Abstract
Primary, or transmitted, HIV antiretroviral resistance is an ongoing concern despite continuing development of new antiretroviral therapies. We examined HIV surveillance data, including both patient demographic characteristics and laboratory data, combined with HIV genotypic test results to evaluate the comprehensiveness of drug resistance surveillance, prevalence of primary drug resistance, and impact, if any, of primary resistance on population-based virological outcomes. The King County, WA Variant, Atypical, and Resistant HIV Surveillance (VARHS) system increased coverage of eligible genotypic testing – within three months of an HIV diagnosis among antiretroviral naïve individuals -- from – 15% in 2003 to 69% in 2010. VARHS under-represented females, Blacks, Native Americans, and injection drug users. Primary drug resistance was more common among males, individuals aged 20 – 29 years, men who had sex with men, and individuals with an initial CD4+ lymphocyte count of 200 cells/µL and higher. High level resistance to two or three antiretroviral classes declined over time. Over 90% of sequences were HIV-1 subtype B. The proportion of individuals with a most recent viral load (closest to April 2011) that was undetectable (<50 copies/mL) was not statistically significantly associated with primary drug resistance. This was true for both number and type of antiretroviral drug class; although small numbers of specimens with drug resistance may have limited our statistical power. In summary, although we found disparities in testing coverage and prevalence of drug resistance, we were unable to detect a significantly deleterious impact of primary drug resistance based on a most recent viral load.
Keywords: HIV-1, HIV transmitted drug resistance, HIV drug resistance surveillance, HIV viral load.
INTRODUCTION
Although the introduction of combination antiretroviral (ARV) therapy has been associated with marked decreases in HIV-related morbidity and mortality [1,2], the ongoing development and forward transmission of HIV-specific antiretroviral resistance is an increasing concern. Primary, or transmitted, HIV drug resistance is defined as an initial infection with a strain of HIV already resistant to one or more HIV-specific antiretrovirals [3]. Primary resistance occurs in about 15% of new infections in the U.S. [4]. Some primary resistance strains persist over time, other resistant strains may revert to wild-type virus [5-7]. Primary ARV drug resistance may be associated with adverse outcomes, or, paradoxically, with reduced viral fitness; certainly drug resistance makes HIV treatment more complicated and potentially more costly [8-14].
To better manage individuals with primary resistance, and increase the likelihood of detecting minority resistant strains, drug resistance testing in patients newly diagnosed with HIV-1 is recommended for all patients initiating HIV-1 care regardless of ARV commencement [15]. With the development of new antiretroviral therapies, including new classes of antiretrovirals, and refinement of antiretroviral usage (therapy including three or more drugs and two or more drug classes being the current norm), it is important to monitor the prevalence of and outcomes associated with primary drug resistance on a community level. To our knowledge, there have been no prior presentations of population-based outcomes of primary drug resistance in the modern highly active antiretroviral (HAART) era, including the proportions of individuals who achieve undetectable plasma virus level based on resistance status.
Monitoring population-wide rather than individual or cohort-specific outcomes is a key public health function. Recently mean community viral loads have been presented as a way to monitor the population-wide impact of successful viral load therapy and tie successful therapy to a reduction in forward viral transmission [16]. Rather than base our monitoring of viral load on population means, to reduce the impact of an asymmetrical distribution skewed towards outlying high viral loads, we present proportions of sub-populations with undetectable virus at a most recent viral load test.
King County is the metropolitan area encompassing Seattle and the home of roughly one-third of Washington State residents, but two-thirds of Washington State HIV cases. To examine the prevalence of, and outcomes associated with primary drug resistance, we conducted analyses of HIV-1 genotypic test results linked to HIV/AIDS case surveillance data in King County, Washington State. Our specific aims included (1) describing demographic and clinical factors associated with genotypic resistance testing and the prevalence of primary resistance; and (2) examining correlations between later viral outcomes (undetectable recent HIV-1 viral load) HIV-1 subtypes and antiretroviral drug resistance detected near the time of HIV diagnosis.
MATERIALS AND METHODOLOGY
We included individuals who were newly diagnosed with HIV (including concurrent AIDS) from 2003 through 2010 and who were residents of King County, WA, at time of HIV/AIDS diagnosis and reported to Public Health – Seattle & King County’s (PH) HIV/AIDS reporting system (HARS) as of March 28, 2011. Drug resistance surveillance was conducted among antiretroviral naïve individuals first as a pilot and then through an ongoing Centers for Disease Control and Prevention (CDC) protocol called Variant, Atypical, and Resistant HIV Surveillance (VARHS). VARHS uses remnant HIV diagnostic sera from participating laboratories to conduct genotypic drug resistance testing, and increasingly has also relied on collection of sequence data submitted by laboratories conducting drug resistance testing ordered by medical providers in the community [4,17]. Remnant sera and genotypes conducted in a clinical setting must be from a specimen collected within three months of documented HIV diagnosis in order to be included in VARHS. Eligible genotypic testing is also referred to as “early”. Both remnant sera and genotypic sequence data from community providers came from a mix of public and private clinics. The results of genotypic tests performed by VARHS were always returned to the HIV testing facility and, to the greatest extent possible, also to a primary care provider if the testing facility did not provide primary care.
Genotypic tests on remnant diagnostic sera were conducted at the University of Washington and at Stanford Laboratory. Genotypic test sequence data are reportable in King County and are currently reported by five laboratories (University of Washington, LabCorp, Quest, Specialty, and ARUP). The pilot project was originally approved by local and CDC Institutional Review Boards (IRB); however VARHS, as an exempt public health surveillance activity, was later given a non-research determination and IRB review was discontinued.
