Abstract
Background
Techniques that ensure femoral bone preservation after primary THA are important in younger patients who are likely to undergo revision surgery.
Questions/purposes
We examined femoral stem survival, bone deficiency at revision arthroplasty, and radiographic bone loss in hips implanted with a cemented polished double-taper stem in a cohort of patients younger than 55 years.
Methods
We reviewed 197 hips (median patient age, 47 years; range, 16–54 years) after a minimum followup of 2 years (median, 7 years; range, 2–19 years) since primary THA. Clinically, we determined survival to major and minor stem revision and cases of bone deficiency requiring a long stem or impaction bone grafting or created by the need for femoral osteotomy at revision arthroplasty. Radiographically, we assessed stem loosening, femoral osteolysis, and femoral bone deficiency.
Results
Stem survival to major revision for aseptic loosening was 100% at 13 years and for any reason was 97% (95% CI, 93–100%). At revision of seven stems, a long stem was used in one hip, a total femoral replacement in one hip and impaction bone grafting in one hip. No femoral osteotomies were required. Bone was preserved in four hips by cement-within-cement stem exchange. No stems were radiographically loose. Proximal osteolysis was present in 11% of femurs. Femoral bone deficiency was graded as Paprosky Type I (97%) or II (3%) and Endo-Klinik Grade 0 (79%) or I (21%).
Conclusions
Cemented polished taper stems have high survival at 13 years in young patients and enable femoral bone preservation for subsequent revision.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Due to longer life expectancy, higher activity, and nonosteoarthritis reasons, young patients are at greater risk of failure of their primary THA than older patients [2, 29, 30]. Failure is often associated with prosthesis loosening and periprosthetic bone loss, which not only necessitate revision surgery but also contribute to the poorer function of revision THA [18, 34]. Techniques that enhance bone preservation after primary THA, particularly on the femoral side, are important in younger patients. This was proposed as a reason for the move away from cemented to uncemented fixation of femoral stems [13, 19], but the possibility exists that some designs of cemented stems have more advantages to preserve bone in the long term.
In determining whether a particular femoral stem is associated with bone loss, the following indicators might be used. First, because loosening is associated with bone loss, stem survival to the end point of revision for loosening would be important. Second, the need to use a long stem at revision implies sacrifice of bone. This would be important, as would the need for femoral impaction bone grafting and the requirement to undertake osteotomy to remove a well-fixed ingrown uncemented stem or cement. Third, radiographic assessment would include the analysis of linear and nonlinear osteolysis. Finally, an overview of the femoral appearance would be useful. In this regard, there is no grading system that has been applied to solid femoral stems, but there are systems to grade bone deficiency before revision and we believed these might usefully be employed to provide an overview of the femoral bone loss around all femoral stems, unrevised or revised.
The polished collarless double-taper femoral stems, including the Exeter™ (Stryker Howmedica Osteonics, Berkshire, UK) and CPT® (Zimmer, Inc, Warsaw, IN, USA), are associated with high survival rates in older patients [10, 16, 22, 35, 36]. Stem survival to the end point of loosening is reportedly 100% at 12.5 years in younger patients when performed by specialist hip surgeons [3, 21], although such high survival may not necessarily reflect those of the general orthopaedic surgeon. General orthopaedic surgeons have a shared case load of arthroplasty, general orthopaedics, and orthopaedic trauma but usually perform most THAs in public hospitals.
We therefore examined a cohort of patients younger than 55 years who had primary cemented polished double-taper stems and were operated on by general orthopaedic surgeons in a teaching hospital. Specifically, we determined survival to femoral stem revision for loosening and survival for all causes; bone deficiency at revision requiring the use of a long stem or femoral impaction grafting or created by the need for femoral osteotomy; and radiographic loosening, osteolysis, and femoral bone deficiency.
Patients and Methods
Between March 1988 and September 2005, 169 patients younger than 55 years had 197 primary THAs in which the femoral prosthesis used was a cemented collarless polished double-taper femoral stem (Fig. 1). We excluded eight patients with primary or secondary malignancy who underwent THA with this stem design. There were 17 supervising consultant general orthopaedic surgeons, all of whom did general orthopaedics, orthopaedic trauma, and joint arthroplasty. The mean number of THAs performed by the participating surgeons at the study hospital per year was 17 (median, 13; range, 1–56). The consultants supervised the surgery performed by visiting fellows undertaking a posttraining arthroplasty fellowship and orthopaedic trainees. This study was approved by the institutional human research ethics board.
Fig. 1.
A flowchart summarising the process for excluding and including patients in the study.
