Abstract
Background
Single-legged hop tests are commonly used functional performance measures that can capture limb asymmetries in patients after anterior cruciate ligament (ACL) reconstruction. Hop tests hold potential as predictive factors of self-reported knee function in individuals after ACL reconstruction.
Hypothesis
Single-legged hop tests conducted preoperatively would not and 6 months after ACL reconstruction would predict self-reported knee function (International Knee Documentation Committee [IKDC] 2000) 1 year after ACL reconstruction.
Study Design
Cohort study (prognosis); Level of evidence, 2.
Methods
One hundred twenty patients who were treated with ACL reconstruction performed 4 single-legged hop tests preoperatively and 6 months after ACL reconstruction. Self-reported knee function within normal ranges was defined as IKDC 2000 scores greater than or equal to the age- and sex-specific normative 15th percentile score 1 year after surgery. Logistic regression analyses were performed to identify predictors of self-reported knee function within normal ranges. The area under the curve (AUC) from receiver operating characteristic curves was used as a measure of discriminative accuracy.
Results
Eighty-five patients completed single-legged hop tests 6 months after surgery and the 1-year follow-up with 68 patients classified as having self-reported knee function within normal ranges 1 year after reconstruction. The crossover hop and 6-m timed hop limb symmetry index (LSI) 6 months after ACL reconstruction were the strongest individual predictors of self-reported knee function (odds ratio, 1.09 and 1.10) and the only 2 tests in which the confidence intervals of the discriminatory accuracy (AUC) were above 0.5 (AUC = 0.68). Patients with knee function below normal ranges were over 5 times more likely of having a 6-m timed hop LSI lower than the 88% cutoff than those with knee function within normal ranges. Patients with knee function within normal ranges were 4 times more likely to have a crossover hop LSI greater than the 95% cutoff than those with knee function below normal ranges. No preoperative single-legged hop test predicted self-reported knee function within normal ranges 1 year after ACL reconstruction (all P > .353).
Conclusion
Single-legged hop tests conducted 6 months after ACL reconstruction can predict the likelihood of successful and unsuccessful outcome 1 year after ACL reconstruction. Patients demonstrating less than the 88% cutoff score on the 6-m timed hop test at 6 months may benefit from targeted training to improve limb symmetry in an attempt to normalize function. Patients with minimal side-to-side differences on the crossover hop test at 6 months possibly will have good knee function at 1 year if they continue with their current training regimen. Preoperative single-legged hop tests are not able to predict postoperative outcomes.
Keywords: anterior cruciate ligament reconstruction, hop testing, self-report measure, knee function
Anterior cruciate ligament (ACL) injuries are prevalent in athletics,15 with more than 125,000 ACL reconstructions performed annually in the United States.24,27 Athletes are frequently counseled to undergo ACL reconstruction with the expectation that surgery will restore knee function and facilitate return to previous levels of activity.33,39 Surgical reconstruction of the ACL, however, does not guarantee a return to previous levels of activity, good knee function, or future joint preservation.7,14,33 Although returning to preinjury levels or back to sport may be a short-term goal after reconstruction,6 intent to return to sports is not predictive of actual return to play.3 Patients may reduce their activity levels for a variety of reasons, including social reasons, knee problems, or fear of reinjury.39,52
The International Knee Documentation Committee 2000 subjective knee form (IKDC 2000) is a knee-specific outcome measure for assessing symptoms, function, and sports activity.25 The IKDC 2000 is frequently used to assess knee function in patients after ACL reconstruction and contains items highly relevant to individuals with a reconstructed ACL.17 It differentiates patients with more knee symptoms from those with fewer symptoms, as well as those with lower knee function from those with higher knee function.1 The normative database of the IKDC 2000 can be used as a standard of successful patient-reported outcomes.16 Not all individuals regain satisfactory knee function after ACL reconstruction.2,4 Impairments or physical performance measures that predict successful knee function can be used to optimize rehabilitation to maximize knee function after ACL reconstruction.
Age, sex, body mass index (BMI), smoking, concomitant injuries, and physical impairments before and after surgery are important determinants of expected and final outcomes after ACL reconstruction28,29,48 but do not fully explain the observed variance in knee function after ACL reconstruction and rehabilitation. Performance-based measures are important indicators of knee function after ACL reconstruction48 and capture different aspects of overall knee performance and function from physical impairments.13
Single-legged hop tests are performance-based measures used to assess the combination of muscle strength, neuromuscular control, confidence in the limb, and the ability to tolerate loads related to sports-specific activities.46 These tests are commonly used to quantify knee performance in patients after reconstruction.46,48,53 Hop tests hold potential as predictive factors in identifying self-reported knee function in individuals after ACL reconstruction. Single-legged hop tests can discriminate between those individuals who return to previous activity level from those who do not after ACL injury or reconstruction.2,11 In addition, involved limb deficits can be detected with single-legged hop tests, indicating that those individuals may need more targeted interventions to reduce limb-to-limb differences.36,42 Although these tests have good discriminative ability, no studies have examined the predictive ability of hop tests for knee function after ACL reconstruction. The purpose of this study was to determine if single-legged hop tests could be used to predict medium-term (1-year) self-reported knee function in patients after ACL reconstruction. We hypothesized that single-legged hop tests conducted preoperatively would not and those conducted 6 months after surgery would predict self-reported knee function 1 year after ACL reconstruction. If these simple tests of functional performance can identify those who will have unsuccessful outcome, they can be used to inform clinical decision making and direct interventions to improve knee function.
