Abstract
Objectives
To examine if incident severe sepsis is associated with increased risk of subsequent depressive symptoms and to assess which patient characteristics are associated with increased risk of depressive symptoms.
Design
Prospective longitudinal cohort study.
Setting
Population-based cohort of older U.S. adults interviewed as part of the Health and Retirement Study (1998–2006).
Participants
439 patients who survived 471 hospitalizations for severe sepsis and completed at least one follow-up interview.
Measurements
Depressive symptoms were assessed with a modified version of the Center for Epidemiologic Studies Depression Scale. Severe sepsis was identified using a validated algorithm in Medicare claims.
Results
The point prevalence of substantial depressive symptoms was 28% at a median of 1.2 years before sepsis, and remained 28% at a median of 0.9 years after sepsis. Neither incident severe sepsis [Relative Risk (RR) 1.00, 95%Confidence Interval (95%CI) (0.73, 1.34)] nor severe sepsis-related clinical characteristics were significantly associated with subsequent depressive symptoms. These results were robust to potential threats from missing data or alternative outcome definitions. After adjustment, pre-sepsis substantial depressive symptoms [RR 2.20, 95%CI (1.66, 2.90)] and worse post-sepsis functional impairment [RR 1.08 per new limitation, 95%CI (1.03, 1.13)] were independently associated with substantial depressive symptoms following sepsis.
Conclusions
The prevalence of substantial depressive symptoms in severe sepsis survivors is high, but is not increased relative to their pre-sepsis levels. Identifying this large subset of severe sepsis survivors at increased risk for major depression, and beginning interventions prior to hospital discharge, may improve outcomes.
Keywords: depression, sepsis, critical care, outcome assessment (health care)
INTRODUCTION
Millions of Americans are surviving critical illnesses annually, and patient-centered outcomes such as emotional well-being are becoming increasingly important.1,2 Serious acute illnesses such as acute lung injury and severe sepsis expose patients to enormous stressors such as respiratory insufficiency, pain, and delirium,3 and survivors may face considerable physical limitations during recovery which might plausibly cause depression.3,4 Two systematic reviews of 24 cohort studies of general intensive care unit and acute lung injury survivors have found that 28% of patients surviving critical illnesses may have substantial depressive symptoms.3,5 Major depression following critical illness is an important public health problem as depression is both a sizeable contributor to disability world-wide and independently associated with increased health care costs as well as adverse medical outcomes.6–8 Depression may also hamper patients' ability to participate in their often prolonged post-illness rehabilitation and thereby promote enduring disability.2
Yet, it is unclear if the illness experience, either through illness or treatment-related exposures, independently increases the risk of subsequent depression. Studies have argued that critical illnesses and their associated treatment-related exposures may have a causal role in increasing the risk of subsequent depression;9–13 these studies have motivated an NIH-funded randomized controlled trial of empiric escitalopram for patients undergoing mechanical ventilation (ClinicalTrials.gov identifier: NCT00872027). However, very few studies of post-critical illness depression are appropriately designed to test this hypothesis – only two have examined the contribution of premorbid depression using a standardized measure,14,15 of which only one examined pre-critical illness depressive symptoms prospectively in a small sample of critical illness survivors.15
In particular, little is known about the mental health outcomes of survivors of severe sepsis, the most common non-cardiac cause of critical illness.16 Depression in this patient population is especially concerning in light of recent evidence that older patients who survive severe sepsis are at increased risk for incident cognitive impairment and functional disabilities.17 Prior studies have suggested that post-critical illness physical and cognitive impairment may be associated with increased risk of depression.10,14,18 Since hundreds of thousands of patients develop severe sepsis annually,16 ascertaining the prevalence of, and risk factors for, depressive symptoms in survivors is vital since depression could be a contributor to functional decline in these patients that is amenable to treatment.
The present study utilizes an ongoing longitudinal cohort of older Americans to examine whether incident severe sepsis is associated with an increased risk of subsequent substantial depressive symptoms. This approach offers the distinct advantages of national scope and prospective assessment of depressive symptoms with a consistent instrument, and avoids the challenges of using proxy or retrospective assessment of baseline symptoms.19 We hypothesized that hospitalization for severe sepsis in-and-of-itself would not be significantly associated with an increased risk of subsequent substantial depressive symptoms after controlling for pre-sepsis depressive symptoms. In addition, we tested for an increased risk of substantial depressive symptoms among patients with select baseline characteristics, severe sepsis-related exposures, and post-severe sepsis functional impairments, hypothesizing that patients with pre-sepsis substantial depressive symptoms would be at increased risk for post-sepsis substantial depressive symptoms.