The cohort study period was defined by the first case of the senior author (DWH) and the last case that met the requirement for a minimum 2-year followup. We included surgeons using the cemented collarless double-taper stem throughout the study period up until the end of the study period or to the end of their contract at the hospital, whichever came first. Apart from one consultant surgeon, all cases were consecutive by surgeon. For one surgeon (DWH), cases were consecutive except during the period of two randomized controlled trials of alternative implants (n = 17 hips). A total of 1139 primary and 676 revision THAs were undertaken by the surgeons during the study period. There were no contraindications for cemented stem use. The diagnoses were primary osteoarthritis for 87 hips (44%), osteoarthritis secondary to trauma for 14 hips (7%) or avascular necrosis for three hips (2%), avascular necrosis for 30 hips (15%), inflammatory arthritis for 23 hips (12%), dysplasia for 23 hips (12%), and other diagnoses for 17 hips (9%). The median age of the patients at primary THA was 47 years (range, 16–54 years). At latest review, 14 patients (15 hips) had died 2 months to 7 years after surgery for causes unrelated to THA.
A posterior approach was used in 160 hips (81%), a lateral approach in 30 hips (15%), and a transtrochanteric approach in seven hips (4%). The collarless double-taper polished stems included 123 stainless steel Exeter™ and 32 stainless steel and 42 cobalt-chrome CPT® stems, both FDA-approved devices (Table 1). A cemented acetabular component was used in 65 hips and an uncemented component in 132 hips. Femoral preparation involved use of a distal plug, pulse lavage, and retrograde Simplex® bone cement (Howmedica International, London, UK) introduction with a gun and pressurization. Patients received perioperative intravenous antibiotics and were allowed full weightbearing on the first day postoperatively.
Table 1.
Patient demographics and details
| Variable | Exeter™ | CPT® | All stems |
|---|---|---|---|
| Number of hips | 123 | 74 | 197 |
| Age (years)* | 48 (16–54) | 47 (17–54) | 47 (16–54) |
| Male:female | 53:53 | 34:32 | 86:83 |
| Primary osteoarthritis | 60 (49%) | 27 (37%) | 87 (44%) |
| Femoral head diameter (22 mm:26 mm:28 mm:30 mm) | 8:114:0:1 | 4:0:70:0 | 12:114:70:1 |
| Acetabular component fixation (cemented:uncemented) | 65:58 | 0:74 | 65:132 |
| Lost to followup | 3 (2%) | 1 (1%) | 4 (2%) |
| Deaths | 10 | 4 | 14 |
| Followup of surviving patients (years)† | 10 (10, 5–19) | 4 (4, 2–7) | 8 (7, 2–19) |
* Values are expressed as median, with range in parentheses; †values are expressed as mean, with median and range in parentheses; the remaining values are expressed as number of patients.
Patients were reviewed preoperatively and at regular postoperative intervals of 3 and 12 months and every 2 to 3 years thereafter. Four patients (four hips, 2%) were lost to followup at 2, 6, 6, and 9 years. For the remaining 151 patients (178 hips), the minimum followup to last review or reoperation was 2 years (mean, 8 years; median, 7 years; range, 2–19 years). The minimum followup was 10 years for 85 hips. At latest review of 171 hips in surviving patients that had not undergone femoral stem reoperation, 114 were reviewed in clinic, and for patients unable to attend clinic, mailed questionnaires were completed for review of 46 hips and telephone interviews were performed to review 11 hips. Of those patients unable to attend clinic, radiographs were arranged in community clinics for 26 of 57 hips and forwarded for assessment. Including the surviving and deceased patients, 132 hips that had not undergone femoral reoperation had a minimum of 5 years’ followup.
Femoral stem revision was defined as major if both the stem and the cement were removed. Revision was defined as minor if the stem was removed without affecting the cement-bone interface and included cement-within-cement stem exchange. We calculated prosthesis survival using femoral stem major revision for aseptic loosening, and major or minor revision for any reason as end points. Survival analyses were undertaken using the Kaplan-Meier method with 95% CIs. Survival was reported at a maximum of 13 years when a minimum of 20 patients were uncensored. Worst-case analysis (WCA) survival was determined using the assumption that stems in patients lost to followup had been revised. The incidence of femoral bone deficiency at revision was calculated by including the number of cases of postoperative periprosthetic fractures, classified according to the Vancouver classification [7], or cavitary bone loss requiring the use of a long stem, those where impaction bone grafting was used to reconstruct bone, and those requiring femoral osteotomy to remove a well-fixed stem.
