Abstract
Psychological distress is common in patients with implantable cardioverter defibrillators (ICDs) and has been associated with a worse prognosis. The authors examined whether spiritual wellbeing is associated with reduced psychological distress in patients with ICDs. The Functional Assessment of Chronic Illness Therapy-Spiritual Wellbeing (FACIT-SWB) questionnare and the Hospital Anxiety and Depression Scale (HADS) were used to measure spiritual wellbeing and overall psychological distress. Multivariate linear regression was used to explore the relationship between these variables.
The study sample included 46 ICD outpatients (32 M, 14 F; age range 43–83). An inverse association between HADS and FACIT-SWB scores was found, persisting after adjustment for demographics, anxiety/depression, medications, therapist support, and functional status (F = 0.001; β= −0.31, CI: −0.44, −0.19). In conclusion, spiritual wellbeing was independently associated with lower psychological distress in ICD outpatients. Spiritual wellbeing could act as a protective factor against psychological distress in these high-risk patients.
Keywords: prevention, spirituality, cardioverter defibrillators
INTRODUCTION
Primary and secondary prevention trials have consistently shown the efficacy of implantable cardioverter defibrillators (ICDs) in preventing sudden cardiac death and life-threatening arrhythmias compared to anti-arrhythmic agents alone. According to guidelines published in 2008,[1] the ICD is now the treatment of choice not only for patients with documented life-threatening arrhythmias, but also for patients with impaired cardiac function (ejection fraction <35%), regardless of previous arrhythmic episodes.
However, as an increasing number of patients have received ICDs, several device-related problems have surfaced.[2] Although most patients adapt fairly well to living with an ICD over time, a significant proportion of patients will experience psychological problems, with estimates reaching up to 38% for clinically significant anxiety.[3] Young age (<50 years), female gender, poor device understanding, and experiencing multiple ICD shocks are important risk factors for the development of psychological problems in these patients.[3]
Psychological and emotional well-being in ICD patients is important for several reasons. Anxiety and depression may contribute to cardiovascular mortality and morbidity of patients with coronary heart disease [4, 5] and emotional[6, 7] and mental[8] stress may have a detrimental effect on cardiac perfusion and function. Reduced heart rate variability,[9, 10] impaired baro-reflex control,[11, 12] and alterations in the coagulation system[13] have been considered as possible mechanisms for the negative effect of anxiety and depression on cardiac outcomes.
Although it is uncertain whether spirituality may have a positive impact on physical health in patients with cardiovascular disease,[14] current evidence suggests that it may protect these patients from emotional distress and improve their quality of life. Spiritual well-being appears to have a protective effect on depression in patients with heart failure,[15] and faith can play a role in the emotional health of individuals recovering from a stroke[16, 17] or with severe chronic disabilities.[18] In addition, pilot spiritual interventions and holistic rehabilitation programs addressing the spiritual needs of cardiac patients have shown promising results in improving the quality of life and psychological well-being of these patients.[19–21]
However, little is known about the possible role of spiritual well-being in buffering psychological distress in patients with ICDs, despite several indications that the spiritual dimension has often been neglected in these patients. Although ICD carriers are often survivors of a cardiac arrest, have advanced heart failure and have to face difficult end-of life decisions, the educational material provided to ICD patients typically addresses only the technical/educational aspects of the ICD experience while ignoring its emotional and spiritual dimensions.[22] Clinicians are often pressed for time and they are often not forthcoming in the discussion of end-of-life issues with their patients.[23]
The purpose of this study was to evaluate whether better overall spiritual well-being may be associated with lower psychological distress in a group of outpatients who underwent ICD implantation.
METHODS
Design and population
We conducted a cross-sectional analysis on baseline data collected from 46 patients screened for participation in a pilot study of a mindfulness-based intervention for patients with ICDs. The study was conducted at the University Campus of the UMass Memorial Medical Center in Worcester, MA. All consecutive patients scheduled for an ICD related procedure at the catheterization lab were screened for study eligibility within a month of the ICD procedure. Patients were eligible if they were >21 years old, able to understand and speak English, and had access to a telephone; exclusion criteria included inability/unwillingness to give informed consent; signs of cognitive impairment; New York Heart Association functional class>III or otherwise clinically unstable; pending coronary bypass or heart transplantation; co-morbid life-threatening conditions; and ongoing severe depression or psychosis. The Blessed Orientation Memory and Concentration test [24] was used to screen patients for cognitive impairment and subjects with scores ≥10 were excluded. Screening for ongoing depression and psychosis was based on DSM criteria of major depressive disorder or psychosis as documented by the physician in the patient’s chart at the time of the most recent medical evaluation. All eligible patients received a letter inviting them to participate in the study and once they expressed interest, a screening visit was scheduled. After confirmation of study eligibility and provision of informed consent, patients completed a series of self-administered questionnaires. The study protocol was approved by the Committee for the Protection of Human Subjects at the University of Massachusetts Medical School.