METHODS
Patients
Between October 2006 and May 2009, 160 patients with a unilateral ACL rupture (mean, 54.6 days from injury; range, 8–279 days from injury) were included in this prospective international cohort study. Eighty patients (50%) were included from site A (Oslo) and 80 patients from site B (Delaware). Patients ranged in age from 15 to 54 years (mean, 26.0) and were regular participants in level I or II activities (≥50 h/y) before ACL rupture.5 Patients were excluded if they had concomitant ligamentous injury, bilateral lower limb involvement, symptomatic meniscal injury, fracture, or full-thickness articular cartilage damage. The ACL rupture was confirmed by magnetic resonance imaging and ≥3-mm side-to-side difference5 with a KT-1000 arthrometer (MedMetrics, San Diego, California).
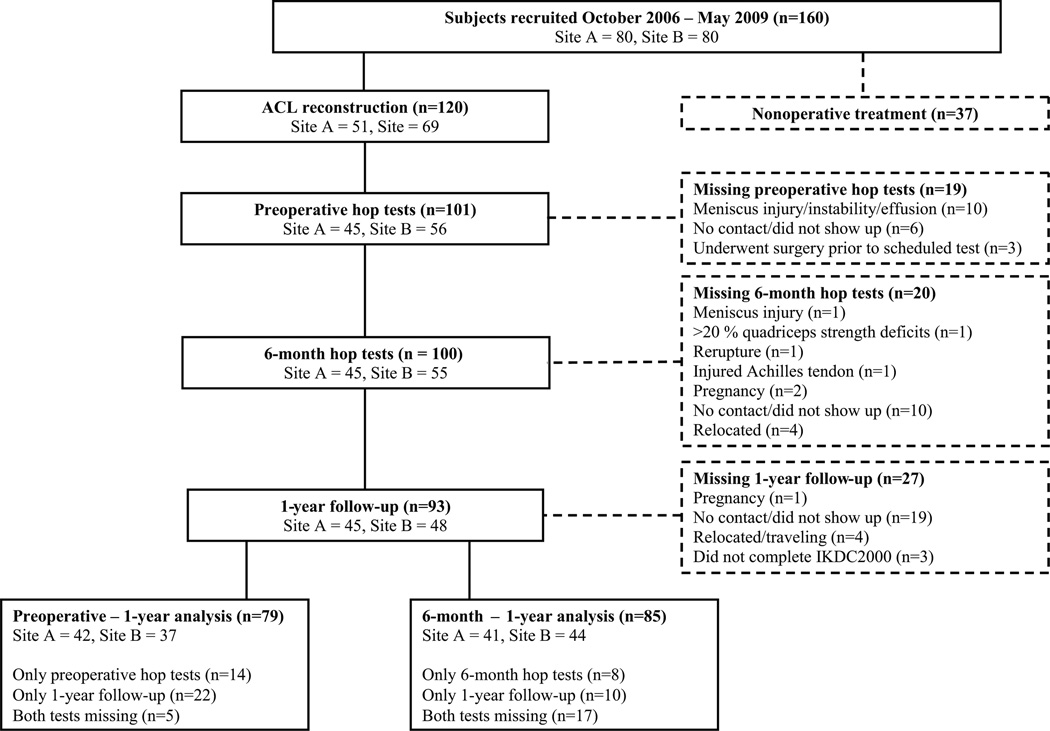
Of the 160 patients included in this study, 37 (23.1%) chose to pursue nonoperative management. Three patients were lost to follow-up, and we were not able to determine if they had undergone ACL reconstruction. One hundred twenty subjects (75.0%) underwent reconstructive surgery and compose the target population in this study. The flow diagram for subject participation in this study is presented in Figure 1. All patients gave informed consent at the time of inclusion. The study was approved by the ethical/human subjects committees at the Regional Ethics Committee for South-Eastern Norway and University of Delaware.
Figure 1.
Flow diagram for subject participation. ACL, anterior cruciate ligament; IKDC, International Knee Documentation Committee.
Testing and Rehabilitation
All patients underwent initial rehabilitation to address acute impairments. Once patients had minimal knee effusion, no limitations in knee range of motion, a quadriceps side-to-side strength deficit less than 30%, and the ability to hop on the involved limb without subsequent pain or effusion, they were enrolled in a 10-session preoperative rehabilitation program.12 Preoperative rehabilitation consisted of a progressive exercise training program emphasizing aggressive quadriceps strengthening and specialized perturbation training to restore muscle strength and appropriate neuromuscular responses. Muscle strength training involved the use of high loads and low repetitions as recommended by the American College of Sports Medicine position stand on progression models in resistance training for healthy adults45 for nonweightbearing (open chain) and weightbearing (closed chain) quadriceps strengthening exercises.10,20 Perturbation training was administered according to the protocol outlined by Fitzgerald et al.12
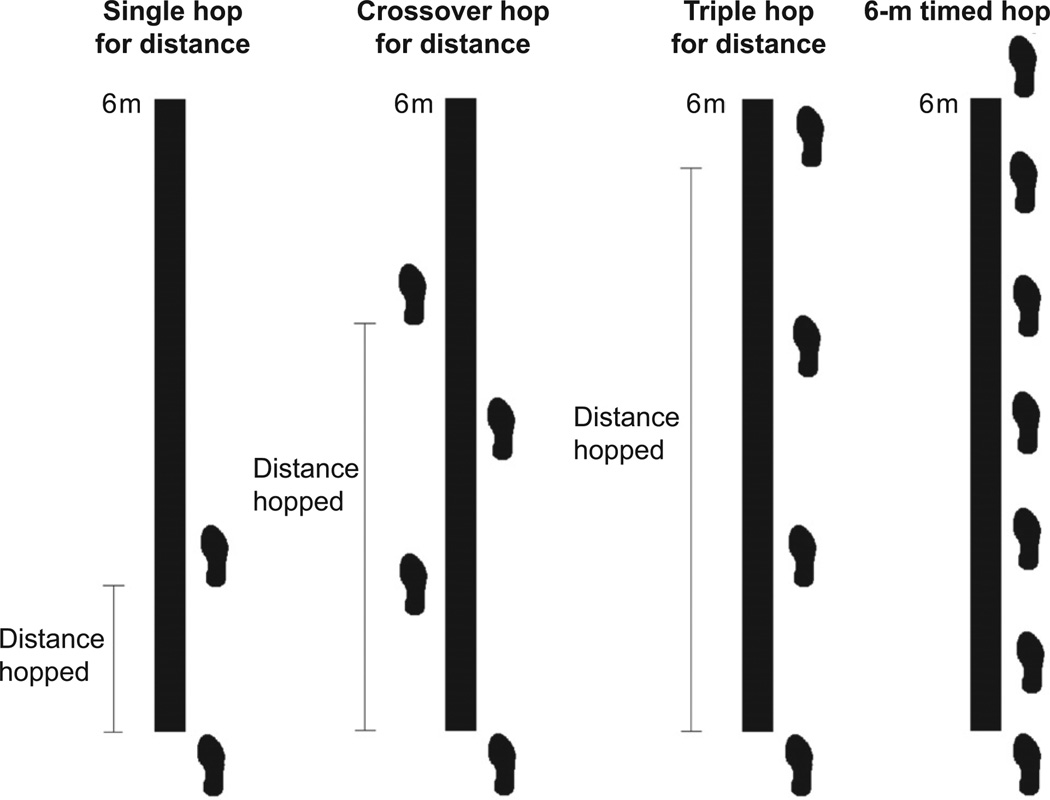
Upon completion of the preoperative rehabilitation phase, patients performed 4 single-legged hop tests: the single hop for distance (single hop), crossover hop for distance (crossover hop), triple hop for distance (triple hop), and 6-meter timed hop (6-m timed hop) (Figure 2).40 These 4 tests have demonstrated good test-retest reliability in normal, young adults49 and in patients after ACL reconstruction.46 The single hop for distance was performed with the patient standing on the leg to be tested, hopping as far as possible, and landing on the same leg. For the crossover hop for distance, patients stood on 1 leg, then hopped as far as possible forward 3 times while alternately