METHODS
Study Sample
Our study cohort comes from the Health and Retirement Study (HRS), a longitudinal investigation of community-dwelling U.S. adults over age 50. The study began in 1992, and to date over 27,000 individuals have participated. Subjects (and their spouses if married) are re-interviewed every 2 years. The HRS follow-up rate has exceeded 90–95%, including proxies,20 and 16,772 participants have consented for linkage of their Medicare claims records with study data. The HRS protocol was approved by the University of Michigan Institutional Review Board. Study participants provided informed consent upon enrollment and again for linkage to Medicare claims.
The present study examines all HRS respondents with at least 1 interview from 1998–2004 and for whom there were Medicare claims-based data for a subsequent hospitalization for severe sepsis from 1998–2005. All patients were followed up through death or the 2006 survey. Our analyses focus on severe sepsis hospitalizations that patients survived long enough to complete at least 1 interview.
Demographic and Clinical Characteristics
We obtained data on demographics (i.e., age, race and ethnicity, sex, education, and marital/partnered status), alcohol use and smoking from the HRS interviews.
Severe sepsis-related clinical characteristics were abstracted from the Medicare claims, including chronic medical conditions to compute a Charlson Comorbidity score,21 an organ dysfunction score (the sum of the number of organ failures of cardiovascular, neurologic, hematologic, hepatic, renal, or respiratory origin),16,22 hospital length of stay, admission to an intensive care unit, as well as requirements for mechanical ventilation, major surgery, and dialysis.
Definition of Severe Sepsis
We utilized a clinically validated and widely-used claims-based definition of severe sepsis.16,23–26 The definition requires evidence of a concomitant infection and new-onset organ dysfunction during a single hospitalization, consistent with the international consensus conference definitions of severe sepsis.24 We focus on severe sepsis as a single syndrome, rather than the underlying inciting infections, in line with current thinking that emphasizes the importance of the common host response in the pathogenesis and treatment of severe sepsis.27–32 For patients who had more than 1 distinct septic hospitalization, each hospitalization was included, with appropriate adjustment of the standard errors as described below.
Depressive Symptoms
The HRS assessed depression at each wave with an 8-item version of the Center for Epidemiologic Studies Depression Scale (CES-D).33 Prior studies have reported that this modified version loses little of the structure and precision of the original scale.34,35 Using a cutoff of 3 or more has been found to have a sensitivity of 71% and specificity of 79% for the diagnosis of major depression compared to structured diagnostic interview.36 We used a cutoff score of 4 or higher on the 8-item CES-D to define substantial depressive symptoms because this threshold was estimated to be comparable to the cutoff score of 16 or higher on the full CES-D by HRS investigators,37 and has been used in several prior studies.38–40 We defined pre-sepsis substantial depressive symptoms as a CES-D score reaching threshold at any interview before severe sepsis, while post-sepsis substantial depressive symptoms was defined similarly for any interview after severe sepsis.
Cognitive and Functional Impairment
The HRS assessed cognitive impairment in 2 ways as described in detail elsewhere.17 Briefly, participants were administered versions of the Telephone Interview for Cognitive Status. For those patients who were unable to be interviewed themselves, a proxy respondent completed assessments of cognitive impairment. We defined thresholds on the cognitive assessments for mild and moderate to severe cognitive impairment based on prior HRS studies.17,41
To examine functional status, respondents (or their proxies) were asked if they required assistance with any of 6 activities of daily living (ADLs): walking, dressing, bathing, eating, getting into or out of bed, and toileting, or 5 instrumental ADLs (IADLs): preparing a hot meal, shopping for groceries, making telephone calls, taking medicines, and managing money. We summed the number of impairments in ADLs and IADLs to create a total functional impairment score.17
Statistical Analysis
Our unit of analysis for all analyses was the hospitalization. Our outcome variable for all analyses was the presence of substantial depressive symptoms, operationalized as a dichotomous variable defined as a score of 4 or more depressive symptoms on the 8-item CES-D. We conducted two classes of analyses as described below:
Severe Sepsis and Substantial Depressive Symptoms
In order to test the hypothesis that severe sepsis is associated with an increased risk of substantial symptoms of depression, we used so-called “fixed effects” models which use the longitudinal nature of the data to control for all stable characteristics of the patients.17 We grouped patients who survived a severe sepsis hospitalization by the number of interviews they had completed since the severe sepsis episode. In these models, time from admission for severe sepsis to interview was measured to the day as a continuous variable. We used a hospitalization-level fixed effect, sometimes called conditional models.42 These results controlled for the patient's depressive symptoms status before his/her severe sepsis episode. Since our outcome was not rare, we used fixed-effects Poisson regression analyses to estimate the relative risk (RR) and 95% confidence intervals (95%CIs) for post-severe sepsis substantial depressive symptoms.43 We implemented this analysis using xtpoisson, fe in STATA 11 (Stata Corporation, College Station, TX). However, xtpoisson as currently implemented in STATA does not allow for correction of the standard errors to take into account the HRS' complex sampling design.44,45 Since there was a relatively small number of sepsis survivor cases per sampling strata in the HRS, we did not anticipate the HRS sampling design to undermine our application. Nonetheless, we replicated our analyses using within-person conditional logistic regression, implemented using STATA's clogit command. We found that our interpretation was invariant to whether or not sampling design was accounted for using a Taylor series linearized approximation (results available from authors upon request), and present the results of our fixed-effects Poisson regression models here. Additional information about our statistical approach is included in the appendix on statistical methods for the analyses (see document, Supplemental Digital Content 1).