Psychological distress
Psychological distress (outcome variable) was assessed using the Hospital Anxiety and Depression Scale (HADS). [25] This is a 14-item self-administered questionnaire with two sub-scales measuring anxiety and depression, with higher scores indicating greater psychological morbidity. The use of the HADS questionnaire has been validated in cardiac patients [26] and is particularly useful in these patients since it focuses on cognitive symptoms of psychological distress instead of physical symptoms, which may be similar to those resulting from the underlying cardiac disease. A cut-off of 8 is used for the two subscales, while a cut-off score of 10 is usually recommended for the total score. Total HADS scores of 10 or higher indicate the presence of psychological distress.
Spiritual well-being
The primary predictor variable was overall spiritual well-being, assessed using the Functional Assessment of Chronic Illness Therapy-Spiritual Well Being (FACIT-SWB). This is a 12 item self-reported measure of spiritual well-being that has shown high internal consistency, reliability, and convergent validity with other measures of religion/spirituality in individuals with chronic diseases.[27] This instrument includes two subscales measuring different domains of spiritual well-being – a meaning/peace subscale assessing to what extent an individual experiences peace, harmony, and a sense of meaning, and a faith subscale evaluating the extent to which a patient finds strength or comfort in his religious beliefs. The range for the total score is 0–48, with higher scores indicating greater spiritual well-being.
Demographic characteristics and other covariates
Information was collected at baseline on patient demographic characteristics and medical history. Demographic characteristics were collected by means of self-reported questionnaires and included age, gender, income, marital status, education, and racial/ethnic background. Information on cardiac diagnosis, previous diagnosis of anxiety or depression, current use of β-blockers, anti-arrhythmics, anxiolytics and antidepressants, indication for ICD implantation (primary vs. secondary prevention), type and time since ICD procedure, prior ICD shocks, New York Heart Association class, and ejection fraction (End diastolic volume - End systolic volume/End diastolic volume from an echocardiogram or a ventriculogram) was gathered from the Medical Record. Functional status was measured using the physical limitation subscale of the Seattle Angina Questionnaire.[28] Patients were also asked to report the number of times they engaged in physical exercise and whether they met with any therapist or spiritual counselor during the previous four weeks.
Statistical analysis
We conducted a preliminary analysis to evaluate the appropriateness of the model’s assumptions, and assess correlations between covariates to avoid collinearity in the multivariate model. The distribution of baseline demographic and clinical characteristics were compared between patients with high (≥50th percentile for this population) and low (≥50th percentile) spiritual well-being using t-test (or Wilcoxon) for continuous variables and two-tailed Fisher exact test to compare proportions.
The association between psychological distress and spiritual well-being was assessed using linear regression models. Variables that may confound the association between spiritual well-being and psychological distress (age, gender, income, education, marital status, prior depression or anxiety, use of antidepressants or anxiolytics, cardiovascular disease severity, and functional status) showing an association with the outcome (p ≤0.10) were included in a multivariate linear regression model. Results are presented as unadjusted and adjusted beta coefficients (with confidence intervals), where the null hypothesis was that β1 = 0. P values <0.05 were considered to be statistically significant. All analyses were performed using STATA 10 (2007) statistical software (StataCorp, LP; College Station, TX).
RESULTS
Forty-six outpatients (32 M, 14 F) aged 43–83 years (mean, 65 years) completed a series of questionnaires at the initial screening visit (Table 1). Eighty-five percent of the study sample was in New York Heart Association class II or higher and the mean ejection fraction was 0.3 (SD 0.13). Half of the participants had total HADS scores higher than 10, the threshold indicating the presence of psychological distress. Mean FACIT-SWB scores were 35±8 (scale range 0 – 48). No patient reported to have met a spiritual counselor during the previous month, and 13% reported meeting with a therapist or social worker.