Radiographic examination included an AP pelvic radiograph and AP and rolled lateral hip radiographs. One of the authors (LBS) who was not involved in the surgery assessed radiographs of 116 of 132 hips (88%) that had not undergone femoral reoperation with a minimum of 5 years’ followup (mean, 8 years; range, 5–19 years). This included radiographs of hips that had undergone acetabular component revision only. The femoral stem was classified as stable or possibly or probably loose using the radiographic criteria of Harris et al. [15]. Definite loosening was defined as greater than 5 mm of subsidence at the cement-bone interface or stem fracture [15, 25]. Osteolysis was defined as a nonlinear demarcated radiolucent lesion more than 3 mm in diameter [26] and graded according to Goetz et al. [12] as mild if it occupied one or two Gruen zones [14] or had a combined area of less than 2.5 cm2, intermediate if it occupied three to five Gruen zones or had an area of 2.5 to 10 cm2, and extensive if it occupied at least six Gruen zones or had an area of more than 10 cm2. Femoral bone deficiencies at latest review of hips without reoperation were graded radiographically using the classifications of Aribindi et al. (“Paprosky”) [1] and Engelbrecht and Heinert (“Endo-Klinik”) [9]. For hips that had undergone femoral revision, radiographic loosening and osteolysis and classification of bone deficiency were assessed on prereoperation radiographs and on the latest postreoperation radiographs of those femurs with a cemented collarless double-taper stem in situ. The prereoperation Paprosky and Endo-Klinik classifications were not determined in cases of periprosthetic fracture or infection.
Results
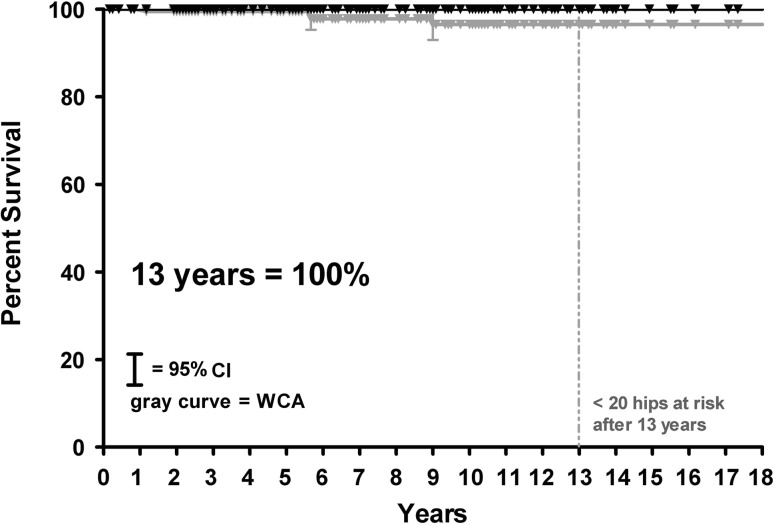
Femoral stem survival at 13 years to the end point of revision for loosening was 100% (WCA = 97%; 95% CI, 93%–100%) (Fig. 2). Stem survival at 13 years to the end point of any major revision for all causes was 97% (95% CI, 93%–100%) (WCA = 95%; 95% CI, 91%–99%). Stem survival to the end point of major or minor stem revision for any reason was 92% (95% CI, 86%–99%) (WCA = 89%; 95% CI, 82%–96%). There were three major revisions of the stem in three hips and minor revision in four hips (Table 2).
Fig. 2.
Survival curves, including WCA, of cemented polished double-taper femoral stems with major revision for aseptic loosening or osteolysis as end points are shown. Survival at 13 years is 100% (WCA = 97%; 95% CI, 93%–100%).
Table 2.
Minor and major revisions
| Reason for reoperation | Number of hips | Acetabular | Femoral | ||
|---|---|---|---|---|---|
| Minor | Major | Minor cement-within-cement | Major | ||
| Acetabular | |||||
| Aseptic loosening | 9 | 8 | 2 | ||
| Dislocation | 3 | 3 | 1 | ||
| Component/cement fracture | 1 | 1 | |||
| Femoral | |||||
| Periprosthetic femoral fracture | 1 | 1 | |||
| Acetabular/femoral | |||||
| Infection | 2 | 2 | 2* | ||
| Leg length discrepancy | 1 | 1 | |||
| Total | 17 | 14 | 4 | 3 | |
Minor stem revision means the stem was removed without affecting the cement-bone interface; major stem revision involved removal of both the stem and the cement; * previous plate fixation for femoral periprosthetic fracture in one of these hips also.