To evaluate population-based coverage of drug resistance surveillance, we compared all newly diagnosed HIV cases from HARS who did and did not have a genotypic test result from a test conducted within 90 days of HIV diagnosis and reported to PH. We compared demographic characteristics (gender, race/ethnicity, age, HIV transmission risk category, homeless status) and clinical characteristics (CD4 and AIDS status at the time of diagnosis).
Unless specified otherwise, we defined drug resistance as infection with a strain of HIV with one or more pre-selected antiretroviral resistance associated mutations important to surveillance as defined by CDC VARHS staff [4,18] or high level resistance of clinical importance as defined by the Stanford laboratory database [19]. High level resistance indicates that patients would be unlikely to have a strong virologic response to the drug or that the mutation pattern is similar to virus with the highest in vitro resistance. The CDC VARHS staff resistance-associated mutations were selected to exclude common polymorphisms and were optimized to fit the predominantly subtype B U.S. epidemic. We added high level resistance of clinical significance because infection with subtypes other than B were more common in King County relative to other VARHS sites [4] and also to optimize the number of sequences included where we had the Stanford interpretation but not the CDC interpretation. We also looked at individuals with high-level drug resistance per the Stanford interpretation independently of the CDC VARHS definition, as multiclass drug resistance is typically defined as high level resistance to antiretrovirals in two or more antiretroviral drug classes. We compared demographic and clinical characteristics of individuals with and without resistance to antiretrovirals in any of these classes: non-nucleoside reverse transcriptase inhibitors (NNRTI), nucleoside/necleotide reverse transcriptase inhibitors (NRTI), and protease inhibitors (PI). Transmitted drug resistance thus only refers to these three classes and none of the newer classes of antiretrovirals (i.e. fusion, entry, and integrase inhibitors).
Among individuals with and without primary drug resistance, we compared the proportion whose most recent viral load (plasma HIV-1 viral load in RNA copies/mL) was undetectable versus detected. Viral loads were plasma viral loads reported routinely to HARS. Since March 2006 all HIV viral loads have been reportable in Washington State whether or not there was detectable virus. “Most recent” viral loads were those closest to data analyses in April 2011. Five percent of the most recent viral loads were from the period before undetectable viral load reporting was required, yet reporting of undetectable results was occurring as 11% of most recent viral loads prior to March 2006 were undetectable. Because the threshold of detection may have changed over the course of the project with newer more sensitive tests, viral loads under 50 copies/mL were considered undetectable. In part because antiretroviral initiation data are not routinely collected by VARHS or HARS, we present data stratified by nadir CD4+ lymphocyte count (CD4) in categories of 0-349, 350-499, and 500+ cells. These categories correspond to levels of immunosuppression where antiretrovirals would have been uniformly recommended, increasingly recommended, and optional (respectively) throughout the observation period. Statistical analyses included Chi square (Χ2) and Chi square for trend (Χ2trend) tests calculated using SAS version 9.2 (SAS Institute Inc, Cary, NC, U.S.) and EpiInfo version 6.04 (CDC, Atlanta, GA, U.S. in collaboration with World Health Organization, Geneva, Switzerland).
RESULTS
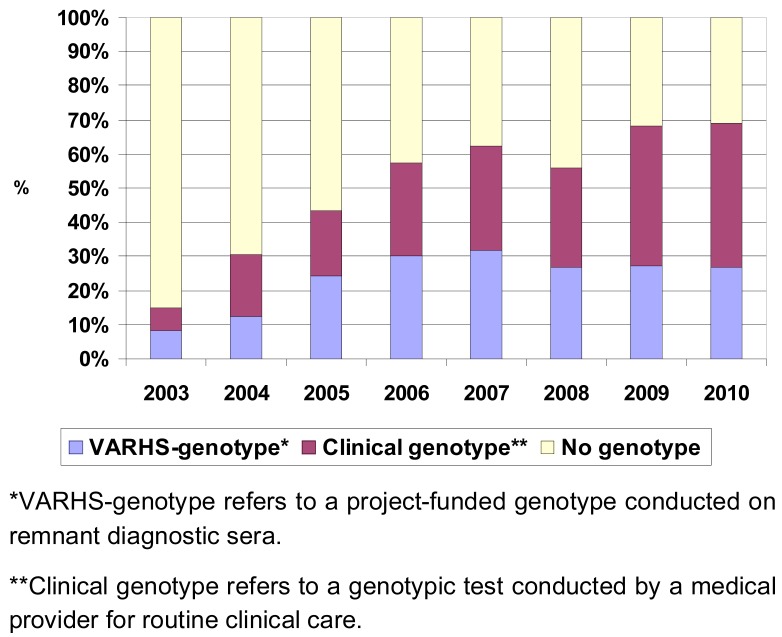
Between 2003 and 2010, Public Health–Seattle & King County obtained an early HIV genotype sequence (within three months of HIV diagnosis) for 1,303 King County residents; this represents 49% of the 2,643 HIV diagnoses reported over the period. The mean length of time from an HIV diagnosis was 0.5 months with an interquartile range of 0 to 1.0 month. Both overall VARHS coverage and the proportion of genotypic test results which were reported from clinical practice have increased since 2003 (Fig. 1). In recent years, nearly 70% of newly-diagnosed HIV cases in King County had a VARHS-eligible genotype. Currently, about 60% of the genotypic test results included in VARHS are reported by laboratories based on testing in routine clinical practice; the other 40% are genotypic tests conducted by VARHS on remnant sera. Subgroups that were most likely to have an early genotype included in VARHS were men who had sex with men (MSM) (including injection drug using MSM); subgroups less likely to have an early genotype were females, Blacks, Native Americans, injection drug users (Table 1). The mean follow time from HIV diagnosis to a most recent viral load test was 39.3 months with an interquartile range of 12.9 to 63.0 months.