crossing over a 15-cm marked strip on the floor. The total distance hopped forward was recorded. The triple hop for distance was performed with the patient standing on 1 leg and performing 3 consecutive hops as far as possible. The single hop, the crossover hop, and the triple hop for distance were considered successful if the landing was stable. To be considered a valid trial, the landing must be on 1 limb, under complete control of the patient. If the patient landed with early touchdown of the contralateral limb, had loss of balance, touched the wall, or had additional hops after landing, the hop was repeated. Patients were instructed to begin with the uninjured leg, with their lead toe behind a marked starting line. The hop distance was measured to the nearest centimeter from the starting line to the patient’s heel with a standard tape measure. For the 6-m timed hop, patients stood on 1 leg, then hopped as fast as possible over a marked distance of 6 meters. The time was recorded with a standard stopwatch. The stopwatch was started when the patient’s heel left the floor and stopped when the patient crossed the finish line. Measurements were recorded to the nearest 100th of a second. All single-legged hop tests were conducted by physical therapists who had undergone detailed training in the test procedures. In accordance with the respective clinic guidelines, no patients wore a knee brace at site A (Oslo), whereas all patients wore a functional knee brace at site B (Delaware). All other test procedures were similar at the 2 sites.
Figure 2.
The 4 single-legged hop tests: single hop for distance, crossover hop for distance, triple hop for distance, and 6-m timed hop. Grindem H, Logerstedt D, Eitzen I, et al. Single-legged hop tests as predictors of self-reported knee function in nonoperatively treated individuals with anterior cruciate ligament injury. Am J Sports Med. 2011;39(11):2347–2354, copyright ©2011 SAGE Publications. Reprinted with permission.
All patients (n = 120) underwent reconstructive surgery with a semitendinosus-gracilis autograft, bone–patellar tendon–bone autograft, or soft tissue allograft. After surgery, the same ACL reconstruction rehabilitation guidelines were followed for all patients.32,47 Patients were systematically progressed through rehabilitation based on the clinical milestones outlined in the guidelines. They underwent the same 4 single-legged hop tests 6 months after surgery and completed the IKDC 200025 one year after surgery. The IKDC 2000 is a joint-specific outcome measure pertinent to a variety of knee conditions for assessing symptoms, function, and sports activity.25 The form contains 18 questions, in which the total scores are expressed as a percentage from 0% to 100%, with higher scores representing better knee function and less symptoms. The IKDC 2000 is a valid and reliable self-reported outcome measure.25
Data Management and Statistics
The single-legged hop scores were calculated as the average of 2 measured trials for each limb. The limb symmetry index (LSI) was expressed as a percentage of the averaged involved limb hop distances divided by the averaged uninvolved limb hop distances for each patient and each hop distance test. For the 6-m timed hop, LSI was expressed as the percentage of the averaged uninvolved limb hop time divided by the averaged involved limb hop time.