There were three cases of bone deficiency at revision (1.5%). One stem underwent major revision to a long-length CPT® cemented stem after a Vancouver B2 periprosthetic fracture at 3 months. One hip underwent open reduction and internal fixation of a Vancouver B1 fracture using a plate, cables, and a tibial bone strut graft at 5 years postoperatively. After further infection in this hip, a two-stage major revision to a total femoral replacement was undertaken. One hip underwent two-stage major revision for infection 2 years postoperatively. Reconstruction was with a standard-length cemented CPT® stem with impaction bone grafting using bone from two femoral heads to treat cancellous bone deficiency after removal of infected bone. No femoral osteotomies were required. Importantly, femoral bone was preserved in four hips by cement-within-cement exchange at minor revision using a standard-length cemented collarless double-taper stem (Fig. 3A–B).
Fig. 3A–B.
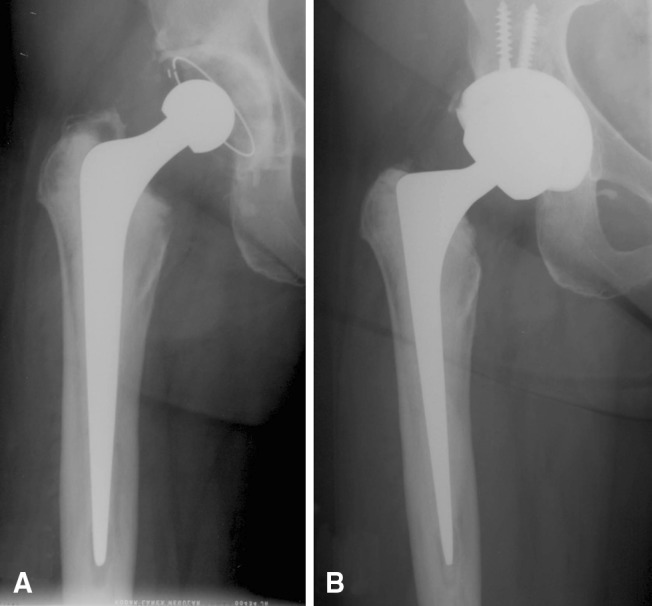
(A) An AP radiograph of the right hip with a cemented polished double-taper stem shows excellent femoral bone preservation at 13 years after primary THA and before revision of the acetabular component for recurrent dislocation. (B) Femoral bone preservation is maintained in the same hip 3 years after acetabular revision and cement-within-cement stem exchange to a new polished stem.
At latest radiographic review of 116 unrevised femurs with a minimum of 5 years’ followup, all stems were radiographically stable. Femoral osteolysis was present in 13 hips (11%). In all cases, the osteolysis was localized proximally in Gruen Zone 1, 7, 13, or 14 and was graded as mild in nine hips (8%) and intermediate in four hips (3%). At latest radiographic review, femoral bone quality was graded as Paprosky Type I in 112 hips (97%) and Paprosky Type II in four hips (3%). The Endo-Klinik grades were 0 in 92 hips (79%) and I in 24 (21%).
The seven stems that underwent major or minor revision were all radiographically stable preoperatively and this was confirmed intraoperatively. The one stem revised for the periprosthetic fracture was removable by hand from the cement. There was no femoral osteolysis. Excluding the fractures and the hip revised for infection, the reoperated femurs were all graded as Paprosky Type I and Endo-Klinik Grade 0. At latest postrevision followup at average 5.5 years (range, 3–9 years), all cemented polished double-taper stems were radiographically stable, there was no osteolysis, and femurs were graded as Paprosky Type I and Endo-Klinik Grade 0.
Discussion
Techniques that can be used by the general orthopaedic surgeon to ensure femoral bone preservation throughout the life of a THA and at revision are important in younger patients. We therefore examined femoral stem survival, bone deficiency at revision arthroplasty, and radiographic bone loss in hips implanted with a cemented polished double-taper stem in a cohort of patients younger than 55 years.
We acknowledge limitations to our study. First, all cases were consecutive by surgeon, but for some surgeons, cases represented their early experience using the collarless double-taper stem. Although not evident by our current data, this could unfavorably bias the longer-term survival. Second, we had no quantitative measurement of femoral bone deficiency. In the absence of prospective quantitative assessment of bone loss using such techniques as dual-energy x-ray absorptiometry or CT, which are not routinely undertaken after primary THA, we believed proxy measures of bone preservation were reasonable. These included the avoidance of bone-damaging femoral osteotomies or long-stem revisions, radiographic loosening and osteolysis, and a new use of common grading systems routinely used to describe the amount of bone damage before revision. Third, the low incidence of femoral stem complications did not allow an analysis of whether there was increased risk of complications for patients of lower-volume versus higher-volume surgeons, which has been previously reported [4, 24]. Using Medicare claims data, Losina et al. [24] reported an increased risk and 57% of complications occurred within the first 18 months. Given our minimum 2-year followup, it is therefore unlikely longer-term followup will identify any difference in risk in this series.
