Abstract
Objective
Few articles have examined specific counseling tools used to increase antiretroviral therapy (ART) adherence. We present communication tools used in the context of Project MOTIV8, a randomized clinical trial.
Methods
We developed, piloted, and evaluated pictorial images to communicate the importance of consistent dose timing and the concept of drug resistance. Electronic drug monitoring (EDM) review was also used to provide visual feedback and facilitate problem solving discussions. Adherence knowledge of all participants (n=204) was assessed at baseline and 48 weeks. Participant satisfaction with counseling was also assessed.
Results
Adherence knowledge did not differ at baseline, however, at 48 weeks, intervention participants demonstrated significantly increased knowledge compared to controls F(1,172) = 10.76, p=0.001, (12.4% increase among intervention participants and 1.8% decrease among controls). Counselors reported that the tools were well-received, and 80% of participants felt the counseling helped them adhere to their medications.
Conclusions
Counseling tools were both positively received and effective in increasing ART adherence knowledge among a diverse population.
Practice Implications
While developed for research, these counseling tools can be implemented into clinical practice to help patients; particularly those with lower levels of education or limited abstract thinking skills to understand medical concepts related to ART adherence.
Keywords: ART adherence, counseling tools, patient communication tools, concrete, education tools, high and low resource, electronic drug monitoring (EDM) review, Motivational Interviewing
1. Introduction
Despite its importance, maintaining high levels of antiretroviral therapy (ART) adherence has proven to be difficult for the majority of people living with HIV. [1,2] A pooled analysis of North American studies (17,573 patients total) indicated that only 55% (95% CI, 49%-62%) of patients sampled (mostly self-reported) achieved adequate levels of adherence. [3] In low-resource settings where ART access continues to increase, the implications of non-adherence are great, as few second line regimens are available to those who develop resistance and experience treatment failure. [4] Despite a variety of regimen options in high resource settings, the costs of resistance-induced treatment failure are still high [5,6] and negatively impact the cost-effectiveness of treatment. [7]
While the literature is filled with studies exploring the predictors and correlates of ART adherence, [8-10] methodologies for measuring adherence, [11] and behavioral interventions to improve adherence, [12-13] few articles have focused on the use of specific counseling tools used to increase adherence. Concrete counseling tools that communicate how HIV impacts immune functioning and the importance of ART adherence can improve understanding of complex medical concepts. Several studies have demonstrated the association between low health literacy and/or lower educational attainment with poorer ART adherence. [14-16] Effective pictorial communication tools may be particularly useful to improve understanding and subsequent ART adherence among such populations.
1.1. Use of pictorial diagram tools to explain abstract adherence concepts
The biomedical interactions between HIV, one’s immune system, and antiretroviral drugs are abstract concepts that are not easily translated into everyday language. Even people living with HIV/AIDS (PLHA) without general literacy challenges may struggle to fully comprehend the technical and domain-specific vocabulary often used by health professionals to explain concepts like drug resistance. [17] Concrete tools such as pictographs have been used to simplify complex medical concepts in the context of health education, [18-20] and are frequently used to communicate instructions for medication use (e.g., time of day, with or without food) among elderly and low literacy patients. [21] Pictographs have been the best method for communicating risk and benefit information regarding treatment options for patients with both low and high numeric literacy. [21] Patients report trusting information that is conveyed in pictographs. [22] Such pictorial tools are particularly important for use among populations with minimal education, challenged cognitive skills, or in settings where providers are not fluent in the varied languages or dialects of their patients.
1.2. Use of electronic drug monitoring (EDM) as a tool to support adherence counseling
EDM has recently been assessed as a tool to enhance adherence. Among a sample of people living with HIV in China, those whose provider used monthly EDM print outs as a counseling tool to discuss percent of doses taken and percent of doses taken on time had significantly higher adherence than those who received standard counseling without EDM feedback (96.5 vs. 84.5%, p=0.003). [23] Similarly, de Bruin and colleges (2010) contrasted visual images of patients’ ideal level of adherence with that of their own EDM print outs. Researchers then discussed strategies to reach participants’ ideal level of adherence as a way to increase motivation to adhere. [24] Finally, among HIV-positive patients with a history of substance abuse, Rosen and colleagues found that contingency management counseling, including EDM data review, improved short term adherence by 15% (61% to 76%) during a 16 week period. [25] While data regarding the impact of EDM review on ART adherence is emerging, discussion of how to incorporate EDM review into adherence counseling is missing.
1.3 Background of MOTIV8 intervention
This paper describes the counseling tools utilized in the context of Project MOTIV8, a three armed, multisite randomized controlled trial of behavioral interventions to increase ART adherence among HIV-positive urban clinic patients. The study’s primary aim was to determine whether Motivational Interviewing-based Cognitive Behavioral Therapy (MI-CBT) counseling combined with modified Directly Observed Therapy (mDOT) is more effective than MI-CBT counseling alone or standard care in increasing adherence to ART. In this manuscript, we present concrete, pictorial communication tools used to enhance patients’ understanding of drug resistance and the importance of taking medications on time, as well as procedures for incorporating the review of EDM data into MI-CBT counseling sessions. We examine the impact of these counseling tools on patients’ ability to apply information to vignettes of real dosing schedules. Finally, we discuss the application in both low and high resource clinical settings.