Normative data of the IKDC 2000 for men and women with no current or previous knee problems have been previously established.1 We operationally defined self-reported knee function within normal ranges as IKDC 2000 scores greater than or equal to the subject-specific age- and sex-matched population 15th percentile, indicating 85% of the uninjured population would describe their knee within normal ranges. The 15th percentile from the normative data from uninjured individuals was chosen as the cutoff score to ensure that individuals who scored below the cutoff were different from what could be considered a normal variation in IKDC scores.16
The LSI from preoperative and 6-month postoperative single-legged hop tests was used to predict self-reported knee function at 1 year. Comparisons between patients from each site and individuals with knee function within normal ranges and below normal ranges were made using χ2 tests for nominal data and the Mann-Whitney U test for continuous data. Univariate logistic regression was performed to evaluate if hop test LSI preoperatively and 6 months postoperatively predicted knee function within normal ranges 1 year postoperatively. The resulting odds ratios were presented, representing the increase in odds of having self-reported knee function within normal ranges for every 1-point increase in LSI. Interaction was assessed in a logistic regression model that included hop test LSI, site, and a multiplicative interaction term. No interaction of site and hop test LSI preoperatively (all P > .11) and 6 months postoperatively (all P > .13) was found in predicting knee function within normal ranges 1 year postoperatively, and therefore data from both sites were merged for further analysis. The area under the curve (AUC) from receiver operating characteristic (ROC) curves were used to determine the overall discriminative accuracy of each single-legged hop test.18 Optimal cutoff scores for each single-legged hop test were determined by the hop LSI with the highest product of sensitivity and specificity. The corresponding sensitivity, specificity, positive likelihood ratio, and negative likelihood ratio were reported. Sensitivity was reported as the percentage of patients with hop LSI below the cutoff value correctly identified as having knee function below normal ranges and specificity as the percentage of patients with hop LSI above the cutoff value correctly identified as having knee function within normal ranges. A priori a level of 0.05 was set for all analyses. All analyses were conducted in PASW version 18 (SPSS, Inc, an IBM Company, Chicago, Illinois).
RESULTS
Of the 120 patients who underwent ACL reconstruction, 101 (84%) performed preoperative hop testing, 100 (83%) completed 6-month hop testing, and 96 (80%) participated in 1-year on-site testing, but 3 patients did not complete IKDC 2000 (Figure 1). Reasons for patients not completing hop testing were meniscal injury, poor dynamic stability, marked joint effusion, marked quadriceps weakness, soft tissue injury, pregnancy, rupture of the ACL graft, missed appointment, or relocated out of the area (Figure 1). No differences were found in IKDC 2000 scores between those who hopped and those who did not hop preoperatively (P = .357) or 6 months after ACL reconstruction (P = .858). Six months after ACL reconstruction, the mean (SD) IKDC 2000 score was 83.0 (12.9). One year after ACL reconstruction, the mean (SD) IKDC 2000 score was 90.8 (11.1).
Seventy-nine patients completed both preoperative single-legged hop tests and the 1-year follow-up. Sixty-one (77.2%) were classified as having self-reported knee function within normal ranges 1 year after reconstruction, meaning that their IKDC 2000 score was above the age- and sex-specific 15th percentile score of an uninjured population. The remaining 18 (22.8%) were classified as having knee function below normal ranges. There were no significant differences in preoperative hop test LSI between patients with IKDC 2000 scores within and below normal ranges (Table 1). None of the preoperative single-legged hop tests significantly predicted self-reported knee function 1 year after ACL reconstruction (Table 2).
TABLE 1.
Preoperative Single-legged Hop Test Symmetry Indexes in Individuals With Self-reported Knee Function at 1 Yeara
| Preoperative Single-legged Hop Tests |
Below Normal Ranges (n = 18), Median (IQR) |
Within Normal Ranges (n = 61), Median (IQR) |
Above Normal Ranges, AUC (95% CI) |
P Value |
|---|---|---|---|---|
| Single hop for distance LSI | 95.6 (11.7) | 95.1 (13.8) | 0.47 (0.31, 62) | .67 |
| Crossover hop for distance LSI | 95.8 (11.1) | 94.6 (9.4) | 0.42 (0.24, 0.59) | .34 |
| Triple hop for distance LSI | 94.3 (8.0) | 93.6 (11.5) | 0.50 (0.33, 0.66) | .96 |
| 6-m timed hop LSI | 94.7 (7.0) | 97.6 (9.5) | 0.60 (0.46, 0.73) | .22 |
AUC, area under the curve; CI, confidence interval; IQR, interquartile range; LSI, limb symmetry index.
TABLE 2.
Preoperative Univariate Logistic Regression Analysis Results of Predictors of Self-reported Knee Function Within Normal Rangesa
| Preoperative Single-legged Hop Tests | Within Normal Ranges, Odds Ratio (95% CI) | P Value |
|---|---|---|
| Single hop for distance LSI | 1.00 (0.96, 1.04) | .99 |
| Crossover hop for distance LSI | 0.97 (0.90, 1.04) | .35 |
| Triple hop for distance LSI | 1.00 (0.94, 1.07) | .91 |
| 6-m timed hop LSI | 1.03 (0.96, 1.09) | .44 |
CI, confidence interval; LSI, limb symmetry index.
Eighty-five (70.8%) patients completed both single-legged hop tests 6 months after surgery and the 1-year follow-up. Sixty-eight (80.0%) were classified as having self-reported knee function within normal ranges 1 year after reconstruction. No significant differences were seen in sex, preinjury activity level, or median age between patients with knee function within and below normal ranges (Table 3).
TABLE 3.
Patient Demographics in Individuals With Self-reported Knee Function Within and Below Normal Rangesa
| Below Normal Ranges at 12 mo (n = 17) | Within Normal Ranges at 12 mo (n = 68) | P Value | |
|---|---|---|---|
| Women/men (% women) | 8/9 (47.1) | 30/38 (44.1) | .83 |
| Preinjury activity level I/II (% AL I) | 12/5 (70.6) | 57/11 (83.8) | .21 |
| Age, median (IQR) | 24.0 (18.0, 28.4) | 23.3 (17.9, 31.8) | .97 |
AL, activity level; IQR, interquartile range.
