Abstract
The objectives of this study were to describe contemporary post-discharge death rates of patients hospitalized at all Worcester (MA) hospitals after an initial acute myocardial infarction (AMI) and to examine factors associated with a poor prognosis. We reviewed the medical records of patients discharged from 11 central Massachusetts medical centers after an initial AMI during 2001, 2003, 2005, and 2007, identifying 2,452 patients. This population was comprised of predominantly older individuals, men (58%), and whites. Overall, the 3 month, 1 year, and 2 year all-cause death rates were 8.9%, 16.4%, and 23.4%, respectively. Over time, reductions in post-discharge mortality were observed in crude as well as multivariable adjusted analyses. In 2001, the 3 month, 1 year, and 2 year all-cause death rates were 11.1%, 17.1%, and 25.6%, respectively, compared with rates of 7.9%, 12.7%, and 18.6% among patients discharged in 2007. Older age, male sex, hospitalization for an NSTEMI, renal dysfunction, and pre-existing heart failure were associated with an increased risk of dying after hospital discharge. Our results suggest that the post-discharge prognosis of patients with an initial AMI has improved, likely reflecting both enhanced inhospital and post-discharge management practices. In conclusion, patients with an initial AMI can also be identified who are at increased risk for dying after hospital discharge in whom increased surveillance and targeted treatment approaches can be directed.
Keywords: initial AMI, prognosis, changing trends
Introduction
Using data from the Worcester Heart Attack Study [1–3], we describe trends in post-discharge total mortality among residents of the Worcester (MA) metropolitan area who survived hospitalization for an initial AMI during recent years and factors associated with a poor long-term prognosis.
Methods
The Worcester Heart Attack Study is an ongoing clinical/epidemiologic investigation that is examining long-term trends in the incidence, hospital, and post-discharge case-fatality rates of AMI among residents of the Worcester metropolitan area hospitalized at all greater Worcester medical centers in 16 biennial periods between 1975 and 2007 [1–3]. Residents of the Worcester metropolitan area hospitalized with a principal or secondary discharge diagnosis of AMI (ICD-9 code 410) were included in our study. In addition, a random sample of records from related diagnostic rubrics in which the diagnosis of AMI might have occurred (e.g., ICD-9 Codes 411-414) was carried out to identify potentially misclassified cases of AMI [1–3]. This study was approved by the Institutional Review Board at the University of Massachusetts Medical School.
The present study sample consisted of patients hospitalized at all 11 greater Worcester medical centers during the most recent years under study (2001, 2003, 2005, 2007) to provide more contemporary insights into possible changing trends in the long-term prognosis of patients with a first AMI.
Cases of AMI were defined as having at least 2 out of 3 clinical, serum biomarker, or electrocardiographic criteria present [1–3]. Standardized definitions for the classification of type of AMI (ST-segment AMI (STEMI) and non-ST-segment AMI (NSTEMI) were utilized [4,5]. Cases of perioperative or trauma-associated AMI were excluded as were patients with a prior diagnosis of AMI, based on the review of information contained in hospital medical records or with ECG changes indicative of prior myocardial necrosis. The clinical complications of AMI that may have developed during hospitalization were assessed on the basis of information available from medical records and use of standardized diagnostic criteria [3,6–9].
The approaches used to ascertain survival status after hospital discharge included a review of medical records for additional hospitalizations and a statewide search of death certificates. Our principal study endpoint was all-cause mortality. For patients discharged from all central Massachusetts hospitals, follow-up was continued through 2009.
Differences in the distribution of demographic and clinical characteristics between respective comparison groups were examined by using chi square tests for discrete variables and t tests for continuous variables. A life-table approach was used to examine the overall long-term death rates, and trends in long-term prognosis, after hospital discharge. A logistic multiple regression approach was used to identify factors associated with post-discharge mortality at 3 and 24 months after hospital discharge. These times points were chosen because several prior investigations have shown these follow-up points to be high-risk periods for patients discharged from the hospital after an AMI [10,11]. In our regression models we did not control for the use of different cardiac treatment approaches because we could not account for confounding by treatment indication given the nonrandomized nature of this study.
Results
The study population consisted of 2,452 residents of the Worcester metropolitan area who were discharged from all central Massachusetts hospitals after an incident AMI between 2001 and 2007 and in whom further follow-up information was obtained. Of these, 715 patients were discharged in 2001, 684 in 2003, 532 in 2005, and 521 patients were discharged in 2007.