An important methodological challenge in the analyses for the present study was that a substantial proportion of subjects (24%) were missing post-sepsis depression measurements, typically because the primary respondent was alive but unable to participate, so a proxy respondent was used. The HRS protocol did not ask proxies to report on depression measures.36 We took two approaches to quantifying the extent to which our results might be systematically biased by the possibility that survivors who had proxies were more likely to be depressed. First, we used propensity score adjustment to account for the likelihood of missing post-sepsis depression data.46 Second, we conducted simulation analyses in which we examined how much our results would change if we randomly assigned different prevalences of substantial depressive symptoms to patients who had converted from self-respondents pre-sepsis to requiring a proxy post-sepsis; we tested prevalences of 17%, 45% and 95%, based on prior studies that used proxy reports of patient depression.47–49 Further details are provided in the appendix on statistical methods for the analyses (see document, Supplemental Digital Content 1).
Patient Characteristics and Risk of Post-Sepsis Substantial Depressive Symptoms
To examine patient characteristics and clinical factors associated with an increased risk of post-sepsis substantial depressive symptoms, we used Poisson regression models with robust error variances.43 Since a history of prior major depression is known to be a potent predictor of depression in the context of stress,50 we initially tested the association of pre-sepsis substantial depressive symptoms with post-sepsis substantial depressive symptoms without adjustment. We then added three groups of potential confounding variables chosen a priori that have been found to be important in depression and general medical/critical illness-related research:3,9,10,12,51 1) demographics (age, sex, race, education, marital status), health risk behaviors (alcohol use and smoking), and medical comorbidity (Charlson score); 2) severe sepsis episode characteristics (organ dysfunction score, hospital length of stay, intensive care unit admission, mechanical ventilation, major surgery, and dialysis); and 3) post-severe sepsis function (level of cognitive impairment and total ADL and IADL impairments) as well as non-response propensity scores.
As a sensitivity analysis, we also examined whether our results were affected by using a cutoff score of 5 or higher to define substantial depressive symptoms on the 8-item CES-D.52
We used two-sided significance tests for all analyses with statistical significance set at a P value of 0.05. Analyses were performed with appropriate components of the IBM SPSS Statistics 18 (SPSS Inc., Chicago, IL) and STATA 11 (Stata Corporation, College Station, TX) statistical software programs.
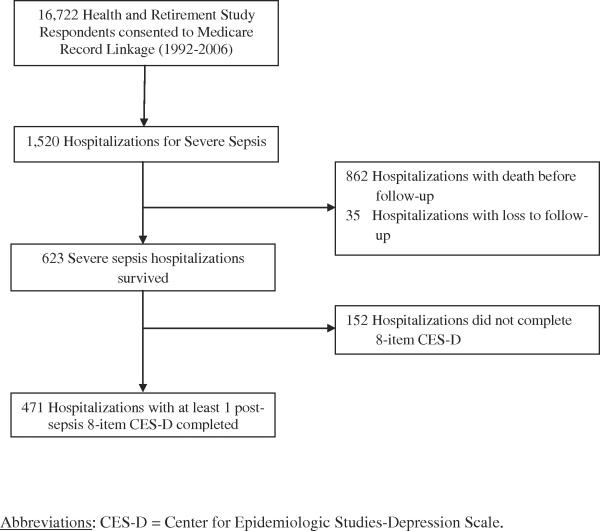
RESULTS
From 1998–2005, 516 HRS respondents survived 623 hospitalizations for severe sepsis (Figure 1). Of the surviving hospitalizations, 439 individuals (85%) completed at least one follow-up depression assessment. Patients were followed up for up to 4 surveys before severe sepsis (mean: 6.9 years) and up to 4 surveys (mean: 7.1 years) afterward. Table 1 describes the 471 hospitalizations for severe sepsis that completed at least one depression assessment. Their mean age at hospitalization was 75.3 years. As in other cohorts of patients who survive severe sepsis (16), nearly half were admitted to an intensive care unit, one quarter underwent major surgery, and mean length of stay was 10.8 days (S.D.: 10.3 days).