Patients who were classified as having self-reported knee function within normal ranges at the 1-year follow-up had significantly higher crossover hop and 6-m timed hop symmetry indexes 6 months after surgery (Table 4). The single hop, crossover hop, triple hop, and the 6-m timed hop 6 months after ACL reconstruction significantly predicted self-reported knee function 1 year after ACL reconstruction (Table 5). Of the 4 single-legged hop tests, the 6-m timed hop and the crossover hop were the strongest individual predictors of self-reported knee function (odds ratio [OR] = 1.10 for 6-m timed hop and 1.09 for crossover hop) and had the highest discriminative accuracy (AUC = 0.68 for 6-m timed hop and crossover hop). The discriminative accuracy (AUC), optimum cutoff scores, and corresponding sensitivity and specificity for the 4 individual single-legged hop tests are shown in Tables 4 and 6. The optimal cutoff for the 6-m timed hop was 87.7% LSI with a sensitivity of 53%, specificity of 90%, and positive likelihood ratio of 5.14. The optimal cutoff for the crossover hop was 94.9% LSI with a sensitivity of 88%, specificity of 47%, and negative likelihood ratio of 0.25.
TABLE 4.
Six-Month Single-legged Hop Test Symmetry Indexes in Individuals With Self-reported Knee Function at 12 Monthsa
| Six-Month Single-legged Hop Tests |
Below Normal Ranges (n = 17), Median (IQR) |
Within Normal Ranges (n = 68), Median (IQR) |
Within Normal Ranges, AUC (95% CI) |
P Value |
|---|---|---|---|---|
| Single hop for distance LSI | 88.6 (25.7) | 93.3 (13.5) | 0.64 (0.49, 0.79) | .08 |
| Crossover hop for distance LSI | 91.7 (19.6) | 92.9 (10.7) | 0.68 (0.53, 0.83) | .02 |
| Triple hop for distance LSI | 91.8 (17.3) | 93.1 (9.9) | 0.64 (0.48, 0.79) | .08 |
| 6-m timed hop LSI | 87.7 (18.2) | 96.1 (9.9) | 0.68 (0.53, 0.84) | .02 |
AUC, area under the curve; CI, confidence interval; IQR, interquartile range; LSI, limb symmetry index.
TABLE 5.
Six-Month Univariate Logistic Regression Analysis Results of Predictors of Self-reported Knee Function Within Normal Rangesa
| Six-Month Single-legged Hop Tests | Within Normal Ranges, Odds Ratio (95% CI) | P Value |
|---|---|---|
| Single hop for distance LSI | 1.05 (1.01, 1.09) | .02 |
| Crossover hop for distance LSI | 1.09 (1.03, 1.16) | .005 |
| Triple hop for distance LSI | 1.06 (1.01, 1.12) | .02 |
| 6-m timed hop LSI | 1.10 (1.03, 1.17) | .006 |
CI, confidence interval; LSI, limb symmetry index.
TABLE 6.
Overall Optimum Cutoff Scores, Sensitivity and Specificity, and Likelihood Ratios for Single-legged Hop Testsa
| Six-Month Single-legged Hop Tests |
Optimum Cutoff Scores, % |
Sensitivity (95% CI) |
Specificity (95% CI) |
Positive Likelihood Ratio (95% CI) |
Negative Likelihood Ratio (95% CI) |
|---|---|---|---|---|---|
| Single hop for distance LSI | 89.3 | 0.53 (0.31, 0.74) | 0.72 (0.60, 0.81) | 1.90 (1.05, 3.42) | 0.65 (0.39, 1.10) |
| Crossover hop for distance LSI | 94.9 | 0.88 (0.66, 0.97) | 0.47 (0.36, 0.59) | 1.67 (1.26, 2.21) | 0.25 (0.10, 0.50) |
| Triple hop for distance LSI | 95.2 | 0.77 (0.53, 0.90) | 0.46 (0.34, 0.57) | 1.41 (0.10, 1.98) | 0.52 (0.21, 1.26) |
| 6-m timed hop LSI | 87.7 | 0.53 (0.26, 0.69) | 0.90 (0.80, 0.95) | 5.14 (2.24, 11.82) | 0.53 (0.32, 0.87) |
CI, confidence interval; LSI, limb symmetry index.
DISCUSSION
The purpose of this investigation was to determine if preoperative and postoperative single-legged hop tests predict self-reported knee function 1 year after ACL reconstruction. Preoperative hop tests did not significantly predict self-reported knee function 1 year after ACL reconstruction. However, hop tests conducted 6 months postoperatively statistically significantly predicted self-reported knee function (P < .02). Of the 4 hop tests, the 6-m timed hop and the crossover hop were the best predictors and the only 2 tests in which the confidence intervals of the discriminatory accuracy (AUC) were above 0.5. With a specificity of 90% (Table 6), the 6-m timed hop test was the most useful test for identifying patients with self-reported knee function below normal ranges at 1 year. The crossover hop test had a sensitivity of 88% (Table 6) and was thus the test that most accurately identified patients with knee function within normal ranges. These results have significant implications for the clinical management of patients after ACL reconstruction as the ease of application of these hop tests allows for a practical method to determine the need for directed interventions to restore medium-term knee function.