Table 1.
Baseline demographic and clinical characteristics of the study sample*
| n | 46 |
| Age (mean, SD) | 65.0 (10.5) |
| Males | 32 (69.6) |
| White -non Hispanic | 43 (93.5) |
| Hispanic | 2 (4.3) |
| Asian | 1 (2.2) |
| High School | 13 (28.3) |
| Some college | 14 (30.4) |
| College graduate | 10 (21.7) |
| Post graduate | 9 (19.6) |
| Married or in committed relationship | 35 (76.1) |
| Separated/divorced/single | 11 (23.9) |
| How hard to pay for basics† | |
| Not at all hard | 26 (56.5) |
| Somewhat hard | 13 (28.3) |
| Very hard | 6 (13.0) |
| Does not know | 1 (2.2) |
| Coronary heart disease | 29 (63.0) |
| Idiopathic dilated cardiomyopathy | 9 (19.6) |
| Other | 8 (17.4) |
| Prior cardiac arrest | 10 (21.7) |
| New ICD | 27(58.7) |
| ICD upgrade | 4 (8.7) |
| Battery change/lead revision | 9 (19.6) |
| ICD shocks/storms | 6 (13.0) |
| Months from ICD procedure (median (25th–75th percentile)) | 1.45 (0.56, 14.2) |
| Beta-blockers | 40 (86.9) |
| Anxiolytics | 10 (21.7) |
| Anti-depressants | 11 (23.9) |
| Ejection fraction (mean (SD)) | 0.30 (0.13) |
| New York Heart Association class | |
| I | 7 (15.2) |
| II | 16 (56.6) |
| III | 13 (28.2) |
| FACIT-SWB score (mean, SD ) | 35.4 (8.6) |
| Prior diagnosis of depression | 11(23.9) |
| Prior diagnosis of anxiety | 9 (19.6) |
| Total HADS score>10 | 23 (50) |
| Have seen a spiritual counselor ‡ during past month | 0 (0) |
| Have seen a therapist§ during past month | 6 (13.0) |
| Physical exercise at least 30 min/week during previous months | 21 (45.7) |
Values are n (%) unless otherwise indicated
Food, housing, medical care and heating
Priest, minister, rabbi or spiritual guide
Psychologist, psychiatrist, or clinical social worker
ICD = Implantable cardioverter Defibrillator; HADS= Hospital Anxiety and Depression Scale; FACIT-SWB = Functional Assessment of Chronic Illness Therapy-Spiritual Well Being
Patients with FACIT-SWB scores above the 50th percentile (Table 2) had significantly lower HADS scores as well as a lower prevalence of psychological distress compared to patients with FACIT-SWB scores below the 50th percentile. Although most differences were not statistically significant due to the relatively small sample size, they were also older, more frequently married, less educated, and had a lower prevalence of a prior diagnosis of anxiety or depression and of use of antidepressants or anxiolytics, while the severity of clinical conditions did not differ between groups as indicated by similar mean ejection fraction values and prevalence of prior cardiac arrest and ICD shocks.
Table 2.