2. Methods
2.1. Design
The 204 participants were randomly assigned to one of three groups: 1) Standard Care (SC) which received medical care as usual (n=65, 32%), 2) Motivational Interviewing-based Cognitive Behavioral Therapy (MI-CBT) adherence counseling (n=70, 34%), or 3) MI-CBT adherence counseling with modified Directly Observed Therapy (MI-CBT/mDOT; n=69, 34%). The MI-CBT adherence counseling provided in the two active intervention arms was identical, and no additional counseling was conducted during mDOT visits. We combined data from patients in both intervention arms (n=139) compared to standard of care (n=65).
MI-CBT Adherence Counseling
Participants in the two intervention arms (MI-CBT and MI-CBT/mDOT, n=139) were assigned to receive 10 counseling sessions (six face-to-face, four by phone) over a 24 week period from extensively trained Master’s level project counselors. The intervention was guided by the Information-Motivation-Behavioral Skills (IMB) model of behavior change, [27] which asserts that information is a prerequisite, but in itself insufficient to alter behavior, and that motivation and behavioral skills are critical determinants in promoting behavior change. Counseling aimed to provide information, enhance motivation and develop problem solving skills to increase adherence to ART.
Standard of Care
Evaluation of the quality of the standard of care was conducted by medical record abstraction, patient surveys and provider interviews which revealed high (>80%) compliance with current ART treatment guidelines and frequent discussion of adherence challenges. [28] While established clinic-based adherence support was provided to participants in the standard of care arm, the intervention arms provided unique educational counseling tools, the review of EDM data, and a motivational interviewing style.
2.2. Development and use of counseling tools
A combination of ART counseling tools were employed in the MOTIV8 intervention. Pictorial tools conveying adherence concepts through the use of visual images and color are categorized as low resource tools because the costs associated with their development and utilization are minimal. However, the use of EDM as a counseling tool is considered a high resource adherence counseling tool due to the expense of the EDM devices, associated software, and computer requirements for utilization. Recognizing the diversity in clinical settings providing ART adherence counseling, we present both low and high resource adherence counseling tools for consideration.
2.2.1. Low resource, pictorial tools to increase understanding of adherence
Study staff developed a range of strategies to communicate the benefits and necessity for high ART adherence. To make tools concrete and understandable to all participants, the use of pictographic images, color scales, and differing size dimensions were developed and piloted among a group of patients from the target population. Patient feedback was incorporated and the finalized counseling tools were used to illustrate the importance of taking prescribed medications on time and in the manner indicated (e.g., with/without food). Tools were also developed to assist participants in understanding the concept of drug resistance. We describe below two pictographic images used in MOTIV8 to enhance participants’ knowledge and understanding of ART adherence.
“Target Tool”
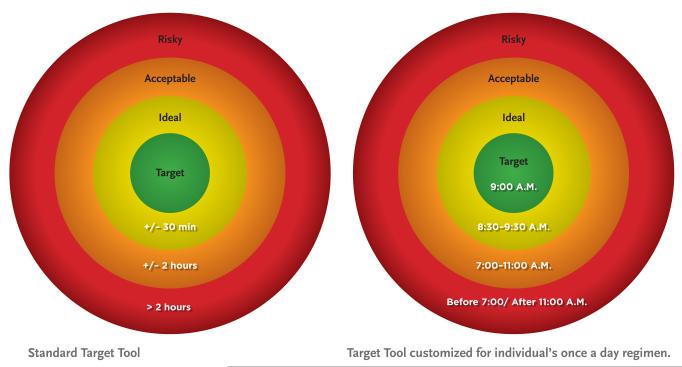
The Target Tool (Figure I) was developed to communicate the concept of a “window period” (WP) to increase the percent of doses taken on time. To guide participants when to take their medications, the ideal WP (center green zone) around one’s dose time was defined as +/−30 minutes from their scheduled (or “target”) dosing time, and the acceptable WP (middle yellow zone) for once or twice a day dosing was defined as +/− 2 hours from their scheduled dosing time. The acceptable WP for medications that should be taken three times a day was +/− 1 hour. Participants were informed that taking medication in the acceptable WP was more effective than taking it outside of the WP, or skipping a dose altogether; however, the goal of taking medications within the ideal WP was stressed. The outer red zone was described as risky given the increased threat of viral mutation and development of drug resistance when medications were taken beyond the two hour WP.
FIGURE 1.
Target Tool to increase understanding of the ideal ‘window period’ for taking ARVs.
The Target Tool facilitated conversations on how to link taking one’s medications with other consistently occurring daily events such as the morning or evening news. Counselors utilized the tool to illustrate the ideal and acceptable WP for each participant based on their specific regimen. Together, they then customized the target tool by writing in the target, ideal, and acceptable times to take their medications (second image of Figure 1).