Figure 1.
Health and Retirement Study cohort for post-severe sepsis depression analyses
Table 1.
Patient and clinical characteristics of severe sepsis survivors with post-sepsis depression data
| Variables | Post-sepsis Depression Data Present (n = 471) |
|---|---|
| Panel A: Demographic & Social Characteristics | |
|
| |
| Age (years) | 75.3 (8.4) |
| Female | 248 (52.6%) |
| Race | |
| White | 378 (80.2%) |
| Black | 87 (14.0%) |
| Other | 6 (1.3%) |
| Education | |
| High school or less | 177 (37.6%) |
| Some college | 166 (35.2%) |
| College graduate | 128 (27.2%) |
| Living Arrangement | |
| Married/partnered | 256 (54.3%) |
| Unmarried but living with others | 78 (16.6%) |
| Unmarried and living alone | 135 (28.7%) |
| Alcohol use (days/week) | 1.6 (1.1) |
| Smoking Status | |
| Never smoked | 146 (31.0%) |
| Former smoker | 256 (54.4%) |
| Current smoker | 69 (14.6%) |
| Charlson Comorbidity Score | 1.9 (1.5) |
| Pre-sepsis cognitive function | |
| Normal | 441(93.6%) |
| Mild to moderate impairment | 22 (4.7%) |
| Moderate to severe impairment | 8 (1.7%) |
| Pre-sepsis ADL/Instrumental ADL impairments | 1.7 (2.5) |
| Missing pre-sepsis depression data | 9 (1.9%) |
|
| |
| Panel B: Characteristics of the Severe Sepsis Hospitalization | |
|
| |
| Organ Dysfunction Score | 1.2 (0.4) |
| Acute conditions | |
| Cardiovascular dysfunction | 125 (26.5%) |
| Neurologic dysfunction | 36 (7.6%) |
| Hematologic dysfunction | 100 (21.2%) |
| Hepatic dysfunction | 2 (0.4%) |
| Renal dysfunction | 184 (39.1%) |
| Respiratory dysfunction | 94 (20.0%) |
| Admitted to an intensive care unit | 220 (46.7%) |
| Required mechanical ventilation | 94 (20.0%) |
| Required major surgery | 106 (22.5%) |
| Required dialysis | 22 (4.7%) |
| Hospital length of stay (days) | 10.8 (10.3) |
| Post-sepsis cognitive function | |
| Normal | 456 (96.8%) |
| Mild to moderate impairment | 6 (1.3%) |
| Moderate to severe impairment | 9 (1.9%) |
| Post-sepsis ADL/Instrumental ADL impairments | 1.2 (2.1) |
All values are mean ± SD or n (%) unless otherwise indicated.
Abbreviations (in alphabetic order): ADL = Activities of Daily Living.
Pre- and Post-sepsis Depressive Symptom Prevalences
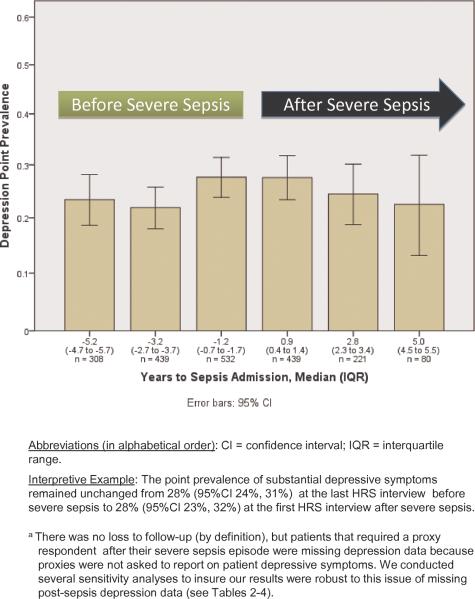
Figure 2 presents the point prevalence of substantial depressive symptoms before and after severe sepsis. The point prevalence of pre-sepsis substantial depressive symptoms was 28% (95%CI: 24%, 31%) at the most recent interview before sepsis, a median of 1.2 years pre-sepsis. The point prevalence of post-sepsis substantial depressive symptoms was unchanged, at 28% (95%CI: 23%, 32%) at the first interview after severe sepsis, a median of 0.9 years later.
Figure 2.
