Abstract
Background
Stabilization of a pelvic discontinuity with a posterior column plate with or without an associated acetabular cage sometimes results in persistent micromotion across the discontinuity with late fatigue failure and component loosening. Acetabular distraction offers an alternative technique for reconstruction in cases of severe bone loss with an associated pelvic discontinuity.
Questions/Purposes
We describe the acetabular distraction technique with porous tantalum components and evaluate its survival, function, and complication rate in patients undergoing revision for chronic pelvic discontinuity.
Methods
Between 2002 and 2006, we treated 28 patients with a chronic pelvic discontinuity with acetabular reconstruction using acetabular distraction. A porous tantalum elliptical acetabular component was used alone or with an associated modular porous tantalum augment in all patients. Three patients died and five were lost to followup before 2 years. The remaining 20 patients were followed semiannually for a minimum of 2 years (average, 4.5 years; range, 2–7 years) with clinical (Merle d’Aubigné-Postel score) and radiographic (loosening, migration, failure) evaluation.
Results
One of the 20 patients required rerevision for aseptic loosening. Fifteen patients remained radiographically stable at last followup. Four patients had early migration of their acetabular component but thereafter remained clinically asymptomatic and radiographically stable. At latest followup, the average improvement in the patients not requiring rerevision using the modified Merle d’Aubigné-Postel score was 6.6 (range, 3.3–9.6). There were no postoperative dislocations; however, one patient had an infection, one a vascular injury, and one a bowel injury.
Conclusions
Acetabular distraction with porous tantalum components provides predictable pain relief and durability at 2- to 7-year followup when reconstructing severe acetabular defects with an associated pelvic discontinuity.
Level of Evidence
Level IV, therapeutic study. See Instructions for Authors for a complete description of levels of evidence.
Introduction
Acetabular revision in the presence of severe bone loss will become increasingly common as revision THA is performed more frequently and in younger patients [10]. Osteolysis and stress shielding often progress asymptomatically with well-fixed, cementless, acetabular components [9]. The severity of bone loss can be quite pronounced before the cup migrates or the patient experiences symptoms. Similarly, migration of a cemented acetabular component may result in a large amount of bone destruction [1]. Pelvic discontinuity, with separation of the superior and inferior portions of the pelvis, may occur in cases of severe bone loss. Solid fixation of the acetabular prosthesis is more difficult to obtain due to motion between the superior and inferior hemipelvis. Successful reconstruction may involve a purely mechanical construct that gains stability through supplemental fixation strategies or one that achieves stability with bone ingrowth into the porous acetabular component. For ingrowth to occur, the initial reconstruction must minimize micromotion and the surrounding milieu must remain biologically active.
Several authors have suggested concomitant compression plating of the posterior column at the time of reconstruction in patients with a pelvic discontinuity [5, 8, 19]. This technique provides initial mechanical stability and ideally subsequent biologic fixation once bone healing occurs. Success of this technique depends on both (1) adequate bone stock and (2) a favorable biologic environment necessary for primary bone healing [1]. However, these two essential conditions are less likely in cases of a chronic pelvic discontinuity [5, 19]. Severe bone loss along the posterior column with an associated discontinuity may preclude direct bony apposition and initial stability of a hemispherical socket with internal fixation techniques. Historically, bulk acetabular allografts were utilized in these cases. Previously published data from the senior author (WGP) revealed rates of aseptic loosening of 50% with this technique [14]. Acetabular cages have been used to bridge the defect and obtain relative fixation along the iliac wing and ischium [6, 8, 15, 16]. With this mechanical approach, bone ingrowth into the acetabular cage does not occur and micromotion and stress on the mechanical construct persist [6, 15, 16]. Failure rates from 50% to 60% have been reported due to mechanical loosening or broken flanges [6, 16]. Because of reported high failure rates with these various approaches, two of us (SMS, WGP) developed a novel method of reconstruction with porous tantalum components placed into a distracted pelvic discontinuity. We presumed this method would provide adequate initial mechanical stability for bone ingrowth to occur into the prosthesis both superiorly and inferiorly to bridge the discontinuity in a biologic fashion. Thus, we anticipate a decreased incidence of mechanical failure with our method of acetabular distraction.
We therefore describe the technique of acetabular distraction and report the (1) survival, (2) function, and (3) complications associated with this method.