Fig. (1).
Proportion of cases with genotype obtained within 3 months of HIV diagnosis. Variant, Atypical, and Resistant HIV Surveillance, King County, WA, USA 2003 – 2010.
Table 1.
Demographic and Clinical Characteristics of Individuals by Early Genotype Status and by Presence of Primary Resistance. Variant, Atypical, and Resistant HIV Surveillance, King County, WA, USA 2003 - 2010
| Characteristics* | Have an Earlyb
Genotypic Test Result |
X2 or X2trend p-Value | Evidence of Drug Resistance-Associated Mutationsc |
X2 or X2trend p-Value | |||
|---|---|---|---|---|---|---|---|
| Yes No. (%) |
No No. (%) |
Yes No. (%) |
No No. (%) |
||||
| Gender | Female | 137 (43) | 182 (57) | P=.015 | 12 (9) | 125 (91) | P=.003 |
| Male | 1166 (50) | 1158 (50) | 222 (19) | 944 (81) | |||
| Age in years at HIV diagnosis | <20 | 17 (41) | 24 (59) | P=.089 X2trend p=.181 |
1 (6) | 16 (94) | P<.0001 X2trend p<.0001 |
| 20-29 | 340 (54) | 287 (46) | 90 (26) | 250 (74) | |||
| 30-39 | 447 (47) | 496 (53) | 72 (16) | 375 (84) | |||
| 40-49 | 334 (48) | 364 (52) | 56 (17) | 278 (83) | |||
| 50-59 | 134 (50) | 132 (50) | 15 (11) | 119 (89) | |||
| 60+ | 31 (46) | 37 (54) | 0 (0) | 31 (100) | |||
| Race/ethnicitya | White | 786 (51) | 753 (49) | P=.013 | 156 (20) | 630 (80) | P=.117 |
| Black | 225 (43) | 299 (57) | 29 (13) | 196 (87) | |||
| Hispanic | 186 (52) | 171 (48) | 28 (15) | 158 (85) | |||
| Asian/Pacific Islander | 66 (50) | 67 (50) | 14 (21) | 52 (79) | |||
| Native American | 10 (38) | 16 (62) | 2 (20) | 8 (80) | |||
| HIV risk category | Men who had sex with men (MSM) | 870 (52) | 819 (48) | P<.0001 | 189 (22) | 681 (78) | P<.0001 |
| Injection drug user (IDU) | 48 (41) | 70 (59) | 4 (8) | 44 (92) | |||
| MSM-IDU | 118 (58) | 84 (42) | 17 (14) | 101 (86) | |||
| Other | 136 (43) | 177 (57) | 16 (12) | 120 (88) | |||
| Unknown | 131 (41) | 190 (59) | 8 (6) | 123 (94) | |||
| Homeless at HIV diagnosis | Yes | 58 (61) | 37 (39) | P=.020 | 4 (7) | 54 (93) | P=.025 |
| No | 1245 (49) | 1303 (51) | 230 (18) | 1015 (82) | |||
| Initial CD4 count | < 200 cells/µL | 321 (47) | 367 (53) | P<.0001 X2trend p=.230 |
33 (10) | 288 (90) | P=.001 X2trend P<.0001 |
| 200-349 | 259 (55) | 216 (45) | 51 (20) | 208 (80) | |||
| 350-499 | 268 (50) | 265 (50) | 52 (19) | 216 (81) | |||
| 500 + | 406 (51) | 390 (49) | 86 (21) | 320 (79) | |||
| Unknown | 49 (32) | 102 (68) | 12 (24) | 37 (76) | |||
| AIDS at HIV diagnosis | Yes | 360 (52) | 332 (48) | P=.095 | 45 (12) | 315 (88) | P=.002 |
| No | 943 (48) | 1008 (52) | 189 (20) | 754 (80) | |||
| Initial viral load | 0-49 | 30 (23) | 102 (77) | P<.0001 X2trend P <.0001 |
2 (7) | 28 (93) | P=.005 X2trend P=.072 |
| 50-999 | 72 (38) | 119 (62) | 13 (18) | 59 (82) | |||
| 1,000-9,999 | 200 (49) | 209 (51) | 49 (24) | 151 (76) | |||
| 10,000-99,999 | 469 (57) | 356 (43) | 89 (19) | 380 (81) | |||
| 100,000+ | 459 (57) | 353 (43) | 62 (14) | 397 (86) | |||
| Missing | 73 (35) | 128 (65) | 19 (26) | 54 (74) | |||
| Overall | 1303 (49) | 1340 (51) | 234 (18) | 1069 (82) | |||
Unknown categories are included in the table when representing 5% or more of the total but are not included in the statistical comparisons.
White, Black, Asian/Pacific Islander, and Native American groups are non-Hispanic.
Early or eligible genotypic result refers to a genotypic test result within three months of an HIV diagnosis.
Among those with an early genotypic test result.