In the current study, the 6-m timed hop was the strongest independent predictor and had the highest discriminatory accuracy. Patients with knee function below normal ranges were more than 5 times more likely to have 6-m timed hop LSI lower than 88% at 6 months than those with knee function within normal ranges. Previous work by Fitzgerald et al11 has shown that the 6-m timed hop along with other variables can identify those with poor dynamic knee stability from those with good knee stability early after ACL injury. In those individuals with good dynamic knee stability, this test can also discriminate between those who did not successfully return to high-level sports from those who did.11 The 6-m timed hop, the least demanding hop,23,46 can effectively challenge neuromuscular control in patients who have deficits in limb-to-limb differences. These asymmetries strongly predict those who will have knee function below normal ranges at 1 year. Limb asymmetries may be the result of underlying impairments, such as quadriceps weakness,26,53 that may contribute to low hop performance and should be identified and corrected. In addition, limb asymmetries in athletes may result in suboptimal performance on the playing field and are linked with an increased risk of a second ACL injury.22,38,43 Sports-specific activities are more challenging than landing from a planned hop in a controlled environment, and thus the deficits seen in single-legged hop performance may be magnified in sports-specific activities, potentially predisposing the ipsilateral or contralateral knee to injury. Our data suggest that patients demonstrating an LSI less than 88% on a 6-m timed hop test may benefit from continued rehabilitation to address impairments and functional performance in an attempt to normalize function.35,42 Restoration of symmetrical function between limbs remains an important goal of postoperative rehabilitation, and limb asymmetry for all patients remains a risk for poor knee function.
The crossover hop predicted knee function within normal ranges, with similar predictive ability and discriminatory accuracy as the 6-m timed hop. Patients with knee function within normal ranges were 4 times more likely to have crossover hop LSI greater than 95% than those with knee function below normal ranges. The crossover hop is the most demanding hop test as it imposes forces in frontal and transverse planes, combined with multiple hops in the sagittal plane. Side-to-side differences are minimized in these patients, likely indicating superior neuromuscular control, therefore increasing the probability of knee function within normal ranges at 1 year. These patients appear to have improved their ability to generate and attenuate forces on the involved limb.35,37 Furthermore, patients with high limb symmetry after ACL reconstruction favor the involved limb less during functional activities, are more confident in its function, move more symmetrically, and are more likely to attempt full competition sports.3,31 Patients with minimal side-to-side differences on the crossover hop test at 6 months possibly will have good knee function at 1 year if they continue with their current training regimen.
The timing of hop testing affects prediction models. Conducting hop tests 6 months after ACL reconstruction is appropriate for predictive purposes. The ability to predict knee function is better after a period of rehabilitation than acutely after injury or surgery.9,19 Six months after surgery is a typical time point in which patients begin to transition to sports or preinjury activities,30 so administering hop testing at this time point provides clinicians valuable information relevant to patients’ current function, their progress during rehabilitation and the necessity for additional rehabilitation, and their readiness to return to sporting activities.
Self-reported measures are frequently used as an outcome variable for knee function.8,29,51 Patient demographics, health behaviors, concomitant injuries, meniscal surgery, and knee extension range-of-motion loss have been identified as predictors of self-reported knee function.21,29,44 Lower knee function based on self-report outcomes after ACL reconstruction has been associated with lower patient satisfaction and fear of reinjury.28,31 Impaired medium-term self-reported knee function was predictive of symptomatic radiographic knee osteoarthritis 10 to 15 years after reconstruction.41 Being able to ascertain after ACL surgery those patients who will more likely have knee function below normal ranges highlights the importance of identifying modifiable predictive factors, such as the 6-m timed hop LSI, that can be readily administered by clinicians to develop targeted interventions to potentially improve knee function, increase patient satisfaction, and reduce the risk of symptomatic arthritis.
Preoperative hop testing was not predictive of postoperative knee function. Eitzen et al8 found that neither the preoperative triple nor the stair hop test was predictive of knee function 2 years after reconstruction. The LSI after preoperative rehabilitation does not delineate between those who will have IKDC 2000 scores within normal ranges compared with those with scores below normal ranges 1 year after surgery. The median LSI for all hop tests preoperatively was greater than 93% after preoperative neuromuscular rehabilitation, indicating as a group, patients were able to achieve adequate limb symmetry in all 4 hops. Although prediction is better after rehabilitation than before rehabilitation, the ACL reconstruction is a “game-changer,” and the passive stability it provides likely makes the preoperative functional hop performance irrelevant to outcome after ACL reconstruction.34,48 Although preoperative impairments, such as quadriceps weakness and knee extension range of motion, can influence knee function after reconstruction,8,50 preoperative hop performance does not predict postoperative knee function.
Furthermore, in patients who are treated nonoperatively, hop tests provide a different assessment. Fitzgerald et al11 found that the 6-m timed hop test along with other measures can predict return to previous activity level in the short term. In a prospective cohort study in nonoperatively treated individuals with ACL injury, Grindem et al,16 using a similar design and methodology of the current study, reported that only the single-hop test significantly predicted self-reported knee after 1 year. Therefore, the effect of a stabilization procedure such as ACL reconstruction may affect which hop tests predict knee function.
Limitations
Many factors may contribute to the failure to achieve self-reported knee function within normal ranges. Our group was young and active and may only be generalizable to this physically active age population. This study had some incomplete data. Some patients did not meet the minimal criteria for allowing hop testing (weakness, effusion, recurrent instability) at each time period. The results can only be generalized to those with isolated ACL injuries or asymptomatic concomitant injuries and cannot be generalized to individuals with symptomatic concomitant injuries. The hop test battery was administered in the same fashion each session11,40 and may not be generalized to different hop test paradigms. A portion of patients did not complete either 6-month or 1-year testing, reducing the participants available for analysis.
CONCLUSION
Preoperative hop tests are not predictive of knee function after ACL reconstruction. Hop tests are clinically useful in predicting future outcomes16 as individual hop tests 6 months after ACL reconstruction can predict who will have knee function within or below normal ranges in the medium term (1 year after ACL reconstruction). These tests have considerable implications on clinical decision making on future knee function as they can be used to inform the clinician and patient about the patient’s likely prognosis and the development of directed rehabilitation to address hop limb asymmetries to promote normal knee function.