Baseline sample characteristics according to spiritual well-being status
| High spiritual well-being (FACIT - SWB≥36.5) |
Low spiritual well-being (FACIT - SWB<36.5) |
P value† | |
|---|---|---|---|
| N | 23 | 23 | |
| Age (mean, CI) | 69.2 (65.8, 72.6) | 60.8 (56.1, 65.5) | 0.0114 |
| Females | 50.0 (7) | 50.0 (7) | 1.00 |
| College or post-graduate education | 15.2 (7) | 26.1 (12) | 0.48 |
| Married or in committed relationship | 54.3 (19) | 45.7 (16) | 0.49 |
| Not at all hard to pay for basics‡ | 42.3 (11) | 57.7 (15) | 0.36 |
| Somewhat hard | 69.2 (9) | 30.8 (4) | |
| Very hard | 50 (3) | 50 (3) | |
| Does not know | 1 (100) | 0 (0) | |
| Coronary heart disease | 55.2 (16) | 44.8 (13) | 0.70 |
| Prior cardiac arrest | 50 (5) | 50 (5) | 1.00 |
| New ICD | 48.2 (13) | 51.8 (14) | 0.52 |
| ICD shocks/storms | 50.0 (3) | 50.0 (3) | 0.66 |
| Prior diagnosis of depression | 27.3 (3) | 72.7 (8) | 0.16 |
| Prior diagnosis of anxiety | 44.4 (4) | 55.6 (5) | 1.00 |
| Counselors | 33.3 (2) | 66.7 (4) | 0.67 |
| Beta-blockers | 50 (20) | 50 (20) | 1.00 |
| Anxiolytics | 40.0 (4) | 60.0 (6) | 0.72 |
| Anti-depressants | 27.3 (3) | 72.7 (8) | 0.16 |
| Ejection fraction (mean, CI) | 0.29 (0.26, 0.33) | 0.30 (0.23, 0.37) | 0.69 |
| Functional status (mean, CI) | 64.4 (55.7, 73.0) | 53.8 (42.7, 64.8) | 0.17 |
| Total HADS score (mean, CI) | 6.7 (4.4, 9.0) | 13.8 (11.4, 16.2) | 0.0001 |
| HADS score>10 | 21.7 (5) | 78.3 (18) | 0.0001 |
| Physical exercise at least 30 minutes/week during past month | 61.9 (13) | 38.1 (8) | 0.236 |
Values are n (%) unless otherwise indicated
Wilcoxon or 2-sided Fisher exact test
Heating, groceries, and health insurance
ICD = Implantable cardioverter Defibrillator; HADS= Hospital Anxiety and Depression Scale; FACIT-SWB = Functional Assessment of Chronic Illness Therapy-Spiritual Well Being
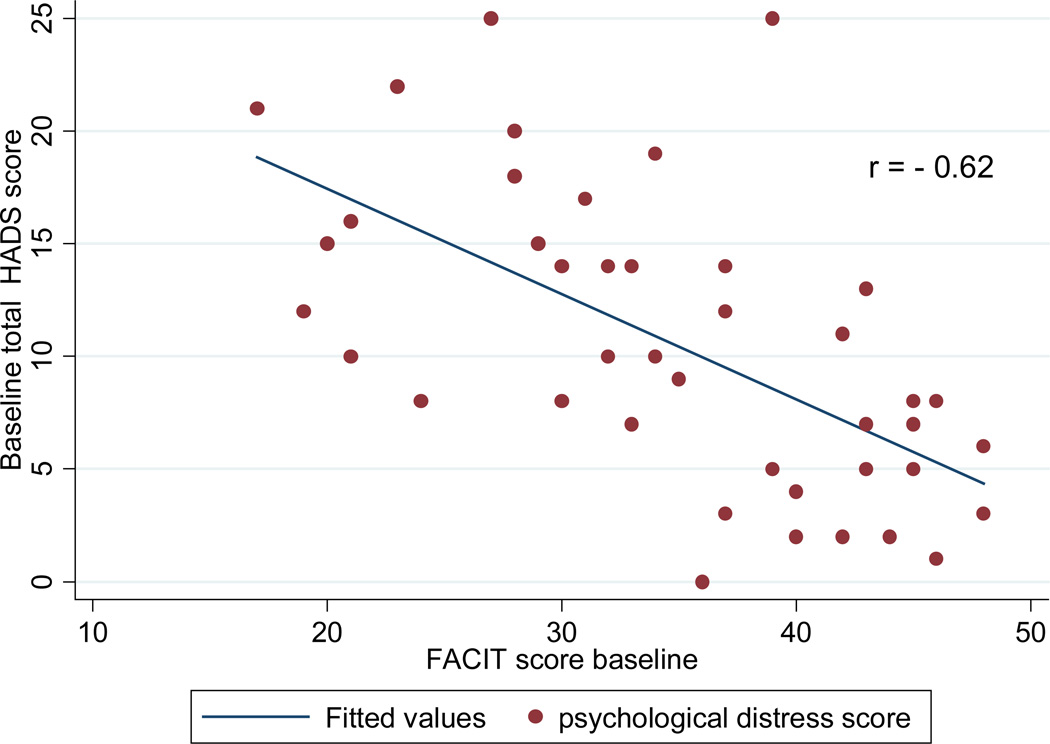
Table 3 shows the results of the unadjusted and adjusted linear regression models. Psychological distress scores were significantly and inversely associated with FACIT-SWB scores (Figure 1). In multivariate models, spiritual well-being was significantly associated with lower psychological distress independently of demographics (model 2); of a previous diagnosis of anxiety or depression, use of anxiolytics or antidepressants and counseling (model 3); and of physical exercise or functional status (model 4).