Patients and Methods
Through our institutional data repository, we identified all 28 patients with a chronic pelvic discontinuity undergoing revision THA with the technique of acetabular distraction between 2002 and 2006. This cohort represents a fully consented, unselected series of patients treated for a chronic pelvic discontinuity as no other patient with pelvic discontinuity during this time interval underwent reconstruction with an alternate treatment strategy. Before a minimum 2-year followup, five patients had been lost and three others had died from causes unrelated to the revision procedure. These eight patients were excluded from the study cohort. The remaining 20 patients had a minimum followup of 24 months (average, 54 months; range, 24–84 months). Fifteen of these patients were women while five were men. The average age at the time of the revision procedure was 67.5 years (range, 43–85 years), and the average number of previous surgeries was 2.6 (range, 1–6). Within this cohort, the original diagnosis was osteoarthritis in 10, rheumatoid arthritis in nine, and developmental dysplasia of the hip in one. Aseptic loosening was the reason for revision in all 20 patients. The acetabular defects were classified using the system described by the senior author [13]. Four of the acetabuli were classified as Type IIC, three as Type IIIA, and the remaining 13 as Type IIIB [2, 13]. Briefly, Type IIC defects are those defects that have distortion of the superior rim, less than 3 cm of superior migration, medial migration to Kohler’s line, and minimal ischial osteolysis. Type IIIA defects have greater superior rim distortion with greater than 3 cm of superolateral migration, intact Kohler’s line, and moderate ischial osteolysis. Type IIIB defects have substantial superior dome destruction with greater than 3 cm of superomedial migration, broken Kohler’s line, and severe ischial osteolysis. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. We had prior institutional review board approval.
Each surgery was performed by one of us (SMS, WGP) through a posterior approach. After the acetabular component was explanted, the lower portion of the ischium was stressed with a Cob elevator and motion between the superior and inferior portions of the acetabulum confirmed the presence of a discontinuity. All interposed fibrous tissue and granulation tissue were débrided to uncover viable host bone where punctate bleeding was encountered. Full hemispherical reamers were then placed in the acetabular defect at the level of the native hip center to determine the anterior-posterior dimension of the pelvic defect. Sequentially larger reamers were used until the anterior-superior and posterior-inferior margins of the acetabulum were engaged. With severe bone defects, the reamer may not fully engage these specific regions of the acetabulum. In these situations, we relied on porous tantalum augments to reestablish this relationship and fill any large cavitary defects. Careful attention is necessary to avoid reaming eccentrically into either the anterior or posterior direction. The type and position of additional porous tantalum augments were dictated by the location and severity of bone loss after the anterior-superior and posterior-inferior regions were engaged with the reamer. Large defects are often encountered in the anterior-superior region of the acetabulum necessitating the use of a buttress augment; this concomitantly serves to increase the surface area available for biologic ingrowth. In this series, 11 of the 20 patients received augments; the remaining nine patients required no augments. One augment was used in eight patients, either in the anterior-superior region (six) or in the posterior-superior region (Fig. 1). In three of these 11 patients, two augments were used to provide secure points of fixation for the socket in anterior-superior and posterior-inferior defects of the acetabulum. Augments were first secured to the host bone with screws. Next, the acetabular component was impacted into place with polymethylmethacrylate cement limited to the augment-cup interface. Attempts were made to maximize the amount of host bone contact with the augments and acetabular component. Particulate graft was placed into any remaining cavities before the revision shell was impacted into place. The superior and inferior aspects of the hemipelvis were distracted through the discontinuity by placing a porous tantalum acetabular component 6 to 8 mm larger than the last hemispherical reamer. The distraction of the pelvis was accomplished by initially placing the inferior aspect of the porous acetabular component against the remaining ischium followed by bringing the implant to the desired position while continuously placing an inferiorly directed stress. This distraction of the pelvis created a press fit, which provided the initial mechanical stability of the cup until multiple cancellous screws were placed into the remaining ilium and ischium. As described by Laflamme et al. [11], a polyethylene liner was cemented into the cup to allow screws to function as a fixed-angle construct. The femoral head size was maximized in all patients. Two patients with deficient abductors had a constrained liner, nine patients had a tripolar (unconstrained) articulation due to a retained femoral component, six had a 40-mm head size, one had a 36-mm head size, and two had a 32-mm head size.