ACKNOWLEDGMENT
We acknowledge the Musculoskeletal and Sport Medicine Clinic, Hjelp24 NIMI (www.hjelp24.no), for supporting the Norwegian Research Center for Active Rehabilitation (NAR) (www.active-rehab.no) with rehabilitation facilities and research staff. We thank physical therapists Håvard Moksnes, Annika Storevold, Ida Svege, Espen Selboskar, Karin Rydevik, and Marte Lund for their assistance with data collection, the University of Delaware Physical Therapy Clinic (www.udel.edu/pt) with their assistance in the data collection of this study, and Martha Callahan for data organization
One or more authors have declared the following potential conflict of interest or source of funding: This work was supported by National Institutes of Health (NIH R01 HD37985) and a Promotional of Doctoral Studies scholarship from the Foundation for Physical Therapy. Dr Axe is a consultant to Smith & Nephew.
Footnotes
Investigation performed at University of Delaware Physical Therapy Clinic, Newark, Delaware, and Hjelp24 Norwegian Sports Medicine Clinic (Hjelp24 NIMI), Ullevaal, Oslo, Norway
Presented at the annual meeting of the AOSSM, Baltimore, Maryland, July 2012.
REFERENCES
- 1.Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34(1):128–135. doi: 10.1177/0363546505280214. [DOI] [PubMed] [Google Scholar]
- 2.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- 3.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011;39(3):538–543. doi: 10.1177/0363546510384798. [DOI] [PubMed] [Google Scholar]
- 4.Biau DJ, Tournoux C, Katsahian S, Schranz P, Nizard R. ACL reconstruction: a meta-analysis of functional scores. Clin Orthop Relat Res. 2007;458:180–187. doi: 10.1097/BLO.0b013e31803dcd6b. [DOI] [PubMed] [Google Scholar]
- 5.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med. 1994;22(5):632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 6.Dunn WR, Spindler KP. Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38(10):2040–2050. doi: 10.1177/0363546510370280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dye SF, Wojtys EM, Fu FH, Fithian DC, Gillquist I. Factors contributing to function of the knee joint after injury or reconstruction of the anterior cruciate ligament. Instr Course Lect. 1999;48:185–198. [PubMed] [Google Scholar]
- 8.Eitzen I, Holm I, Risberg MA. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med. 2009;43(5):371–376. doi: 10.1136/bjsm.2008.057059. [DOI] [PubMed] [Google Scholar]
- 9.Eitzen I, Moksnes H, Snyder-Mackler L, Engebretsen L, Risberg MA. Functional tests should be accentuated more in the decision for ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1517–1525. doi: 10.1007/s00167-010-1113-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA. A progressive 5-week exercise therapy program leads to significant improvement in knee function early after anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2010;40(11):705–721. doi: 10.2519/jospt.2010.3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fitzgerald GK, Axe MJ, Snyder-Mackler L. A decision-making scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2000;8(2):76–82. doi: 10.1007/s001670050190. [DOI] [PubMed] [Google Scholar]
- 12.Fitzgerald GK, Axe MJ, Snyder-Mackler L. The efficacy of perturbation training in nonoperative anterior cruciate ligament rehabilitation programs for physical active individuals. Phys Ther. 2000;80(2):128–140. [PubMed] [Google Scholar]
- 13.Fitzgerald GK, Lephart SM, Hwang JH, Wainner RS. Hop tests as predictors of dynamic knee stability. J Orthop Sports Phys Ther. 2001;31(10):588–597. doi: 10.2519/jospt.2001.31.10.588. [DOI] [PubMed] [Google Scholar]
- 14.Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc. 2006;14(10):1021–1028. doi: 10.1007/s00167-006-0050-9. [DOI] [PubMed] [Google Scholar]
- 15.Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8(3):141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Grindem H, Logerstedt D, Eitzen I, et al. Single-legged hop tests as predictors of self-reported knee function in nonoperatively treated individuals with anterior cruciate ligament injury. Am J Sports Med. 2011;39(11):2347–2354. doi: 10.1177/0363546511417085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hambly K, Griva K. IKDC or KOOS: which one captures symptoms and disabilities most important to patients who have undergone initial anterior cruciate ligament reconstruction? Am J Sports Med. 2010;38(7):1395–1404. doi: 10.1177/0363546509359678. [DOI] [PubMed] [Google Scholar]
- 18.Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- 19.Hartigan E, Axe MJ, Snyder-Mackler L. Perturbation training before ACL reconstruction improves gait asymmetries in non-copers. J Orthop Res. 2009;27(6):724–729. doi: 10.1002/jor.20754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2010;40(3):141–154. doi: 10.2519/jospt.2010.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heijne A, Ang BO, Werner S. Predictive factors for 12-month outcome after anterior cruciate ligament reconstruction. Scand J Med Sci Sports. 2009;19(6):842–849. doi: 10.1111/j.1600-0838.2008.00852.x. [DOI] [PubMed] [Google Scholar]
- 22.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 23.Hopper DM, Strauss GR, Boyle JJ, Bell J. Functional recovery after anterior cruciate ligament reconstruction: a longitudinal perspective. Arch Phys Med Rehabil. 2008;89(8):1535–1541. doi: 10.1016/j.apmr.2007.11.057. [DOI] [PubMed] [Google Scholar]
- 24.Hughes G, Watkins J. A risk-factor model for anterior cruciate ligament injury. Sports Med. 2006;36(5):411–428. doi: 10.2165/00007256-200636050-00004. [DOI] [PubMed] [Google Scholar]
