Abstract
Objectives
To examine trends in use of long-acting reversible contraceptive (LARC) methods — the IUD and implant — and the extent to which these methods have replaced permanent sterilization and less-effective short-acting methods.
Design
We tabulated data from female survey respondents overall and by demographic subgroups. We performed t-tests of the differences in the proportions of female contraceptors using LARC in 2007 and 2009. We also looked at use of LARC, sterilization, other methods and no method among women at risk of unintended pregnancy.
Setting
Secondary analysis of the 2002 and 2006–2010 National Survey of Family Growth, an in-home, nationally representative survey of women 15–44.
Patients
All female respondents to the surveys.
Interventions
None.
Main outcome measures
Current use of LARC methods in 2009, and change in use from 2007.
Results
The proportion of contraceptors using LARC increased significantly from 2.4% in 2002 to 3.7% in 2007 and 8.5% in 2009. The increase occurred among women in almost every age, race, education and income group. Among women at risk of unintended pregnancy, increases in LARC use more than offset decreases in sterilization.
Conclusions
LARC methods (primarily IUDs) are contributing to an increase in contraceptive effectiveness in the United States.
INTRODUCTION
Unintended pregnancy is a seemingly intractable problem in the United States. The unintended pregnancy rate of 52 per 1,000 women of reproductive age in 2006 is high compared to many other industrialized countries, and about half of all pregnancies are unplanned (1). Many reproductive health researchers, advocates and clinical authorities have argued for increased use of long-acting reversible contraceptive (LARC) methods such as IUDs and implants among women of all ages as a way to reduce unintended pregnancy. LARC methods require little intervention on the part of the user and do not interfere with sex. The failure rate for IUDs is about equal to permanent sterilization, and the failure rate for the implant is actually lower (2). These are thus two of the most efficacious contraceptive methods available. They are also two of the most cost-effective methods currently available — IUDs can be used for up to 10 years and implants for up to three, allaying high upfront costs through long-term benefits to yield a much more economical method of preventing unintended pregnancy (3).
Unintended pregnancy rates are particularly high among sexually active teenagers and women 20–24 (1;4). This is in part due to changes in Americans’ sexual and relationship patterns. The median age at first marriage has shifted later, while timing of sexual initiation has changed little. As a result, the period between first sex and first birth has lengthened, exposing younger women to greater risk of unintended pregnancy and associated morbidities (5;6). However, long-acting methods have traditionally been seen as appropriate only for women who have completed their childbearing. For example, the Mirena IUD is not labeled for nulliparous women. These constraints have resulted in low use of these methods by young women in the past, and greater use of less-effective methods such as the pill and condom.
The lengthening of the typical time between first sex and first birth allows for a reframing of this period: Rather than focusing only on condoms and pills, the period before childbearing can now be considered suitable for long-acting methods. Reproductive health experts and clinical authorities have attempted to convey this point; guidelines from the American Congress of Obstetricians and Gynecologists cite these methods as “first-line” choices for all women and encourage their use by adolescents and young adults seeking longer-acting methods (7). Additionally, ACOG’s revised recommendations for less frequent Pap smear screenings (8), coupled with adolescents’ and young adults’ declining use of reproductive health services (9), suggest the need for methods that do not rely on frequent or repeat visits to a health care provider to ensure better reproductive health outcomes. Furthermore, the CDC’s recently released Medical Eligibility Criteria for Contraceptive Use (MEC) guidelines concluded after extensive scientific review that IUDs are safe and effective for younger and nulliparous women (10).
The above paragraphs describe one potential benefit of shifting to long-acting methods: increased contraceptive protection for those who shift away from less-effective methods. There is a second potential benefit for parous women who are not comfortable with sterilization. Women younger than 30 at the time of sterilization report especially high levels of post-sterilization regret, and are almost twice as likely to report regret as those older than 30 after adjustments for other factors (11). Greater use of long-acting methods among younger parous women could reduce the incidence of sterilization regret.
American women and men may be responding to this increased clinical focus as well as increased public awareness of these methods via advertising (2): Use of long-acting contraception increased from 2.4% of all method use in 2002 to 5.6% in 2006–08 (12). Still, LARC use remains relatively low among contraceptive users, and these methods may be particularly underutilized by young women. In this report, we analyze newly available data to see if this pattern has continued and to identify groups where the change has been the most prominent, and look at whether LARC is taking the place of sterilization or less-effective methods.