Table 3.
Results of the unadjusted and adjusted linear regression models testing the association between total HADS scores and FACIT-SWB scores
| β | 95% CI | R squared | |
|---|---|---|---|
| Model 1 | −0.32 | −0.37, −0.13 | 0.44 |
| Model 2 | −0.30 | −0.43, −0.17 | 0.56 |
| Model 3 | −0.32 | −0.45, −0.20 | 0.67 |
| Model 4 | −0.31 | −0.44, −0.19 | 0.69 |
Model 1: unadjusted
Model 2: adjusted for demographics (age, marital status, financial status)
Model 3: adjusted for variables included in model 2 + prior depression and anxiety, use of psychotropic drugs, counselors/therapists during past month
Model 4: adjusted for variables included in model 3 + functional status, and physical exercise
HADS= Hospital Anxiety and Depression Scale; FACIT-SWB = Functional Assessment of Chronic Illness Therapy-Spiritual Well Being
Figure 1.
Unadjusted association between overall psychological distress and spiritual well-being
DISCUSSION
Despite indications that spirituality is an important component of the psychological well-being of patients with severe chronic diseases,[29–31] a limited number of studies have examined its characteristics in patients with cardiovascular disease.[15, 16, 32] A possible explanation for the limited interest in this topic in the cardiology literature is that spirituality is an elusive concept, encompassing both subjective dimensions that are difficult to define and operationalize, and more easily measurable, objective dimensions such as frequency of spiritual activities or spiritual/religious affiliation.[33]
This is the first paper describing the characteristics associated with spiritual well-being in patients living with an ICD and investigating the possible impact of spiritual well-being on the self-reported psychological health of these patients. In our study, patients with higher spiritual well-being had significantly less psychological distress and a lower prevalence of concurrent psychiatric morbidity and psychotropic drug use compared to patients with lower spiritual well-being. On the other hand, clinical conditions and functional status were similar between the two groups, suggesting that differences in psychological well-being were independent from the severity of the cardiac condition. There was an inverse linear relationship between psychological distress scores and spiritual well-being scores that persisted after taking into account a number of possible confounding variables.
The limited data currently available describing the role of spiritual well-being in patients with chronic cardiovascular disease is typically based on patients with advanced heart failure. These studies, usually qualitative or cross-sectional in nature, have shown the centrality of spirituality in the life of patients and caregivers alike [34, 35] and its association with better quality of life [36] and adjustment to advanced heart failure.[37]
Our results are consistent with those of a cross-sectional analysis showing a strong inverse association between spiritual well-being and depression in 60 patients with heart failure, independent of gender, income, social support, physical symptoms, and health status.[15] This is not surprising, considering that ICD patients usually have concomitant heart failure and, in fact, 85% of our patients were in New York Heart Association class II or III. One important addition of our paper to the current literature is that we adjusted for other important confounders such as co-morbid depression or anxiety, psychotropic medications, and ongoing psychosocial support. Furthermore, patients with ICDs are somewhat unique among patients with heart failure, in that they often have experienced a cardiac arrest (21% of our population) and usually have more severe cardiac conditions.
Several limitations need to be kept in mind in interpreting the results of the present study. The first concerns our choice of the instrument to assess spiritual well-being. The FACIT-SWB is a measure of spiritual well-being, and not of spirituality, and has been criticized because of the overlap with measures of psychological well-being.[30, 38] However, the finding of an inverse association between spiritual well-being and psychological distress has been consistently reported in various populations using different measures of spirituality and psychological distress.[30, 39] Furthermore, in our analysis the association between spiritual well-being and psychological distress was still evident after we accounted for psychological co-morbidity, use of psychotropic medications, and support from therapists, thus suggesting that spiritual well-being may uniquely contribute to reducing overall psychological distress. An additional limitation is that we limited our assessments to one dimension of spirituality, namely its emotional aspects, while we did not address other components such as affiliation or frequency of spiritual practice. Moreover, due to the cross-sectional nature of this study, resulting in the assessment of spiritual well-being and psychological distress at the same point in time, we cannot draw conclusions about the direction of this association. We also cannot exclude the possibility of selection bias, since this analysis was conducted on data collected as part of the baseline assessments of patients screened for participation in a pilot randomized clinical trial. The prevalence of anxiety and depression in our study, however, are consistent with that reported in similar studies of ICD outpatients. [3, 40] The vast majority of our study population was white, and our findings may not be generalizable to minority populations in which dimensions of spirituality other than spiritual well-being, such as attendance at worship services or spiritual beliefs, could be more relevant.