- 25.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 26.Keays SL, Bullock-Saxton J, Keays AC, Newcombe P. Muscle strength and function before and after anterior cruciate ligament reconstruction using semitendonosus and gracilis. Knee. 2001;8(3):229–234. doi: 10.1016/s0968-0160(01)00099-0. [DOI] [PubMed] [Google Scholar]
- 27.Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011;93(11):994–1000. doi: 10.2106/JBJS.I.01618. [DOI] [PubMed] [Google Scholar]
- 28.Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, Hawkins RJ. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2002;84(9):1560–1572. doi: 10.2106/00004623-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Kowalchuk DA, Harner CD, Fu FH, Irrgang JJ. Prediction of patient-reported outcome after single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2009;25(5):457–463. doi: 10.1016/j.arthro.2009.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kvist J. Rehabilitation following anterior cruciate ligament injury: current recommendations for sports participation. Sports Med. 2004;34(4):269–280. doi: 10.2165/00007256-200434040-00006. [DOI] [PubMed] [Google Scholar]
- 31.Kvist J, Ek A, Sporrstedt K, Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2005;13(5):393–397. doi: 10.1007/s00167-004-0591-8. [DOI] [PubMed] [Google Scholar]
- 32.Manal T, Snyder-Mackler L. Practice guidelines for anterior cruciate ligament rehabilitation: a criterion-based rehabilitation progression. Oper Tech Orthop. 1996;6(3):190–196. [Google Scholar]
- 33.Marx RG, Jones EC, Angel M, Wickiewicz TL, Warren RF. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19(7):762–770. doi: 10.1016/s0749-8063(03)00398-0. [DOI] [PubMed] [Google Scholar]
- 34.Moksnes H, Risberg MA. Performance-based functional evaluation of non-operative and operative treatment after anterior cruciate ligament injury. Scand J Med Sci Sports. 2008;19(3):345–355. doi: 10.1111/j.1600-0838.2008.00816.x. [DOI] [PubMed] [Google Scholar]
- 35.Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric vs. dynamic stabilization and balance training on power, balance, and landing force in female athletes. J Strength Cond Res. 2006;20(2):345–353. doi: 10.1519/R-17955.1. [DOI] [PubMed] [Google Scholar]
- 36.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Biomechanics laboratory-based prediction algorithm to identify female athletes with high knee loads that increase risk of ACL injury. Br J Sports Med. 2010;45(4):245–252. doi: 10.1136/bjsm.2009.069351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19(1):51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 38.Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36(6):385–402. doi: 10.2519/jospt.2006.2222. [DOI] [PubMed] [Google Scholar]
- 39.Myklebust G, Bahr R. Return to play guidelines after anterior cruciate ligament surgery. Br J Sports Med. 2005;39(3):127–131. doi: 10.1136/bjsm.2004.010900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19(5):513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 41.Oiestad BE, Holm I, Gunderson R, Myklebust G, Risberg MA. Quadriceps muscle weakness after anterior cruciate ligament reconstruction: a risk factor for knee osteoarthritis? Arthritis Care Res (Hoboken) 2010;62(12):1706–1714. doi: 10.1002/acr.20299. [DOI] [PubMed] [Google Scholar]
- 42.Paterno MV, Myer GD, Ford KR, Hewett TE. Neuromuscular training improves single-limb stability in young female athletes. J Orthop Sports Phys Ther. 2004;34(6):305–316. doi: 10.2519/jospt.2004.34.6.305. [DOI] [PubMed] [Google Scholar]
- 43.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35(4):564–574. doi: 10.1177/0363546506296042. [DOI] [PubMed] [Google Scholar]
- 45.Ratamess NA, Alvar BA, Evetoch TK, et al. American College of Sports Medicine position stand: progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009;41(3):687–708. doi: 10.1249/MSS.0b013e3181915670. [DOI] [PubMed] [Google Scholar]
- 46.Reid A, Birmingham TB, Stratford PW, Alcock GK, Giffin JR. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther. 2007;87(3):337–349. doi: 10.2522/ptj.20060143. [DOI] [PubMed] [Google Scholar]
- 47.Risberg MA, Holm I, Myklebust G, Engebretsen L. Neuromuscular training versus strength training during first 6 months after anterior cruciate ligament reconstruction: a randomized clinical trial. Phys Ther. 2007;87(6):737–750. doi: 10.2522/ptj.20060041. [DOI] [PubMed] [Google Scholar]
- 48.Risberg MA, Holm I, Tjomsland O, Ljunggren E, Ekeland A. Prospective study of changes in impairments and disabilities after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29(7):400–412. doi: 10.2519/jospt.1999.29.7.400. [DOI] [PubMed] [Google Scholar]
- 49.Ross MD, Langford B, Whelan PJ. Test-retest reliability of 4 single-leg horizontal hop tests. J Strength Cond Res. 2002;16(4):617–622. [PubMed] [Google Scholar]
- 50.Shelbourne KD, Gray T. Minimum 10-year results after anterior cruciate ligament reconstruction: how the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am J Sports Med. 2009;37(3):471–480. doi: 10.1177/0363546508326709. [DOI] [PubMed] [Google Scholar]
- 51.Spindler KP, Huston LJ, Wright RW, et al. The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction: a population cohort study. Am J Sports Med. 2011;39(2):348–359. doi: 10.1177/0363546510383481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9(1):9–15. doi: 10.1016/j.ptsp.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 53.Wilk KE, Romaniello WT, Soscia SM, Arrigo CA, Andrews JR. The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee. J Orthop Sports Phys Ther. 1994;20(2):60–73. doi: 10.2519/jospt.1994.20.2.60. [DOI] [PubMed] [Google Scholar]