Abstract
Background
Owing to concerns attributable to problems associated with metal-on-metal bearing surfaces, current evidence for the use of hip resurfacing is unclear. Survival rates reported from registries and individual studies are controversial and the limited long-term studies do not conclusively allow one to judge whether hip resurfacing is still a reasonable alternative to conventional THA.
Questions/purposes
We asked whether the long-term survival rate of hip resurfacing is comparable to that of conventional THA and certain factors can be identified that influence serum ion concentration 10 years postoperatively. We specifically assessed (1) the 10-year survivorship in the whole cohort and in male and female patients, (2) serum concentrations of metal ions in patients with hip resurfacing who had not undergone revision surgery, and (3) potential influencing factors on the serum ion concentration.
Methods
We retrospectively reviewed our first 95 patients who had 100 hip resurfacings performed from 1998 to 2001. The median age of the patients at surgery was 52 years (range, 28–69 years); 49% were men. We assessed the survival rate (revision for any reason as the end point), radiographic changes, and serum ion concentrations for cobalt, chromium, and molybdenum. The correlations between serum ion concentration and patient-related factors (age, sex, BMI, activity) and implant-related factors (implant size, cup inclination, stem-shaft angle) were investigated. The minimum followup was 9.3 years (mean, 10 years; range, 9.3–10.5 years).
Results
The 10-year survivorship was 88% for the total cohort. The overall survival rate was greater in men (93%) than in women (84%). Median serum ion levels were 1.9 μg/L for chromium, 1.3 μg/L for cobalt, and 1.6 μg/L for molybdenum. Radiolucent lines around acetabular implants were observed in 4% and femoral neck thinning in 5%.
Conclusions
Although our overall failure rate was greater than anticipated, the relatively low serum ion levels and no revisions for pseudotumors in young male patients up to 10 years postoperatively provide some evidence of the suitability of hip resurfacing in this subgroup.
Level of Evidence
Level IV, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
The 1- to 8-year (median, 3.3 years) survival rates of metal-on-metal hip resurfacing in patients with hip osteoarthritis younger than 65 years reportedly range from 96% to 100% [2, 10, 16, 25, 34, 46]. However, data from national hip registries [2, 4, 39, 45] and recent reviews [9, 29, 44, 48] show a 1.5- to fivefold increased risk for revision for resurfacing up to 8 years postoperatively when compared with conventional THA. Although the survival rates still seem comparable to those of THA in a subgroup of young male patients with appropriate bony anatomy [3, 9, 39], the long-term side effects of hip resurfacing have been debated. The main concerns are systemic risks of metal ion exposure [1], and local adverse reactions to metal debris (ARMD) [22]. Although there is theoretical concern regarding potential toxic, mutagenic, or teratogenic effects of elevated metal ion levels [41], to our knowledge, no reports of clinically relevant complications are available. The reported prevalence of ARMD, which may require revision surgery, ranges from 0.1% to 6.5% [8, 20]. However, owing to the heterogeneity of published studies with limited followups, lack of standardized inclusion criteria, and different outcome variables, it is difficult to weigh the potential advantages of hip resurfacing against these risks.
The aims of our study therefore were to (1) assess the 10-year survivorship in the whole cohort and in female and male subgroups of our first 100 consecutive hip resurfacings, (2) determine serum metal ion concentrations in patients without revision surgery, and (3) analyze influencing factors on the serum ion concentration.
Patients and Methods
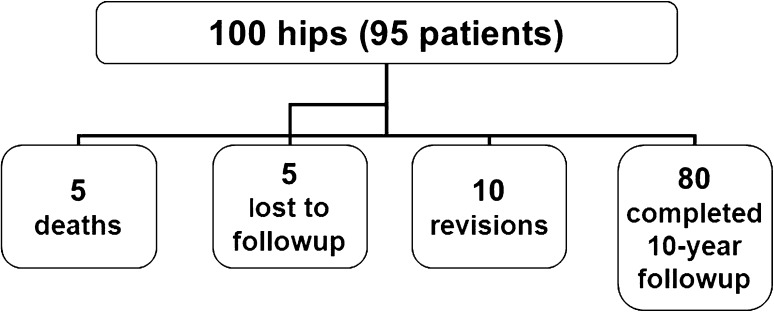
We retrospectively reviewed our first 95 patients (100 hips) who underwent hip resurfacing at our institution between September 1998 and March 2001. The indications for resurfacing surgery during that period were patient age younger than 70 years, idiopathic or secondary osteoarthritis with Kellgren-Lawrence Grades 3–4, physically active lifestyle, and good bone quality. The contraindications were massive femoral bone deformities and advanced avascular necrosis of the head. The median age of the patients at surgery was 52 years (range, 28–69 years); 49% of the patients were men (Table 1). The median BMI was 27 (range, 19–41). Owing to a high prevalence of developmental dysplasia in the East German population, 65% of our patients had secondary osteoarthritis attributable to hip dysplasia. Five patients died due to unrelated causes, with well-functioning implants in situ. Three patients who did not attend followup for personal reasons but reported having well-functioning implants in situ and two patients for whom no information could be obtained were considered lost to followup (Fig. 1). Ten patients had undergone revision surgery, leaving 75 patients (80 hips) for study. The minimum followup was 9.3 years (mean, 10 years; range, 9.3–10.5 years).
Table 1.
Patient characteristics at the time of surgery
| Variable | Results |
|---|---|
| Number of patients (women/men) | 95 (48/47) |
| Number of hips (women/men) | 100 (51/49) |
| Age (years)* | 52.0 (28–69) |
| BMI (kg/m2)* | 27.3 (19.0–41.0) |
| Preoperative Harris hip score (points)* | 50.5 (18–78) |
| Primary osteoarthritis (number of hips) | 26 |
| Secondary osteoarthritis (number of hips) | |
| Developmental dysplasia | 65 |
| Avascular necrosis | 6 |
| Tilt deformity | 3 |
* Values are expressed as median, with range in parentheses.