In conclusion, spiritual well-being was independently associated with lower psychological distress in a group of outpatients with ICDs. These findings need to be confirmed in larger and more diverse populations, and using a prospective design to evaluate whether spiritual if this association is maintained over time. In consideration of the possible unique contribution of spiritual well-being to the overall psychological well-being and quality of life of patients with ICDs, the spiritual-existential dimension of the experience of living with an ICD should probably receive more attention in the care of these patients.
ACKNOWLEDGEMENTS
We would like to thank all participants for their contribution to this study; and Mary Stanley, MS, NP, and Karen Rose, MS, NP, for their help with recruitment.
Financial disclosures/funding: This study was partially supported by a grant of the National Center of Complementary and Alternative Medicine (F32AT005048). Elena Salmoirago-Blotcher is funded by a grant from the National Center for Complementary and Alternative Medicine (NCCAM F32AT005048)
Footnotes
Authors contributions: Elena Salmoirago-Blotcher designed the study, collected the data, conducted the data analysis, and wrote the manuscript draft; Sybil Crawford provided statistical advice and revised the manuscript; Chau Tran contributed to the study design and data collection; Robert Goldberg, Ira Ockene and Lawrence Rosenthal revised the manuscript. All authors approved the final version of the manuscript for publication.
Presentations: This study has been accepted as a poster presentation at the annual conference of the Society of Behavioral Medicine (New Orleans April 2012
Conflicting interests: none. No honorarium, grant, or other form of payment was given to anyone to produce the manuscript.
Ethical Approval: The study protocol and all study materials were approved by the Committee for the Protection of Human Subjects at the University of Massachusetts Medical School (Docket H-13078).
References
- 1.Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices). Developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;51(21):e1–e62. doi: 10.1016/j.jacc.2008.02.032. [DOI] [PubMed] [Google Scholar]
- 2.Bostwick JM, Christopher LS. An updated review of implantable cardioverter/defibrillators, induced anxiety, and quality of life. Psychiatr Clin North Am. 2007;30(4):677–688. doi: 10.1016/j.psc.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Sears SF, Jr, Conti JB. Quality of life and psychological functioning of ICD patients. Heart. 2002;87(5):488–493. doi: 10.1136/heart.87.5.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barefoot JC, Helms MJ, Mark DB, et al. Depression and long-term mortality risk in patients with coronary artery disease. Am J Cardiol. 1996;78(6):613–617. doi: 10.1016/s0002-9149(96)00380-3. [DOI] [PubMed] [Google Scholar]
- 5.Lesperance F, Frasure-Smith N, Talajic M, Bourassa MG. Five-year risk of cardiac mortality in relation to initial severity and one-year changes in depression symptoms after myocardial infarction. Circulation. 2002;105(9):1049–1053. doi: 10.1161/hc0902.104707. [DOI] [PubMed] [Google Scholar]
- 6.Ironson G, Taylor C, Boltwood M, et al. Effects of anger on left ventricular ejection fraction in coronary artery disease. Am J Cardiol. 1993;70(3):281–285. doi: 10.1016/0002-9149(92)90605-x. [DOI] [PubMed] [Google Scholar]
- 7.Wittstein IS, Thiemann DR, Lima JAC, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. New Engl J Med. 2005;352(6):539–548. doi: 10.1056/NEJMoa043046. [DOI] [PubMed] [Google Scholar]
- 8.Rozanski A, Bairey C, Krantz D, Friedman J. Mental stress and the induction of silent myocardial ischemia in patients with coronary artery disease. N Engl J Med. 1988;318(16):1005–1012. doi: 10.1056/NEJM198804213181601. [DOI] [PubMed] [Google Scholar]