Overall, the population was predominately Caucasian with an average age of 69 years, 42% were women, and most were diagnosed with NSTEMI (Table 1). The two most common cardiovascular co-morbidities in these patients were hypertension and diabetes. Hospital length of stay averaged 5.6 days and a considerable proportion of patients developed heart failure or atrial fibrillation while hospitalized. In comparing the characteristics of patients hospitalized in 2001 and 2007, there was a decrease in the average age at the time of the patient’s index hospitalization, length of stay, and slightly lower levels of serum glucose, total cholesterol, and LDL-cholesterol (Table 1).
Table 1.
Demographic and Clinical Characteristics of the Study Population, Overall and by Time Period of Hospitalization
| Characteristic | Overall population (n=2,452) | 2001 Cohort (n=715) | 2007 Cohort (n=521) |
|---|---|---|---|
| Age (Years) | |||
| Mean | 68.7 | 69.2 | 66.3 |
| <65 | 933 (38.1%) | 256 (35.8%) | 216 (41.5%) |
| 65–74 | 484 (19.8%) | 162 (22.7%) | 80 (15.4%) |
| 75–84 | 636 (26.0%) | 200 (28.0%) | 141 (27.2%) |
| ≥85 | 397 (16.2%) | 97 (13.6%) | 82 (15.8%) |
| Male | 1414 (57.7%) | 425 (59.4%) | 316 (60.7%) |
| White | 2180 (88.9%) | 646 (90.4%) | 465 (89.3%) |
| Pre-hospital delay (mean, hours) | 3.9 | 3.4 | 3.5 |
| Length of stay (mean, days) | 5.6 | 6.6 | 4.8 |
| STEMI | 913 (37.2%) | 284 (39.7%) | 179 (34.4%) |
| Angina pectoris | 336 (13.7%) | 130 (18.2%) | 39 (7.5%) |
| Hypertension | 1638 (66.8%) | 450 (62.9%) | 357 (68.5%) |
| Atrial fibrilation | 270 (11.0%) | 79 (11.1%) | 60 (11.5%) |
| Diabetes mellitus | 674 (27.5%) | 206 (28.8%) | 146 (28.0%) |
| Heart failure | 356 (14.5%) | 107 (15.0%) | 63 (12.1%) |
| Stroke | 207 (8.4%) | 65 (9.1%) | 45 (8.6%) |
| Kidney disease | 329 (13.4%) | 78 (10.9%) | 90 (17.3%) |
| Physiologic variables (mean) | |||
| Ejection fraction (%) | 49 | 48 | 50 |
| eGlomerular filtration rate (mL/min/1.73m2) | 63 | 62 | 66 |
| Diastolic blood pressure (mm Hg) | 79 | 80 | 79 |
| Systolic blood pressure (mm Hg) | 144 | 146 | 142 |
| Glucose (mg/dL) | 169 | 178 | 159 |
| Total cholesterol (mg/dL) | 180 | 186 | 173 |
| Hospital complications | |||
| Atrial fibrillation | 477 (19.5%) | 134 (18.7%) | 90 (17.3%) |
| Heart failure | 780 (31.8%) | 228 (31.9%) | 170 (32.6%) |
| Cardiogenic shock | 87 (3.6%) | 32 (4.5%) | 24 (4.6%) |
| Stroke | 21 (0.9%) | 6 (0.8%) | 2 (0.4%) |
The overall post-discharge death rates at 3 months, 1 year, and 2 years were 8.9%, 16.4%, and 23.4%, respectively (Figure 1). We observed a decrease in the death rates at each of these time points among patients discharged in the most recent study year compared with those discharged during earlier study years. The 3 month death rate declined from 11.1% in 2001 to 7.9% in 2007, the 1 year death rate declined from 17.1% to 12.7%, and the 2 year death rate declined from 25.6% to 18.6% (Figure 1). After we adjusted for several baseline demographic, medical history, and clinical characteristics, patients discharged from the hospital in 2007 were more likely to have survived to 3 months (OR = 0.53; 95% CI 0.43, 0.98), 1 year (OR = 0.74; 95% CI 0.48,1.14), and 2 years (OR = 0.95; 95% CI 0.61,1.49) compared with those discharged in 2001.