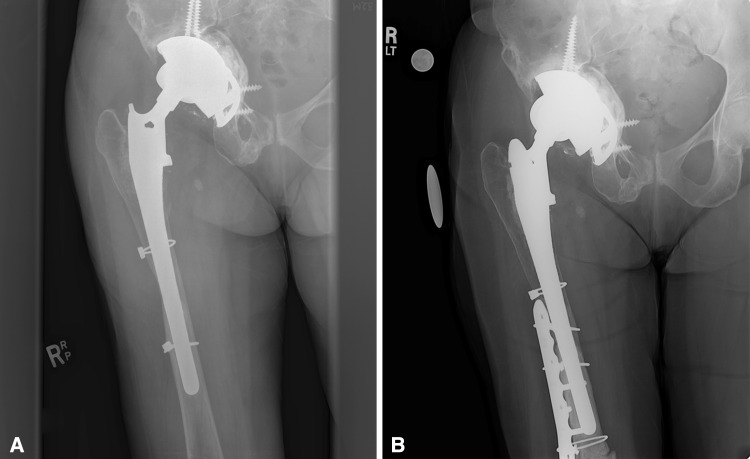
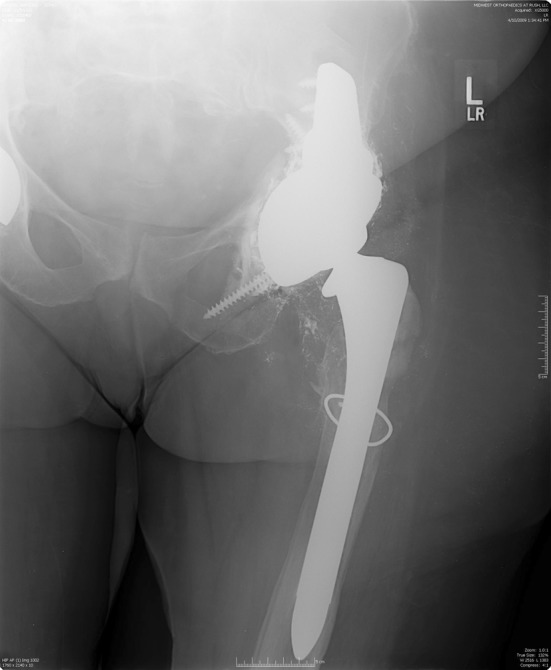
Fig. 1.
A tantalum elliptical cup is shown spanning the pelvic discontinuity. A superior augment was used in this case.
All patients were restricted to touch-down weightbearing for 12 weeks, followed by partial weightbearing with a walker for an additional 12 weeks.
All patients were examined clinically and radiographically at 2 weeks, 6 weeks, 3 months, 6 months, and yearly thereafter for a minimum of 2 years. Clinical outcome measures included the Merle d’Aubigné-Postel pain and walking scores [3]. This assessment for pain assigns 6 points for no pain, 5 points for slight/intermittent pain, 4 points for pain after some activities, 3 points for pain allowing only limited activities, 2 points for severe pain with activity, 1 point for severe/spontaneous pain, and 0 points for severe/constant pain. The walking component assigns 6 points for no cane/limp, 5 points for no cane with mild limp, 4 points for being able to walk short distances without a cane, 3 points for being able to walk short distances with a cane, 2 points for being able to walk very limited distances with a cane, 1 point for needing a walker, and 0 points when unable to walk. Complications were subdivided into major complications that necessitated further surgery and minor complications that did not.
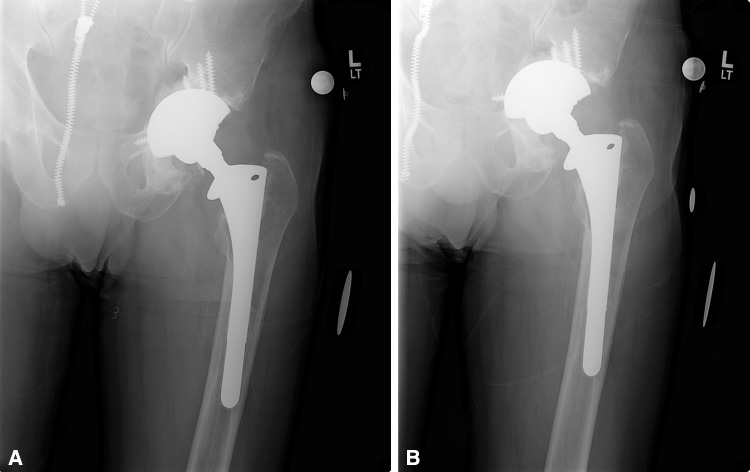
Radiographic evaluation consisted of standard AP radiographs of the pelvis and AP and Lowenstein lateral radiographs of the hip. These were obtained preoperatively and at all postoperative time points (Fig. 2). The most recent radiographs were compared with the initial postoperative radiographs. Two reviewers (SMS, VKK) independently evaluated all radiographs for loosening and migration. Loosening was defined as a change in the component abduction angle of greater than 10° or a change in the horizontal or vertical position of greater than 6 mm after correcting for magnification (Fig. 3).