Point prevalence of substantial depressive symptoms among severe sepsis survivorsa
Effects of Severe Sepsis on Subsequent Substantial Depressive Symptoms
In fixed-effects regression, which controls for all patient characteristics that do not change over time, the incidence of severe sepsis was not associated with subsequent substantial depressive symptoms (Table 2). In a first sensitivity analysis, in which we adjusted for non-response propensity scores, we found the same result.
Table 2.
Severe sepsis and subsequent clinically significant depressive symptoms in survivorsa
| Relative Risk (95% Confidence Interval) | Z Statistic | P Value | |
|---|---|---|---|
| Analysis unadjusted for non-response propensity | |||
| Before sepsis (per additional year) | 1.05 (0.99–1.11) | 1.59 | 0.11 |
| Effect of sepsis | 1.00 (0.73–1.34) | −0.01 | 0.99 |
| After sepsis (per additional year) | 1.03 (0.93–1.13) | 0.52 | 0.60 |
| Adjusted for non-response propensity | |||
| Before sepsis (per additional year) | 1.03 (0.97–1.10) | 1.08 | 0.28 |
| Effect of sepsis | 0.95 (0.69–1.31) | −0.30 | 0.76 |
| After sepsis (per additional year) | 1.01 (0.91–1.12) | 0.19 | 0.85 |
Results of fixed-effects Poisson regression with hospitalization-level fixed effects, controlling for all time-invariant characteristics of the patient.
In our second sensitivity analysis, in which we varied the prevalence of substantial depressive symptoms among survivors who had converted from self-respondents pre-sepsis to requiring a proxy post-sepsis, we found no significant independent associations between incident severe sepsis and subsequent depressive symptoms in any of our simulations—including the extreme case where the randomly imputed prevalence of substantial depressive symptoms among patients who had converted from self-respondents pre-sepsis to requiring a proxy post-sepsis was 95% (Table 3).
Table 3.
Sensitivity analyses of severe sepsis and subsequent depression with imputation of depression prevalence of new post-sepsis proxy-requiring respondentsa
| 17% depression prevalence among new post-sepsis proxy-requiring respondents45 | 45% depression prevalence among new post-sepsis proxy-requiring respondents46 | 95% depression prevalence among new post-sepsis proxy-requiring respondents47 | |
|---|---|---|---|
| Median RR for Effect of Sepsis | 0.90 | 1.03 | 1.16 |
| 95% Range for Point Estimates of Effect of Severe Sepsis (2.5th percentile – 97.5th percentile for point estimate of RRs for effect of sepsis) | 0.82–0.99 | 0.93–1.13 | 1.13–1.20 |
| % of all simulations with statistically significant positive association between severe sepsis and depression | 0 | 0 | 0 |
Abbreviations (in alphabetical order): % = percent; RR = relative risk.
The results presented are from three sets of simulations of the fixed-effects regression analyses in which we imputed the presence of substantial depressive symptoms based on random assignment to patients who had converted from self-respondents pre-sepsis to requiring a proxy post-sepsis. These simulations were replicated 100 times.
In a third sensitivity analysis, we used the total 8-item CES-D score as a continuous variable in a fixed effects regression, assessing the total load of depressive symptoms rather than a dichotomous variable; again, there was no association between severe sepsis and depressive symptoms. There was also no association between severe sepsis and subsequent substantial depressive symptoms when we used a more stringent cutoff on the 8-item CES-D.
Factors Associated with Post-Sepsis Substantial Depressive Symptoms
In unadjusted Poisson regression analyses, substantial symptoms of depression at any interview prior to severe sepsis was associated with 2.62-times the risk [95%CI (2.00, 3.43), z = 7.01, P < 0.001] of substantial depressive symptoms at any interview following severe sepsis compared to patients without pre-sepsis substantial depressive symptoms. After sequential adjustment for baseline characteristics and severe sepsis-related clinical characteristics, only presepsis clinically significant depressive symptoms and female sex were consistently associated with post-sepsis substantial depressive symptoms (see documents, Supplemental Digital Content 2 and 3, which present the results of sequential adjusted analyses in tabular form). Notably, neither any single clinical characteristic of the severe sepsis-related hospitalization – nor the entire set of covariates in a joint test (χ2 = 8.20, degrees of freedom = 6, P = 0.22) – was significantly associated with risk of post-sepsis substantial depressive symptoms after controlling for pre-sepsis substantial symptoms of depression.