Figure 1.
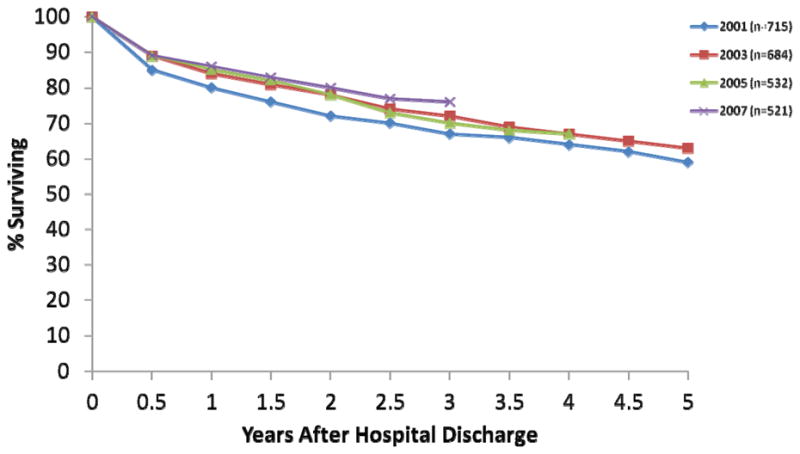
Post-Hospital Discharge Survival for Patients With an Initial Acute Myocardial Infarction
We examined factors associated with an increased risk of dying at 3 months using a logistic regression model (Table 2). Being older, male, having an NSTEMI, and having a prior history of stroke, heart failure, and kidney disease were important predictors of three month death rates. Development of atrial fibrillation, heart failure, cardiogenic shock, or a stroke during hospitalization were associated with a significantly poorer prognosis at 3 months; a low systolic blood pressure at the time of hospital presentation was also an important predictor of dying during the first 3 months of hospital discharge.
Table 2.
Odds of Dying at 3 and 24 Months With an Initial Acute Myocardial Infarction (AMI) According to Selected Factors
| Characteristic | 0–3 months
|
3–24 months
|
||
|---|---|---|---|---|
| OR* | 95% CI | OR | 95% CI | |
| Age (years) | ||||
| 55–64 | 0.92 | 0.31,2.68 | 1.71 | 0.82,3.57 |
| 65–74 | 3.51 | 1.46,3.48 | 4.96 | 2.55,9.68 |
| ≥75 | 7.88 | 3.39,18.35 | 7.77 | 4.04,14.94 |
| Male | 1.40 | 1.02,1.93 | 1.34 | 1.02,1.76 |
| White race | 1.25 | 0.70,2.21 | 1.18 | 0.76,1.83 |
| Length of stay | 1.03 | 1.00,1.05 | 1.02 | 0.99,1.04 |
| STEMI | 0.81 | 0.56,1.18 | 0.53 | 0.38,0.73 |
| Co-morbidities | ||||
| Hypertension | 0.72 | 0.50,1.04 | 0.92 | 0.67,1.28 |
| Atrial fibrillation | 1.31 | 0.86,2.02 | 0.60 | 0.41,0.87 |
| Stroke | 1.83 | 1.20,2.78 | 1.61 | 1.08,2.40 |
| Heart failure | 1.88 | 1.29,2.74 | 2.22 | 1.58,3.11 |
| Diabetes | 1.33 | 0.92,1.93 | 1.04 | 0.75,1.43 |
| Kidney disease | 1.65 | 1.11,2.45 | 1.31 | 0.90,1.91 |
| In-hospital complications | ||||
| Atrial | 1.56 | 1.10,2.21 | 0.66 | 0.47,0.93 |
| fibrillation | ||||
| Heart failure | 1.60 | 1.13,2.25 | 1.60 | 1.19,2.13 |
| Cardiogenic | 1.86 | 0.95,3.67 | 2.42 | 1.25,4.69 |
| shock | ||||
| Stroke | 3.30 | 1.13,9.64 | 1.83 | 0.56,6.02 |
| Hemorrhage | 1.37 | 0.96,1.94 | 1.19 | 0.88,1.61 |
| Physiologic variables | ||||
| Systolic BP (mm Hg) | ||||
| <100 | 1.76 | 1.03,3.03 | 1.16 | 0.67,2.04 |
| 120–139 | 0.79 | 0.50,1.27 | 0.84 | 0.56,1.27 |
| 140–159 | 0.67 | 0.42,1.08 | 0.59 | 0.39,0.88 |
| ≥160 | 0.60 | 0.38,0.96 | 0.74 | 0.50,1.08 |
| Glomerular filtration rate (mL/min) | ||||
| <30 | 1.65 | 0.97,2.79 | 4.14 | 2.59,6.64 |
| 30–59 | 1.19 | 0.82,1.73 | 1.41 | 1.04,1.91 |
| Glucose (mg/dL) | ||||
| <80 | 1.07 | 0.33,3.47 | 1.34 | 0.42,4.29 |
| 110–140 | 1.09 | 0.66,1.80 | 0.82 | 0.54,1.24 |
| 140–180 | 1.03 | 0.61,1.73 | 1.23 | 0.81,1.85 |
| ≥180 | 0.95 | 0.56,1.62 | 1.08 | 0.70,1.66 |
referent categories: age (<55 years), female, nonwhite, NSTEMI, absence of selected comorbidities, absence of selected hospital clinical complications, systolic BP 100–119 mmHg, eGFR ≥60 ml/min/1.73m2, serum glucose 80–109 mg/dl
odds ratio
After multivariate adjustment, older age, male sex, an NSTEMI, a low estimated glomerular filtration rate (<60mL/min), and having a medical history of heart failure or stroke were important predictors of mortality at 2 years. In addition, a hospital course complicated by heart failure or cardiogenic shock were important clinical predictors of death at 2 years (Table 2).