- 9.Carney RM, Blumenthal JA, Freedland KE, et al. Low heart rate variability and the effect of depression on post-myocardial infarction mortality. Arch Intern Med. 2005;165(13):1486–1491. doi: 10.1001/archinte.165.13.1486. [DOI] [PubMed] [Google Scholar]
- 10.Kawachi I, Sparrow D, Vokonas PS, Weiss ST. Decreased heart rate variability in men with phobic anxiety (data from the Normative Aging Study) Am J Cardiol. 1995;75(14):882–885. doi: 10.1016/s0002-9149(99)80680-8. [DOI] [PubMed] [Google Scholar]
- 11.Watkins LL, Blumenthal JA, Carney RM. Association of anxiety with reduced baroreflex cardiac control in patients after acute myocardial infarction. Am Heart J. 2002;143:460–466. doi: 10.1067/mhj.2002.120404. [DOI] [PubMed] [Google Scholar]
- 12.Watkins LL, Grossman P. Association of depressive symptoms with reduced baroreflex cardiac control in coronary artery disease. Am Heart J. 1999;137(3):453–457. doi: 10.1016/s0002-8703(99)70491-6. [DOI] [PubMed] [Google Scholar]
- 13.Von Kanel R, Mills PJ, Fainman C, Dimsdale JE. Effects of psychological stress and psychiatric disorders on blood coagulation and fibrinolysis: a biobehavioral pathway to coronary artery disease? Psychosom Med. 2001;63(4):531–544. doi: 10.1097/00006842-200107000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Feinstein M, Liu K, Ning H, et al. Burden of cardiovascular risk factors, subclinical atherosclerosis, and incident cardiovascular events across dimensions of religiosity: The Multi-Ethnic Study of Atherosclerosis. Circulation. 2010;121(5):659–666. doi: 10.1161/CIRCULATIONAHA.109.879973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bekelman DB, Dy SM, Becker DM, et al. Spiritual well-being and depression in patients with heart failure. J Gen Intern Med. 2007;22(4):470–477. doi: 10.1007/s11606-006-0044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giaquinto S, Spiridigliozzi C, Caracciolo B. Can faith protect from emotional distress after stroke? Stroke. 2007;38(3):993–997. doi: 10.1161/01.STR.0000257996.26950.59. [DOI] [PubMed] [Google Scholar]
- 17.Johnstone B, Franklin KL, Yoon DP, et al. Relationships among religiousness, spirituality, and health for individuals with stroke. J Clin Psychol Med Settings. 2008;15(4):308–313. doi: 10.1007/s10880-008-9128-5. [DOI] [PubMed] [Google Scholar]
- 18.Johnstone B, Yoon DP. Relationships between the Brief Multidimensional Measure of Religiousness/Spirituality and health outcomes for a heterogeneous rehabilitation population. Rehabil Psychol. 2009;54(4):422–431. doi: 10.1037/a0017758. [DOI] [PubMed] [Google Scholar]
- 19.Delaney C, Barrere C, Helming M. The influence of a spirituality-based intervention on quality of life, depression, and anxiety in community-dwelling adults with cardiovascular disease: a pilot study. J Holist Nurs. 2010;29(1):21–32. doi: 10.1177/0898010110378356. [DOI] [PubMed] [Google Scholar]
- 20.Warber SL, Ingerman S, Moura VL, et al. Healing the heart: a randomized pilot study of a spiritual retreat for depression in acute coronary syndrome patients. Explore (NY) 2011;7(4):222–233. doi: 10.1016/j.explore.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 21.Kreikebaum S, Guarneri E, Talavera G, et al. Evaluation of a holistic cardiac rehabilitation in the reduction of biopsychosocial risk factors among patients with coronary heart disease. Psychol Health Med. 2011;16(3):276–290. doi: 10.1080/13548506.2010.542170. [DOI] [PubMed] [Google Scholar]
- 22.Bolse K, Johansson I, Stromberg A. Organisation of care for Swedish patients with an implantable cardioverter defibrillator, a national survey. J Clin Nurs. 2010;20(17–18):2600–2608. doi: 10.1111/j.1365-2702.2010.03540.x. [DOI] [PubMed] [Google Scholar]
- 23.Goldstein NE, Lampert R, Bradley E, et al. Management of implantable cardioverter defibrillators in end-of-life care. Ann Intern Med. 2004;141(11):835–838. doi: 10.7326/0003-4819-141-11-200412070-00006. [DOI] [PubMed] [Google Scholar]