Sequences were analyzed for resistance-associated mutations to three classes of antiretrovirals: NNRTIs, NRTIs, and PIs. A total of 234 (18% of 1,303) individuals had primary HIV drug resistance detected within three months of their HIV diagnosis. Ninety-three percent were classified as resistant based on resistance-associated mutations from the CDC definition and 7% were added based on high level clinical resistance from the Stanford database. Characteristics of individuals with and without primary drug resistance (Table 1) indicate transmitted drug resistance was more common in: males relative to females, individuals diagnosed with HIV between 20 and 29 years of age versus younger or older people, MSM versus other transmission risk groups, people who were not homeless at the time of an HIV diagnosis relative to homeless individuals, and individuals whose initial CD4+ lymphocyte count was above 199 cells per µL versus those with lower initial CD4 counts.
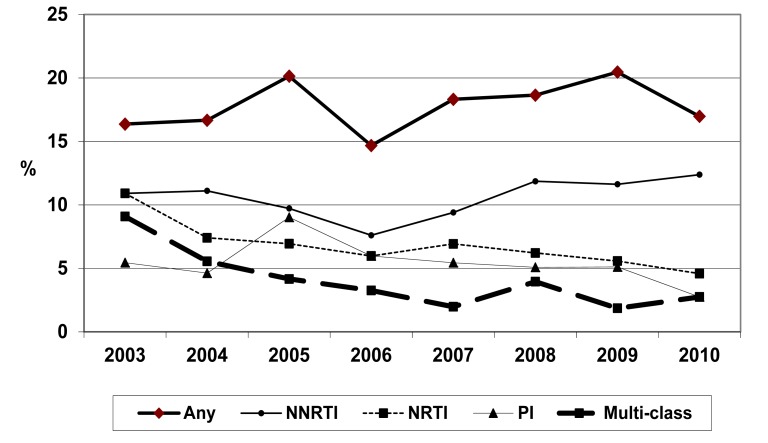
Trends in overall and antiretroviral class-specific primary drug resistance are presented in Fig. (2a). Over the eight years, 2003-2010, there was a decline in primary resistance to two or more classes (Χ2trend P value = .02). Among King County residents diagnosed with HIV between 2008 and 2010, 17%-20% had any resistance to one or more antiretroviral class. Resistance to NNRTIs was most common (12% in the past 3 years), followed by resistance to NRTIs (5-6%), and PIs (3-5%). Between two and four percent had resistance to two or three drug classes.
Fig. (2a).
Trends in OVERALL antiretroviral resistance by drug class. Variant, Atypical, and Resistant HIV Surveillance, King County, WA, USA 2003 – 2010.
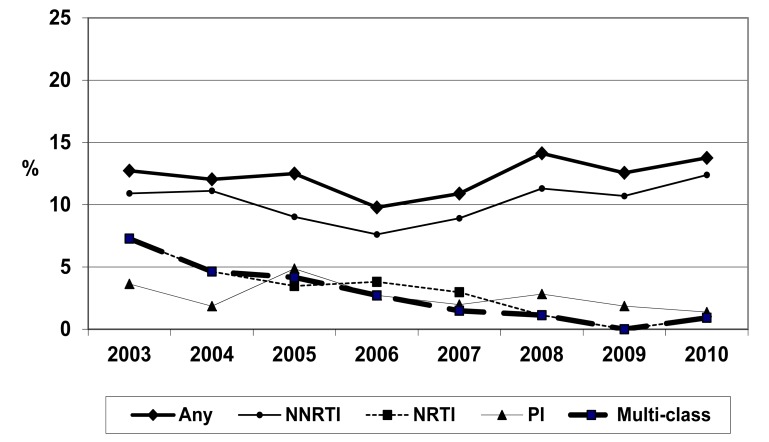
The proportion of newly-diagnosed individuals with high-level resistance was also examined over time (Fig. 2b). High level resistance roughly followed the trends of overall resistance patterns based on presence of CDC/VARHS-defined mutations important to surveillance [4], albeit at slightly lower prevalence levels. In the three most recent years, 2008-2010, 13%-14% had strains had high-level resistance to one or more drug classes, 11%-12% had high level NNRTI resistance, 1-3% had high-level PI resistance and 0-1% had high-level resistance to NRTIs. Less than 1% of sequences had high-level resistance to antiretrovirals in two or more drug classes (multi-class drug resistance). Both multi-class resistance (p<.0001) and high level NRTI resistance (p<.0001) had statistically significant decreases over time by Χ2trend testing. There was no statistically significant increase in the proportion of individuals with high level drug resistance in aggregate. If limited to 2006 through 2010, the increases in NNRTI resistance, both overall (Fig. 2a) and high level (Fig. 2b) are of borderline statistical significance (p=.092 and p=.096 respectively).
Fig. (2b).
Trends in HIGH-LEVEL antiretroviral resistance by drug class. Variant, Atypical, and Resistant HIV Surveillance, King County, WA, USA 2003 – 2010.