Fig. 2.
A well-fixed porous tantalum metal cup is shown. No cup migration or hardware failure can be seen at 6 years postoperatively.
Fig. 3A–B.
(A) A radiograph taken 39 months after surgery shows a well-fixed cup. (B) In a radiograph taken 50 months after surgery, migration of the cup is noted.
The pre- and postoperative Merle d’Aubigné-Postel scores were compared using a paired Student’s t-test. Kaplan-Meier survival plots were constructed with radiographic loosening and clinical failure as discrete end points (SPSS® for Windows®, Version 14.0; IBM Corp, Armonk, NY, USA).
Results
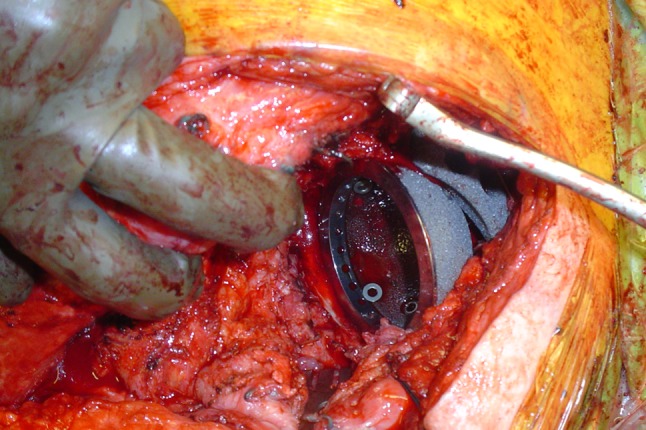
Among the 20 patients in this cohort, one construct failed. The patient had rerevision for symptomatic aseptic loosening at 9 months; this was due to the loss of ischial fixation and subsequent failure of ingrowth resulting in acetabular component protrusio (Fig. 4). Radiographically, in the remaining 19 patients, four were loose with component migration at followup times ranging from 12 to 48 months. All of these radiographic failures were in patients with Type IIIB acetabular defects that demonstrated changes in abduction angle, horizontal or vertical position, and loss of ischial fixation. Two radiographic loosenings were identified within the first year of followup; one was identified within 2 years’ followup and one at 4 years’ followup. Two of these four also had fractures of supplementary bone screws (Fig. 5). However, all implants classified as loose have subsequently remained stable over an average period of 49 months with no further radiographic migration.
Fig. 4A–B.
(A) A radiograph taken 3 months after surgery shows a well-fixed prosthesis. (B) At 9 months, the cup has lost ischial fixation resulting in acetabular component protrusio. The patient was symptomatic and needed a revision.
Fig. 5.

Broken screws can be seen as this cup has migrated from its previously well-fixed position. The patient is now 6 years postoperative and no further component migration has occurred. The patient remains asymptomatic.
Clinically, 17 of 19 patients denied pain in the operative hip: one patient reported minimal pain after walking six blocks or more and one patient reported pain with sitting for long periods of time. Seven patients walked without assistive devices, four patients used a cane for long distances, five patients used a cane at all times, and three patients used a walker at all times. None of the patients used a wheelchair. The mean (± SD) improvement (p < 0.001) of the Merle d’Aubigné-Postel pain and ambulation score was 6.6 ± 1.2 (3.3 preoperatively to 9.6 postoperatively). At most recent followup, the four patients with radiographic loosening were pain free and functioning well with an average Merle d’Aubigné-Postel score improvement (p < 0.001) of 5.6 ± 1.0 (3.0 preoperatively to 8.6 postoperatively).
Associated perioperative complications included three major and one minor complication. One patient with an iatrogenic colonic perforation required general surgical intervention, another with an intraoperative femoral artery injury required repair by a vascular surgeon, a third with a superficial infection was treated with irrigation and débridement, and a fourth with a greater trochanteric fracture was treated nonoperatively. At the most recent followup, there were no postoperative dislocations.