Fig. 1.
A flow diagram summarizes the followup status of all included patients.
Four senior surgeons performed surgery, with the majority (78%) performed by one of them (WCW). In all cases, a single FDA-approved device (Birmingham Hip® Resurfacing [BHR]; Midland Medical Technology Ltd, Birmingham, UK) and a posterior approach were used. After dislocation of the hip and removal of osteophytes, the minimal femoral head size was measured. The mean femoral head size was 50 mm (range, 42–58 mm). Then the acetabulum was reamed in 2-mm steps up to the determined cup size, followed by implantation of the cementless monoblock cup. After preparation of the femur, the head cap was cemented using low-viscosity cement (Simplex®; Stryker GmbH & Co KG, Freiburg, Germany), and a bone marrow suction device for drying the femoral head was applied. Finally, ROM and stability were checked, and the wound was closed in layers.
Postoperatively, patients were allowed to mobilize with pain-adjusted full weightbearing from the first day. All patients received daily physiotherapy during the 4 to 7 days as an inpatient with muscle strengthening and gait exercises. This was continued less frequently after discharge unless patients attended an ambulant or inpatient rehabilitation program for 3 weeks. Patients were advised to use crutches for 4 to 6 weeks.
Clinical investigation (Harris hip score [HHS]) and radiographic imaging (AP view of the pelvis and lateral view) were performed preoperatively and during routine followups at 6 weeks, 3 months, and then every year up to 5 years after surgery.
For this study, we performed an additional review at 10 years postoperatively (range, 9.3–10.5 years). We obtained clinical and radiographic assessments and serum ion analysis for all 75 patients except three for whom we had only the questionnaire-based responses. We again calculated the HHS [18] and used the UCLA activity scale to evaluate hip scoring system assessment of current physical activity [6]. During the clinical examination, we recorded groin pain by performing an impingement test (internal rotation of the hips in 90° flexion and adduction) and asked for any history of groin pain indicative of hip impingement. For all patients who had undergone revision surgery, we obtained detailed information about the reason for failure and subsequent procedures.
We obtained an AP view of the pelvis and a lateral view of the surgically treated hip. One observer (KPG) experienced in interpreting radiographs after THA and hip resurfacing assessed all radiographs. Implant position (cup inclination, metaphyseal stem-femoral shaft angle) and the presence of neck thinning (latest radiograph compared with the first postoperative and further available radiographs) were recorded. Acceptable intraobserver reliability of implant position measurements in hip resurfacing has been reported [36, 40]. Signs of radiolucency or osteolysis were identified in three zones around the short metaphyseal stem and the acetabular component as described by Amstutz et al. [3].
For metal ion analysis, blood samples were collected in 7.5-mL S-Monovette® tubes for trace metal analysis (Sarstedt AG & Co, Nümbrecht, Germany), using a specific steel needle for trace metal analysis (Sarstedt). Plasma was separated by centrifugation within 1 hour and stored at −20°C before being analyzed for chromium, cobalt, and molybdenum content using a Hitachi Z-8270 graphite furnace atomic absorption spectrometer with polarized Zeeman absorption (Hitachi Ltd, Tokyo, Japan) [26, 38]. The accuracy and precision of the method are validated to less than 10% using the control material SeronormTM Trace Elements Serum (SERO AS, Billingstad, Norway). The detection limit of the method is estimated at 0.5 μg/L for each element (mean + 3 SDs from buffer). The Dixon test was used to eliminate aberrant values. All probes having ion levels less than the detection levels were adjusted to less than 0.25 μg/L. There is no reliable information regarding the relationship of wear debris, height of serum ion values, and extent of tissue destruction. We nevertheless defined a cutoff level of 10 μg/L of chromium and/or cobalt serum ion concentration, above which we obtain CT to search for pseudotumors. Independent from the current study, this protocol applies to our followup regime for all patients with previous metal-on-metal arthroplasty.
If not stated otherwise, numerical calculations are given as medians and ranges (minimum, maximum). Survivorship was calculated on the basis of the time between initial surgery and revision as the end point with CIs in accordance with Murray et al. [31]. We compared survivorship between male and female patients using a log-rank test. To investigate possible contributing factors for metal ion concentrations, the dataset was analyzed by a linear regression model based on the two different metal ion concentrations (chromium and cobalt). Age, sex (female versus male), BMI, patient activity at followup, acetabular cup inclination, metaphyseal stem-femoral shaft angle, and size of femoral implant were analyzed as potential predictive factors for serum ion levels. Statistical analyses were performed with SPSS® software (Version 19.0; SPSS Inc, Chicago, IL, USA).
