculture for an average of 125 days in the prior year. Two-thirds rated their own general health as fair or poor relative to others, and just over one-third would ask a dentist for dental advice. ARSMA-II acculturation scale scores indicated that the sample was highly oriented to Mexican culture. Adults reported an average of 6 years of education, and most (77%) had incomes below $20,000 to support an average household size of five. Two-thirds did not have dental insurance; virtually all of those with any dental insurance had Medicaid (Denti-Cal). Less than half (44%) had a regular source of dental care. Nearly all adults (86%) believed they needed dental care, and self-reported an average of 4 symptoms. Almost half (46%) had untreated caries, and another 46% gums bled when probed.
Table 1. Characteristics of the study sample of adult agricultural workers (N=326).
| Variable | n | % | mean | sd | min | max |
|---|---|---|---|---|---|---|
| Predisposing factors | ||||||
| Age (years) | 36.7 | 9 | 20 | 61 | ||
| Male | 106 | 32.5 | ||||
| Married | 217 | 66.6 | ||||
| Days worked farming in last year | 125.4 | 83.9 | 20 | 250 | ||
| Ask dentist advice | 113 | 34.7 | ||||
| Fair/Poor general health | 209 | 64.1 | ||||
| Enabling factors | ||||||
| ARSMA-II Acculturation scale | −3.4 | 1 | −4 | 1.5 | ||
| Education | 6.4 | 3.6 | 0 | 22 | ||
| Income <$10,000 | 110 | 33.7 | ||||
| Income $10,000-$19,999 | 142 | 43.6 | ||||
| Income >$20,000 | 74 | 22.7 | ||||
| Household size | 5.1 | 1.6 | 2 | 14 | ||
| No dental insurance | 216 | 66.3 | ||||
| Regular source of dental care | 142 | 43.6 | ||||
| Need factors | ||||||
| Untreated decay (DS>0) | 151 | 46.3 | ||||
| Any gum bleeding on probing | 150 | 46.0 | ||||
| Subjective need | 280 | 85.9 | ||||
| Self-reported symptoms | 4.2 | 3 | 0 | 12 | ||
| Outcome | ||||||
| Dental visit in prior year | 112 | 34.4 | ||||
Figure 1 displays the time since prior dental visit. Overall, 12% had never been to a dentist, and about one-third had been in the prior year, while the remainder reported a visit more than one year prior. Among those who did not get dental care when needed, (n=182), half indicated it was due to cost, and one-third indicated it was due to lack of insurance. The remainder did not know (7%), while 6% reported encountering various barriers such as not getting time off work, being afraid, difficulty getting an appointment, waiting too long for an appointment, not knowing where to go, or the dentist not accepting their insurance. A few noted other unspecified reasons (2%). Among those who had ever been to the dentist (n=270), 58% went in for a problem or pain, 29% went in on their own for an exam or cleaning, 6% went in for treatment, 3% were for other unspecified reasons, 3% were contacted by the dentist for an exam or cleaning, and <1% didn't know.
The statistically significant bivariable associations between the explanatory variables and outcome are summarized in Table 2. Several predisposing, enabling, and all of the need factors were significantly associated with prior year dental visits. Older age, being married, and asking a dentist for advice were predisposing factors positively associated with prior utilization. Higher income, larger household size, and a regular source of dental care were enabling factors positively associated with prior utilization, while lack of insurance was negatively associated. All the need factors were negatively associated with the outcome.
Table 2. Bivariable associations between past year dental visits and the predisposing, enabling, and need factors and prior year dental visit.