Discussion
In response to suboptimal outcomes in the management of severe acetabular defects associated with pelvic discontinuity, we have developed a novel method of acetabular distraction with porous tantalum components. We believe this provides adequate initial mechanical stability for bone ingrowth to occur into the prosthesis both superiorly and inferiorly to bridge the discontinuity in a biologic fashion. Our first purpose was to describe the technique of distraction and report its survival. Our second purpose was to describe the clinical function and complications associated with this method in a series of patients. The intent is to frame these results in the context of previous fixation strategies for chronic pelvic discontinuity encountered in revision THA.
Our study is associated with a few notable limitations. First, the absence of a control group makes it difficult to draw conclusions regarding the impact of this technique and patient-related factors that may affect outcome compared to other techniques. Second, the series is relatively small. One large revision series identified 31 pelvic discontinuities in 3505 patients (0.9%) [1]. The low incidence of these difficult cases underscores the paucity of literature that clearly discerns the efficacy and survival of the different philosophies to reconstruction. Our study is one of the largest series evaluating severe defects in the setting of pelvic discontinuity. Most of the literature evaluating chronic pelvic discontinuities encountered at the time of revision acetabular surgery comes in the form of an analysis of these difficult cases as a subset of a larger, more diverse revision series. Third, with a followup of 2 to 7 years, we cannot ensure the long-term durability of these reconstructions, especially in the setting of four radiographic failures that are functioning well clinically. Fourth, the retrospective design of this study is a discernible limitation. At this time, there are no randomized trials comparing this technique to others. Fifth, we did not report bony healing of the discontinuity as it is difficult to reliably and accurately evaluate radiographic healing of a pelvic discontinuity using this surgical technique. This method of reconstruction relies on acetabular bone ingrowth from the superior and inferior hemipelvis for stable fixation. Therefore, we believe component migration or change in position can be used as a surrogate for stable fixation and healing. Sixth, we did not assess intraobserver variability for assessing radiographs. Finally, we lost five patients to followup; consequently, that may introduce a potential bias in the rate of mechanical failure rate.
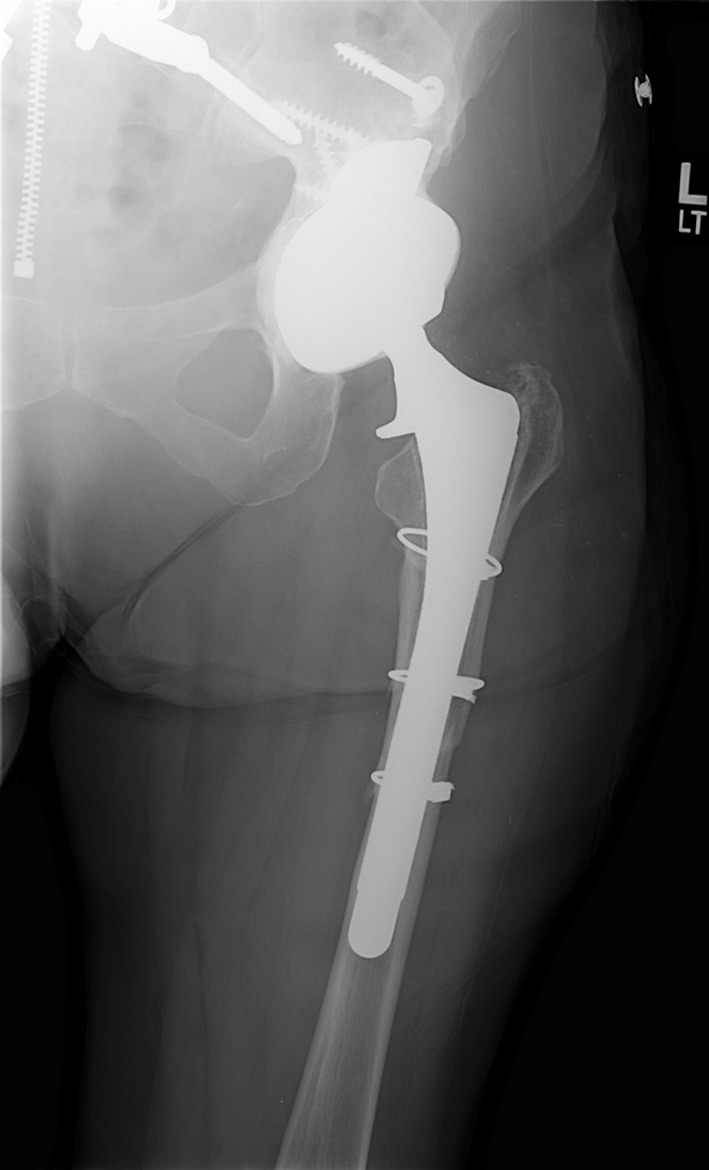
