Abstract
Background
In a previous experiment studying cementation of liners into cementless acetabular shells, placing grooves in the liner in a spider-web configuration created the greatest construct strength. Scoring shells without screw holes or other texturing helped prevent failure at the shell-cement interface. However, it was unclear whether these practices caused durable constructs in patients.
Questions/purposes
We therefore determined (1) rerevision rates; (2) functional scores (Harris hip scores, WOMAC, and SF-36); (3) acetabular loosening rates; and (4) acetabular osteolysis rates in patients in whom we cemented nonconstrained liners into well-fixed and well-positioned acetabular shells.
Methods
We prospectively followed 30 patients with 31 total hip arthroplasties in which a worn acetabular liner was revised by cementing a new liner into the existing shell that was stable and well positioned. Acetabular liners were prepared as determined by our previous study. Twenty-seven of the 30 patients (28 hips) were evaluated clinically. We recorded revisions and determined radiographic loosening and osteolysis. The minimum clinical followup was 2 years (mean, 5.3 years; range, 2–10 years). Twenty-six hips (87%) had minimum 2-year radiographic followup with an average length of 4.8 years.
Results
No hip required rerevision during the followup interval. Two hips (6%) dislocated once, both treated nonoperatively. Harris hip scores, WOMAC, and SF-36 scores increased over preoperatively at last followup. All acetabular shells and liners were radiographically stable without evidence of loosening or progressive acetabular osteolysis.
Conclusions
Cementation of a liner into a well-fixed cementless shell after scoring in a spider-web configuration provided secure fixation with no failures of the construct at average 5.3 years followup.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Study of cementless acetabular component fixation has demonstrated long-term durability with loosening rates of 1% to 2% at 20 years [5, 6]. However, wear-through of the polyethylene into the shell requiring reoperation occurs in 3% to 4% of hips long term in series in which gamma irradiated in air polyethylene or noncrosslinked polyethylene was used [1, 2]. When this occurs and the shell is both secure and well positioned, one option is to cement a new liner into the shell.
Heck and Murray [9] first described the option of cementing a replacement liner into an existing acetabular shell provided that the shell is both stable and well positioned. We previously performed a biomechanical experimental study of 10 types of shell preparation to determine an appropriate liner and shell preparation for optimal construct stability [7]. We found that placing grooves in the liner in a spider-web configuration created the greatest construct strength. Specifically, intersecting longitudinal and circumferential grooves provide torsional stability and lever-out resistance to failure, respectively. Additionally, it was determined that if the existing shell did not have screw holes or other texturing, the surgeon should score the shell to prevent failure at the shell-cement interface.
In the current study we applied these findings to prepare the acetabular constructs in cases in which we cemented liners into shells. We therefore determined (1) rerevision rates; (2) functional scores (Harris hip scores, WOMAC, and SF-36); (3) acetabular loosening rates; and (4) acetabular osteolysis rates.
Patients and Methods
We reviewed the records of all 30 patients who had undergone 31 revision hip surgeries in which a new nonconstrained liner was cemented into an existing acetabular shell that was stable and well positioned from January 2000 to January 2007. In all cases, there had been excessive wear of a modular acetabular liner that had been placed into a cementless acetabular shell.
The indications for this technique were: (1) a secure cementless acetabular shell; (2) a well-positioned acetabular shell; (3) a broken or inadequate capturing mechanism for the acetabular liner; and (4) an adequate acetabular shell diameter to allow for a 2- to 4-mm cement mantle around the new acetabular liner to be inserted. The contraindications were: (1) a loose acetabular shell; (2) a malpositioned acetabular shell; or (3) an acetabular shell with a diameter too small to allow for a 2- to 4-mm cement mantle around the new acetabular liner to be inserted. During this interval, the senior author (JJC) performed 21 additional revision THAs in which a constrained liner was cemented into a secure acetabular shell. The results of this technique using constrained liners have been previously reported [3]. Three of the 30 patients (three hips) were excluded for the following reasons: two patients had died and one patient was lost to followup. Thus, the study cohort was somewhat selected and consisted of 31 hips in 30 patients. The average age at the time of primary THA was 41 years (range, 24–64 years). The average length of time from primary THA to revision surgery with cementation of liner (index surgery) was 11 years (range, 5–21 years). The average age at the time of index revision surgery was 51 years (range, 33–77 years). Study participants included 18 women (19 hips) and 12 men (12 hips). There were 17 left hips (55%) and 14 right hips (45%). In one patient, a cemented liner was placed in both hips. The average body mass index at the time of index surgery was 31 kg/m2 (range, 19–49 kg/m2). As a result of the fact that many of the primary surgeries were performed by surgeons at outside institutions, the diagnoses before primary surgery could not be established in many cases. The reason for the index revision surgery was extensive polyethylene liner wear with impending mechanical failure. Before revision, all patients had a preoperative workup to rule out infection, including erythrocyte sedimentation rate, C-reactive protein, and aspiration of the hip when indicated. The minimum followup among living patients was 2 years (mean, 5 years; range, 2–10 years). The average age of the living patients at last followup was 56 years (range, 39–83 years). After locating patients, consent for study participation was obtained as per the protocol previously approved by the Institutional Review Board.