MATERIALS AND METHODS
We examined data from the 2002 and 2006–10 National Surveys of Family Growth (NSFG), nationally representative in-home surveys of women aged 15–44 and arguably the best available sources of information on U.S. contraceptive use. The NSFG also surveys men, but our analyses were limited to female respondents because their responses to questions about contraceptive use are considered to be more accurate. We previously published estimates using a partial version of this dataset, the 2006–08 NSFG. This earlier version contained data from interviews with 7,356 women between June 2006 and December 2008. Since that time, a complete version of the dataset has been released that contains 12,279 interviews conducted from June 2006 to June 2010. Unlike the previous version, the new data can be weighted into two 2-year periods: June 2006 to June (not December) 2008 and July 2008 to June 2010. The reference years represented by these two periods are 2007 and 2009, respectively, and the numbers of respondents were 5,851 and 6,428, respectively. In this paper, we present estimates for these two periods. IRB approval was not necessary for this secondary analysis of deidentified public-use NSFG data.
We defined long-acting methods as those that last longer than three months, which includes the IUD and implant but excludes the injectable. The NSFG does not distinguish between specific types of IUDs or implants. We tabulated the proportion of all contraceptive users who were currently using long-acting methods at the time of interview, for all women and by several demographic and reproductive health characteristics. We also looked at the proportion of long-acting method use that each of these two methods represented. We performed t-tests of the difference between the proportions reporting use of LARC in 2007 and 2009.
The analyses described above used all current contraceptors as the denominator. To see how changes in LARC use have affected method use overall, we conducted a second set of analyses on a larger sample: all women at risk of unintended pregnancy, including those who were not currently using any method. Among this group, we looked at how changes in LARC use related to use of nonreversible sterilization, other methods and no method over the same period, by age and parity. To do so, we performed t-tests comparing the proportions using each of these method groups in 2007 and 2009, which allowed us to compare the proportion using a specific method, as well as chi-square tests comparing the overall distributions in 2007 and 2009.
The NSFG distinguished between male and female sterilization, but did not distinguish between different types of female sterilization (e.g., tubal ligation vs. tubal occlusion). We report all those relying on female or male sterilization as one group. “Other” methods include all other hormonal and barrier methods as well as fertility awareness methods.
RESULTS
The proportion of all contraceptors using LARC increased significantly and substantially between 2007 (3.7%) and 2009 (8.5%, Table 1). As in the past, LARC use continued to be nearly synonymous with IUD use, although implant use approached 1% of contraceptors in 2009.
Table 1.
Percentage of current contraceptors who are currently using long-acting reversible contraception (LARC), including intrauterine devices (IUDs) and implants, by selected demographic characteristics, 2002, 2007 and 2009; and p-values from t-tests of the difference between 2007 and 2009
| Characteristic | 2002 | 2007 | 2009 | p-value '07 vs '09 |
|---|---|---|---|---|
| All | 2.4 | 3.7 | 8.5 | <.001 |
| IUD | 2.0 | 3.5 | 7.7 | <.001 |
| Implant | 0.4 | 0.1 | 0.8 | .003 |
| Age | ||||