Fifteen of our 20 reconstructions remained clinically and radiographically stable at an average of 4.5 years postoperatively while four of the 20 hips demonstrated early migration of the acetabular component. None of the four have had further radiographic change in component position implying bony ingrowth, and all patients remain pain free. Only one socket required revision, and this was for aseptic loosening. The cause of this failure was believed to be inadequate fixation into the ischium. We now strive to obtain a minimum of two screws into the ischium (Fig. 6) to avoid early vertical displacement of the acetabular component. There have been recent reports of a 57.7% versus 14.3% 5-year mechanical failure rate, comparing a novel cemented cage technique to porous metal constructs in pelvic discontinuity [7]. We have previously reported poor intermediate-term results with structural or cancellous allografts combined with acetabular cages in patients with chronic pelvic discontinuities [15]. At an average followup of 5 years, five of 16 reconstructions were revised for loosening, while an additional three appeared radiographically loose. We presumed these discontinuities did not heal and persistent micromotion led to eventual fatigue failure of the cages. Others have reported on the use of a custom triflange device in 20 hips with severe bone loss and discontinuity at an average followup of 10 years [4]. Definite healing was concluded radiographically in 18 of 20 hips with no cases of implant migration. Six patients demonstrated nonprogressive radiolucent lines, one patient sustained partial sciatic nerve palsy, and five patients sustained one or more dislocations. Holt and Dennis [8] reported on the use of the custom triflange device in 26 hips. In that series, however, only three of the 26 hips had a pelvic discontinuity. Two of these three pelvic discontinuities failed secondary to loss of inferior fixation in the ischium. The authors recommended caution in the use of the device without additional column plating. When taken as a whole, the current literature indicates mechanical constructs appear to provide unreliable outcomes, given the potential for fatigue and late loosening (Table 1). Recent reports recommend compression plating of the acetabular columns to reduce and stabilize the pelvis in an attempt to create a solid bony substrate for acetabular reconstruction [5, 8, 19]. One potential disadvantage of this technique is that larger surgical exposure and soft tissue stripping may lead to increased infection rates and decreased osteogenic healing potential of the remaining host bone [19, 20]. Additionally, the severity of bone loss encountered with discontinuity may result in segmental bone defects making the possibility of healing between the superior and inferior hemipelvis unlikely. In this context, we became interested in highly porous metal constructs for these difficult acetabular reconstructions. We began to use these sockets, along with particulate bone graft, when healing across a discontinuity was believed to be impaired, such as in chronic cases [17]. Theoretically, these cups offered a greater opportunity for a biologic solution, potentially leading to better patient outcomes and improved component survival.
Fig. 6.
In addition to the use of superior augments to stabilize this defect, it is imperative to obtain adequate fixation of the ischium with two screws to prevent cutout and subsequent vertical displacement.
Table 1.