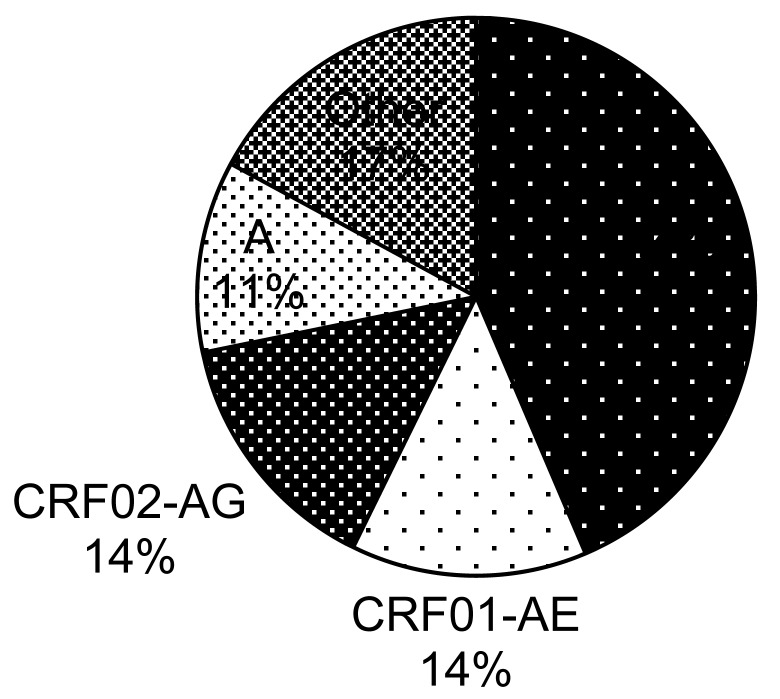
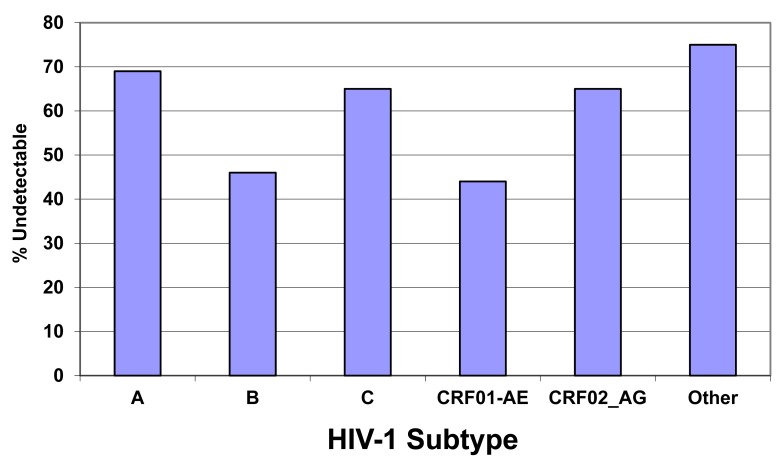
Genotype sequences were also examined for HIV-1 subtype. Overall, 91% of VARHS-eligible King County sequences 2003-2010 were subtype B and 9% were other subtypes. The distribution of these subtypes is presented in Fig. (3a) with subtype C being the most common (44% of 121 non-B subtypes). Individuals infected with subtypes B and CRF01-AE were less likely to have a most recent viral load of undetectable (44-46%) relative to individuals infected with other subtypes (65-75%, p < .001) (Fig. 3b).
Fig. (3a).
HIV-1 subtypes among 121 (9.3% of 1,303 total) Non-B subtype HIV-1 sequences. Variant, Atypical, and Resistant HIV Surveillance, King County, WA, USA 2003 – 2010.
Fig. (3b).
Proportion of individuals with a most recent viral load of undetectable or < 50 copies per mL by subtype. Variant, Atypical, and Resistant HIV Surveillance, King County, WA, USA 2003 – 2010.
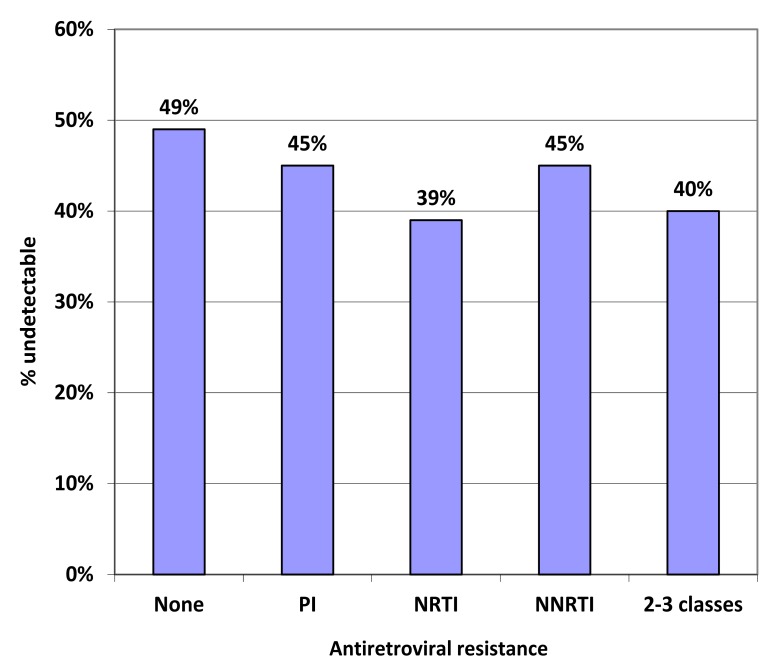
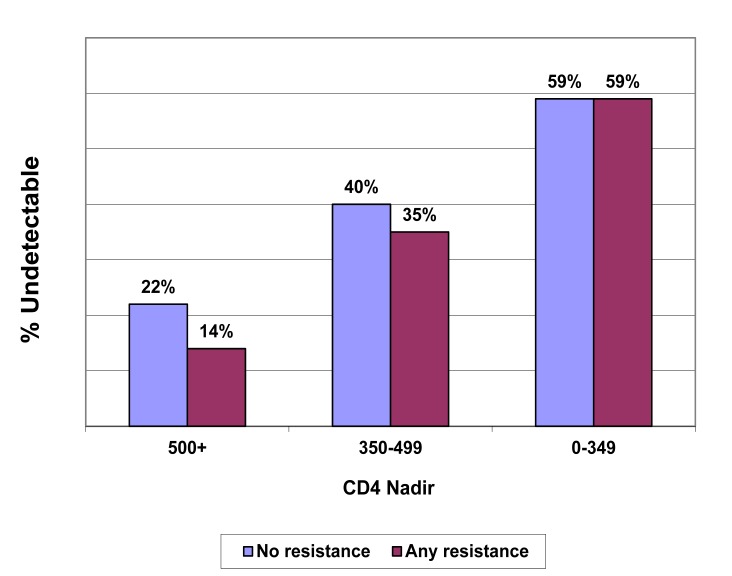
The proportion of individuals with a most recent viral load that was undetectable (or less than 50 viral copies per mL plasma) decreased –albeit not statistically significantly -- with increasing numbers of classes of drug resistance. We examined viral load status by class of antiretroviral resistance (Fig. 4) and found a lower proportion of those with resistance to NRTI (39%) had undetectable viral loads at their most recent test relative to individuals without NRTI resistance, although this difference was only of borderline statistical significance (p=.097). Among individuals with no transmitted drug resistance, 49% had undetectable plasma viral load at their most recent test, with resistance to one class, 45% were undetectable, and among those with two or three classes of resistance, 40% were undetectable. In Fig. (5), the proportion of individuals with undetectable virus is stratified by primary resistance status and nadir CD4 count (0-349, 350-499, and 500+ cells/µL). Those with the lowest nadir CD4 counts (0 – 349), which may be a proxy for initiation of antiretrovirals, were most likely to achieve undetectable status at a most recent viral load, regardless of the presence of primary resistance. Among those with higher nadir CD4 counts (350 – 499 and 500+) the presence of primary drug resistance lowered the proportion with a most recent viral load that was undetectable, but these differences did not achieve statistical significance.
Fig. (4).
Proportion of individuals with an undetectable plasma viral load according to class of HIV-1 antiretroviral drug resistance among those with a genoptypic HIV-1 resistance test within three months of an HIV diagnosis. Variant, Atypical, and Resistant HIV Surveillance, King County, WA, USA 2003 – 2010. PI = protease inhibitors; NRTI = nucleoside reverse transcriptase inhibitors; NNRTI = non-nucleoside reverse transcription inhibitors.
Fig. (5).
Percent of HIV-infected individuals with a most recent plasma viral load of undetectable among those with and without resistant virus within three months of HIV, by nadir CD4 count. Variant, Atypical, and Resistant HIV Surveillance, King County, WA, USA 2003 – 2010.