| GEE logit model | |||
|---|---|---|---|
| OR | 95% CI | p-value | |
| Predisposing factors | |||
| Age | 1.05 | 1.03-1.09 | <0.0001 |
| Male | 0.76 | 0.49-1.18 | 0.2160 |
| Married | 1.96 | 1.13-3.39 | 0.0171 |
| Days work farming | 1.00 | 0.99-1.01 | 0.4818 |
| Ask dentist advice | 3.73 | 2.24-6.20 | <0.0001 |
| Fair/Poor general health | 0.75 | 0.45-1.26 | 0.2835 |
|
| |||
| Enabling factors | |||
| ARSMA-II Acculturation scale | 1.09 | 0.87-1.38 | 0.4408 |
| Education | 0.98 | 0.92-1.05 | 0.5329 |
| Income $10,000-$19,999 | 1.26 | 0.77-2.06 | 0.3524 |
| Income $20,000+ | 1.76 | 1.00-3.12 | 0.0514 |
| Household size | 1.17 | 1.01-1.35 | 0.0332 |
| No dental insurance | 0.25 | 0.15-0.41 | <0.0001 |
| Regular source dental care | 4.45 | 2.73-7.23 | <0.0001 |
|
| |||
| Need factors | |||
| Untreated decay | 0.61 | 0.38-0.99 | 0.0462 |
| Any gum bleeding on probing | 0.55 | 0.35-0.89 | 0.0138 |
| Self-reported symptoms | 0.81 | 0.74-0.88 | <0.0001 |
| Subjective need | 0.52 | 0.28-0.95 | 0.0329 |
OR = odds ratio
CI = confidence interval
Reference groups for categorical variables: female, not married, not ask dentist for dental advice, good/very good/excellent general health, income less than $10,000, has dental insurance, no regular source of dental care, no untreated decay, no bleeding on probing, no subjective need.
Table 3 presents results from the nested logistic regression analyses. In Model 1, two predisposing factors were positively associated with prior year dental visits. Older adults were more likely to have had a visit (odds ratio, or OR = 1.05, 95% confidence interval, or CI = 1.02-1.08, p<0.001), and those that would ask a dentist for advice were over three times more likely to have a visit (OR = 3.35, 95% CI = 1.88-5.95, p<0.001). Age was not statistically significant in later models, but asking a dentist for advice remained important and in Model 2 (OR = 4.79, 95% CI = 2.45-9.36, p<0.001) when enabling factors were added. Those with a regular source of dental care were nearly five times as likely to have a prior year dental visit (OR = 4.90, 95% CI = 2.57-9.37, p<0.001). Finally, Model 3 assessed all predisposing, enabling, and need factors simultaneously. Asking a dentist for advice and having a regular source of care remained statistically significant with estimates of similar magnitude as the previous model. The only need variable related to the outcome was the count of self-reported dental symptoms. The more symptoms adults reported, the less likely they were to have a past year dental visit (OR = 0.85, 95% CI = 0.76-0.94, p<0.001). There was no evidence of a departure of linearity for the symptoms measure. Each variable in the models is included not only as a means of assessing its individual impact on recent dental visit, but also as a potential confounding variable whose inclusion in the model is vital to reduce possible bias on other variables.
Table 3. GEE Logit regression analyses for adults with a prior year dental visit (N=326).
| MODEL 1 | MODEL 2 | MODEL 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Predisposing | Predisposing and enabling | Predisposing, enabling & need | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | ||||
| Predisposing factors | |||||||||
| Age | 1.05 | *** | 1.02-1.08 | 1.03 | 0.99-1.06 | 1.02 | 0.98-1.05 | ||
| Male | 0.59 | 0.33-1.06 | 0.66 | 0.36-1.23 | 0.63 | 0.34-1.14 | |||
| Married | 1.71 | 0.93-3.12 | 1.28 | 0.69-2.37 | 1.28 | 0.68-2.32 | |||
| Days worked farming | 1.00 | 0.99-1.01 | 1.00 | 0.99-1.01 | 1.00 | 0.99-1.01 | |||
| Ask dentist advice | 3.35 | *** | 1.88-5.95 | 4.79 | *** | 2.45-9.36 | 4.62 | *** | 2.25-9.50 |
| Fair/poor general health | 0.86 | 0.49-1.50 | 0.81 | 0.44-1.48 | 0.94 | 0.48-1.79 | |||
| Enabling factors | |||||||||
| ARSMA-II Acculturation scale | 0.85 | 0.65-1.11 | 0.86 | 0.66-1.14 | |||||
| Education | 0.93 | 0.85-1.02 | 0.94 | 0.86-1.03 | |||||
| Income $10,000-$19,999 | 1.71 | 0.84-3.47 | 1.58 | 0.78-3.20 | |||||
| Income $20,000+ | 1.28 | 0.54-3.02 | 1.08 | 0.45-2.60 | |||||
| Household size | 1.10 | 0.94-1.29 | 1.12 | 0.94-1.34 | |||||
| No dental insurance | 0.56 | 0.30-1.04 | 0.62 | 0.33-1.17 | |||||
| Regular source of dental care | 4.90 | *** | 2.57-9.37 | 4.82 | *** | 2.46-9.43 | |||