Results
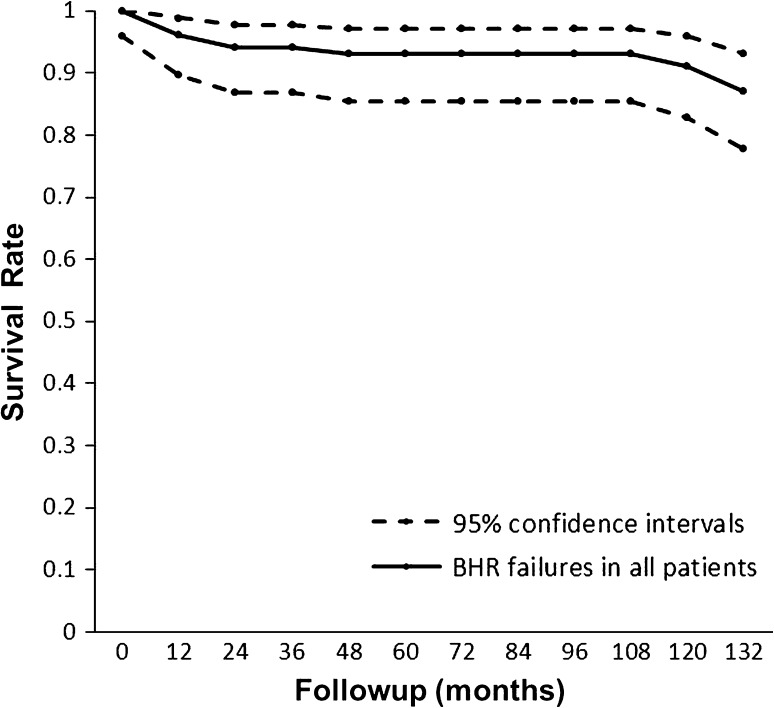
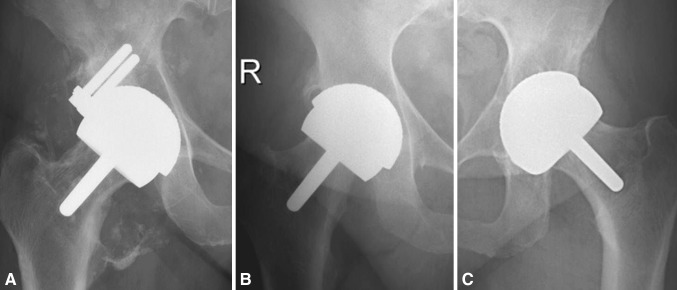
The 10-year survivorship for revision for any cause was 88% (95% CI, 77.7%–93.1%) in the whole cohort (Fig. 2). Separate calculation for male and female patients showed 10-year survival rates of 93% (95% CI, 80.3%–98.9%) and 84% (95% CI, 65.9%–91.6%), respectively (p = 0.292). For the first 7 years, the two groups had similar survival, but they differed at followup of more than 10 years. Ten patients (seven women, three men) had revision surgery. Eight patients underwent conversion to THA (two with infections, one with a neck fracture, three with pseudotumors, two with aseptic loosening), and two additional patients needed isolated revision of the acetabular component (one with psoas impingement, one with cup loosening). Three revisions were performed within the first month postoperatively (one patient with infection, one with neck fracture, one with cup loosening) and three additional revisions were performed within 4 years postoperatively (one patient with infection, one with psoas impingement, one with aseptic loosening). Three male patients and three female patients were included in this group with early to intermediate revision. In another four female patients, revisions were performed 10.2 to 10.5 years postoperatively (three pseudotumors, one aseptic loosening). All pseudotumors occurred in women aged 53 to 58 years at surgery. All had received a relatively small implant (46-mm head size), and their acetabular cup inclinations were 40° (Fig. 3A), 42° (Fig. 3B), and 62° (Fig. 3C).
Fig. 2.
A Kaplan-Meier survival curve for all 100 hips (revision for any reason as the end point) shows the 10-year survivorship was 88% (95% CI, 77.7%–93.1%). The dotted lines represent upper and lower limits of the 95% CI.
Fig. 3A–C.
The latest hip radiographs of three patients before revision for pseudotumor formation are shown. (A) This radiograph shows the hip of a 69-year-old woman with 40° cup inclination, periprosthetic osteolysis, and disseminated calcification 10.5 years after surgery. (B) A 64-year-old woman has a cup inclination of 42° and small osteolysis at the craniolateral margin 10.5 years after resurfacing of her hip. (C) A 66-year-old woman has an acetabular cup inclination of 62° and osteolysis in the acetabular roof 10.2 years after surgery.
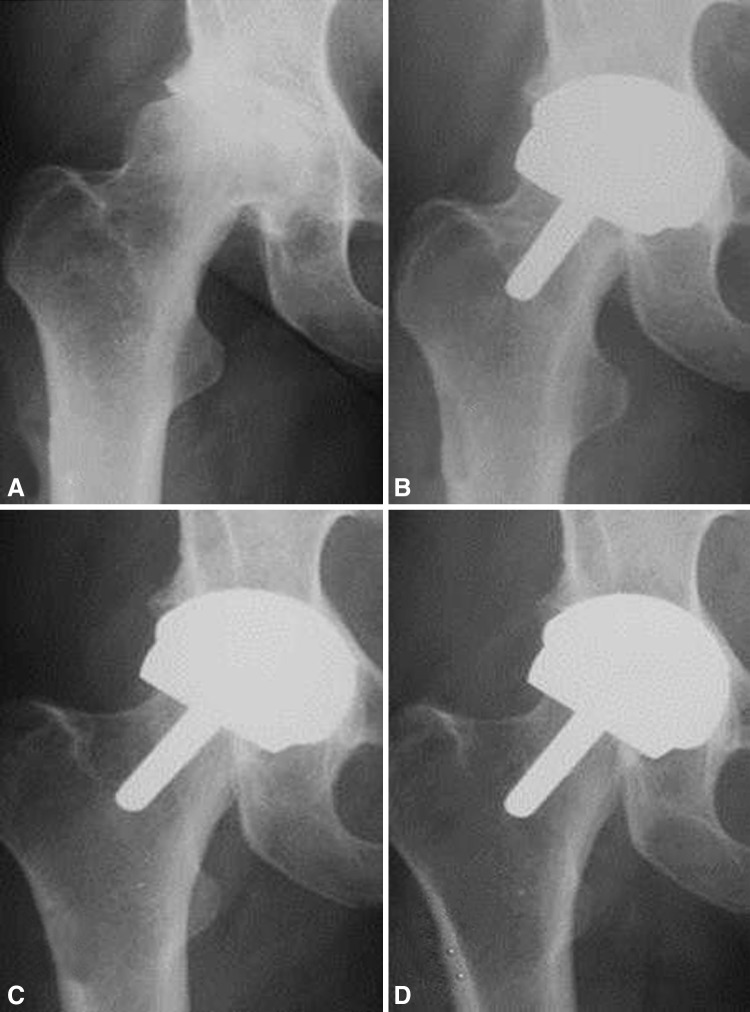
In the patients who had not undergone revision, the median HHS increased from 51 points (range, 18–78 points) preoperatively to 94 points (range, 48–100 points) at 10 years’ followup (Table 2). The median postoperative UCLA activity score was 6 (range, 5–7). We found a median cup inclination of 46° (range, 34°–64°) and a median metaphyseal stem-femoral shaft angle of 138° (range, 113°–158°). We observed periprosthetic radiolucencies in the cohort without revision in two hips (limited to < 10 mm at the inferior edge of the acetabular cup). No periprosthetic radiolucency around the short metaphyseal stem was found, but six patients showed radiographic signs of neck thinning within the first 5 postoperative years. All of them were nonprogressive up to 10 years’ followup (Fig. 4).