In this young cohort of 197 hips with a cemented polished double-taper stem, there was 100% stem survival to the end point of revision for stem loosening at 13 years, only 1.5% incidence of clinical femoral bone deficiency, and minimal to no bone deficiency on radiographs. Our stem survival of 100% is consistent with the published studies of cemented polished double-taper stems in similarly aged patients [3, 6, 21, 32] (Table 3). Importantly, these survival rates in young patients often with complex hip disorders were also comparable to those for longer-term followups of this stem design in older patients [3, 6, 10, 16, 21, 32, 37] (Table 3). Lewthwaite et al. [21] reported 17-year stem survivals of 100% and 99% for the end points of revision for stem loosening and for any reason, respectively, in young patients. Their series of 130 hips with Exeter™ stems involved both Exeter™-based specialist hip surgeons (68%) and general orthopaedic surgeons (32%). Their high survival, achieved with surgeons of varying expertise, were comparable to our findings where the THAs were undertaken by general orthopaedic surgeons of varying expertise in a non-Exeter™-based center. To compare these results to those for uncemented stems in young patients, we reviewed the meta-analysis performed by Springer et al. [33]. In their analysis of 22 studies of uncemented THA comprising 6408 hips, the reported pooled failure rates for modern uncemented femoral stems in young patients aged 32 to 55 years using the end points of revision for aseptic loosening and revision for any reason were 1.3% (95% CI, 1.0%–1.7%) and 3.1% (95% CI, 2.7%–3.7%), respectively, at a mean followup of 8.4 years. At the same average followup, the femoral failure rates in our study of young cemented hips were 0% and 1.5%, respectively. Given the low incidence, however, it may be difficult to distinguish between the two fixation methods in young patients based on survival or loosening alone. Given this, the potential for femoral bone preservation throughout the lifetime of the prosthesis and bone deficiency caused at reoperation are therefore now as important and should be reported in cohort studies of cemented and uncemented primary stems in the younger patient.
Table 3.
Comparison of results of published series of cemented polished collarless double-taper stems in young patients (< 55 years) and in two series of patients of all ages
| Study | Number of hips | Single- or multiple- surgeon series | Varying experience | Consecutive series | Age (years)* | Followup (years)* | Number of hips lost to followup | Number of stems revised for loosening/other | Stem survival (%) to end point of revision for: | Radiographic loosening (cement-bone) | Radiographic distal osteolysis | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aseptic loosening | Any reason | Time (years) | |||||||||||
| Patients < 55 years | |||||||||||||
| Burston et al. [3] | 58 | Multiple | Yes | Yes | < 50 | 12.5 (10–17) | 0 | 0 | 100 | NR | 12 | 0 | NRS |
| Lewthwaite et al. [21]† | 130 | Multiple | Yes | No | 42 (≤ 50) | 12.5 (10–17) | 0 | 0/1 | 100 | 99 | 17 | 0 | 0 |
| Simon et al. [32] | 42‡ | Single | Yes | 25 (17–34) | 9.7 (5–17) | 2 | 0/0 | 100 | 100 | 10 | 0 | 0 | |
| de Kam et al. [6] | 104 | Two | No | Yes | 31 (16–39) | 6.2 (2–13) | 0 | 0/3 | 100 | 96 | 7 | 0 | 0 |
| Current study | 197 | Multiple | Yes | Yes | 44 (16–54) | 8 (2–19) | 2 | 0/3 | 100 | 97 | 13 | 0 | 0 |
| All patients | |||||||||||||
| Carrington et al. [5]† | 325 | Multiple | Yes | NR | 68 (24–87) | 15.7 (15–17) | 0 | 0/1 | 100 | NR | 17 | 0 | 1/106 (distal) |
| Young et al. [37] | 230 | Multiple | Yes | Yes | 69 (44–89) | 11.2 (10–13) | 1 | 0/3 | 100 | 95 | 13 | 0 | 0 |
The criteria for inclusion were prospective series involving all hip disorders, using cemented polished collarless double-taper stem designs (Exeter™, CPT®); * values are expressed as mean, with range in parentheses; †Exeter™-based studies of Exeter™ stems; ‡bilateral THAs in all cases; NR = not reported; NRS = not reported separately from acetabular results.