When we controlled for post-sepsis cognitive and functional impairment, only pre-sepsis substantial depressive symptoms [RR 2.20, 95%CI(1.67, 2.90), z = 5.56, P < 0.001] and an increasing number of ADL and IADL impairments following sepsis [1.08, 95%CI(1.04, 1.13), z = 3.49, P < 0.001] were significantly associated with post-sepsis substantial depressive symptoms. Adjustment for non-response propensity scores (Table 4) did not significantly change the results. In addition, our results were not substantively affected by using a cutoff of 5 or more depressive symptoms to define substantial depressive symptoms on the 8-item CES-D.
Table 4.
Fully adjusted associations of patient and clinical characteristics associated with substantial depressive symptoms among survivors of severe sepsisa
| Relative Risk (95% Confidence Interval) | Z Statistic | P Value | |
|---|---|---|---|
| Pre-sepsis patient characteristics | |||
| Substantial symptoms of depression at any HRS survey pre-sepsis | 2.20 (1.66–2.90) | 5.56 | < 0.001 |
| Age | 0.99 (0.96–1.02) | −0.81 | 0.42 |
| Female | 1.32 (1.00–1.75) | 1.93 | 0.05 |
| Black | 0.80 (0.58–1.09) | −0.65 | 0.52 |
| Education beyond high school | 0.99 (0.75–1.32) | −0.07 | 0.95 |
| Single and living alone | 1.22 (0.88–1.68) | 1.19 | 0.24 |
| Alcohol use (days/week) | 1.00 (0.87–1.16) | 0.04 | 0.97 |
| Current smoker | 0.73 (0.45–1.19) | −1.26 | 0.21 |
| Charlson Comorbidity Score | 1.05 (0.96–1.14) | 1.13 | 0.26 |
| Severe sepsis-related hospitalization characteristics | |||
| Organ dysfunction score | 0.95 (0.70–1.30) | −0.30 | 0.77 |
| Admitted to an intensive care unit | 0.81 (0.60–1.09) | −1.40 | 0.16 |
| Required mechanical ventilation | 1.18 (0.82–1.71) | 0.91 | 0.37 |
| Required major surgery | 1.11 (0.78–1.59) | 0.58 | 0.56 |
| Required dialysis | 0.64 (0.32–1.28) | −1.27 | 0.21 |
| Hospital length of stay | 0.99 (0.97–1.00) | −1.48 | 0.14 |
| Post-sepsis characteristicsb | |||
| Mild to moderate cognitive impairment | 1.03 (0.60–1.76) | 0.10 | 0.92 |
| Total ADL/instrumental ADL impairments | 1.08 (1.03–1.13) | 3.49 | <0.001 |
Abbreviations (in alphabetical order): ADL = Activities of Daily Living; HRS = Health and Retirement Study.
Adjusted for non-response propensity.
Since only 9 patients with moderate to severe cognitive impairment had a post-severe sepsis depression measure, the model omitted this covariate.
DISCUSSION
This examination of the largest, prospectively assessed cohort of older severe sepsis survivors demonstrates several previously unrecognized features of the association between severe sepsis and depression. First, the prevalence of substantial depressive symptoms is quite high among severe sepsis survivors – both before and after their hospitalization. Both the prevalence of substantial depressive symptoms at the last HRS interview before severe sepsis (28%) and the first interview after sepsis (28%) are considerably higher than the 1-year prevalence of substantial depressive symptoms in a study of U.S. community-dwelling older adults assessed with the same standardized instrument.53 Second, severe sepsis was not independently associated with an increased risk of subsequent substantial depressive symptoms, suggesting that surviving a severe illness by itself may not be sufficient as a cause of depression. Third, a prior history of depression was the most potent risk factor associated with substantial depressive symptoms following severe sepsis, even after adjusting for baseline patient characteristics, sepsis-related clinical factors, and post-sepsis functional impairment. To our knowledge, this study is the first investigation of depressive symptoms in survivors of severe sepsis, and is only the second study of post-critical illness depression to include a standardized measure of depressive symptoms administered to patients prospectively and prior to their critical illness.15
In contrast to the interpretation of past work, we found no significant associations between severe sepsis and subsequent depressive symptoms. Previous studies identified similar high rates of depression after intensive care unit admissions and acute lung injury.3,5 Our resultsv confirm these findings of a high post-illness prevalence of depressive symptoms, but substantially alter the interpretation by demonstrating that high prevalence to be unchanged from levels of depressive symptoms before the illness, at least among older Americans. Prior studies have also identified exposure to specific aspects of care as potential risk factors for subsequent depression,9,10,12 which we did not replicate. This discrepancy may be rooted in prior studies' inability to adequately control for premorbid depression, as depression is independently associated with acute care and intensive care unit admissions for medical illnesses.54,55 Further, some of these studies examined very early post-discharge depression, which is not well measured in the HRS. However, the median time from hospitalization for severe sepsis and first follow-up assessment in our study was 0.9 years (interquartile range 0.4–1.4 years), suggesting that the HRS allows the assessment of medium- and long-term associations with acute hospitalizations.