| Need factors | |||||||||
| Untreated decay | 1.01 | 0.54-1.92 | |||||||
| Any gum bleeding on probing | 0.57 | 0.31-1.06 | |||||||
| Self-reported symptoms | 0.85 | ** | 0.76-0.94 | ||||||
| Subjective need | 0.77 | 0.37-1.64 | |||||||
p<0.05;
p<0.01;
p<0.001
OR = odds ratio
CI = confidence interval
Reference groups for categorical variables: female, not married, not ask dentist for dental advice, good/very good/excellent general health, income less than $10,000, has dental insurance, no regular source of dental care, no untreated decay, no bleeding on probing, no subjective need.
Discussion
This study explored the predisposing, enabling, and need factors associated with prior year dental utilization in a California adult sample of agricultural workers. Only 34% of adults reported a prior year visit, which falls in the 20-47% range of reported estimates from prior studies of other adult agricultural worker populations [2, 3, 5, 7]. The low utilization rates suggest that the historical barriers to access still persist for farmworkers, who continue to mostly seek care for major dental problems and pain. Examining factors related to utilization may help to better understand how to improve access to dental services.
Based on the multivariable regression analyses, two factors were positively associated with prior visits – asking a dentist for advice and having a regular source of dental care – while a greater number of self-reported symptoms was negatively associated. We did not find the same pattern of sociodemographic or socioeconomic status (SES) factors related to utilization as some past studies of adult samples [14, 18], which is likely due to the relatively homogenous sample and most agricultural worker families being very low SES. Instead, the perceptions about dentists were important, and asking a dentist for dental advice over a physician, family, friends, promotora or others was related to prior utilization. However, most adults in our study did not have a regular dental provider, so they would be unable to seek dental advice from a dentist. It is also unclear where they get dental information, or how accurate that information might be. The survey question does not reflect actual behavior of having asked a dentist for dental advice, and instead this question likely captures a belief that a dentist has recognized expertise in this area, or perhaps is a trusted source of dental information. Trust has been positively associated with having a dental home in one study [25], but asking a dentist for advice was not correlated with having a regular source of dental care in our study. Although dental attitudes and knowledge were not extensively assessed in this survey, the positive regard for dentists is promising. It is possible that if dental providers were more accessible to serve this population, their recommendations for seeking routine and preventive care may be heeded and utilization patterns improved.
A regular source of dental care (dental home) was also related to a prior year visit, but less than half of adults (44%) had a dental home. Several other studies showed that a regular source of dental care is important for utilization [14, 15, 26], which is not surprising. Historically, a major access issue has been a large shortage of dentists and other healthcare providers to serve agricultural worker populations [5]. Mendota is already designated as a Health Professional Shortage Area (HPSA) [27], and although there are federal programs for provider loan repayment for working in HPSAs, the program budget and dentist enrollment are not enough to meet the need of HPSAs nationwide. This problem may best be addressed through systemic policy changes that offer better incentives to entice healthcare providers to practice in underserved areas. The agricultural worker families in this study are somewhat atypical in that they are mostly non-migrant workers, and part of a stable population having lived and worked in Mendota for several years. For these adults to establish a dental home and have a regular source of care, there needs to be more dental providers offering culturally appropriate dental services during hours the workers can attend.