All surgery was performed by the senior author (JJC). The surgical approach for the index revision operation was posterolateral for all patients and included reattachment of the capsule and external rotators. Six types of acetabular shells were retained at the time of index surgery (Table 1). The acetabular orientation on preoperative radiographs as well as intraoperative inspection was between 35° and 50° of abduction and 1° and 20° of anteversion. The most common shells were HG-I (20) and HG-II (six) made by Zimmer (Warsaw, IN, USA). All hips received a new nonconstrained liner, which was either 5 mrad remelt moderately crosslinked (Marathon; DePuy, Warsaw, IN, USA) in 28 hips or 10 mrad e-beam crosslinked (Trilogy Longevity; Zimmer) in three hips during the index surgery. The outside diameter of the polyethylene liners ranged from 40 to 56 mm and the femoral head size after revision ranged from 22 to 32 mm (Table 2). Liners were chosen to allow for a 2- to 4-mm cement mantle between the outer liner and inner surface of the cementless acetabular shell once the liner was inserted. Care was taken to avoid placement of a liner that was not contained in the shell. The backs of all acetabular liners were scored in a spider-web pattern (intersecting longitudinal and circumferential grooves) to a depth of 1 to 2 mm as was determined optimal in the previously performed biomechanics study to provide lever-out and torsional stability. If the existing acetabular shell had no holes and/or a polished surface, then a high-speed burr was used to create additional scoring in a similar spider-web pattern on the inner aspect of the shell. If there were any existing screws, they were checked for stability and any loose screws were removed. The cement technique was such that doughy cement (Simplex; Howmedica, Rutherford, NJ, USA) was pressurized into a clean and dry acetabular shell with the bulb end of a large irrigation syringe. Next, the previously prepared liner was pressurized into the cement mantle. Antibiotics were routinely used in the cement. Patients began ambulating on postoperative Day 2, full weightbearing with assistive devices, and did so for 4 to 6 weeks. No other therapy was prescribed. After having two early postoperative dislocations (neither recurred), patients were either placed in braces or single-leg pantaloon casts for the first 6 weeks (there were no further dislocations).
Table 1.
Components used in primary THA
| Number of hips | |
|---|---|
| Acetabular shell | |
| HG-I | 20 |
| HG-II | 6 |
| Duraloc | 2 |
| Dow Corning Wright | 1 |
| Longevity | 1 |
| Osteonics | 1 |
| Acetabular size (mm) | |
| 42 | 1 |
| 44 | 1 |
| 48 | 4 |
| 50 | 12 |
| 52 | 7 |
| 54 | 2 |
| 56 | 3 |
| 58 | 1 |
Table 2.
Components used in index (revision) THA
| Number of hips | |
|---|---|
| Liner type | |
| Duraloc Marathon (10º) | 16 |
| Duraloc Marathon (neutral) | 8 |
| Pinnacle Marathon Bantam | 4 |
| Trilogy Longevity Crosslinked | 3 |
| Liner outer diameter (mm) | |
| 40 | 1 |
| 42 | 1 |
| 45 | 1 |
| 46 | 3 |
| 48 | 11 |
| 50 | 7 |
| 52 | 5 |
| 54 | 1 |
| 56 | 1 |
| Head diameter (mm) | |
| 22 | 3 |
| 26 | 2 |
| 28 | 24 |
| 32 | 2 |
Patients were routinely followed at 2-year intervals. An investigator (DWH) not involved in the surgical procedures and not receiving compensation from the implant manufacturer contacted all patients. Twenty-seven patients (28 hips) were known to be alive, two patients (two hips) were known to have died, and one patient (one hip) was lost to followup. Patients were evaluated clinically by outcome measures including the Harris hip score [8], the WOMAC [2], and the SF-36 score [13].