| 15–19 | 0.3 | 1.5 | 4.5 | .08 |
| 15–17 | 0.6 | 0.8 | 0.6 | .75 |
| 18–19 | 0.0 | 1.9 | 6.6 | .007 |
| 20–24 | 1.9 | 4.2 | 8.3 | .02 |
| 25–29 | 4.8 | 5.5 | 11.4 | .004 |
| 30–34 | 3.8 | 4.4 | 10.3 | .003 |
| 35–39 | 1.7 | 3.0 | 10.8 | <.001 |
| 40–44 | 1.4 | 2.7 | 4.0 | .35 |
| Race/ethnicity | ||||
| Non-Hispanic white, single race | 1.6 | 3.4 | 8.3 | <.001 |
| Non-Hispanic black, single race | 1.5 | 2.3 | 9.2 | <.001 |
| Non-Hispanic other or multiple race | 2.9 | 4.2 | 9.2 | .08 |
| Hispanic | 7.1 | 5.5 | 8.5 | .02 |
| Born outside the U.S. | ||||
| No | 1.6 | 3.1 | 8.3 | <.001 |
| Yes | 7.5 | 6.9 | 9.5 | .20 |
| Relationship status | ||||
| Not married or cohabiting | 1.4 | 1.9 | 5.7 | .001 |
| Married | 3.1 | 5.1 | 10.2 | <.001 |
| Cohabiting | 2.5 | 2.2 | 10.2 | <.001 |
| Education | ||||
| Not high school graduate | 3.3 | 1.3 | 7.3 | <.001 |
| High school graduate or GED | 2.5 | 4.5 | 7.9 | .02 |
| Some college | 2.2 | 3.9 | 9.1 | .001 |
| College graduate | 2.1 | 4.0 | 9.2 | .002 |
| Employment | ||||
| Not working full-time | 2.4 | 4.0 | 9.2 | <.001 |
| Working full-time | 2.5 | 3.3 | 7.6 | <.001 |
| Income as a percent of poverty | ||||
| <100% | 4.7 | 3.4 | 8.1 | .003 |
| 100–199% | 3.0 | 4.1 | 9.6 | .001 |
| 200–299% | 1.9 | 4.1 | 7.7 | .01 |
| ≥300% | 1.5 | 3.3 | 8.3 | <.001 |
| Current insurance coverage | ||||
| Private | 1.9 | 3.1 | 7.1 | <.001 |
| Medicaid | 3.8 | 4.6 | 11.5 | .002 |
| Other | 1.0 | 5.5 | 8.1 | .49 |
| None | 4.5 | 4.7 | 10.6 | .001 |
| Religious affiliation | ||||
| None | 2.8 | 5.6 | 9.4 | .09 |
| Catholic | 3.3 | 3.6 | 7.6 | .005 |
| Protestant | 1.9 | 2.5 | 7.6 | <.001 |
| Other | 2.2 | 6.1 | 16.1 | .02 |
| Number of live births | ||||
| 0 | 0.6 | 0.7 | 2.1 | .03 |
| 1–2 | 3.4 | 6.0 | 15.0 | <.001 |
| 3 or more | 3.0 | 3.4 | 6.3 | .02 |
| Visited clinic in past 12 months for family planning services? | ||||
| No | 1.6 | 2.2 | 6.1 | <.001 |
| Yes | 4.4 | 7.1 | 13.8 | .002 |
| Unweighted N | 4619 | 3443 | 3861 | |
The proportion of contraceptors using LARC increased among almost every subgroup: Women of almost all ages, races, marital and educational statuses, income levels and religions saw significant increases. Increases were also observed for both women who had visited a family planning provider in the last year and women who had not, as well as for both parous and nulliparous women. The highest levels of use were seen among women aged 25–39, married and cohabiting women, women covered by Medicaid, and women with a religious affiliation other than Catholic or Protestant and those with no affiliation. Even among women aged 15–19, use of LARC tripled from 1.5% to 4.5%; virtually all of this increase occurred among women 18–19. Discrepancies by race and ethnicity seen in 2002 continued through 2007 but were largely eliminated by 2009. The latest figures also show no real differences by income level. Women born in the U.S. appear to be “catching up” to women born outside the U.S., who already had a higher level of use, likely due to a greater prevalence of these methods in Mexico.
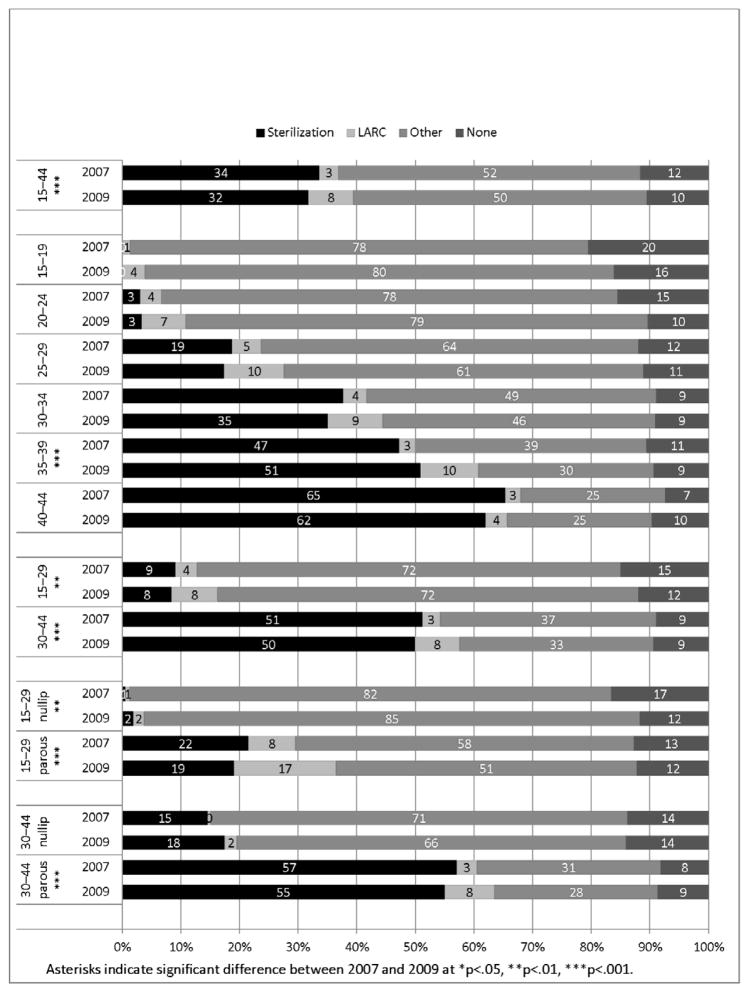
The increase in LARC use was only partially accounted for by decreases in the proportion of women who were sterilized (Figure 1). Among all women at risk of unintended pregnancy (including those who were not using any method), the proportion who were currently relying on sterilization declined from 34% to 32% between 2007 and 2009, but this change was not statistically significant, and was just a 2% decline compared to the 4% increase in LARC users. The proportion of at-risk women using any method increased by about 1% over the period, an increase that appears to be due to increased LARC use.