DISCUSSION
VARHS is a population-based project with a goal of obtaining a genotype for all HIV-infected people at or near the time of their HIV diagnosis. In 2003, when the project commenced, 15% of individuals with newly diagnosed HIV had a genotypic test result included. By 2010 nearly 70% of newly diagnosed cases had VARHS-eligible genotypes. Increases in antiretroviral resistance testing with stable or decreasing prevalence of resistance have been previously reported within other cohorts [20-23]. Primary or transmitted antiretroviral resistance was present in 18% of people newly diagnosed with HIV in King County 2003 through 2010, and transmitted high level multi-class drug resistance remains uncommon, occurring in less than 2% of people newly diagnosed with HIV. Non-B subtypes were present in 9% of individuals, predominantly subtypes C, CRF01, and CRF02.
We examined a most recent viral load of undetectable or less than 50 copies as an outcome among HIV-infected individuals with and without primary antiretroviral resistance. We found that regardless of resistance status, a similar proportion of individuals achieved an undetectable viral load within nadir CD4 categories. This was especially true among individuals with a CD4 nadir of <350 cells/µL where 59% of individuals had an undetectable viral load whether primary resistance was present or not. This finding is consistent with medical providers delaying initiation of antiretrovirals among individuals with primary resistance at higher CD4 counts and ensuring that antiretroviral regimens used are appropriate to each individual’s strain. Although not statistically significant, partially due to small numbers, the proportion of individuals with two or more classes of drug resistance with undetectable viral load at their most recent test (40%) was lower than those with no primary resistance (49%).
Adverse outcomes that have been linked to primary HIV resistance previously include a more rapid CD4-positive T-lymphocyte (CD4) decline early in the course of disease [8, 12] and a longer interval to viral suppression following antiretroviral initiation [24, 25]. These deleterious outcomes may be reduced when providers have knowledge of resistance and expert advice in tailoring of regimens for individuals with drug resistance [26, 27] and due to the availability newer classes of antiretrovirals. Accordingly, despite the presence of transmitted resistance, researchers have found equivalent outcomes based on viral suppression [28, 29]. Neither viral suppression nor CD4 increase was statistically associated with transmitted drug resistance in a European cohort (EuroSIDA) comprised of nearly 300 individuals examined 6-12 months after starting antiretrovirals [28]. In a larger cohort (EuroCoord-CHAIN, which includes EuroSIDA) of close to 10,000 individuals, transmitted resistance was not significantly associated with viral suppression when a fully active antiretroviral regimen, especially a boosted PI regimen, was used[29]. Resistant strains of HIV may not be associated with accelerated disease progression if the viral fitness is compromised [11, 13].