All patients were encouraged to return to the clinic for full clinical and radiographic evaluation. Radiographs including low AP of the pelvis and AP and lateral of the femur to include the hip were obtained. If the patient was unable or unwilling to return for full clinical evaluation, local or portable radiographic evaluation was arranged. Among the patients who had died, contact was made with a surviving relative in all patients to assure that no further surgeries had occurred. Twenty-six hips (87%) had minimum 2-year radiographic followup with an average length of 5 years (range, 2–11 years). Two authors (JJC, DWH) reviewed all radiographs with interpretation reported by consensus. Acetabular components were evaluated for bone-prosthesis radiolucencies, acetabular osteolysis, and acetabular component migration according to the criteria of Massin et al. [11]. Radiographic loosening of the acetabular shell was defined as the presence of a complete radiolucent line in all three zones, cup migration, or change in cup position [4].
We compared Harris hip, WOMAC, and SF-36 scores at last followup with those of the preindex revision scores using paired t-tests.
Results
No additional revision surgeries of the acetabular construct were required in any hips. Hence, survivorship for rerevision for any reason was 100%.
At last followup, the average Harris hip score was 76.8 (range, 40.7–100), which was similar to that of the prerevision score (p = 0.18). The average WOMAC scores were 86.1 (range, 20–100) for pain, 70.7 (range, 37.5–100) for stiffness, and 76.4 (range, 29.5–100) for function. Compared with the prerevision surgery scores (Table 3), we found an improvement in the WOMAC pain (p = 0.0009) and stiffness scores (p = 0.0002). At last followup, there was an increase in both the average SF-36 physical component score of 76.8 (range, 40.7–100; p = 0.022) and the mental component score of 56.5 (range, 28.7–69.9; p = 0.011) compared with prerevision scores.
Table 3.
Clinical followup in the study cohort
| Score | Average prerevision (range) | Average final followup (range) | p value |
|---|---|---|---|
| Harris hip score | 69.9 (29–99) | 76.8 (40.7–100) | 0.18 |
| WOMAC pain | 64.8 (20–100) | 86.1 (20–100) | 0.0009* |
| WOMAC stiffness | 48.6 (0–100) | 70.7 (37.5–100) | 0.0002* |
| WOMAC function | 62.4 (7.9–100) | 76.4 (29.5–100) | 0.21 |
| SF-36 physical component score | 34.4 (15.4–55.9) | 41.1 (19.8–57.0) | 0.022* |
| SF-36 mental component score | 49.7 (27.4–64.5) | 56.5 (28.7–69.9) | 0.011* |
* Significant.
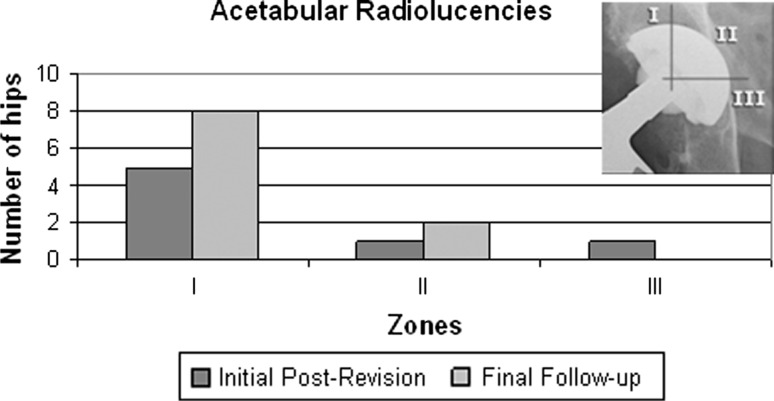
In comparison to the initial postrevision films, there were four instances of progressive acetabular radiolucencies (but the progression was minimal and all radiolucencies were 1 mm or less) seen on last followup films (Fig. 1). No shell had circumferential radiolucencies. There were no cases of acetabular component migration or progressive osteolysis. In the majority of cases in which bone graft was used (13 of 15 cases), the followup radiographs demonstrated complete or partial graft incorporation (nonrecurrence of osteolysis in the cystic areas). In the two other cases in which bone graft was used, there was some graft resorption. Additionally, one other hip (nongrafted) demonstrated pelvic osteolysis (< 1 cm2 in Zone 1) that was not present on initial postrevision radiographs.