Figure 1.
Among all women at risk of unintended pregnancy, percent using each type of method, by age, 2007 and 2009
Among women under 30, negligible decreases in sterilization use were more than offset by increases in LARC use. This was also true for older women, although their level of sterilization use is much higher. For women under 25, we found increases in overall use, which appear to be driven by LARC. For most 5-year groups, there was an increase in the percentage of women using highly effective methods (either sterilization or LARC).
Analyses by age and parity together (Figure 1) echo Table 1 in showing that most of the increase in LARC use has taken place among women with at least one child. However, among parous women, the increase was greater among those under 30: The percentage who used LARC methods increased from 8% to 17%, while the percentage relying on sterilization declined from 58% to 51%. Parous women over 30 continued to rely more heavily on sterilization.
DISCUSSION
Use of LARC methods in the U.S. increased significantly between 2007 and 2009, a trend primarily driven by the use of IUDs, which have been on the market longer than the implant. The more popular levonorgestrel IUD (Mirena) was approved for use in 2000, and since being marketed in 2001 has seen a heavy direct-to-consumer advertising campaign. Although the copper IUD (ParaGard) has been available in the U.S. since 1988, its manufacturer’s marketing efforts have also increased in more recent years. Meanwhile, the implant available to U.S. consumers during this period, Implanon, was not approved until 2006, and may not have benefited from the same levels of awareness among American women.
Despite the increases reported here, LARC use in the U.S. is among the lowest of any developed country (13;14). Data for the mid-to-late 2000s indicate that these two methods are used by 15% of contraceptors worldwide, including 11% of British users, 23% of French users, 27% of Norwegian users and 41% of Chinese users. The large majority of this use is IUD use (15). U.S. rates of LARC use are much lower than our European counterparts likely because sterilization is more common in the U.S. than in many other developed nations (15), and because Mirena is not labeled for use by nulliparous women in the U.S. However, increases in LARC use would increase overall contraceptive effectiveness only to the extent that the methods substitute for less-effective methods rather than permanent sterilization. The increase in LARC use in 2009 more than offset the decrease in sterilization use for the same time period.
In the context of high national unintended pregnancy rates, the substantial increase in use of these highly effective, long-acting methods between 2007 and 2009 is a promising indicator, especially if this increase marks the beginning of a larger upward trend in LARC use. Increasing LARC utilization could diversify the overall method mix and present women with options that better meet their contraceptive needs at different life stages. Because unintended pregnancy rates are highest among women 18–24 and younger sexually active teens, the displacement of short-term methods by more effective LARC methods represents enhanced ability to prevent unintended pregnancy and/or delay childbearing among this group. Among nulliparous women, the method allows for effective contraception without preventing future fertility, and those with children avoid the potential for regret that some women experience after undergoing sterilization. As such, providers should rely on the CDC’s Medical Eligibility Criteria for Contraceptive Use guidelines to ensure that these methods are part of the method mix available to all women, and especially young and nulliparous women, who have so far had smaller increases in use of these methods.
Women who had experienced 1–2 live births, and particularly those under 30, saw some of the largest increases in LARC use in 2009, which may indicate a provider-level bias for LARC methods toward women who have already reached their fertility goals and towards cohabiting and married women, who are more likely to be monogamous. However, older women may also benefit from the increased focus on LARC as simpler and safer than sterilization, without the risk of regret. For women aged 35–39, who may have experienced a compression of their childbearing years into a later and shorter time period, thus reaching their fertility goals as they near the end of their fecund period, the increased use of both LARC and sterilization underscores the deliberateness of women’s family planning decisions and need for a variety of effective methods at all ages.