When we examined whether the factors associated with a poor long-term survival had changed between our initial (2001) and most recent years under study (2007), most factors associated with higher death rates retained their prognostic importance. In contrast to patients hospitalized in 2001, however, patients discharged from all greater Worcester medical centers in 2007 who developed either atrial fibrillation or cardiogenic shock in the hospital were no longer at risk for dying over the long-term, whereas developing a stroke in the hospital was associated with higher 2 year death rates.
In comparing the use of cardiac treatments between our initial and most recent study years, a greater percentage of patients were treated with aspirin (91.9% vs 76.4%), beta blockers (89.6% vs. 75.1%), ACE inhibitors/ARB’s (65.8% vs 48.8%), and lipid lowering drugs (88.5% vs. 52.7%) at the time of hospital discharge in 2007 than in 2001 whereas fewer patients were discharged on calcium channel antagonists (10.8% vs 13.4%). We observed an increase in the proportion of patients undergoing cardiac catheterization (78.7% vs. 58.6%) and a percutaneous coronary intervention (57.0% vs. 35.2%) during their index hospitalization, whereas fewer patients underwent coronary bypass surgery (7.5% vs. 10.4%) in 2007 compared with 2001.
Discussion
The results of this study in residents of central Massachusetts suggest that long-term survival after an initial AMI has improved between 2001 and 2007. Advanced age, male sex, developing an NSTEMI, presence of selected cardiovascular co-morbidities, and development of several in-hospital clinical complications were associated with a poorer post-discharge prognosis. In addition, the use of effective cardiac medications at the time of hospital discharge has increased during the period under study.
The findings from a limited number of U.S. and European studies were similar to those observed in the present investigation, noting an improvement in long-term prognosis after hospitalization for AMI over time [12–15].
In prior analyses from the Worcester Heart Attack Study, we have demonstrated declines in out-of-hospital mortality attributed to CHD [16], inhospital case-fatality rates [3,17], as well as post discharge death rates during varying study years [17,18]. We extend these findings by demonstrating declines in the post-discharge death rates during the most recent years under study among hospital survivors of an initial AMI.
Our encouraging findings likely reflect the beneficial effects of the more aggressive management of patients during hospitalization for AMI and likely increased adherence to effective cardiac medications after hospital discharge for AMI. Improving trends in long-term survival may also reflect the increasing adoption of positive lifestyle practices after hospital discharge for AMI though this hypothesis is purely speculative since we did not collect information about possible contributory factors that may have been altered after hospital discharge.
Irrespective of the reasons underlying the decline in post discharge death rates, the risk of dying during the first several years after hospital discharge for an initial AMI remained relatively high. We observed a 19% 2-year death rate in 2007, highlighting the need for increased surveillance and investigation into how to optimize all aspects of medical care of these patients.