- 24.Katzman R, Brown T, Fuld P, et al. Validation of a short Orientation-Memory-Concentration Test of cognitive impairment. Am J Psychiatry. 1983;140(6):734–739. doi: 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- 25.Zigmond A, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 26.Stafford L, Berk M, Jackson HJ. Validity of the Hospital Anxiety and Depression Scale and Patient Health Questionnaire-9 to screen for depression in patients with coronary artery disease. General Hosp Psychiatry. 2007;29(5):417–424. doi: 10.1016/j.genhosppsych.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 27.Peterman AH, Fitchett G, Brady MJ, et al. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy--Spiritual Well-being Scale (FACIT-Sp) Ann Behav Med. 2002;24(1):49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 28.Spertus JA, Winder JA, Dewhurst TA, et al. Development and evaluation of the Seattle Angina questionnaire: A new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25(2):333–341. doi: 10.1016/0735-1097(94)00397-9. [DOI] [PubMed] [Google Scholar]
- 29.Breitbart W. Spirituality and meaning in supportive care: spirituality- and meaning-centered group psychotherapy interventions in advanced cancer. Support Care Cancer. 2002;10(4):272–280. doi: 10.1007/s005200100289. [DOI] [PubMed] [Google Scholar]
- 30.McClain CS, Rosenfeld B, Breitbart W. Effect of spiritual well-being on end-of-life despair in terminally-ill cancer patients. Lancet. 2003;361(9369):1603–1607. doi: 10.1016/S0140-6736(03)13310-7. [DOI] [PubMed] [Google Scholar]
- 31.Koenig HG, George LK, Titus P. Religion, spirituality, and health in medically ill hospitalized older patients. J Am Geriatr Soc. 2004;52(4):554–562. doi: 10.1111/j.1532-5415.2004.52161.x. [DOI] [PubMed] [Google Scholar]
- 32.Giaquinto S, Sarno S, Dall'Armi V, Spiridigliozzi C. Religious and spiritual beliefs in stroke rehabilitation. Clin Exp Hypertens. 2010;32(6):329–334. doi: 10.3109/10641960903443566. [DOI] [PubMed] [Google Scholar]
- 33.Koenig H, McCullough M, Larson D. Handbook of religion and health. New York: Oxford University Press; 2001. [Google Scholar]
- 34.Murray SA, Kendall M, Boyd K, et al. Exploring the spiritual needs of people dying of lung cancer or heart failure: a prospective qualitative interview study of patients and their caregivers. Palliat Med. 2004;18(1):39–45. doi: 10.1191/0269216304pm837oa. [DOI] [PubMed] [Google Scholar]
- 35.Groleau D, Whitley R, Lesperance F, Kirmayer LJ. Spiritual reconfigurations of self after a myocardial infarction: Influence of culture and place. Health Place. 2010;16(5):853–860. doi: 10.1016/j.healthplace.2010.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beery TA, Baas LS, Fowler C, Allen G. Spirituality in persons with heart failure. J Holist Nurs. 2002;20(1):5–25. doi: 10.1177/089801010202000102. [DOI] [PubMed] [Google Scholar]
- 37.Westlake C, Dracup K. Role of spirituality in adjustment of patients with advanced heart failure. Prog Cardiovasc Nurs. 2001;16(3):119–125. doi: 10.1111/j.0889-7204.2001.00592.x. [DOI] [PubMed] [Google Scholar]
- 38.Murphy PE, Canada AL, Fitchett G, et al. An examination of the 3-factor model and structural invariance across racial/ethnic groups for the FACIT-Sp: a report from the American Cancer Society's Study of Cancer Survivors-II (SCS-II) Psychooncology. 2010;19:264–272. doi: 10.1002/pon.1559. [DOI] [PubMed] [Google Scholar]
- 39.Bekelman DB, Parry C, Curlin FA, et al. A comparison of two spirituality instruments and their relationship with depression and quality of life in chronic heart failure. J Pain Symptom Manage. 2010;39(3):515–526. doi: 10.1016/j.jpainsymman.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kapa S, Rotondi-Trevisan D, Mariano Z, et al. Psychopathology in patients with ICDs over time: results of a prospective study. Pacing Clin Electrophysiol. 2010;33(2):198–208. doi: 10.1111/j.1540-8159.2009.02599.x. [DOI] [PubMed] [Google Scholar]