Fig. 1.
A histogram and diagram demonstrates the number of hips (of the 26 hips with 2-year radiographic followup) and the location of radiolucent lines on the AP view of the acetabulum.
Two hips (6%) have experienced single dislocations and both were treated nonoperatively. There were no cases of liner spin-out and no infections.
Discussion
Long-term followup of cementless acetabular components have demonstrated durable fixation; however, polyethylene wear, including wear-through of the liner, especially with gamma irradiated in air or noncrosslinked polyethylene, has been a long-term problem [5]. When an acetabular shell is stable and well positioned, one option is to cement a new liner into the shell. The advantages of this technique are the relative ease of the procedure without destroying bone (which can occur with shell removal). A potential disadvantage is the potential failure of the cemented liner-shell construct. The purpose of this study was to assess the outcomes of THA revisions in which a nonconstrained liner was cemented into a secure cementless acetabular shell in cases in which there was wear-through of the polyethylene liner. Specifically, we determined (1) rerevision rates; (2) functional scores (Harris hip scores, WOMAC, and SF-36); (3) acetabular loosening rates; and (4) acetabular osteolysis rates. Acetabular liner and shell preparation was performed in a manner demonstrated in our biomechanical study to provide optimal stability of the shell-liner construct.
We acknowledge limitations to our study. First, the series was somewhat selective in that, if there was any recognized concern for stability, a constrained cemented liner was used [3]. Second, two of us independently reviewed the radiographs and we reached a consensus on differences. We did not determine the reliability of the radiographic observations.
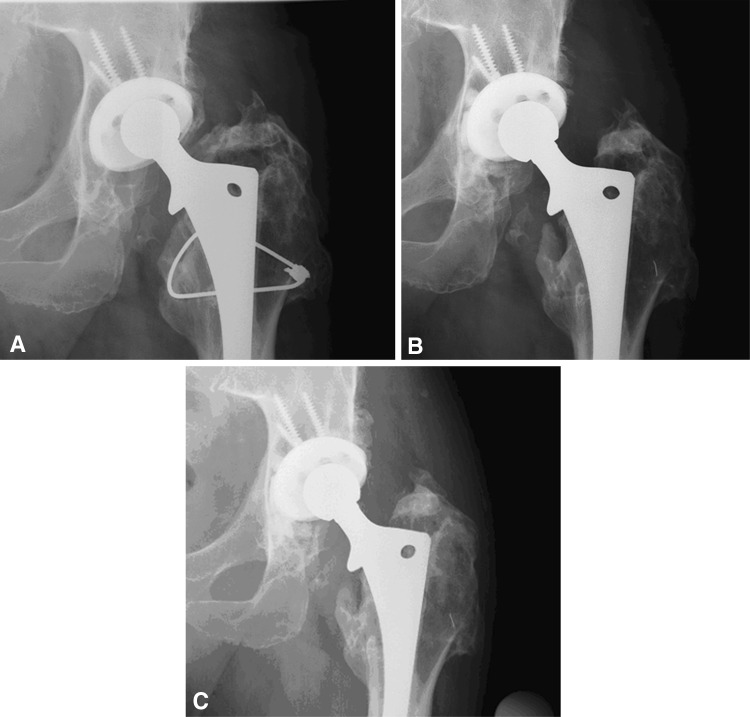
This cohort of 30 patients (31 hips) was followed for 2 to 10 years. We found cementation of a liner into a well-fixed cementless shell provided durable fixation (Fig. 2) and no failures occurred at an average 5.3 years followup. Twenty-six hips (87%) obtained minimum 2-year radiographic followup (average, 4.8 years); no cases demonstrated acetabular loosening and only one case demonstrated a new small osteolytic lesion (< 1 cm2). In the vast majority of cases in which bone grafting was used, complete or partial graft incorporation was demonstrated at followup. No liners became dislodged and there was no demonstrable wear of the cemented moderately crosslinked liners, although the average followup was only 5.3 years.