Consistent with the published literature, we found an association between advancing age and male sex with poor prognosis after AMI [17,19]. In addition, having an NSTEMI was predictive of a poor prognosis at each of our post-discharge follow-up points examined, findings consistent with the published literature [11,20].
Prior studies have demonstrated a poorer long-term prognosis for patients with AMI who also had coexisting diabetes, hypertension, kidney disease, and stroke [21–23]. Our study found an association between several of these cardiovascular comorbidities with higher 3 month death rates. The strong association we found between previously diagnosed heart failure and a poor long-term prognosis is not surprising, given that the prognosis of patients with heart failure is particularly grim [9,24]. Patients with a prior history of stroke have been found to be treated less aggressively with subsequently increased post-discharge mortality [25].
A low systolic blood pressure was associated with higher death rates at 3 months, whereas kidney dysfunction was associated with a poor 2 year prognosis. This latter finding is consistent with previous studies which also found an increase in short and long-term death rates in patients with renal dysfunction and AMI [26,27]. Patients with a low systolic blood pressure are likely to be hemodynamically compromised and be at markedly increased risk for developing heart failure, cardiogenic shock, and dying.
We found that the in-hospital development of atrial fibrillation (AF) was associated with a poor short-term prognosis, but not at 2-years. This counterintuitive finding was surprising since prior studies have suggested that developing AF following admission to the hospital for AMI is predictive of poor short and long-term mortality [8,28]. Our results may reflect a “healthy survivor effect”, namely that new onset AF tends to complicate more severe cases of AMI and is associated with higher in-hospital, but not long-term, death rates. We also found that having a hospital course complicated by heart failure, cardiogenic shock, or a stroke was associated with higher long-term death rates, findings similar to the results of previous observational studies [3,6,29].
Future studies are needed to explore the impact of these factors on other clinically meaningful endpoints after hospital discharge for an initial AMI, including hospital readmission, development of a recurrent AMI, and quality of life. Research into new biomarkers and genomic tests to identify and further refine the characteristics of patients at increased risk for adverse outcomes after hospital discharge for AMI will be crucial to improving the treatment and prognosis of these patients.
Although limited by the non-randomized nature of this study, the increases in long-term survival that we observed in 2007 compared with 2001 may have resulted from improvements in the hospital and post discharge medical management of patients. In this and other community-based investigations, the use of effective cardiac medications and coronary interventional procedures has increased markedly over time.
The major strength of this study is our population-based design which included only validated cases of initial AMI occurring in the greater Worcester population during the years under study. On the other hand, since this central Massachusetts community is predominately white, the generalizability of our findings to persons of other race/ethnicities might be limited. We did not collect information on patient’s socioeconomic or cognitive status, or about other factors that have been shown to affect long-term prognosis after AMI, such as severity of the AMI and extent of underlying atherosclerosis. We did not collect information on patient’s adherence to various post-discharge treatment regimens or changes in patient’s lifestyle practices after being discharged from the hospital.