Consistent with similar studies [6, 21], infection and periprosthetic fracture, and not linear or nonlinear osteolysis, brought stems to revision and were the causes of bone deficiency. Two-stage exchange, femoral impaction bone grafting, and revision to a standard-length stem successfully treated the bone deficiency in one infected hip, which we have reported previously [17]. Use of a long stem to bypass periprosthetic fractures or to salvage femurs after infection occurred in 1% of cases and is not a good result in terms of preservation of bone. Long stems pose major problems throughout the life of a young person. Examples include interference with ipsilateral total knee revision stems and distal periprosthetic fractures. After multiple revisions with longer and longer stems, surgical options become limited and lead eventually to total femoral replacement, which is associated with high complication rates, including deep infections and amputations, as well as poor function [11, 23].
In our study, bone damage was avoided by cement-within-cement exchange of well-fixed femoral stems. Young patients with THA will come to revision for many causes other than the femoral stem but which may require stem exchange. A particular advantage of reoperations involving cemented polished stems, which are modular in cement, is that cement-within-cement stem exchange can be performed, which preserves bone. We and others have previously reported no stem rerevision or radiographic complications after cement-within-cement exchange using the cemented collarless double-taper stem at up to 15 years in a series of 23 and 53 hips, respectively [8, 27]. In contrast, bone-sacrificing techniques such as transfemoral and extended trochanteric osteotomies requiring the use of long stems are used to remove well-fixed uncemented stems or remove cement and stems that are not modular within cement [31]. Use of this approach over conventional exposure, with its inherent risk of femoral fracture, remains controversial however [20]. Mardones et al. [28] undertook extended osteotomies in 18% of their revision THA operations and reported nonunion and intraoperative fracture in 3% and 4% of their cases, respectively. However, in their review of the literature, they recognized complications can occur in up to 24% of cases.
Consistent with the stem survival data, there was minimum radiographic evidence of femoral bone deficiency at up to 19 years, including when the femoral stems had undergone reoperation. We used gradings of bone deficiency, usually reserved for studies of revision THA [1, 9], as these are important to demonstrate bone preservation in the absence of diagnostics. There was no endosteal bone loss according to the Endo-Klinik classification and minimal diaphyseal damage in only 3% of femurs according to the Paprosky classification. The relatively benign appearance of the femur, even at long-term followup as reported in most other series of this stem design (Table 3), suggests a low probability of impending loosening or failure.
In summary, at intermediate- to long-term followup, femoral bone can be preserved in younger patients using a cemented polished tapered stem. Importantly, the good survival and bone preservation with this stem were achieved in the hands of general orthopaedic surgeons, and therefore we believe a high-survival can be generalized to nonspecialty orthopaedic centers.
Acknowledgments
We thank Susan Pannach for assisting with patient followup. We also thank all consultants, fellows, and residents for their contribution to the study. We also acknowledge the Australian Institute of Health and Welfare for providing National Death Index data.
Footnotes
The institution of the authors has received, in any 1 year, research funding from the Australian Orthopaedic Association Research Foundation (Melbourne, Australia), the Royal Adelaide Hospital (Adelaide, Australia), Zimmer Ltd Australia (Sydney, Australia), and Bristol-Myers Squibb/Zimmer (Warsaw, IN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with the ethical principles of research.
This work was performed at Royal Adelaide Hospital, Adelaide, Australia.
Contributor Information
Donald W. Howie, Email: donald.howie@adelaide.edu.au.
Kerry Costi, Email: kerry.costi@health.sa.gov.au.