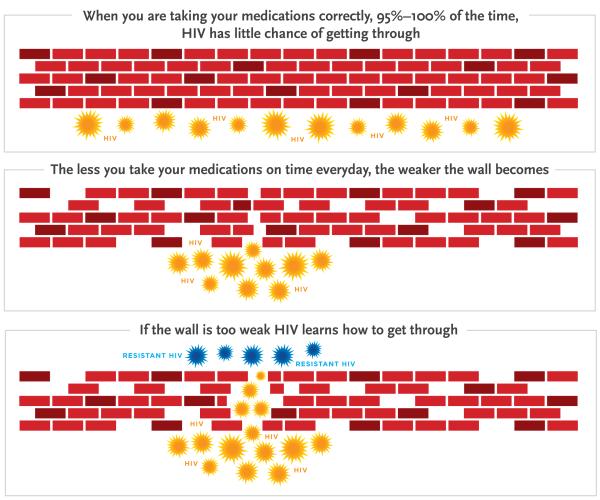
Illustration of viral suppression, viral mutation and drug resistance
Pilot testing revealed that the concepts of viral suppression, viral mutation and drug resistance do not lend themselves to simple verbal explanation with both low and high literacy participants. To address this, an image to illustrate these complicated and abstract concepts was developed. As seen in Figure II, the image of a brick wall was used to represent how ART medication, when properly taken, creates a barrier that blocks HIV from copying itself. Counselors explained that when patients take their ART medications timely and exactly as prescribed, the wall stays strong and HIV cannot get through. However, if doses are missed or untimely, the wall will become weak with exposed gaps allowing HIV to get through it.
FIGURE 2.
Brick Wall Image to Illustrate the Concept of Drug Resistance
Next, the idea of viral mutation from suboptimal adherence was communicated by explaining that once HIV learns how to break through the wall, it will be able to get through that part of the barrier forever. If this frequently happens, HIV will become exceptionally smart, and the medication that built that part of the wall (including similar medications) eventually won’t work. To communicate this, the final image depicts a wall weakened by poor adherence with several gaps allowing HIV to break through and become resistant. Participants were encouraged to think of their medications as building blocks that were fortifying the wall against HIV.
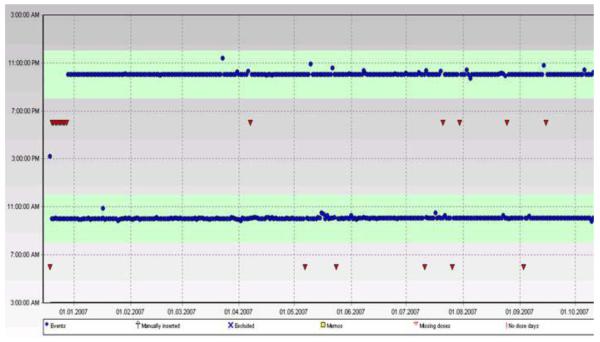
2.2.2. High resource tool to increase adherence to ART
Utilization of EDM feedback as part of counseling EDM (specifically, the Medication Event Monitoring System; http://www.aardex.ch) were used to measure adherence. Review of the data from the EDM was incorporated into the adherence counseling for intervention participants. At the beginning of each face-to-face session, counselors uploaded data from the EDM and, together with participants, reviewed a graph of their adherence over the period of time since their last session (usually two weeks). The first screen shot looked like a calendar and recorded a 0, 1, 2 or 3 on each day (depending on their dosing regimen) representing the number of times the EDM was opened in each 24 hour period, see Figure III. Counselors would first ask participants if the screen shot looked like an accurate representation of their recent adherence. This provided participants the opportunity to inform them of any occasions where they “pocketed pills” (i.e., prematurely putting a dose in their pocket to be taken later to avoid carrying the bottle) or particular challenges that may have impaired adherence.
Figure III.
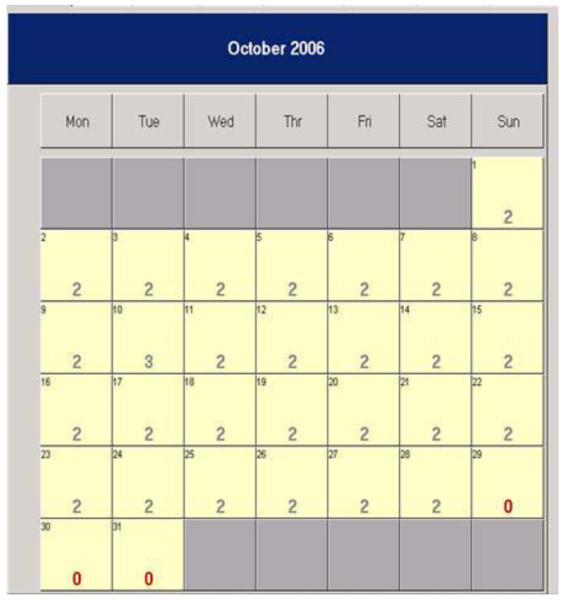
Initial calendar view of the EDM print screen showing number of MEMS bottle openings per day.