Table 2.
Postoperative results of clinical and radiographic examinations
| Variable | All patients | Female patients | Male patients | p value | Test |
|---|---|---|---|---|---|
| Harris hip score* (points) | 94 (48–100) | 93 (59–99) | 96 (48–100) | 0.063 | Wilcoxon |
| UCLA* activity score (points) | 6 (5–7) | 6 (5–7) | 7 (6–7) | 0.084 | Wilcoxon |
| Hip impingement positive (number) | 0 | 0 | 0 | ||
| Cup inclination* (°) | 46 (34–64) | 46 (33–60) | 47 (34–62) | 0.812 | Wilcoxon |
| Metaphyseal stem-femoral shaft angle* (°) | 138 (113–158) | 138 (113–150) | 138 (114–158) | 0.644 | Wilcoxon |
| Cup radiolucencies (number) | 3 | 1 | 2 | 1.000 | Chi-square; Fisher |
| Stem radiolucencies (number) | 0 | 0 | 0 | ||
| Neck thinning (number) | 4 | 3 | 1 | 0.615 | Chi-square; Fisher |
* Values are expressed as median, with range in parentheses.
Fig. 4A–D.
(A) A preoperative hip radiograph shows the hip of a 53-year-old woman. Between (B) the immediate postoperative radiograph and (C) the control at 4 years postoperatively, narrowing of the femoral neck could be observed, (D) which did not continue as observed at the 10-year followup.
Median serum ion levels after 10 years were 1.9 μg/L (range, 0.5–151.5 μg/L) for chromium, 1.3 μg/L (0.5–285.3 μg/L) for cobalt, and 1.6 μg/L (0.5–7.1 μg/L) for molybdenum. Twelve patients (14 hips) had chromium serum levels greater than 5 μg/L, of which six patients (seven hips) had levels greater than 10 μg/L. Ten patients (12 hips) had cobalt serum levels greater than 5 μg/L, with four patients (four hips) of these patients having levels greater than 10 μg/L.
We identified one factor predicting high serum ion concentrations (Table 3): high cup inclination was associated with high cobalt levels. No factors predicted high serum chromium ion concentrations (Table 4).
Table 3.
Linear regression analysis based on cobalt ion concentration
| Factor | Odds ratio | CI | p value |
|---|---|---|---|
| BMI | 0 | −0.14 to 0.15 | 0.950 |
| Age at the time of surgery | 0.02 | -0.01 to 0.01 | 0.619 |
| Cup inclination | 0.19 | 0.06 to 0.32 | 0.050 |
| Cup size | −0.006 | −0.03 to 0.01 | 0.486 |
| Shaft angle | −0.006 | −0.01 to 0 | 0.065 |
| Sex | −0.032 | 0.53 to 3.6 | 0.661 |
| UCLA activity | −0.026 | −0.06 to 0.01 | 0.157 |
Table 4.
Linear regression analysis based on chromium ion concentration
| Factor | Odds ratio | CI | p value |
|---|---|---|---|
| BMI | 0.19 | 0 to 0.04 | 0.051 |
| Age at the time of surgery | 0.01 | 0 to 0.02 | 0.056 |
| Cup inclination | 0.13 | −0.04 to 0.29 | 0.137 |
| Cup size | −0.01 | −0.03 to 0.01 | 0.421 |
| Shaft angle | −0.001 | −0.01 to 0.01 | 0.876 |
| Sex | 0.06 | −0.13 to 0.25 | 0.523 |
| UCLA activity | −0.01 | −0.06 to 0.04 | 0.599 |
Discussion
Throughout the last decade, hip resurfacing has regained popularity owing to the introduction of new metal-on-metal implants and advanced surgical procedures, which seemed to have solved previous problems with this technique [28, 30]. Encouraging short- and medium-term results have been reported, with low failure rates and high patient satisfaction [2, 10, 16, 35, 46, 50]. However, concerns regarding the long-term survival and safety have been raised due to the potential risks of metal hypersensitivity and increased serum levels of metal ions [1, 14, 17, 19, 23]. To weigh the potential benefits of hip resurfacing against the inherent risks of this alternative treatment compared with conventional THA, it is necessary to collect appropriate data from patient cohorts with sufficient followups. The purposes of our investigation therefore were to (1) determine the 10-year survival in a consecutive series of our first 100 consecutive hip resurfacings, (2) evaluate serum metal ion concentrations in patients without revision surgery, and (3) analyze potential influencing factors on the serum ion concentration.