Our results also revealed that despite most adults reporting an average of four dental symptoms, most did not go to the dentist in the prior year. While the perceived severity and impact of each symptom was not assessed, pain and dental problems were the main reasons for past visits. Some studies have found similar results showing those with more symptoms being less likely to have utilized dental services [18], while some document the opposite relationship [19]. It could be that those who have sought care previously have been treated, provided education and prevention so they had fewer symptoms at the time of assessment. Conversely, it could be that symptoms have not yet reached a high enough level of pain to warrant immediate attention. With cross-sectional data the temporal sequence cannot be ascertained. However, there is a widespread recognition of need for care, and it is likely there are simply too many financial and access barriers to obtaining care. The major reasons cited for not getting needed care were the cost and lack of dental insurance.
Expanding dental insurance coverage in this population might have been a possible implication from our findings before this year. Unfortunately, given the country's economic downturn and California's recent budget crisis, adult Denti-Cal benefits were virtually eliminated as of July 1, 2009 [28]. This means the one-third of adults who reported having Denti-Cal at the time of data collection for this study now lack dental insurance. Since under Medicaid adult dental coverage is an optional benefit for states, these benefits might be reinstated at a later date, but its future is uncertain. The impact of this cut will undoubtedly be negative for the state's agricultural workers and many other lower income groups who previously relied on this insurance to help them access dental services. Now, almost none of the adults in this population will have dental insurance, which will further inhibit regular dental service utilization. State or national level policy changes to remedy the problem of the uninsured and better integrate oral health into general health are needed [29].
Access to care has historically been difficult for this population in California, as well as across the nation. The common barriers of a lack of time, money, transportation, ability to take time off from work, basic oral health knowledge, perceived need, and dental providers have persisted for decades [5, 7, 9]. Cultural factors based on limited access to care and patterns of utilization in their countries of origin may also play a role in current utilization. Even prior to the Denti-Cal cuts, options for dental services were limited. Agricultural workers' access is similar to that of other lower income groups. Despite the existence of some state and federal programs that provide health services specifically for agricultural workers, not all offer dental care due to lack of funds and providers [30, 31].
This study contributes to the dearth of current research on dental utilization patterns among adult agricultural worker families, and has several strengths. The size and scope of the dental exams and interviews are broader than in many other previous studies, collecting information from a fairly large number of families drawn from a population-based sample. Agricultural families in this part of California are especially difficult to recruit, examine, interview and follow-up, and warrant study to produce current detailed statistics about them. Alternate analyses (not shown) exploring different definitions for the main outcome and different operationalizations of explanatory variables were explored, and similar results were found. Few other studies have included both clinically determined as well as self-assessed need variables when using this model [16, 19]. A benefit of this model is the ability to identify the most important potentially modifiable characteristics of the population at risk associated with accessing care and utilization of services. Our findings have policy action implications to help improve access to care for this group.
There are some limitations to consider as well. This analysis was cross-sectional, thus causality can not be determined. It is possible that some important predisposing, enabling, and need factors were not assessed and so could not be included in the model, such as dental beliefs or biological risk factor information. Future studies could be designed to address some of these issues.
Adult agricultural workers are a fairly unique and historically underserved population with many dental symptoms and unmet needs. Many barriers need to be overcome including greater availability of dental advice to facilitate transition of care seeking due to pain or problems to a more regular and preventive focused mode of service use. Having a regular source of care was very positively associated dental utilization indicating that these barriers are not insurmountable.
Acknowledgments
We gratefully acknowledge the participating Mendota families, and Dr. Schenker and our UC Davis colleagues for including this dental component in their larger study.
Research Support: This research was part of a larger, population-based study supported by USDHHS/NIH#U54DE14251, NIOSH#2U50OH007550-06 & The California Endowment, conducted by the University of California San Francisco's Center to Address Disparities in Children's Oral Health (Jane Weintraub, PI) in partnership with colleagues from the University of California, Davis. These findings were presented in part on October 28, 2008 at the American Public Health Association annual meeting in San Diego, CA.
Contributor Information
Tracy L. Finlayson, San Diego State University, Graduate School of Public Health.