The second screen shot, see Figure IV, graphed the number and timing of daily openings of the medication bottle, demarking those that occurred within the ideal two hour window around target dosing times (shaded area) and indicating missed doses with triangles. Counselors would briefly summarize the results without judgment, indicating the percent of doses taken and the percent taken on time. Counselors would then elicit from participants their thoughts regarding their recent adherence, and if below 95%, discuss the challenges that were impeding higher adherence. Using the screen shots allowed counselors and participants to easily see what was really occurring and to compare and contrast current and past adherence. This is in contrast to the more typical questioning, e.g., “How is your adherence going?”, which requires patients to rely on their memory and ability to average over a long period of time, and supports social desirable responding. Having the data visually displayed also facilitated a discussion of how and why adherence was either becoming easier or more difficult and naturally led to problem solving. For example, if the counselor and participant were able to observe that the morning doses did not present a challenge, but that it was more difficult to adhere to the evening doses, they could work together to develop a plan to overcome barriers more commonly experienced at the end of the day. This process of evaluating EDM data has the potential to be confrontational, particularly if a patient has poor adherence. Maintaining a patient-centered style of communication (i.e. Motivational Interviewing) was critical in avoiding negative interactions and handling resistance in a constructive manner.
Figure IV.
Graphic EDM feedback illustrating ART doses taken and those taken on time.
2.3. Evaluation of ART knowledge and counseling satisfaction
2.3.1. Procedure
Participants’ ART adherence knowledge and satisfaction with the counseling experience were assessed via measures developed for this study and administered via audio computer-assisted self-interview. For the purposes of this study, we used ART adherence knowledge data collected at baseline and 48 weeks. Satisfaction with the counseling experience was assessed at 24 weeks, which coincided with the conclusion of counseling.
The material resources required to replicate the target tool and resistance image are nominal, and individuals can be easily trained in their use. Color copying and optional lamination of each image makes these tools a feasible option for clinics and programs in low resource settings. Effective use of the counseling tools requires less than 1 hour of training, presuming that providers/counselors already have a solid understand of the dynamics of HIV adherence, viral suppression, viral mutation and drug resistance.
The use of visual EDM feedback data as a counseling tool to improve adherence requires significantly more resources. The cost of EDM devices (MEMS caps) used in this study was approximately US$100 each (www.aardexgroup.com, purchased in 2004). The likelihood of lost or non-functioning devices that require replacement should be calculated into potential expenses, which in our study was 15% (30 replacements for 204 participants). Counseling rooms require a computer and EDM reader with specialty software (approximately $365 and $406, respectively). Training for the EDM review procedures could be conducted during a full day session, however, mastery of the motivational interviewing style takes considerably more intense training. Counseling skills specific to the EDM review could be taught in 1-2 days, which is similar to the training requirements estimated by Sabin and colleagues. [23] The average face-to-face counseling session in this study was 10 minutes, with a range of 5-20 minutes depending on participant’s level of adherence.
2.3.2. Measures
ART Adherence Knowledge: The knowledge measure consisted of vignettes created to assess participants’ understanding of the importance of dose timing to avoid drug resistance. Participants were presented with three vignettes and asked to identify the target, ideal and acceptable dosing schedule for once, twice and/or three times per day ART regimens. Vignettes were matched to participants own dosing regimens so that participants were only asked about dosing schedules that they were actually on. For example, participants on only once per day ART medications were administered only the once per day questions. Participants with a combination of required doses responded to multiple vignettes as appropriate. The three vignettes and response options for the once per day dosing regimen are presented in Table 1. An ART adherence knowledge total score was produced by calculating the percent of correct answers over the total number of questions administered for each participant.
Table 1.
Vignettes used to assess knowledge of target, ideal, and acceptable dose for patients on a once per day ART regimen.
| Vignettes | Response Options | |
|---|---|---|
| 1 | David has been given an HIV regimen that involves taking pills once per day. In your opinion, which one of the following options for taking his medication would be IDEAL so he has the smallest possible chance of developing resistance? |
|
| 2 | LaShonda cannot take her medication exactly at the time she is supposed to. In your opinion, how much can LaShonda be off from the perfect time before she increases her chance of developing resistance even slightly? In other words, which one for the following options is the largest amount of time before or after the scheduled time that you would still consider IDEAL so she has the smallest possible chance of developing resistance? |
|
| 3 | Julie cannot take her medication exactly at the time she is supposed to. In your opinion, how much can Julie be off from the perfect time before she significantly increases her chance of developing resistance? In other words, which one of the following options is the largest amount of time before or after the scheduled time that you would still consider ACCEPTABLE to avoid significantly increasing her chance of developing resistance? |
|
Note. Correct answers for each vignette in bold.
Participants were presented with vignettes that reflected their own ART dosing regimen (once, twice, three times per day dosing or a combination of the above). Only once per day dosing vignettes are presented in Table 1.