Our study has some limitations. First, our series involves our initial experience with this new technology. Four surgeons performed the procedures and it must be assumed all cases fell into their learning curve. We know the outcome of hip resurfacing is substantially influenced by technical details of the surgical procedure [7, 41, 42], which has an impact on the surgeon’s experience [35, 43]. Nevertheless, we have included all patients from the beginning, reflecting the actual results of an innovative surgical treatment. Second, we have a limited radiographic analysis of structural changes. Although performed in a blinded order to avoid bias, all measurements were made by one reader (KPG). We did not assess the reliability of his assessment, but he is experienced in reading radiographs of hip resurfacing, and a generally acceptable intrarater reliability has been documented in other studies [36, 40]. Third, we performed no studies to observe local soft tissue reactions to metallic debris on plain radiographs. Metal artifacts impair the application of MRI, and we did not want to expose our patients to additional ionization through CT. There are some studies in which ultrasonography was used either alone [27] or in combination with MRI and CT [20, 37] to assess the frequency of pseudotumor formation after hip resurfacing. As sensitivity and reliability of this observer-influenced imaging technique are not proven for ARMD, we did not include it in this study. Instead, we performed serum ion measurement at followup, as substantially elevated levels can be considered valid surrogate parameters of resurfacing failure [13, 21, 24]. However, we cannot determine the true incidence of ARMD.
The first purpose of our study was to determine the 10-year survival of resurfacing in our total cohort and in female and male patient subgroups. The number of studies of hip resurfacing with similar followup is limited [3, 5, 11, 47] (Table 5), and all of them are single-surgeon series. Only two [33, 48] reported a revision rate less than 10% after 10 years, which some authors regard as the current benchmark of satisfactory performance of a primary [33, 48]. The overall survival rate of 88% in our patient group does not meet this full 10-year benchmark, although we could observe a superior survival rate of 93% in a cohort of male patients. A revision rate of 7% after 10 years is close to the reported results for conventional THA in male patients younger than 65 years from the Australian hip registry (5.0–6.2 cumulative percent revision at 9 years) [4]. Nevertheless, the survival in our female patient cohort was only 84%. One conversion attributable to early femoral neck fracture and all revisions attributable to ARMD were performed in this group. It is known the higher revision rate in female patients might be related to differences in the proportion of males and females who receive smaller sizes of femoral components [39, 43]. Women, however, seem to have a greater incidence of pseudotumor formation than men [14], which might be attributed to mechanical and nonmechanical factors [32]. Therefore, we now rarely offer hip resurfacing to female patients.
Table 5.
Comparison of Kaplan-Meier survival rates for hip resurfacing
| Study | Number of hips (type of implant) | Number of surgeons | Mean followup (years) | Kaplan-Meier survival rate* (95% CI) |
|---|---|---|---|---|
| Amstutz et al. [3] | 100 (Conserve® Plus) | 1 | 11.7 (10.8–12.9) | 88.5% (80.2%–93.6%)§ |
| Daniel et al. [11] | 107 (BHR†) | 1 1 |
10.6 (10.0–11.4) | 93.0% (92.2%–99.8%) 86.0% (80.5%–91.5%) |
| 184 (BHR‡) | 10.5 (10.0–11.1) | |||
| Baker et al. [5] | 63 (BHR) | 1 | 9.0 (8.2–10.3) | Not calculated |
| Treacy et al. [47] | 144 (BHR) | 1 | 10.8 (10.2–12.2) | 93.5% (89.2%–97.6%) |
| Current study | 100 (BHR) | 4 | 10.0 (9.3–10.5) | 87.8% (77.7%–93.1%) |
* All calculations are based on the assumption that patients lost to followup have not undergone revision; †with single thermal treatment of either hot isostatic pressing or solution heat treatment after being cast; ‡with double heat treatment after casting; §survival rate calculated at 10 years’ followup; BHR = Birmingham Hip® Resurfacing.
In addition to calculation of implant survivorship, potential radiographic signs of implant failure or stress shielding might show revision will be needed in the future. After 10 years, we observed a low rate of radiolucency and osteolysis in nonrevised implants and a low number of patients with femoral neck thinning. These positive results were confirmed in similar cohorts after BHR implantation [11, 47]. In contrast, Baker et al. [5] observed a considerable number of progressive radiographic changes and even migrations in their patients who had undergone surgery with the same implant. The reason for these different findings and the probability of incident radiographic changes in the future is uncertain.
The second purpose of our study was to evaluate serum metal ion concentrations in patients with clinically well-functioning hip resurfacings 10 years after implantation. At followup, the median serum ion levels for chromium, cobalt, and molybdenum were only slightly elevated above the normal reference values of our laboratory (0.5 μg/L). Only six patients showed serum ion levels of chromium and cobalt greater than 10 μg/L. We are obtaining regular MRIs on these six patients and none to date have signs of pseudotumor formation. However, we currently cannot determine the incidence in the remaining patients or the potential for development of ARMD in the future. A serum ion level for chromium and cobalt less than 10 μg/L does not exclude the risk of localized ARMD, systemic toxicity, or carcinogenicity, which are additional concerns of resurfacing [1, 41]. There currently is no generally agreed on unacceptable threshold for metal ion concentrations in body fluids. Therefore, it is necessary to obtain more information from future clinical studies with larger numbers of patients and appropriate followup to determine the true incidence of metal-related local and systemic complications.