References
- 1.Aribindi R, Barba M, Solomon MI, Arp P, Paprosky W. Bypass fixation. Orthop Clin North Am. 1998;29:319–329. doi: 10.1016/S0030-5898(05)70330-8. [DOI] [PubMed] [Google Scholar]
- 2.Annual Report. Adelaide, Australia: Australian Orthopaedic Association; 2010. [Google Scholar]
- 3.Burston BJ, Yates PJ, Hook S, Moulder E, Whitley E, Bannister GC. Cemented polished tapered stems in patients less than 50 years of age: a minimum 10-year follow-up. J Arthroplasty. 2010;25:692–699. doi: 10.1016/j.arth.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 4.Camberlin C, Vrjens F, Guaquier K, Devriese S, Sande S. Provider volume and short-term complications after elective total hip replacement: an analysis of Belgian administrative data. Acta Orthop Belg. 2011;77:311–319. [PubMed] [Google Scholar]
- 5.Carrington NC, Sierra RJ, Gie GA, Hubble MJ, Timperley AJ, Howell JR. The Exeter Universal cemented femoral component at 15 to 17 years: an update on the first 325 hips. J Bone Joint Surg Br. 2009;91:730–737. doi: 10.1302/0301-620X.91B6.21627. [DOI] [PubMed] [Google Scholar]
- 6.Kam DC, Klarenbeek RL, Gardeniers JW, Veth RP, Schreurs BW. The medium-term results of the cemented Exeter femoral component in patients under 40 years of age. J Bone Joint Surg Br. 2008;90:1417–1421. doi: 10.1302/0301-620X.90B11.20557. [DOI] [PubMed] [Google Scholar]
- 7.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Inst Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 8.Duncan WW, Hubble MJ, Howell JR, Whitehouse SL, Timperley AJ, Gie GA. Revision of the cemented femoral stem using a cement-in-cement technique: a five- to 15-year review. J Bone Joint Surg Br. 2009;91:577–582. doi: 10.1302/0301-620X.91B5.21621. [DOI] [PubMed] [Google Scholar]
- 9.Engelbrecht E, Heinert K. Klassifikation und Behandlungsrichtlinien von Knochensubstanzverlusten bei Revisionsoperationen am Hüftgelenk: mittelfristige Ergebnisse. In: Arcq M, editor. Primär- und Revisions-Alloarthroplastik Hüft- und Kniegelenk: 10 Jahre Endo-Klinik Hamburg. Berlin, Germany: Springer-Verlag; 1987. pp. 189–201. [Google Scholar]
- 10.Franklin J, Robertsson O, Gestsson J, Lohmander LS, Ingvarsson T. Revision and complication rates in 654 Exeter total hip replacements, with a maximum follow-up of 20 years. BMC Musculoskelet Disord. 2003;4:1–5. doi: 10.1186/1471-2474-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Friesecke C, Plutat J, Block A. Revision arthroplasty with use of a total femur prosthesis. J Bone Joint Surg Am. 2005;87:2693–2701. doi: 10.2106/JBJS.D.02770. [DOI] [PubMed] [Google Scholar]
- 12.Goetz DD, Smith EJ, Harris WH. The prevalence of femoral osteolysis associated with components inserted with or without cement in total hip replacements: a retrospective matched-pair series. J Bone Joint Surg Am. 1994;76:1121–1129. doi: 10.2106/00004623-199408000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Goldring SR, Jasty M, Roelke MS, Rourke CM, Bringhurst FR, Harris WH. Reaction of bone to methacrylate after hip arthroplasty: a long-term gross, light microscopic, and scanning electron microscopic study. Arthritis Rheum. 1986;29:836–842. doi: 10.1002/art.1780290704. [DOI] [PubMed] [Google Scholar]
- 14.Gruen TA, McNiece GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 15.Harris WH, McCarthy JC, O’Neil DA. Femoral component loosening using contemporary techniques of femoral cement fixation. J Bone Joint Surg Am. 1982;64:1063–1067. [PubMed] [Google Scholar]
- 16.Hook S, Moulder E, Yates PJ, Burston BJ, Whitley E, Bannister GC. The Exeter Universal stem: a minimum ten-year review from an independent centre. J Bone Joint Surg Br. 2006;88:1584–1590. doi: 10.1302/0301-620X.88B12.18345. [DOI] [PubMed] [Google Scholar]
- 17.Howie DW, Callary SA, McGee MA, Russell NC, Solomon LB. Reduced femoral component subsidence with improved impaction grafting at revision hip arthroplasty. Clin Orthop Relat Res. 2010;468:3314–3321. doi: 10.1007/s11999-010-1484-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hultmark P, Kärrholm J, Strömberg C, Herberts P, Möse CH, Malchau H. Cemented first-time revisions of the femoral component: prospective 7 to 13 years’ follow-up using second-generation and third-generation technique. J Arthroplasty. 2000;15:551–561. doi: 10.1054/arth.2000.4811. [DOI] [PubMed] [Google Scholar]
- 19.Jones LC, Hungerford DS. Cement disease. Clin Orthop Relat Res. 1987;225:192–206. [PubMed] [Google Scholar]