Satisfaction with Counseling Experience: Participants responded to a series of questions regarding their satisfaction with the overall counseling experience in which the communication tools were used. Specifically: 1) Did the counseling help participants to adhere to their ART medications?; 2) Did it change the way they think about their health?; and 3) Would it be helpful with other types of health issues? Response options ranged from 0 “not at all helpful” to 4 “extremely helpful.”
2.3.3. Analysis
We used a t-test to compare ART Adherence Knowledge total scores between
intervention and standard of care participants at baseline. Changes in knowledge were analyzed using repeated measures ANOVA with group (intervention vs. standard care) as the between-subjects factor and time (baseline to follow-up) as the within-subjects factor. Mauchly’s Test of Sphericity and Schefe’s post hoc test were conducted to estimate marginal means. We used a t-test to compare regimen complexity between the standard of care and intervention groups, descriptive statistics to assess participant satisfaction with the counseling experience, and qualitative data collected from study counselors regarding the use of the counseling tools.
3. Results
3.1. Participants
The majority of participants were male (75%) and African American (57%) with over half of the sample (53%) identifying as either homosexual or bisexual. Mean age of participants was 40.4 years (SD=9.5 ), 53% had the equivalent of a high school education or less, and 65% reported secure housing (rented or owned residence). Approximately one third of participants were ART naïve at baseline.
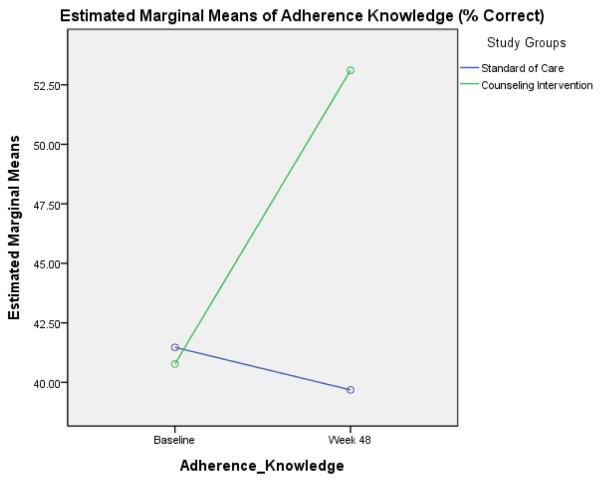
3.2. ART Adherence Knowledge
There were no baseline differences in the percent of correctly answered questions between participants in the intervention and standard care groups (M =40.7, SE=1.9 vs. M=41.5, SE=2.8; t = 0.64, p = 0.53). Furthermore, we found no difference in regimen complexity between the intervention and standard of care groups (M =1.49, SE=0.05 vs. M=1.52, SE=0.07; t = 0.31, p = 0.75). The change in ART Adherence Knowledge from baseline to 48 weeks was significantly different between groups (F(1,172)=10.76, p=0.001). Inspection of the means revealed that intervention participants experienced a 12.4% increase in ART Adherence Knowledge (40.7% to 53.1%) from baseline to 48 weeks whereas standard care participants evidenced a 1.8% decrease (41.5% to 39.7%). Figure V displays the baseline to 48 week changes in ART Adherence Knowledge in the two groups.
Figure V.
ART adherence knowledge (% correct) compared by intervention group at baseline and 48 weeks.
3.3. Participant satisfaction
Overall, 80% of intervention participants felt the counseling was mostly (32%) or very (48%) helpful for adhering to their medications. A majority (57%) agreed that the counseling sessions changed the way they think about their health. Over 80% felt this type of counseling would help them with other types of health issues. 3.4. Qualitative data from counselors on use of the adherence tools Counselors reported that while explaining the Target Tool, several participants experienced “ah-ha” moments regarding the importance of taking the medications at the same time every day. While it is very likely that their provider had previously given this same advice, it was the systematic explanation facilitated by the tool that helped participants apply the advice to their own regimens.
4. Discussion and Conclusion
4.1. Discussion
The counseling tools described in this paper were evaluated in the context of a rigorously conducted randomized controlled trial, and found to significantly increase knowledge of medication timing and avoidance of resistance. Studies assessing ART knowledge have used various measures and definitions. [28,29] In assessing dosing knowledge, the ADEPT (Adherence and Efficacy Protease Therapy) study realized a greater increase in the proportion of participants with correct dosing knowledge at 48 weeks compared to baseline (20% vs. 12% increase), [30] however, their criteria for ‘accurate ART dosing knowledge’ was considerably less rigorous (correctly identifying their dosing time(s) each day vs. knowledge of the window periods beyond their specified dose time that were within the ideal, acceptable and risky categories). While it is recognized that accurate knowledge alone is insufficient for long term behavior change, it is a fundamental element, without which, additional efforts may be wasted. The larger MOTIV8 study measured actual adherence, and found a significant interaction with treatment effects of the MI-CBT/mDOT intervention which was the strongest during the active phase of the intervention and declined over time.[31]
Strengths and Limitations
We recognize that despite the increase achieved through counseling, the absolute level of adherence knowledge regarding medication timing and drug resistance is still low. As this is not a dismantling study of the various intervention components, we cannot identify the exact contribution of each element or counseling tool to participants’ ART adherence knowledge. Rather, we describe counseling tools that were specifically designed to communicate information necessary to correctly answer adherence questions posed in the vignettes. These tools likely increased ART adherence knowledge, were well received by participants, and can be implemented in a variety of settings.