Comparison of mechanical failures, revision rates, function, and complications in chronic pelvic discontinuity
| Study | Number of discontinuities/total number in series | Technique | Number of failures | Revision rate (%) | Clinical score | Complications | Followup (years) |
|---|---|---|---|---|---|---|---|
| Berry et al. [1] | 27/3505 | Antiprotusio cage, anterior-posterior plating | 4 | 33 | 16/27 (60%) satisfactory (own criteria) |
4 recurrent dislocations, 1 infection | 3 |
| DeBoer et al. [4] | 20 | Custom triflanged cage | 2 | 0 | HHS: 41 preop to 80 postop | 5 dislocations, 1 resolved nerve palsy | 10 |
| Eggli et al. [5] | 7 | Ganz ring, anterior-posterior plating | 2 | NR | HHS: 33 preop to 73 postop MP: 7.5 preop to 13.2 postop |
1 nerve palsies, 1 recurrent dislocation | 8 |
| Goodman et al. [6] | 10/61 | Antiprotusio cage | 5 | 50 | NR | 4 nerve palsies, 2 recurrent dislocations, 3 femur fractures, 2 infections | 3.3 |
| Holt and Dennis [8] | 3/26 | Custom triflanged cage | 2 | 66 | HHS: 39 preop to 78 postop | 1 nerve palsies, 1 infection | 4.5 |
| Paprosky et al. [15] | 16 | Cage, plate, allograft | 4 | 25 | MP: 3.7 preop to 6.8 postop | 1 sepsis, 4 nerve palsies, 1 dislocation | 5 |
| Sporer and Paprosky [18] | 13 | Trabecular Metal™ cup/augments, distraction | 1 | 6 | MP: 6.1 preop to 10.3 postop | 1 infection | 2.6 |
| Stiehl et al. [19] | 17 | Allograft, plates | 5 | 47 | NR | 8 dislocations, 2 resections for infection, 2 nerve palsies requiring exploration | 6.9 |
| Current study | 20 | Trabecular Metal™ cup/augments, distraction | 1 | 5 (5 patients lost to followup) |
MP: 3.3 preop to 9.6 postop | No dislocations, 1 vascular injury, 1 colonic perforation, 1 infection, 1 trochanteric fracture | 4.5 |
HHS = Harris hip score; preop = preoperatively; postop = postoperatively; MP = Merle d’Aubigné-Postel score; NR = not reported.
We previously compared the functional scores of 12 patients with pelvic discontinuities treated with porous metal sockets to 12 patients treated with a cage construct [12]. Treatment with the porous tantalum metal shell offered a reproducible and consistent improvement in pain and ambulation at an average of 2.1 years’ followup. In 2006, we produced a 2.6-year followup report of 13 patients with pelvic discontinuity treated with a porous tantalum shell. Those patients had improved Merle d’Aubigné-Postel scores from 6.1 to 10.3 [18]. The current study found a mean improvement of the Merle d’Aubigné-Postel pain and ambulation score of 6.6 (3.3 preoperatively to 9.6 postoperatively). These findings corroborate our previous work from 2006 [18] and demonstrate a major improvement in function with this technique at 4.5-year followup.
With regard to complications in our series, no patient has sustained a postoperative dislocation and only one developed a superficial infection. This is markedly decreased compared to our series of patients with posterior column plating and acetabular cage reconstruction [15]. This may be due to decreased surgical time and minimization of soft tissue stripping with the less extensive dissection. A series of seven patients reported on complications in pelvic discontinuity treated with pelvic plating and acetabular reinforcement ring [5]. One patient sustained incomplete sciatic nerve palsy, one developed recurrent dislocation, and one required revision for aseptic loosening. Another series of 17 pelvic discontinuities were treated with bulk allograft in conjunction with anterior and posterior column pelvic plating [19]. That study reported a high complication rate, including eight dislocations, three infected hips, four loosenings, two sciatic palsies, and an overall reoperation rate of 47%. Reconstruction of chronic pelvic discontinuity with extensive bone loss is fraught with difficulty and complications will occur; our series had only one rerevision due to early mechanical failure. We did not encounter other mechanical failures but did have three complications necessitating further surgery: one vascular injury, one colonic perforation (ileus), and one superficial infection. There was also one greater trochanteric fracture that was treated nonoperatively and remains asymptomatic at latest followup.
In conclusion, acetabular distraction for chronic pelvic discontinuity shows promise in obtaining reliable and durable fixation. To achieve long-term durability, the pelvis must be stabilized to allow primary bone healing of the discontinuity, or this alternative method to bridge the discontinuity may be utilized. Ultimately, both the superior and inferior portions of the pelvis must achieve independent growth into the porous tantalum component for success. In this series of chronic pelvic discontinuities, acetabular distraction provided a more predictable survivorship, an improvement in clinical function, and a decreased reoperation rate for mechanical failure.
Acknowledgments
The authors thank Andrew Michael, MD, Rush University Medical Center, for his participation in this work.
Footnotes
One of the authors (SMS) certifies that he has received or may receive payments or benefits, during the study period, an amount of $10,000 to $100,000, from Zimmer Inc (Warsaw, IN, USA). One of the authors (WGP) certifies that he has received or may receive payments or benefits, during the study period, an amount of $100,001 to $1,000,000, from Zimmer Inc.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Rush University Medical Center (Chicago, IL, USA) and Central Dupage Hospital (Winfield, IL, USA).