Acknowledgments
This research was made possible by the cooperation of participating hospitals in the Worcester metropolitan area. Funding support was provided by the National Institutes of Health (RO1 HL35434). Partial salary support for Drs. Goldberg, Gore, and McManus was provided for by the National Institutes of Health grant 1U01HL105268-01.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in the attack rates and survival rates of acute myocardial infarction (1975–1981): The Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 2.Goldberg RJ, Gorak EJ, Yarzebski J, Hosmer DW, Dalen P, Gore JM, Alpert JS, Dalen JE. A community-wide perspective of gender differences and temporal trends in the incidence and survival rates following acute myocardial infarction and out-of-hospital deaths due to coronary heart disease. Circulation. 1993;87:1947–1953. doi: 10.1161/01.cir.87.6.1947. [DOI] [PubMed] [Google Scholar]
- 3.Floyd KC, Yarzebski J, Spencer FA, Lessard D, Dalen JE, Alpert JS, Gore JM, Goldberg RJ. A 30-year perspective (1975–2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent Trends in the Incidence, Treatment, and Outcomes of Patients with ST and Non-ST-Segment Acute Myocardial Infarction. Am J Med. 2011;124:40–47. doi: 10.1016/j.amjmed.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction) Circulation. 2004;110:e82–292. [PubMed] [Google Scholar]
- 6.Goldberg RJ, Spencer FA, Gore JM, Lessard D, Yarzebski J. Thirty-year trends (1975 to 2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: a population-based perspective. Circulation. 2009;119:1211–1219. doi: 10.1161/CIRCULATIONAHA.108.814947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saczynski JS, Spencer FA, Gore JM, Gurwitz JH, Yarzebski J, Lessard D, Goldberg RJ. Twenty-year trends in the incidence of stroke complicating acute myocardial infarction: Worcester Heart Attack Study. Arch Intern Med. 2008;168:2104–2110. doi: 10.1001/archinte.168.19.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saczynski JS, McManus D, Zhou Z, Spencer F, Yarzebski J, Lessard D, Gore JM, Goldberg RJ. Trends in atrial fibrillation complicating acute myocardial infarction. Am J Cardiol. 2009;104:169–174. doi: 10.1016/j.amjcard.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McManus DD, Chinali M, Saczynski JS, Gore JM, Yarzebski J, Spencer FA, Lessard D, Goldberg RJ. Thirty-year trends in heart failure in patients hospitalized with acute myocardial infarction. Am J Cardiol. 2011;107:353–359. doi: 10.1016/j.amjcard.2010.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sabatine MS, McCabe CH, Morrow DA, Giugliano RP, de Lemos JA, Cohen M, Antman EM, Braunwald E. Identification of patients at high risk for death and cardiac ischemic events after hospital discharge. Am Heart J. 2002;143:966–970. doi: 10.1067/mhj.2002.122870. [DOI] [PubMed] [Google Scholar]
- 11.Chan MY, Sun JL, Newby LK, Shaw LK, Lin M, Peterson ED, Califf RM, Kong DF, Roe MT. Long-term mortality of patients undergoing cardiac catheterization for ST-elevation and non-ST-elevation myocardial infarction. Circulation. 2009;119:3110–3117. doi: 10.1161/CIRCULATIONAHA.108.799981. [DOI] [PubMed] [Google Scholar]
- 12.Nauta ST, Deckers JW, Akkerhuis M, Lenzen M, Simoons ML, van Domburg RT. Changes in clinical profile, treatment, and mortality in patients hospitalised for acute myocardial infarction between 1985 and 2008. PLoS One. 2011;6:e26917. doi: 10.1371/journal.pone.0026917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmidt M, Jacobsen JB, Lash TL, Botker HE, Sorensen HT. 25 year trends in first time hospitalisation for acute myocardial infarction, subsequent short and long term mortality, and the prognostic impact of sex and comorbidity: a Danish nationwide cohort study. Br Med J. 2012;344:e356. doi: 10.1136/bmj.e356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berger AK, Duval S, Jacobs DR, Jr, Barber C, Vazquez G, Lee S, Luepker RV. Relation of length of hospital stay in acute myocardial infarction to postdischarge mortality. Am J Cardiol. 2008;101:428–434. doi: 10.1016/j.amjcard.2007.09.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.García-García C, Subirana I, Sala J, Bruguera J, Sanz G, Valle V, Arós F, Fiol M, Molina L, Serra J, Marrugat J, Elosua R. Long-term prognosis of first myocardial infarction according to the electrocardiographic pattern (ST elevation myocardial infarction, non-ST elevation myocardial infarction and non-classified myocardial infarction) and revascularization procedures. Am J Cardiol. 2011;108:1061–1067. doi: 10.1016/j.amjcard.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg RJ, Glatfelter K, Burbank-Schmidt E, Lessard D, Gore JM. Trends in community mortality due to coronary heart disease. Am Heart J. 2006;151:501–507. doi: 10.1016/j.ahj.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 17.Goldberg RJ, McCormick D, Gurwitz JH, Yarzebski J, Lessard D, Gore JM. Age-related trends in short- and long-term survival after acute myocardial infarction: a 20-year population-based perspective (1975–1995) Am J Cardiol. 1998;82:1311–1317. doi: 10.1016/s0002-9149(98)00633-x. [DOI] [PubMed] [Google Scholar]