Given the need to improve ART adherence counseling in both high and low resource settings, two of the three tools described are feasible for low-resource clinical settings. While EDM review may remain cost prohibitive for many clinics in low and even some high-resource countries due to equipment costs and the need for dedicated personnel, limiting the use of EDM review only to those struggling to maintain adequate (versus high) adherence could reduce costs and increase the feasibility of its use. [23] Future research is needed to develop rigorous cost-benefit analyses of high resource counseling interventions such as EDM review, and the potential savings accrued by reduced frequency of hospitalization and salvage therapies resulting from improved ART adherence. Lastly, participants in the intervention arms did receive more contact time with counselors compared to participants receiving the standard of care. Therefore, it cannot be ruled out that increases in knowledge were influenced not only by the counseling tools and counseling style, but also increased contact.
4.2. Conclusion
Given the challenge of understanding abstract and complex medical concepts, pictorial images are valued for their ability to communicate such information concretely. These counseling tools can be used to facilitate ART adherence communication between patients and their providers. Such visual counseling tools may be especially valuable when working with patients who are not fluent in the provider’s native language, unfamiliar with technical medical terms, or for patients with limited cognitive skills. More of these adherence counseling tools need to be incorporated into low and high resource clinical practice as appropriate.
4.3. Practice implications
These intervention counseling tools can be implemented in many settings to enhance ART adherence counseling. The two low-resource concrete educational tools are appropriate for use by HIV providers, nurses, counselors or NGO staff working with people on ART in both low and high resource settings. The images, particularly the target tool, can be sent home with the patient as a visual reminder or stimulus cue for adherence. Pharmacists may also find such tools useful when counseling clients on how to take their medications. The pictorial tools are ideal for use in all settings, but may be of most benefit in settings with low literacy rates or where provider communication is compromised by language barriers. Additional pilot testing of the images in the local context will likely identify helpful adoptions that will make them more relevant for patients (e.g., replacing the bricks with contextually appropriate material). Additional refinements of the images or how they are explained might also be developed to enhance patients’ understanding of these and other adherence topics (e.g., side effect management).
Although the use of EDM feedback was utilized in the context of a clinical research trial, modified application in a clinical setting could be feasible. The quality and interpersonal style of the counseling may be diminished, but a designated adherence counselor could spend a few minutes reviewing the adherence output and discussing problem solving with patients. While the expense of EDM review as a counseling tool is high, we know that poor adherence negatively affects the cost-effectiveness of ART, since the same expenditure yields declining benefits. [5,32] Investment in EDM and its associated software and training may be warranted in high resource clinics in settings with high HIV prevalence. Additional cost-benefit analyses are needed to inform such investments.
The need to translate not only research findings, but also effective research tools into clinical practice has been emphasized by HIV providers and funding institutions [33]. As our understanding of adherence continues to evolve, visual concrete images to describe concepts such as persistence and the development of co-morbidities will likely be needed. We hope, in small part, to address this gap in the literature by describing and presenting both low and high resource ART adherence counseling tools used in the context of a successful randomized controlled behavioral intervention trial.
I confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
Acknowledgements