Depression in older patients surviving severe sepsis may be especially debilitating. Studies of older primary care patients have found that depression is an independent predictor of cognitive and functional decline.56,57 In light of prior HRS findings that an incident severe sepsis episode is associated with subsequent cognitive and functional impairments,17 substantial depressive symptoms in severe sepsis survivors could exacerbate their cognitive and functional decline or limit their ability to actively participate in rehabilitation.58 Furthermore, the high prevalence of substantial symptoms of depression prior to severe sepsis suggests that additional study is needed to examine if major depression is a potentially modifiable risk factor for sepsis, particularly in light of emerging evidence suggesting a bi-directional relationship between depression and medical conditions such as cardiovascular disorders and diabetes.51
A large body of prior research has established that critical illnesses are associated with subsequent neuromuscular dysfunction.59,60 If functional impairment is a cause of depression following severe sepsis, then efforts targeting early physical and cognitive rehabilitation in the intensive care unit, which have been shown to improve functional outcomes at hospital discharge,61 could prevent the development of subsequent depression. Furthermore, since premorbid depression appears to convey considerable risk for substantial symptoms of depression in the aftermath of severe sepsis, hospital programs that target older patients surviving severe sepsis with a prior history of depression—whether or not formally diagnosed—for careful monitoring of their subsequent mental health may improve outcomes. Studies of interventions that combine screening and treatment for comorbid depression and medical conditions in older adults have demonstrated reductions in depressive symptoms,62 as well as improved physical functioning and medical outcomes.62,63
Our study does have several important limitations. First, we studied older Americans. The associations with severe sepsis and depressive symptoms may be different in younger patients. However, sepsis has been called the “quintessential disease of aging,” 64 and over half of patients with severe sepsis are aged 65 and above.16 Second, since we assessed depressive symptoms with a questionnaire and not a diagnostic interview, a diagnosis of major depression could not be made. Third, the 8-item CES-D has been used in many relevant populations,38–40 but has not been specifically validated for use before and after severe sepsis. Fourth, we used a claims-based definition of severe sepsis, which although not the same as prospective clinical assessment, has been validated and widely used.16,23–26 Fifth, our study focused on patients who survived severe sepsis with treatments utilized in a range of U.S. hospitals at a specific point in time. New treatments for sepsis, as well as changes in life support or other hospital practices, may modify the sequelae of severe sepsis, even if these outcomes are not an explicit target of care. Furthermore, as longitudinal sampling weights are not available at this time for the HRS/Medicare data, this data was analyzed as a cohort of individual patients from a wide-range of hospitals, rather than to provide strict generalizability to the national depression prevalence. Finally, the possibility of residual confounding remains as in any observational study.
In conclusion, using a nationwide sample of older adults, we found that patients surviving severe sepsis have a prevalence of substantial depressive symptoms considerably higher than general population estimates. We did not find evidence that severe sepsis or its treatment-related exposures are associated with increased risk of subsequent depressive symptoms. However, we did identify that the risk of substantial depressive symptoms following a hospitalization for severe sepsis was 2.2-times higher for patients with premorbid substantial depressive symptoms. Additionally, greater post-sepsis functional impairment was also associated with substantial depressive symptoms. Future research to find interventions that prevent or ameliorate depressive symptoms in the aftermath of severe sepsis is particularly important given the enormous toll that sepsis and depression take on older patients, their families, and the healthcare system.
Supplementary Material
Acknowledgments
This work was supported by grants KL2 RR025015, NRSA-T32/MH20021-12, K08 HL091249-03, R01 AG030155, and U01 AG09740 from the National Institutes of Health. The Health and Retirement Study is performed at the Institute for Social Research, University of Michigan. We appreciate the expert programming of Tish Shapiro and Mohammed Kabeto, both at the University of Michigan.