The low sensitivity of standard consensus genotyping can be detrimental to studies of drug resistance [3]. If resistant species are present in fewer than 20% of the circulating viruses, they are unlikely to be detected. However genotypic testing is preferred over phenotypic testing as the former includes information about sentinel mutations that may rapidly lead to resistance under selective pressure of antiretroviral use. Another limitation of our project was the lack of data on antiretroviral commencement, as undetectable viral loads are primarily associated with antiretroviral usage and nadir CD4 is only a rough proxy for antiretroviral usage. Without data on commencement of antiretrovirals. we were unable examine outcomes prior to and following initiation of antiretrovirals. We were also unable to compare the numbers of antiretrovirals and/or drug classes patients may be using to achieve equivalent viral suppression in the presence of resistance. Other limitations focus on the use of surveillance data to collect exposures and outcomes. We were unable to determine, for example, how many viral load or CD4 tests or genotypic drug resistance tests might have been missing from the surveillance system, or did not link to the correct patient. A final limitation was a limited sample size which reduced our ability to examine smaller sub-populations, such as individuals with multiclass resistance, with a high level of statistical precision.
Despite these limitations, we present an innovative exploration of population-based virologic outcomes following surveillance for primary HIV drug resistance. The use of surveillance data to examine clinical outcomes can provide highly representative data at a relatively low cost. Although we found minimal impact of primary resistance on community-based most recent viral loads, the differences seen were in the expected direction (people with no transmitted drug resistance were more likely to have undetectable virus), and individuals with the most immunologic damage from HIV (nadir CD4 below 350) with primary HIV drug resistance appear to be able to realize the same level of antiretroviral benefits as those without primary resistance. Continued monitoring of primary resistance is needed to ensure providers conduct genotypic testing early in the course of HIV for all newly diagnosed individuals and to be alerted to future changes in the prevalence of primary resistance and atypical types of HIV-1.
CONCLUSION
When individuals newly diagnosed with HIV establish medical care, a genotypic HIV drug resistance test is recommended. Our surveillance indicates the tests are not always conducted soon (within three months) after HIV diagnosis, and that the testing and/or reporting is more complete in some populations (such as MSM) than others (women and injection drug users). Among individuals with early genotypic testing, men who have sex with men, and individuals age 20 to 29 years were more likely to have been infected with resistant virus. Multiclass drug resistance declined in King County between 2003 and 2010 and community viral outcomes (as measured by percent of recent viral loads that are undetectable) are equivalent among people with and without primary antiretroviral resistance.
ACKNOWLEDGEMENT
Declared none.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflicts of interest.
REFERENCES
- 1. Buchacz K, Baker RK, Palella FJ , Jr, et al. AIDS-defining opportunistic illnesses in US patients, 1994-2007: a cohort study. AIDS. 2010;24(10 ):1549–59. doi: 10.1097/QAD.0b013e32833a3967. [DOI] [PubMed] [Google Scholar]
- 2. Ray M, Logan R, Sterne JA, et al. The effect of combined antiretroviral therapy on the overall mortality of HIV-infected individuals. AIDS. 2010;24(1 ):123–37. doi: 10.1097/QAD.0b013e3283324283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Booth C. Geretti AM, editor. Transmitted resistance. Antiretroviral Resistance in Clinical Practice NCBI Bookshelf A service of the National Library of Medicine, National Institutes of Health London. 2006.
- 4. Wheeler WH, Ziebell RA, Zabina H, et al. Prevalence of transmitted drug resistance associated mutations and HIV-1 subtypes in new HIV-1 diagnoses, U.S.-2006. AIDS. 2010;24(8):1203–12. doi: 10.1097/QAD.0b013e3283388742. [DOI] [PubMed] [Google Scholar]
- 5. Delaugerre C, Morand-Joubert L, Chaix ML, et al. Persistence of multidrug-resistant HIV-1 without antiretroviral treatment 2 years after sexual transmission. Antivir Ther. 2004;9(3 ):415–21. [PubMed] [Google Scholar]
- 6. Leigh Brown AJ, Frost SD, Mathews WC, et al. Transmission fitness of drug-resistant human immunodeficiency virus and the prevalence of resistance in the antiretroviral-treated population. J Infect Dis. 2003;187(4 ):683–6. doi: 10.1086/367989. [DOI] [PubMed] [Google Scholar]
- 7. Pao D, Andrady U, Clarke J, et al. Long-term persistence of primary genotypic resistance after HIV-1 seroconversion. J Acquir Immune Defic Syndr. 2004;37(5 ):1570–3. doi: 10.1097/00126334-200412150-00006. [DOI] [PubMed] [Google Scholar]
- 8. Bhaskaran K, Pillay D, Walker AS, et al. Do patients who are infected with drug-resistant HIV have a different CD4 cell decline after seroconversion? An exploratory analysis in the UK Register of HIV Seroconverters. AIDS. 2004;18(10 ):1471–3. doi: 10.1097/01.aids.0000131341.45795.33. [DOI] [PubMed] [Google Scholar]
- 9. Grant RM, Hecht FM, Warmerdam M, et al. Time trends in primary HIV-1 drug resistance among recently infected persons. JAMA. 2002;288(2 ):181–8. doi: 10.1001/jama.288.2.181. [DOI] [PubMed] [Google Scholar]
- 10. Little SJ, Frost SD, Wong JK, et al. Persistence of transmitted drug resistance among subjects with primary human immunodeficiency virus infection. J Virol. 2008;82(11 ):5510–8. doi: 10.1128/JVI.02579-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Menzo S, Monachetti A, Balotta C, et al. Processivity and drug-dependence of HIV-1 protease: determinants of viral fitness in variants resistant to protease inhibitors. AIDS. 2003;17(5 ):663–71. doi: 10.1097/01.aids.0000050852.71999.5f. [DOI] [PubMed] [Google Scholar]
- 12. Pillay D, Bhaskaran K, Jurriaans S, et al. The impact of transmitted drug resistance on the natural history of HIV infection and response to first-line therapy. AIDS. 2006;20(1 ):21–8. doi: 10.1097/01.aids.0000196172.35056.b7. [DOI] [PubMed] [Google Scholar]
- 13. Zaccarelli M, Tozzi V, Perno CF, Antinori A. The challenge of antiretroviral-drug-resistant HIV: is there any possible clinical advantage? Curr HIV Res. 2004;2(3 ):283–92. doi: 10.2174/1570162043351192. [DOI] [PubMed] [Google Scholar]
- 14. Zaccarelli M, Tozzi V, Lorenzini P, et al. Multiple drug class-wide resistance associated with poorer survival after treatment failure in a cohort of HIV-infected patients. AIDS. 2005;19(10 ):1081–9. doi: 10.1097/01.aids.0000174455.01369.ad. [DOI] [PubMed] [Google Scholar]
- 15.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. 2011. Oct 1, pp. 1–166.