This research was supported by the National Institutes of Mental Health (RO1 MH68197) and made possible by the participants of Project MOTIV8. We gratefully acknowledge the contributions of the clinicians in our participating clinics: Kansas City Free Health Clinic (Sally Neville, Brooke Patterson, Craig Dietz, Edie Toubes-Klingler), Truman Medical Centers (Rose Farnan, James Stanford, David Bamberger, Maithe Enriquez, Sharon Kathrens, Alan Salkind), Department of Veterans Affairs Medical Center – Kansas City (Arundhati Desai, Vinutha Kumar), Kansas University Medical Center (Lisa Clough, Broderick Crawford, Himal Bajracharya, Dan Hinthorn, Michael Luchi, Stephen Waller), and Infectious Disease Associates (Michael Driks, David McKinsey, Joel McKinsey). We also acknowledge the extraordinary efforts of our MOTIV8 team (Jannette Berkley-Patton, Andrea Bradley-Ewing, Tara Carruth, Delwyn Catley, Kristine Clark, Mary Gerkovich, Kathy Goggin, Kirsten Kakolewski, Domonique Malomo Thomson, Karen Williams, Julie Banderas, Megan Pinkston-Camp, David Martinez, Bradley Clark, Antoni Firner, Robin Liston). We thank Drs. Edward Gardner and Thomas Giordano for their helpful comments.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Proctor V, Tesfa A, Tompkins D. Barriers to adherence to highly active antiretroviral therapy as expressed by people living with HIV/AIDS. AIDS Patient Care STDs. 1999;13:535–544. doi: 10.1089/apc.1999.13.535. [DOI] [PubMed] [Google Scholar]
- 2.Coetzee B, Kagee A, Vermeulen N. Structural barriers to adherence to antiretroviral therapy in a resource-constrained setting: the perspectives of health care providers. AIDS Care. 2011;23:146–51. doi: 10.1080/09540121.2010.498874. [DOI] [PubMed] [Google Scholar]
- 3.Mills E, Nachega J, Buchan I, Orbinski J, Attaran A, Singh S, Rachlis B, Wu P, Cooper C, Thabane L, Wilson K, Guyatt G, Bangsberg D. Adherence to antiretroviral therapy in sub-Saharan Africa and North America: a meta-analysis. JAMA. 2006;296:679–90. doi: 10.1001/jama.296.6.679. [DOI] [PubMed] [Google Scholar]
- 4.Pujades-Rodríguez M, Balkan S, Arnould L, Brinkhof M, Calmy A. Treatment failure and mortality factors in patients receiving second-line HIV therapy in resource-limited countries. AIDS Working Group of MSF. JAMA. 2010;21:303–12. doi: 10.1001/jama.2010.980. [DOI] [PubMed] [Google Scholar]
- 5.Valenti W. Treatment adherence improves outcomes and manages costs. AIDS Read. 2001;11:77–80. [PubMed] [Google Scholar]
- 6.National Council on Patient Information and Education [Accessed January 19, 2007];Enhancing Prescription Medicine Adherence: A National Action Plan. 2007 Aug; http://www.talkaboutrx.org/documents/enhancing_prescription_medicine_adherence.pdf.
- 7.Rosen A, Spaulding A, Greenberg D, Palmer J, Neumann P. Patient adherence: a blind spot in cost-effectiveness analyses. Am J Manag Care. 2009;15:626–32. [PubMed] [Google Scholar]
- 8.Nilsson Schonnesson L, Williams M, Ross M, Bratt G, Keel B. Factors associated with suboptimal antiretroviral therapy adherence to dose, schedule, and dietary instructions. AIDS Behav. 2007;11:175–183. doi: 10.1007/s10461-006-9160-0. [DOI] [PubMed] [Google Scholar]
- 9.Lazo M, Gange S, Wilson T, Anastos K, Ostrow D, Witt M, Jacobson L. Patterns and predictors of changes in adherence to highly active antiretroviral therapy: Longitudinal study of men and women. Clin Infect Dis. 2007;45:1377–1385. doi: 10.1086/522762. [DOI] [PubMed] [Google Scholar]
- 10.Atkinson M, Petrozzino J. An Evidence-Based Review of Treatment-Related Determinants of Patients’ Nonadherence to HIV Medications. AIDS Patient Care STDs. 2009;23:903–914. doi: 10.1089/apc.2009.0024. [DOI] [PubMed] [Google Scholar]
- 11.Cambiano V, Lampe F, Rodger A, Smith C, Geretti A, Lodwick R, Holloway J, Johnson M, Phillips A. Use of a Prescription-based Measure of Antiretroviral Therapy Adherence to Predict Viral Rebound in HIV-infected Individuals with Viral Suppression. HIV Medicine. 2010;11:216–224. doi: 10.1111/j.1468-1293.2009.00771.x. [DOI] [PubMed] [Google Scholar]
- 12.Simoni J, Amico K, Smith L, Nelson K. Antiretroviral Adherence Interventions: Translating Research Findings to the Real World Clinic. Curr HIV/AIDS Rep. 2010;7:44–51. doi: 10.1007/s11904-009-0037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bangsberg D. Modified directly observed therapy to improve HIV treatment outcomes: little impact with potent, once-daily therapy in unselected antiretroviral-naïve patients. Curr HIV/AIDS Rep. 2009;6:173–4. doi: 10.1007/s11904-009-0031-y. [DOI] [PubMed] [Google Scholar]
- 14.Wolf M, Davis T, Osborn C, Skripkauskas S, Bennett C, Makoul G. Literacy, self-efficacy, and HIV medication adherence. Patient Educ Couns. 2007;65:253–60. doi: 10.1016/j.pec.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 15.Kalichman S, Ramachandran B, Catz S. Adherence to combination antiretroviral therapies in HIV patients of low health literacy. J Gen Intern Med. 1999;14:267–273. doi: 10.1046/j.1525-1497.1999.00334.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arnsten J, Li X, Mizuno Y, Knowlton A, Gourevitch M, Handley K, Knight K, Metsch L, INSPIRE Study Team Factors associated with antiretroviral therapy adherence and medication errors among HIV-infected injection drug users. J Acquir Immune Defic Syndr. 2007;46:S64–71. doi: 10.1097/QAI.0b013e31815767d6. [DOI] [PubMed] [Google Scholar]