Our third purpose was to analyze whether there is an association between patient- and implant-related characteristics and the serum ion concentration. Several studies have shown type [15, 21, 23] and positioning of implants [13, 15, 19] and component size [13, 15] can influence serum ion concentrations. With decreasing cup size and increasing inclination, the serum chromium and cobalt concentrations are increased. Evidence is less convincing for age [13] and sex [19], as only a few investigators have analyzed these factors and/or could identify positive associations. The results for physical activity are controversial, as some studies report positive associations [13, 24] and some report negative associations [12, 49]. We identified high cup inclination in our cohort as a predictor for elevated cobalt levels, and we found no predictors for elevated chromium levels. This is in agreement with several studies [13, 15, 19, 22] that found a positive correlation between high cup inclination and increased metal ion concentrations. As most studies [13, 19, 24] have looked at a limited number of factors that potentially might influence the release of serum ions, it is difficult to discuss the relevance of our findings. Due to the limited number of patients with elevated metal ion levels in our series, the statistical analysis may have been biased. However, no other study currently is available with results of serum ion analysis after 10 years of followup. Most of the published data were obtained in investigations with short- and medium-term followups [12, 19, 20, 49] although metal ion release of hip resurfacing implants regularly decreases after the initial running-in phase [49].
Our data confirm observations from other studies that the survival rate of hip resurfacing in male patients with appropriate bone quality can be similar to the outcome after conventional THA, at least after 10 years of followup. However, the low rate of osteolysis and metal-associated radiographic disorders should be interpreted cautiously as we cannot determine future developments in patients with elevated serum ion levels, even taking into account that there currently are only a small number of patients with substantially elevated serum ion levels. Although we could identify only limited evidence for cup inclination as predictor of serum ion elevation, we support other reported risk factors for a bad outcome (ie, cup size, sex). Our conclusion currently is to restrict resurfacing to a carefully selected cohort (male patients with sufficiently large cup size) and try to obtain the best possible component position.
Acknowledgments
We thank our medical documentation assistants, Heike Voigt, Brit Brethfeld, and Susann Pohle, for assistance in collecting data. We also thank Gerd Dinnebier MD for his methodologic support with serum ion measurement.
Footnotes
The institution of one or more of the authors has received, in any 1 year, funding from Aesculap AG & Co KG, Tuttlingen, Germany (JL), Mathys AG, Bettlach, Switzerland (JL, SK), Smith & Nephew GmbH, Marl, Germany (JL, KPG, WCW), Stryker GmbH & Co KG, Freiburg, Germany (JL, SK, KPG), Zimmer GmbH, Winterthur, Switzerland (KPG, SK), and Deutsche Arthrose-Hilfe, Frankfurt/Main, Germany (KPG, SK).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the University Hospital Carl Gustav Carus Dresden, Dresden, Germany.
References
- 1.Akbar M, Brewer JM, Grant MH. Effect of chromium and cobalt ions on primary human lymphocytes in vitro. J Immunotoxicol. 2011;8:140–149. doi: 10.3109/1547691X.2011.553845. [DOI] [PubMed] [Google Scholar]
- 2.Amstutz HC, Beaule PE, Dorey FJ, Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86:28–39. [PubMed] [Google Scholar]
- 3.Amstutz HC, Duff MJ, Campbell PA, Gruen TA, Wisk LE. Clinical and radiographic results of metal-on-metal hip resurfacing with a minimum ten-year follow-up. J Bone Joint Surg Am. 2010;92:2663–2671. doi: 10.2106/JBJS.I.01715. [DOI] [PubMed] [Google Scholar]
- 4.Australian Orthopaedic Association National Joint Replacement Registry. Hip and Knee Arthroplasty, Annual Report 2010. Available at: http://www.dmac.adelaide.edu.au/aoanjrr/publications.jsp?section=reports2010. Accessed June 5, 2011.
- 5.Baker RP, Pollard TC, Eastaugh-Waring SJ, Bannister GC. A medium-term comparison of hybrid hip replacement and Birmingham hip resurfacing in active young patients. J Bone Joint Surg Br. 2011;93:158–163. doi: 10.1302/0301-620X.93B2.25625. [DOI] [PubMed] [Google Scholar]
- 6.Beaule PE, Dorey FJ, Hoke R, Le DM, Amstutz HC. The value of patient activity level in the outcome of total hip arthroplasty. J Arthroplasty. 2006;21:547–552. doi: 10.1016/j.arth.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Beaule PE, Dorey FJ, Duff MJ, Gruen T, Amstutz HC. Risk factors affecting outcome of metal-on-metal surface arthroplasty of the hip. Clin Orthop Relat Res. 2004;418:87–93. doi: 10.1097/00003086-200401000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Beaule PE, Kim PR, Powell J, Mackenzie J, Werle J, Antoniou J, Huk O, Vendittoli PA, Lavigne M, Smith F, Naudie D, McCalden R, Bourne R, Schemitsch E, Garbuz D, Greidanus N, Duncan C, Canadian Hip Resurfacing Study Group A survey on the prevalence of pseudotumors with metal-on-metal hip resurfacing in Canadian academic centers. J Bone Joint Surg Am. 2011;93(suppl 2):118–121. doi: 10.2106/JBJS.J.01848. [DOI] [PubMed] [Google Scholar]
- 9.Corten K, MacDonald SJ. Hip resurfacing data from national joint registries: what do they tell us? What do they not tell us? Clin Orthop Relat Res. 2010;468:351–357. doi: 10.1007/s11999-009-1157-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184. doi: 10.1302/0301-620X.86B2.14600. [DOI] [PubMed] [Google Scholar]