- 20.Lerch M, Lewinski G, Windhagen H, Thorey F. Revision of total hip arthroplasty: clinical outcome of extended trochanteric osteotomy and intraoperative femoral fracture. Technol Health Care. 2008;16:293–300. [PubMed] [Google Scholar]
- 21.Lewthwaite SC, Squires B, Gie GA, Timperley AJ, Ling RS. The Exeter Universal hip in patients 50 years or younger at 10–17 years’ followup. Clin Orthop Relat Res. 2008;466:324–331. doi: 10.1007/s11999-007-0049-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ling RS, Charity J, Lee AJ, Whitehouse SL, Timperley AJ, Gie GA. The long-term results of the original Exeter polished cemented femoral component: a follow-up report. J Arthroplasty. 2009;24:511–517. doi: 10.1016/j.arth.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 23.Lombardi AV, Jr, Berend KR. The shattered femur: radical solution options. J Arthroplasty. 2006;21(4 suppl 1):107–111. doi: 10.1016/j.arth.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 24.Losina E, Barrett J, Mahomed NN, Baron JA, Katz JN. Early failures of total hip replacement: effect of surgeon volume. Arthritis Rheum. 2004;50:1338–1343. doi: 10.1002/art.20148. [DOI] [PubMed] [Google Scholar]
- 25.Malchau H, Kärrholm J, Wang YX, Herberts P. Accuracy of migration analysis in hip arthroplasty: digitized and conventional radiography, compared to radiostereometry in 51 patients. Acta Orthop Scand. 1995;66:418–424. doi: 10.3109/17453679508995578. [DOI] [PubMed] [Google Scholar]
- 26.Maloney WJ, Galante JO, Anderson M, Goldberg V, Harris WH, Jacobs J, Kraay M, Lachiewicz P, Rubash HE, Schutzer S, Woolson ST. Fixation, polyethylene wear, and pelvic osteolysis in primary total hip replacement. Clin Orthop Relat Res. 1999;369:157–164. doi: 10.1097/00003086-199912000-00016. [DOI] [PubMed] [Google Scholar]
- 27.Mandziak DG, Howie DW, Neale SD, McGee MA. Cement-within-cement stem exchange using the collarless polished double-taper stem. J Arthroplasty. 2007;22:1000–1006. doi: 10.1016/j.arth.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 28.Mardones R, Gonzalez C, Cabanela ME, Trousdale RT, Berry DJ. Extended femoral osteotomy for revision of hip arthroplasty: results and complications. J Arthroplasty. 2005;20:79–83. doi: 10.1016/j.arth.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 29.Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ, Coyte PC, Wright JG. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg. 2008;51:428–436. [PMC free article] [PubMed] [Google Scholar]
- 30.Sarmiento A, Ebramzadeh E, Gogan WJ, McKellop HA. Total hip arthroplasty with cement: a long-term radiographic analysis in patients who are older than fifty and younger than fifty years. J Bone Joint Surg Am. 1990;72:1470–1476. [PubMed] [Google Scholar]
- 31.Schmidt J, Porsch M, Sulk C, Hillekamp J, Schneider T. Removal of well-fixed or porous-coated cementless stems in total hip revision arthroplasty. Arch Orthop Trauma Surg. 2002;122:48–50. doi: 10.1007/s004020100344. [DOI] [PubMed] [Google Scholar]
- 32.Simon JP, Robbens E, Maes M, Bellemans J. Single-stage bilateral total hip arthroplasty in patients less than 35 years: forty arthroplasties with 5–17 years follow-up. Acta Orthop Belg. 2009;75:189–199. [PubMed] [Google Scholar]
- 33.Springer BD, Connelly SE, Odum SM, Fehring TK, Griffin WL, Mason JB, Masonis JL. Cementless femoral components in young patients: review and meta-analysis of total hip arthroplasty and hip resurfacing. J Arthroplasty. 2009;24(6 suppl):2–8. doi: 10.1016/j.arth.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 34.Springer BD, Fehring TK, Griffin WL, Odum SM, Masonis JL. Why revision total hip arthroplasty fails. Clin Orthop Relat Res. 2009;467:166–173. doi: 10.1007/s11999-008-0566-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Williams HD, Browne G, Gie GA, Ling RS, Timperley AJ, Wendover NA. The Exeter Universal cemented femoral component at 8 to 12 years: a study of the first 325 hips. J Bone Joint Surg Br. 2002;84:324–334. doi: 10.1302/0301-620X.84B3.12261. [DOI] [PubMed] [Google Scholar]
- 36.Yates PJ, Burston BJ, Whitley E, Bannister GC. Collarless polished tapered stem: clinical and radiological results at a minimum of ten years’ follow-up. J Bone Joint Surg Br. 2008;90:16–22. doi: 10.1302/0301-620X.90B1.19546. [DOI] [PubMed] [Google Scholar]
- 37.Young L, Duckett S, Dunn A. The use of the cemented Exeter Universal femoral stem in a district general hospital: a minimum ten-year follow-up. J Bone Joint Surg Br. 2009;91:170–175. doi: 10.1302/0301-620X.91B2.20473. [DOI] [PubMed] [Google Scholar]