- 18.Botkin NF, Spencer FA, Goldberg RJ, Lessard D, Yarzebski J, Gore JM. Changing trends in the long-term prognosis of patients with acute myocardial infarction: a population-based perspective. Am Heart J. 2006;151:199–205. doi: 10.1016/j.ahj.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen HL, Saczynski JS, Gore JM, Waring ME, Lessard D, Yarzebski J, Reed G, Spencer FA, Li SX, Goldberg RJ. Long-term trends in short-term outcomes in acute myocardial infarction. Am J Med. 2011;124:939–946. doi: 10.1016/j.amjmed.2011.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kushner FG, Hand M, Smith SC, Jr, King SB, 3rd, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE, Jr, Green LA, Hochman JS, Jacobs AK, Krumholz HM, Morrison DA, Ornato JP, Pearle DL, Peterson ED, Sloan MA, Whitlow PL, Williams DO. Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2009;120:2271–306. doi: 10.1161/CIRCULATIONAHA.109.192663. [DOI] [PubMed] [Google Scholar]
- 21.Sachdev M, Sun JL, Tsiatis AA, Nelson CL, Mark DB, Jollis JG. The prognostic importance of comorbidity for mortality in patients with stable coronary artery disease. J Am Coll Cardiol. 2004;43:576–582. doi: 10.1016/j.jacc.2003.10.031. [DOI] [PubMed] [Google Scholar]
- 22.Jabre P, Roger VL, Murad MH, Chamberlain AM, Prokop L, Adnet F, Jouven X. Mortality associated with atrial fibrillation in patients with myocardial infarction: a systematic review and meta-analysis. Circulation. 2011;123:1587–1593. doi: 10.1161/CIRCULATIONAHA.110.986661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Norhammar A, Lindback J, Ryden L, Wallentin L, Stenestrand U. Improved but still high short- and long-term mortality rates after myocardial infarction in patients with diabetes mellitus: a time-trend report from the Swedish Register of Information and Knowledge about Swedish Heart Intensive Care Admission. Heart. 2007;93:1577–1583. doi: 10.1136/hrt.2006.097956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saczynski JS, Darling CE, Spencer FA, Lessard D, Gore JM, Goldberg RJ. Clinical features, treatment practices, and hospital and long-term outcomes of older patients hospitalized with decompensated heart failure: The Worcester Heart Failure Study. J Am Geriatr Soc. 2009;57:1587–1594. doi: 10.1111/j.1532-5415.2009.02407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spencer FA, Gore JM, Yarzebski J, Lessard D, Jackson EA, Goldberg RJ. Trends (1986 to 1999) in the incidence and outcomes of in-hospital stroke complicating acute myocardial infarction (The Worcester Heart Attack Study) Am J Cardiol. 2003;92:383–388. doi: 10.1016/s0002-9149(03)00654-4. [DOI] [PubMed] [Google Scholar]
- 26.Anavekar NS, McMurray JJ, Velazquez EJ, Solomon SD, Kober L, Rouleau JL, White HD, Nordlander R, Maggioni A, Dickstein K, Zelenkofske S, Leimberger JD, Califf RM, Pfeffer MA. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351:1285–1295. doi: 10.1056/NEJMoa041365. [DOI] [PubMed] [Google Scholar]
- 27.Freeman RV, Mehta RH, Al Badr W, Cooper JV, Kline-Rogers E, Eagle KA. Influence of concurrent renal dysfunction on outcomes of patients with acute coronary syndromes and implications of the use of glycoprotein IIb/IIIa inhibitors. J Am Coll Cardiol. 2003;41:718–724. doi: 10.1016/s0735-1097(02)02956-x. [DOI] [PubMed] [Google Scholar]
- 28.Schmitt J, Duray G, Gersh BJ, Hohnloser SH. Atrial fibrillation in acute myocardial infarction: a systematic review of the incidence, clinical features and prognostic implications. Eur Heart J. 2009;30:1038–1045. doi: 10.1093/eurheartj/ehn579. [DOI] [PubMed] [Google Scholar]
- 29.Harjola VP, Follath F, Nieminen MS, Brutsaert D, Dickstein K, Drexler H, Hochadel M, Komajda M, Lopez-Sendon JL, Ponikowski P, Tavazzi L. Characteristics, outcomes, and predictors of mortality at 3 months and 1 year in patients hospitalized for acute heart failure. Eur J Heart Fail. 2010;12:239–248. doi: 10.1093/eurjhf/hfq002. [DOI] [PubMed] [Google Scholar]