- 11.Daniel J, Ziaee H, Kamali A, Pradhan C, Band T, McMinn DJ. Ten-year results of a double-heat-treated metal-on-metal hip resurfacing. J Bone Joint Surg Br. 2010;92:20–27. doi: 10.2106/JBJS.H.01821. [DOI] [PubMed] [Google Scholar]
- 12.Daniel J, Ziaee H, Pradhan C, McMinn DJ. Six-year results of a prospective study of metal ion levels in young patients with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2009;91:176–179. doi: 10.1302/0301-620X.91B2.21654. [DOI] [PubMed] [Google Scholar]
- 13.Desy NM, Bergeron SG, Petit A, Huk OL, Antoniou J. Surgical variables influence metal ion levels after hip resurfacing. Clin Orthop Relat Res. 2011;469:1635–1641. doi: 10.1007/s11999-010-1636-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glyn-Jones S, Pandit H, Kwon YM, Doll H, Gill HS, Murray DW. Risk factors for inflammatory pseudotumour formation following hip resurfacing. J Bone Joint Surg Br. 2009;91:1566–1574. doi: 10.1302/0301-620X.91B12.22287. [DOI] [PubMed] [Google Scholar]
- 15.Griffin WL, Nanson CJ, Springer BD, Davies MA, Fehring TK. Reduced articular surface of one-piece cups: a cause of runaway wear and early failure. Clin Orthop Relat Res. 2010;468:2328–2332. doi: 10.1007/s11999-010-1383-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grigoris P, Roberts P, Panousis K. The development of the Durom™ metal-on-metal hip resurfacing. Hip Int. 2006;16(suppl 4):65–72. doi: 10.1177/112070000601604S13. [DOI] [PubMed] [Google Scholar]
- 17.Haddad FS, Thakrar RR, Hart AJ, Skinner JA, Nargol AV, Nolan JF, Gill HS, Murray DW, Blom AW, Case CP. Metal-on-metal bearings: the evidence so far. J Bone Joint Surg Br. 2011;93:572–579. doi: 10.1302/0301-620X.93B4.26429. [DOI] [PubMed] [Google Scholar]
- 18.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 19.Hart AJ, Skinner JA, Henckel J, Sampson B, Gordon F. Insufficient acetabular version increases blood metal ion levels after metal-on-metal hip resurfacing. Clin Orthop Relat Res. 2011;469:2590–2597. doi: 10.1007/s11999-011-1930-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kwon YM, Ostlere SJ, Lardy-Smith P, Athanasou NA, Gill HS, Murray DW. “Asymptomatic” pseudotumors after metal-on-metal hip resurfacing arthroplasty: prevalence and metal ion study. J Arthroplasty. 2011;26:511–518. doi: 10.1016/j.arth.2010.05.030. [DOI] [PubMed] [Google Scholar]
- 21.Langton DJ, Jameson SS, Joyce TJ, Gandhi JN, Sidaginamale R, Merredy P, Lord J, Nargol AV. Accelerating failure rate of the ASR total hip replacement. J Bone Joint Surg Br. 2011;93:1011–1016. doi: 10.1302/0301-620X.93B8.26040. [DOI] [PubMed] [Google Scholar]
- 22.Langton DJ, Jameson SS, Joyce TJ, Hallab NJ, Natu S, Nargol AV. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: a consequence of excess wear. J Bone Joint Surg Br. 2010;92:38–46. doi: 10.1302/0301-620X.92B1.22770. [DOI] [PubMed] [Google Scholar]
- 23.Langton DJ, Joyce TJ, Jameson SS, Lord J, Orsouw M, Holland JP, Nargol AV, De Smet KA. Adverse reaction to metal debris following hip resurfacing: the influence of component type, orientation and volumetric wear. J Bone Joint Surg Br. 2011;93:164–171. doi: 10.1302/0301-620X.93B2.25099. [DOI] [PubMed] [Google Scholar]
- 24.Langton DJ, Sprowson AP, Joyce TJ, Reed M, Carluke I, Partington P, Nargol AV. Blood metal ion concentrations after hip resurfacing arthroplasty: a comparative study of articular surface replacement and Birmingham Hip Resurfacing arthroplasties. J Bone Joint Surg Br. 2009;91:1287–1295. doi: 10.1302/0301-620X.91B10.22308. [DOI] [PubMed] [Google Scholar]
- 25.Lingard EA, Muthumayandi K, Holland JP. Comparison of patient-reported outcomes between hip resurfacing and total hip replacement. J Bone Joint Surg Br. 2009;91:1550–1554. doi: 10.1302/0301-620X.91B12.22326. [DOI] [PubMed] [Google Scholar]
- 26.Lugowski SJ, Smith DC, McHugh AD, Loon JC. Determination of chromium, cobalt and molybdenum in synovial fluid by GFAAS. J Trace Elem Electrolytes Health Dis. 1991;5:23–29. [PubMed] [Google Scholar]
- 27.McArthur JR, Costa M, Griffin DR, Krikler SJ, Parsons N, Foguet PR. Groin pain following hip resurfacing: a case-control study. Hip Int. 2011;21:602–609. doi: 10.5301/HIP.2011.8688. [DOI] [PubMed] [Google Scholar]
- 28.McBryde CW, Revell MP, Thomas AM, Treacy RB, Pynsent PB. The influence of surgical approach on outcome in Birmingham Hip Resurfacing. Clin Orthop Relat Res. 2008;466:920–926. doi: 10.1007/s11999-008-0121-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McGrory B, Barrack R, Lachiewicz PF, Schmalzried T, Yates AJ, Watters WC, Turkelson CM, Wies JL, Andre JS. Modern metal-on-metal hip resurfacing. J Am Acad Orthop Surg. 2010;18:306–314. doi: 10.5435/00124635-201005000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Mont MA, Seyler TM, Ulrich SD, Beaule PE, Boyd HS, Grecula MJ, Goldberg VM, Kennedy WR, Marker DR, Schmalzried T, Sparling EA, Vail TP, Amstutz HC. Effect of changing indications and techniques on total hip resurfacing. Clin Orthop Relat Res. 2007;465:63–70. doi: 10.1097/BLO.0b013e318159dd60. [DOI] [PubMed] [Google Scholar]
- 31.Murray DW, Carr AJ, Bulstrode C. Survival analysis of joint replacements. J Bone Joint Surg Br. 1993;75:697–704. doi: 10.1302/0301-620X.75B5.8376423. [DOI] [PubMed] [Google Scholar]
- 32.Murray DW, Grammatopoulos G, Gundle R, Gibbons CL, Whitwell D, Taylor A, Glyn-Jones S, Pandit HG, Ostlere S, Gill HS, Athanasou N, McLardy-Smith P. Hip resurfacing and pseudotumour. Hip Int. 2011;21:279–283. doi: 10.5301/HIP.2011.8405. [DOI] [PubMed] [Google Scholar]
- 33.National Institute for Clinical Excellence. Guidance on the selection of prostheses for primary total hip replacement (TA2). Available at: http://www.nice.org.uk. Accessed October 8, 2011.