Fig. 2A–C.
(A) Prerevision, (B) postrevision, and (C) 4.7-year last followup radiographs are demonstrated. This patient was 42.6 years old at the time of the primary THA, 51.5 years old at revision surgery with liner cementation, and 56.2 years old at 4.7 years of followup. He was indicated for revision and liner cementation as a result of severe polyethylene wear. This patient participates in moderately intensive activities and had an increase in his WOMAC pain and stiffness score and SF-36 score after revision.
In this cohort, only two patients had single instances of dislocation (6%). This dislocation rate is lower than the 22% reported by Beaulé et al. [1]. The reason for the relatively low dislocation rate compared with the Beaulé et al. study includes the postoperative casting (single hip spica) or bracing of the patients and the fact that a constrained liner rather than these nonconstrained liners were placed in patients with intraoperative instability. This low dislocation rate occurred although 28-mm and smaller heads were used in most cases because at the time, we were trying to maximize polyethylene thickness. Today we would try to use larger head sizes (ie, 32-mm and rarely 36-mm heads) when possible. Also the two dislocations occurred early in the study before we started using postoperative immobilization of the hip. The lower failure rate of the cemented shell-liner construct at 5.3 years of followup in this study compared with other studies (Table 4) [1, 10, 12, 14] is likely the result of the mechanically optimal liner and shell preparation and the use of moderately crosslinked polyethylene. This is especially encouraging when one considers the young age of the patients (average age, 51.8 years) at the time of revision.
Table 4.
Comparison to study cohorts
| Study | Liner inserted at reoperation | Number in cohort | Number of living patients at followup | Lost to followup | Mean age at primary surgery (years) | Mean age at index surgery (liner exchange) (years) | Mean age at followup (years) | Mean length of followup (years) | Number of failures | Survival from revision | Percent dislocations |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Beaulé et al. (2004) [1] | 17 polyethylene, 15 metal-bearing | 32 hips (30 patients) | NR | 0 patients | 45.1 (20–84) | 53.7 (range, 31–85) | NR | 5.1 (range, 2.0–8.7) | 6 hips (4 aseptic loosening) | 78% for revision for any reason | 22% (7 hips) |
| Springer et al. (2005) [12] | All polyethylene | 17 hips (17 patients) | 17 hips (17 patients) | 0 patients | 63.3 | 68.9 (range, 45–90) | 71.6 | 2.7 (range, 2–5.2) | 1 hip (instability) | NR | 18% (3 hips) |
| Khanuja et al. (2010) [10] | All polyethylene (nonmodular shells) | 28 hips (26 patients) | 21 hips (21 patients) | 4 patients (6 hips) | 48.9 | 54.3 | 60.1 | 5.8 | 4 hips (3 aseptic loosening) | 81% at 5 years | 11% (3 hips) |
| Yoon et al. (2005) [14] | Metal-inlay polyethylene | 39 hips (39 patients) | NR | 0 patients | 47.4 | 55 (range, 32–74) | 58 | 2.8 (range, 2–9) | 1 (aseptic loosening) | NR | 5% (2 hips) |
| Current study | All polyethylene | 31 hips (30 patients) | 28 hips (27 patients) | 1 patient (1 hip) | 41.0 (range, 24.3–64.8) | 51.8 (range, 33.3–77.5) | 55.9 (range, 39.2–83.0) | 5.3 (range, 2.2–10.9) | 0 | 100% | 6% (2 hips) |
NR = not reported.
This study also demonstrates an example of translational biomechanics research in which a clinical problem is identified (liner wear-through), basic experimental work is performed to determine an appropriate clinical solution, and a clinical study is performed to determine whether the experimental study translates into anticipated clinical results. The findings from our mechanical study were used to obtain the durable results of this operative procedure. This approach has averted some of the complications associated with attempting to remove shells and reconstruct the acetabulum in cases in which secure shells are present and extensive osteolysis is present surrounding the shell (including creation of pelvic discontinuity and requirements for cages and allograft bone to reconstruct defects that can be present after shell removal). Our observations have encouraged us to continue using the procedure of cementing liners into secure shells in cases in which polyethylene liner wear-through has occurred, in which the capturing mechanism is inadequate, and the shell diameter is large enough to accept the cemented liner construct.