- 17.Davis T, Williams M, Marin E, Parker R, Glass J. Health literacy and cancer communication. Cancer J Clin. 2002;52:134–149. doi: 10.3322/canjclin.52.3.134. [DOI] [PubMed] [Google Scholar]
- 18.Houts P, Bachrach R, Witmer J, Tringali C, Bucher J, Localio R. Using pictographs to enhance recall of spoken medical instructions. Patient Educ and Couns. 1998;35:83–88. doi: 10.1016/s0738-3991(98)00065-2. [DOI] [PubMed] [Google Scholar]
- 19.Houts P, Witmer J, Egeth H, Loscalzo M, Zabora J. Using pictographs to enhance recall of spoken medical instructions II. Patient Educ and Coun. 2001;43:231–242. doi: 10.1016/s0738-3991(00)00171-3. [DOI] [PubMed] [Google Scholar]
- 20.Kalichman S, Cain D, Fuhrel A, Eaton L, Di Fonzo K, Ertl T. Assessing medication adherence self-efficacy among low-literacy patients: development of a pictographic visual analogue scale. Health Educ Res. 2005;20:24–35. doi: 10.1093/her/cyg106. [DOI] [PubMed] [Google Scholar]
- 21.Chuang M, Lin C, Wang Y, Cham T. Development of pictographs depicting medication use instructions for low-literacy medical clinic ambulatory patients. J Manag Care Pharm. 2010;16:337–45. doi: 10.18553/jmcp.2010.16.5.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hawley S, Zikmund-Fisher B, Ubel P, Jancovic A, Lucas T, Fagerlin A. The impact of the format of graphical presentation on health-related knowledge and treatment choices. Patient Educ Couns. 2008;73:448–55. doi: 10.1016/j.pec.2008.07.023. [DOI] [PubMed] [Google Scholar]
- 23.Sabin L, DeSilva M, Hamer D, Xu K, Zhang J, Li T, Wilson I, Gill C. Using electronic drug monitor feedback to improve adherence to antiretroviral therapy among HIV-positive patients in China. AIDS Behav. 2010;14:580–9. doi: 10.1007/s10461-009-9615-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Bruin M, Hospers HJ, van Breukelen GJ, Kok G, Koevoets WM, Prins JM. Electronic monitoring-based counseling to enhance adherence among HIV-infected patients: a randomized controlled trial. Health Psychol. 2010;29:421–8. doi: 10.1037/a0020335. [DOI] [PubMed] [Google Scholar]
- 25.Rosen M Dieckhaus K, McMahon T, Valdes B, Petry N, Cramer J, Rounsaville B. Improved adherence with contingency management. AIDS Patient Care STDS. 2007;21:30–40. doi: 10.1089/apc.2006.0028. [DOI] [PubMed] [Google Scholar]
- 26.Fisher W, Fisher J. A general social psychological model for changing AIDS risk behavior. In: Pryor J, Reeder G, editors. The Social Psychology of HIV infection. Erlbaum; Hillsdale, NJ: 1993. pp. 127–153. [Google Scholar]
- 27.Banderas J, Thomson D, Gerkovich M, Carruth T, Pinkston M, Williams K, Martinez D, Clark K, Goggin K. Standard Care Assessment in ART Adherence Research. The 5th International Conference on HIV Treatment Adherence; April 2010. [Google Scholar]
- 28.Wagner G, Remien R, Dolezal C, Carballo-Dieguez A. Correlates of adherence to combination antiretroviral therapy among HIV+ members of HIV mixed status couples. AIDS Care. 2002;14:105–9. doi: 10.1080/09540120220097973. [DOI] [PubMed] [Google Scholar]
- 29.Potchoo Y, Tchamdja K, Balogou A, Pitche V, Guissou I, Kassang E. Knowledge and adherence to antiretroviral therapy among adult people living with HIV/AIDS treated in the health care centers of the association “Espoir Vie Togo” in Togo, West Africa. BMC Clin Pharmacol. 2010;10:11. doi: 10.1186/1472-6904-10-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Miller L, Liu H, Hays R, Golin C, Ye A, Beck K, Kaplan A, Wenger N. Knowledge of Antiretroviral Regimen Dosing and Adherence: A Longitudinal Study. Clin Infect Dis. 2003;36:514–518. doi: 10.1086/367857. [DOI] [PubMed] [Google Scholar]
- 31.Goggin K, Gerkovich M, Williams K, Banderas J, Catley D, Berkley-Patton J, Stanford J, Neville S, Kumar V, Bamberger D, Clough L. A RCT examining the efficacy of motivational counseling with observed therapy for ART adherence. In press. [DOI] [PMC free article] [PubMed]
- 32.Keiser P, Nassar N, Kvanli M, Turner D, Smith J, Skiest D. Long-term impact of highly active antiretroviral therapy on HIV related health care costs. J Acquir Immune Defic Syndr. 2001;27:14–9. doi: 10.1097/00126334-200105010-00003. [DOI] [PubMed] [Google Scholar]
- 33.Theme discussed during conference session; Fifth International Conference on HIV Treatment Adherence Conference; Miami Beach, FL. May 24, 2010.2010. [Google Scholar]