- 34.Nishii T, Sugano N, Miki H, Takao M, Koyama T, Yoshikawa H. Five-year results of metal-on-metal resurfacing arthroplasty in Asian patients. J Arthroplasty. 2007;22:176–183. doi: 10.1016/j.arth.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 35.Nunley RM, Zhu J, Brooks PJ, Engh CA, Raterman SJ, Rogerson JS, Barrack RL. The learning curve for adopting hip resurfacing among hip specialists. Clin Orthop Relat Res. 2010;468:382–391. doi: 10.1007/s11999-009-1106-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Olsen M, Davis ET, Gallie PA, Waddell JP, Schemitsch EH. The reliability of radiographic assessment of femoral neck-shaft and implant angulation in hip resurfacing arthroplasty. J Arthroplasty. 2009;24:333–340. doi: 10.1016/j.arth.2008.01.304. [DOI] [PubMed] [Google Scholar]
- 37.Pandit H, Glyn-Jones S, McLardy-Smith P, Gundle R, Whitwell D, Gibbons CL, Ostlere S, Athanasou N, Gill HS, Murray DW. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2008;90:847–851. doi: 10.1302/0301-620X.90B7.20213. [DOI] [PubMed] [Google Scholar]
- 38.Prohaska C, Pomazal K, Steffan I. ETAAS method for the determination of Cd, Cr, Cu, Mn and Se in blood fractions and whole blood. Fresenius J Anal Chem. 2000;368:627–632. doi: 10.1007/s002160000520. [DOI] [PubMed] [Google Scholar]
- 39.Prosser GH, Yates PJ, Wood DJ, Graves SE, Steiger RN, Miller LN. Outcome of primary resurfacing hip replacement: evaluation of risk factors for early revision. Acta Orthop. 2010;81:66–71. doi: 10.3109/17453671003685434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reito A, Puolakka T, Paakkala A, Pajamaki J. Assessment of inter- and intra-observer reliability in the determination of radiographic version and inclination of the cup in metal-on-metal hip resurfacing. Int Orthop. 2012;36:519–525. doi: 10.1007/s00264-011-1328-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shimmin A, Beaule PE, Campbell P. Metal-on-metal hip resurfacing arthroplasty. J Bone Joint Surg Am. 2008;90:637–654. doi: 10.2106/JBJS.G.01012. [DOI] [PubMed] [Google Scholar]
- 42.Shimmin AJ, Back D. Femoral neck fractures following Birmingham Hip Resurfacing: a national review of 50 cases. J Bone Joint Surg Br. 2005;87:463–464. doi: 10.1302/0301-620X.87B4.15498. [DOI] [PubMed] [Google Scholar]
- 43.Smith TO, Nichols R, Donell ST, Hing CB. The clinical and radiological outcomes of hip resurfacing versus total hip arthroplasty: a meta-analysis and systematic review. Acta Orthop. 2010;81:684–695. doi: 10.3109/17453674.2010.533933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Springer BD, Connelly SE, Odum SM, Fehring TK, Griffin WL, Mason JB, Masonis JL. Cementless femoral components in young patients: review and meta-analysis of total hip arthroplasty and hip resurfacing. J Arthroplasty. 2009;24:2–8. doi: 10.1016/j.arth.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 45.Swedish Hip Arthroplasty Register. Annual Report 2008. Available at: https://www.jru.orthop.gu.se. Accessed: October 8, 2011.
- 46.Treacy RB, McBryde CW, Pynsent PB. Birmingham Hip Resurfacing arthroplasty: a minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167–170. doi: 10.1302/0301-620X.87B2.15030. [DOI] [PubMed] [Google Scholar]
- 47.Treacy RB, McBryde CW, Shears E, Pynsent PB. Birmingham Hip Resurfacing: a minimum follow-up of ten years. J Bone Joint Surg Br. 2011;93:27–33. doi: 10.1302/0301-620X.93B1.24134. [DOI] [PubMed] [Google Scholar]
- 48.Weegen W, Hoekstra HJ, Sijbesma T, Bos E, Schemitsch EH, Poolman RW. Survival of metal-on-metal hip resurfacing arthroplasty: a systematic review of the literature. J Bone Joint Surg Br. 2011;93:298–306. doi: 10.1302/0301-620X.93B3.25594. [DOI] [PubMed] [Google Scholar]
- 49.Vendittoli PA, Mottard S, Roy AG, Dupont C, Lavigne M. Chromium and cobalt ion release following the Durom high carbon content, forged metal-on-metal surface replacement of the hip. J Bone Joint Surg Br. 2007;89:441–448. doi: 10.1302/0301-620X.89B4.18054. [DOI] [PubMed] [Google Scholar]
- 50.Witzleb WC, Arnold M, Krummenauer F, Knecht A, Ranisch H, Guenther KP. Birmingham Hip Resurfacing arthroplasty: short-term clinical and radiographic outcome. Eur J Med Res. 2008;13:39–46. [PubMed] [Google Scholar]