When used for their full 3–10 year term, LARC methods offer exceedingly economical options for preventing unintended pregnancy. The high level of LARC use among women on Medicaid (16) suggests that women will make use of these methods if they can afford them. Insurance plans should facilitate access to these methods, and in fact, a provision of the Affordable Care Act requires most plans, starting in August 2012, to cover the full range of contraceptive methods, including LARC, with no patient cost-sharing. This requirement could eliminate the economic barriers for many women who might be interested in using LARC. Public education efforts should highlight these methods’ safety and efficacy, as established by a substantial body of evidence, in order to ensure “mindshare” — a willingness to consider these methods along with condoms, pills and other choices — among women and men of all ages. Although no method is right for every woman or couple, increased use of LARC methods could enable more American women to have a method that best fits their reproductive goals.
Acknowledgments
The authors thank David Hubacher and Susheela Singh for reviewing and commenting on this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Lawrence B. Finer, Guttmacher Institute
Jenna Jerman, Guttmacher Institute
Megan L. Kavanaugh, Guttmacher Institute
Reference List
- 1.Finer LB, Zolna M. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;85:478–85. doi: 10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hatcher RA, Trussell J, Nelson AL, Cates W, Jr, Stewart FH, Kowal D. Contraceptive Technology. 19. New York: Ardent Media; 2007. [Google Scholar]
- 3.Trussell J, Lalla A, Doan Q, Reyes E, Pinto L, Gricar J. Cost-effectiveness of contraceptives in the United States. Contraception. 2009 Jan 1;79:5–14. doi: 10.1016/j.contraception.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Finer LB. Unintended pregnancy among U.S. adolescents: accounting for sexual activity. J Adolesc Health. 2010;47:312–4. doi: 10.1016/j.jadohealth.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. [Accessed January 19, 2012.];Unintended pregnancy prevention. Available at: http://www.cdcgov/reproductivehealth/unintendedpregnancy/
- 6.Centers for Disease Control and Prevention. Prepregnancy contraceptive use among teens with unintended pregnancies resulting in live births — Pregnancy Risk Assessment Monitoring System (PRAMS), 2004–2008. MMWR. 2012 Jan 20;61:25–9. [PubMed] [Google Scholar]
- 7.ACOG. ACOG practice bulletin No. 59: Intrauterine device. Obstet Gynecol. 2005 Jan;105:223–32. doi: 10.1097/00006250-200501000-00060. [DOI] [PubMed] [Google Scholar]
- 8.ACOG. ACOG practice bulletin No. 109: Cervical cytology screening. Obstet Gynecol. 2009 Dec 1;114:1409–20. doi: 10.1097/AOG.0b013e3181c6f8a4. [DOI] [PubMed] [Google Scholar]
- 9.Hall KS, Moreau C, Trussell J. Determinants and disparities in reproductive health service use among adolescent and young adult women in the United States, 2002–2008. Am J Public Health. 2012;102:359–67. doi: 10.2105/AJPH.2011.300380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. U.S. medical eligibility criteria for contraceptive use, 2010. MMWR. 2010 Jun 18;59:52–63. Available from: URL: http://www.cdc.gov/mmwr/pdf/rr/rr5904.pdf. [Google Scholar]
- 11.Hillis SD, Marchbanks PA, Tylor LR, Peterson HB. Poststerilization regret: findings from the United States Collaborative Review of Sterilization. Obstet Gynecol. 1999;93:889–95. doi: 10.1016/s0029-7844(98)00539-0. [DOI] [PubMed] [Google Scholar]
- 12.Kavanaugh ML, Jerman J, Hubacher D, Kost K, Finer LB. Characteristics of women in the United States who use long-acting reversible contraceptive methods. Obstet Gynecol. 2011 Jun;117:1349–57. doi: 10.1097/AOG.0b013e31821c47c9. [DOI] [PubMed] [Google Scholar]
- 13.Clifton D, Kaneda T, Ashford L. [Accessed January 19, 2012.];Family planning worldwide 2008 data sheet. Available at: http://www.prb.org/pdf08/fpds08.pdf.
- 14.Hubacher D. The checkered history and bright future of intrauterine contraception in the United States. Perspect Sex Reprod Health. 2002;34:98–103. [PubMed] [Google Scholar]
- 15.United Nations - Department of Economic and Social Information and Policy Analysis PD. [Accessed January 19, 2012.];World contraceptive use. 2011 Available at http://www.un.org/esa/population/publications/contraceptive2011/wallchart_front.pdf.
- 16.Kavanaugh ML, Jerman J, Hubacher D, Kost K, Finer LB. Characteristics of women in the United States who use long-acting reversible contraceptive methods. Obstet Gynecol. 2011 Jun;117:1349–57. doi: 10.1097/AOG.0b013e31821c47c9. [DOI] [PubMed] [Google Scholar]