References
- 1.Berry DJ, Lewallen DG, Hanssen AD, Cabanela ME. Pelvic discontinuity in revision total hip arthroplasty. J Bone Joint Surg Am. 1999;81:1692–1702. doi: 10.2106/00004623-199912000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Bradford MS, Paprosky WG. Acetabular defect classification: a detailed radiographic approach. Semin Arthroplasty. 1995;6:76–85. [PubMed] [Google Scholar]
- 3.d’Aubigné RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475. [PubMed] [Google Scholar]
- 4.DeBoer DK, Christie MJ, Brinson MF, Morrison JC. Revision total hip arthroplasty for pelvic discontinuity. J Bone Joint Surg Am. 2007;89:835–840. doi: 10.2106/JBJS.F.00313. [DOI] [PubMed] [Google Scholar]
- 5.Eggli S, Müller C, Ganz R. Revision surgery in pelvic discontinuity: an analysis of seven patients. Clin Orthop Relat Res. 2002;398:136–145. doi: 10.1097/00003086-200205000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Goodman S, Sastamoinen H, Shasha N. Complications of ilio-ischial reconstruction rings in revision total hip arthroplasty. J Arthroplasty. 2004;19:436–446. doi: 10.1016/j.arth.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 7.Hansen E, Shearer D, Ries M. Does a cemented cage improve revision THA for severe acetabular defects? Clin Orthop Relat Res. 2011;469:494–502. doi: 10.1007/s11999-010-1546-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holt GE, Dennis DA. Use of custom triflanged acetabular components in revision total hip arthroplasty. Clin Orthop Relat Res. 2004;429:209–214. doi: 10.1097/01.blo.0000150252.19780.74. [DOI] [PubMed] [Google Scholar]
- 9.Howie DW, Neale SD, Stamenkov R, McGee MA, Taylor DJ, Findlay DM. Progression of acetabular periprosthetic osteolytic lesions measured with computed tomography. J Bone Joint Surg Am. 2007;89:1818–1825. doi: 10.2106/JBJS.E.01305. [DOI] [PubMed] [Google Scholar]
- 10.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 11.Laflamme GY, Alami GB, Zhim F. Cement as a locking mechanism for screw heads in acetabular revision shells: a biomechanical analysis. Hip Int. 2008;18:29–34. doi: 10.1177/112070000801800106. [DOI] [PubMed] [Google Scholar]
- 12.Paprosky WG, O’Rourke M, Sporer SM. The treatment of acetabular bone defects with an associated pelvic discontinuity. Clin Orthop Relat Res. 2005;441:216–220. doi: 10.1097/01.blo.0000194311.20901.f9. [DOI] [PubMed] [Google Scholar]
- 13.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty: a 6-year follow-up evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 14.Paprosky WG, Sekundiak TD. Total acetabular allografts. Instr Course Lect. 1999;48:67–76. [PubMed] [Google Scholar]
- 15.Paprosky WG, Sporer S, O’Rourke MR. The treatment of pelvic discontinuity with acetabular cages. Clin Orthop Relat Res. 2006;453:183–187. doi: 10.1097/01.blo.0000246530.52253.7b. [DOI] [PubMed] [Google Scholar]
- 16.Sembrano JN, Cheng EY. Acetabular cage survival and analysis of factors related to failure. Clin Orthop Relat Res. 2008;466:1657–1665. doi: 10.1007/s11999-008-0183-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sporer SM, O’Rourke M, Paprosky WG. The treatment of pelvic discontinuity during acetabular revision. J Arthroplasty. 2005;20(4 suppl 2):79–84. doi: 10.1016/j.arth.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 18.Sporer SM, Paprosky WG. Acetabular revision using a trabecular metal acetabular component for severe acetabular bone loss associated with a pelvic discontinuity. J Arthroplasty. 2006;21(6 suppl 2):87–90. doi: 10.1016/j.arth.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 19.Stiehl JB, Saluja R, Diener T. Reconstruction of major column defects and pelvic discontinuity in revision total hip arthroplasty. J Arthroplasty. 2000;15:849–857. doi: 10.1054/arth.2000.9320. [DOI] [PubMed] [Google Scholar]
- 20.Udomkiat P, Dorr LD, Won YY, Longjohn D, Wan Z. Technical factors for success with metal ring acetabular reconstruction. J Arthroplasty. 2001;16:961–969. doi: 10.1054/arth.2001.27669. [DOI] [PubMed] [Google Scholar]