Stuart A. Gansky, UC San Francisco School of Dentistrys.
Sara G. Shain, UC San Francisco School of Dentistry.
Jane A. Weintraub, UC San Francisco School of Dentistry.
References
- 1.California Department of Food and Agriculture, Agricultural Statistical Review. In the California Agricultural Resource Directory 2008-9. 2007 [cited 2009 July 2]. Available from http://www.cdfa.ca.gov/statistics/files/CDFA_Sec2.pdf.
- 2.Villarejo D, Lighthall D, Williams D, Souter A, Mines R, Bade B, Samuels S, McCurdy SA. Suffering in Silence: A Report on the Health of California's Agricultural Workers. The California Endowment; Woodland Hills, CA: 2000. [Google Scholar]
- 3.Quandt SA, Clark HM, Rao P, Arcury TA. Oral health of children and adults in Latino migrant and seasonal farmworker families. J Immigr Minor Health. 2007;9(3):229–35. doi: 10.1007/s10903-006-9033-7. [DOI] [PubMed] [Google Scholar]
- 4.Quandt SA, Hiott AE, Grzywacz JG, Davis SW, Arcury TA. Oral health and quality of life of migrant and seasonal farmworkers in North Carolina. J Agric Saf Health. 2007;13(1):45–55. doi: 10.13031/2013.22311. [DOI] [PubMed] [Google Scholar]
- 5.Lukes SM, Miller FY. Oral health issues among migrant farmworkers. J Dent Hyg. 2002;76:134–140. [PubMed] [Google Scholar]
- 6.Lukes SM, Simon B. Dental decay in southern Illinois migrant and seasonal farmworkers: an analysis of clinical data. J Rural Health. 2005;21(3):254–8. doi: 10.1111/j.1748-0361.2005.tb00091.x. [DOI] [PubMed] [Google Scholar]
- 7.Entwhistle BA, Swanson TM. Dental needs and perceptions of adult Hispanic migrant farmworkers in Colorado. J Dent Hyg. 1989;63(6):286–92. [PubMed] [Google Scholar]
- 8.Hansen E, Donohoe M. Health issues of migrant and seasonal farmworkers. J Health Care Poor Underserved. 2003;14(2):153–64. doi: 10.1353/hpu.2010.0790. [DOI] [PubMed] [Google Scholar]
- 9.Arcury TA, Quandt SA. Delivery of health services to migrant and seasonal farmworkers. Ann Rev Public Health. 2007;28:345–63. doi: 10.1146/annurev.publhealth.27.021405.102106. [DOI] [PubMed] [Google Scholar]
- 10.Aday L. Indicators and predictors of health services utilization. 4th. Albany, NY: Delmar; 1993. Introduction to health services; pp. 46–70. [Google Scholar]
- 11.Andersen RA. A behavioral model of families' use of health services. Vol. 25. Chicago, IL: Center for Health Administration Studies, University of Chicago, Research Series; 1968. [Google Scholar]
- 12.Atchison KA, Der-Martirosian C, Gift HC. Components of self-reported oral health and general health in racial and ethnic groups. J Pub Health Dent. 1998;58(4):301–8. doi: 10.1111/j.1752-7325.1998.tb03013.x. [DOI] [PubMed] [Google Scholar]
- 13.Shiboski CH, Cohen M, Weber K, Shansky A, Malvin K, Greenblatt RM. Factors associated with use of dental services among HIV-infected and high-risk uninfected women. J Am Dent Assoc. 2005;136(9):1242–1255. doi: 10.14219/jada.archive.2005.0340. [DOI] [PubMed] [Google Scholar]
- 14.Evashwick C, Conrad D, Lee F. Factors related to utilization of dental services by the elderly. Am J Public Health. 1982;72(10):1129–1135. doi: 10.2105/ajph.72.10.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davidson PL, Andersen RM. Determinants of dental care utilization for diverse ethnic and age groups. Adv Dent Res. 1997;11(2):254–262. doi: 10.1177/08959374970110020801. [DOI] [PubMed] [Google Scholar]