- 16. Das M, Chu PL, Santos GM, et al. Decreases in community viral load are accompanied by reductions in new HIV infections in San Francisco. PLoS One. 2010;5(6 ):e11068. doi: 10.1371/journal.pone.0011068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Markovitz AR, Thibault CS, Brandauer PW, Buskin SE. Primary antiretroviral drug resistance in newly human immunodeficiency virus-diagnosed individuals testing anonymously and confidentially. Microb Drug Resist. 2011;17:283–9. doi: 10.1089/mdr.2010.0066. [DOI] [PubMed] [Google Scholar]
- 18. Bennett DE, Camacho RJ, Otelea D, et al. Drug resistance mutations for surveillance of transmitted HIV-1 drug-resistance: 2009 update. PLoS One. 2009;4(3 ):e4724. doi: 10.1371/journal.pone.0004724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Shafer RW. Rationale and uses of a public HIV drug-resistance database. J Infect Dis. 2006;194(Suppl 1 ):S51–8. doi: 10.1086/505356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bracciale L, Colafigli M, Zazzi M, et al. Prevalence of transmitted HIV-1 drug resistance in HIV-1-infected patients in Italy: evolution over 12 years and predictors. J Antimicrob Chemother. 2009;64(3 ):607–15. doi: 10.1093/jac/dkp246. [DOI] [PubMed] [Google Scholar]
- 21. Buchacz K, Baker RK, Young B, Brooks JT. Changes in the use of HIV antiretroviral resistance testing in a large cohort of U.S. patients, 1999 to 2006. J Acquir Immune Defic Syndr. 2010;53(5 ):625–32. doi: 10.1097/QAI.0b013e3181bf1dd2. [DOI] [PubMed] [Google Scholar]
- 22. Mackie NE, Phillips AN, Kaye S, Booth C, Geretti AM. Antiretroviral drug resistance in HIV-1-infected patients with low-level viremia. J Infect Dis. 2010;201(9 ):1303–07. doi: 10.1086/651618. [DOI] [PubMed] [Google Scholar]
- 23. Russell JS, Chibo D, Kaye MB, et al. Prevalence of transmitted HIV drug resistance since the availability of highly active antiretroviral therapy. Commun Dis Intell. 2009;33(2 ):216–20. [PubMed] [Google Scholar]
- 24. Grant RM, Hecht FM, Warmerdam M, et al. Time trends in primary HIV-1 drug resistance among recently infected persons. JAMA. 2002;288(2 ):181–8. doi: 10.1001/jama.288.2.181. [DOI] [PubMed] [Google Scholar]
- 25. Little SJ, Holte S, Routy JP, et al. Antiretroviral-drug resistance among patients recently infected with HIV. N Engl J Med. 2002;347(6 ):385–94. doi: 10.1056/NEJMoa013552. [DOI] [PubMed] [Google Scholar]
- 26. Durant J, Clevenbergh P, Halfon P, et al. Drug-resistance genotyping in HIV-1 therapy: the VIRADAPT randomised controlled trial. Lancet. 1999;353(9171 ):2195–9. doi: 10.1016/s0140-6736(98)12291-2. [DOI] [PubMed] [Google Scholar]
- 27. Tural C, Ruiz L, Holtzer C, et al. Clinical utility of HIV-1 genotyping and expert advice: the Havana trial. AIDS. 2002;16:209–18. doi: 10.1097/00002030-200201250-00010. [DOI] [PubMed] [Google Scholar]
- 28. Bannister WP, Cozzi-Lepri A, Clotet B, et al. Transmitted drug resistant HIV-1 and association with virologic and CD4 cell count response to combination antiretroviral therapy in the EuroSIDA Study. J Acquir Immune Defic Syndr. 2008;48:324–33. doi: 10.1097/QAI.0b013e31817ae5c0. [DOI] [PubMed] [Google Scholar]
- 29. Wittkop L, Günthard HF, de Wolf F, et al. Effect of transmitted drug resistance on virological and immunological response to initial combination antiretroviral therapy for HIV (EuroCoord- CHAIN joint project): a European multicohort study. Lancet Infect Dis. 2011;11:363–71. doi: 10.1016/S1473-3099(11)70032-9. [DOI] [PubMed] [Google Scholar]