Acknowledgments
We thank Andrew S. Malin MD, Christopher W. Wells BA, and Nathan M. Schularick MD for their help with data collection.
Footnotes
One author certifies that he (JJC) has or may receive payments or benefits, in any one year, an amount in excess of $10,000, from a commercial entity (DePuy, Warsaw, IN, USA; Lippincott, Williams & Wilkins, Philadelphia, PA, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation was obtained.
References
- 1.Beaulé PE, Ebramzadeh E, LeDuff M, Prasad R, Amstutz HC. Cementing a liner into a stable cementless acetabular shell: the double-socket technique. J Bone Joint Surg Am. 2004;86:929–934. doi: 10.2106/00004623-200405000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Bellamy N, Campbell J, Stevens J, Pilch L, Stewart C, Mahmood Z. Validation study of a computerized version of the Western Ontario and McMaster Universities VA3.0 Osteoarthritis Index. J Rheumatol. 1997;24:2413–2415. [PubMed] [Google Scholar]
- 3.Callaghan JJ, Parvizi J, Novak CC, Bremner B, Shrader W, Lewallen DG, Johnston RC, Goetz DD. A constrained liner cemented into a secure cementless acetabular shell. J Bone Joint Surg Am. 2004;86:2206–2211. doi: 10.2106/00004623-200410000-00011. [DOI] [PubMed] [Google Scholar]
- 4.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 5.Della Valle CJ, Mesko NW, Quigley L, Rosenberg AG, Jacobs JJ, Galante JO. Primary total hip arthroplasty with a porous-coated acetabular component: a concise follow-up, at a minimum of twenty years, of previous reports. J Bone Joint Surg Am. 2009;91:1130–1135. doi: 10.2106/JBJS.H.00168. [DOI] [PubMed] [Google Scholar]
- 6.Gaffey JL, Callaghan JJ, Pedersen DR, Goetz DD, Sullivan PM, Johnston RC. Cementless acetabular fixation at fifteen years: a comparison with the same surgeon’s results following acetabular fixation with cement. J Bone Joint Surg Am. 2004;86:257–261. [PubMed] [Google Scholar]
- 7.Haft GF, Heiner AL, Dorr LD, Brown TD, Callaghan JJ. A biomechanical analysis of polyethylene liner cementation into a fixed metal acetabular shell. J Bone Joint Surg Am. 2003;85:1100–1110. doi: 10.1302/0301-620X.85B8.14673. [DOI] [PubMed] [Google Scholar]
- 8.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 9.Heck DA, Murray DG. In vivo construction of a metal-backed, high-molecular weight polyethylene cup during McKee-Farrar revision total joint arthroplasty: a case report. J Arthroplasty. 1986;1:203–206. doi: 10.1016/S0883-5403(86)80031-6. [DOI] [PubMed] [Google Scholar]
- 10.Khanuja HS, Aggarwal A, Hungerford MW, Hungerford DS, Jones LC, Mont MA. Cementing polyethylene liners into non-modular acetabular components in revision total hip arthroplasty. J Orthop Surg. 2010;18:184–188. doi: 10.1177/230949901001800210. [DOI] [PubMed] [Google Scholar]
- 11.Massin P, Schmidt L, Engh CA. Evaluation of cementless acetabular component migration: an experimental study. J Arthroplasty. 1989;4:245–251. doi: 10.1016/S0883-5403(89)80020-8. [DOI] [PubMed] [Google Scholar]
- 12.Springer BD, Hanssen AD, Lewallen DG. Cementation of an acetabular liner into a well-fixed acetabular shell during revision total hip arthroplasty. J Arthroplasty. 2005;20:652–657. doi: 10.1016/j.arth.2005.01.019. [DOI] [PubMed] [Google Scholar]
- 13.Ware JE, Sherbourne CD. The MOS 36-Item Short Form Health Survey (SF-36): conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Yoon TK, Seon JK, Song EK, Chung JY, Seo HY, Park YB. Cementation of a metal-inlay polyethylene liner into a stable metal shell in revision total hip arthroplasty. J Arthroplasty. 2005;20:652–657. doi: 10.1016/j.arth.2005.01.019. [DOI] [PubMed] [Google Scholar]