- 16.Reisine S. A path analysis of the utilization of dental services. Community Dent Oral Epidemiol. 1987;15(3):119–24. doi: 10.1111/j.1600-0528.1987.tb00497.x. [DOI] [PubMed] [Google Scholar]
- 17.Atchison KA, Mayer-Oakes SA, Schweitzer SO, Lubben JE, De Jong FJ, Matthias RE. The relationship between dental utilization and preventive participation among a well-elderly sample. J Public Health Dent. 1993;53(2):88–95. doi: 10.1111/j.1752-7325.1993.tb02681.x. [DOI] [PubMed] [Google Scholar]
- 18.Kuthy RA, Odom JG, Salsberry PJ, Nickel JL, Polivka BJ. Dental utilization by low-income mothers. J Public Health Dent. 1998;58(1):44–50. doi: 10.1111/j.1752-7325.1998.tb02989.x. [DOI] [PubMed] [Google Scholar]
- 19.Gilbert GH, Duncan RP, Vogel WB. Determinants of dental care use in dentate adults: Six-monthly use during a 24-month period in the Florida dental care study. Soc Sci Med. 1998;47(6):727–37. doi: 10.1016/s0277-9536(98)00148-8. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention (CDC) Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2001. National Center for Health Statistics (NCHS), National Health and Nutrition Examination Survey Dental Examiners Procedure Manual. [Cited 2009 June 2] Available from http://www.cdc.gov/nchs/data/nhanes/oh-e.pdf. [Google Scholar]
- 21.Cuellar I, Arnold B, Maldonado R. Acculturation Rating Scale for Mexican Americans-II: A Revision of the Original ARSMA Scale. Hispanic J Behav Sci. 1995;17(3):275–304. [Google Scholar]
- 22.Gilbert GH, Duncan RP, Shelton BJ. Social determinants of tooth loss. Health Serv Res. 2003;38(6 Pt 2):1843–62. doi: 10.1111/j.1475-6773.2003.00205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Imputation and Variance Estimation software, or IVEware: University of Michigan's Survey Research Center, Institute for Social Research
- 24.SAS Statistical Package. SAS Institute, Inc.; Cary, N.C.: 2000. [Google Scholar]
- 25.Graham MA, Logan HL, Tomar SL. Is trust a predictor of having a dental home? J Am Dent Assoc. 2004;135(11):1550–1558. doi: 10.14219/jada.archive.2004.0081. [DOI] [PubMed] [Google Scholar]
- 26.Davidson PL, Cunningham WE, Nakazono TT, Andersen RM. Evaluating the Effect of Usual Source of Dental Care on Access to Dental Services: Comparisons among Diverse Populations. Med Care Res Rev. 1999;56(1):74–93. doi: 10.1177/107755879905600105. [DOI] [PubMed] [Google Scholar]
- 27.U.S. Department Health and Human Services, H.R.S.A. Find Shortage Areas: HPSA by State and County. [cited 2009 August 14] Available from http://hpsafind.hrsa.gov/HPSASearch.aspx.
- 28.California Medi-Cal Dental Program. Elimination of most adult dental services. Denti-Cal Bulletin. 2009;25(22):1–7. [Google Scholar]
- 29.Fisher-Owens SA, Barker JC, Adams S, Chung LH, Gansky SA, Hyde S, Weintraub J. Giving Policy Some Teeth: Routes To Reducing Disparities In Oral Health. Health Aff. 2008;27(2):404–412. doi: 10.1377/hlthaff.27.2.404. [DOI] [PubMed] [Google Scholar]
- 30.Lukes SM, Simon B. Dental services for migrant and seasonal farmworkers in US community/migrant health centers. J Rural Health. 2006;22(3):269–272. doi: 10.1111/j.1748-0361.2006.00044.x. [DOI] [PubMed] [Google Scholar]
- 31.Lombardi GR. Dental/oral health services. Migrant Health Issues, Monograph Series. 2002;1:1–8. [Google Scholar]