Footnotes
Potential Conflicts of Interest: The authors have no relevant potential conflicts of interest to disclose.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the US government.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Iwashyna TJ. Survivorship will be the defining challenge of critical care in the 21st century. Ann Intern Med. 2010;153:204–205. doi: 10.7326/0003-4819-153-3-201008030-00013. [DOI] [PubMed] [Google Scholar]
- 2.Needham DM, Feldman DR, Kho ME. The functional costs of ICU survivorship: collaborating to improve post-ICU disability. Am J Respir Crit Care Med. 2011;183:962–964. doi: 10.1164/rccm.201012-2042ED. [DOI] [PubMed] [Google Scholar]
- 3.Davydow DS, Gifford JM, Desai SV, et al. Depression in general intensive care unit survivors: a systematic review. Intensive Care Med. 2009;35:796–809. doi: 10.1007/s00134-009-1396-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boyd CM, Ricks M, Fried LP, et al. Functional decline and recovery of activities of daily living in hospitalized, disabled older women: The Women's Health and Aging Study I. J Am Geriatr Soc. 2009;57:1757–1766. doi: 10.1111/j.1532-5415.2009.02455.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davydow DS, Desai SV, et al. Psychiatric morbidity in survivors of the acute respiratory distress syndrome: a systematic review. Psychosom Med. 2008;70:512–519. doi: 10.1097/PSY.0b013e31816aa0dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lopez AD, Mathers CD, Ezzati M, et al. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 7.Katon W, Lin E, Russo J, et al. Increased medical costs of a population-based sample of depressed elderly patients. Arch Gen Psychiatry. 2003;60:897–903. doi: 10.1001/archpsyc.60.9.897. [DOI] [PubMed] [Google Scholar]
- 8.Pan A, Lucas M, Sun Q, et al. Increased mortality risk in women with depression and diabetes mellitus. Arch Gen Psychiatry. 2011;68:42–50. doi: 10.1001/archgenpsychiatry.2010.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nelson BJ, Weinert CR, Bury CL, et al. Intensive care unit drug use and subsequent quality of life in acute lung injury patients. Crit Care Med. 2000;28:3626–3630. doi: 10.1097/00003246-200011000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Hopkins RO, Key CW, Suchyta MR, et al. Risk factors for depression and anxiety in survivors of acute respiratory distress syndrome. Gen Hosp Psychiatry. 2010;32:147–155. doi: 10.1016/j.genhosppsych.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 11.Dowdy DW, Dinglas V, Mendez-Tellez PA, et al. Intensive care unit hypoglycemia predicts depression during early recovery from acute lung injury. Crit Care Med. 2008;36:2726–2733. doi: 10.1097/CCM.0b013e31818781f5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dowdy DW, Bienvenu OJ, Dinglas VD, et al. Are intensive care factors associated with depressive symptoms 6 months after acute lung injury? Crit Care Med. 2009;37:1702–1707. doi: 10.1097/CCM.0b013e31819fea55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Herridge MS, Tansey CM, Matté A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364:1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 14.Weinert C, Meller W. Epidemiology of depression and antidepressant therapy after acute respiratory failure. Psychosomatics. 2006;47:399–407. doi: 10.1176/appi.psy.47.5.399. [DOI] [PubMed] [Google Scholar]
- 15.Davydow DS, Hough CL, Russo JE, et al. The association between intensive care unit admission and subsequent depression in patients with diabetes. Int J Geriatr Psychiatry. 2011 Feb 9; doi: 10.1002/gps.2684. doi: 10.1002/gps.2684. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Iwashyna TJ, Ely EW, Smith DM, et al. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304:1787–1794. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jackson JC, Hart RP, Gordon SM, et al. Six-month neuropsychological outcome of medical intensive care unit patients. Crit Care Med. 2003;31:1226–1234. doi: 10.1097/01.CCM.0000059996.30263.94. [DOI] [PubMed] [Google Scholar]
- 19.Gifford JM, Husain N, Dinglas VD, et al. Baseline quality of life before intensive care: a comparison of patient versus proxy responses. Crit Care Med. 2010;38:855–860. doi: 10.1097/CCM.0b013e3181cd10c7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. [Accessed March 6, 2011];Health and Retirement Study: Sample sizes and response rates. http://hrsonline.isr.umich.edu/sitedocs/sampleresponse.pdf.
- 21.Charlson ME, Pompei P, Ales KL. A new method for classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 22.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9 CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 23.Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979–2000. N Engl J Med. 2003;34:1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 24.Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31:1250–1256. doi: 10.1097/01.CCM.0000050454.01978.3B. [DOI] [PubMed] [Google Scholar]
- 25.Weycker D, Akrhas KS, Edelsberg J, et al. Long-term mortality and medical care charges in patients with severe sepsis. Crit Care Med. 2003;31:2316–2323. doi: 10.1097/01.CCM.0000085178.80226.0B. [DOI] [PubMed] [Google Scholar]
- 26.Lee H, Doig CJ, Ghali WA, et al. Detailed cost analysis of care for survivors of severe sepsis. Crit Care Med. 2004;32:981–985. doi: 10.1097/01.ccm.0000120053.98734.2c. [DOI] [PubMed] [Google Scholar]
- 27.Angus DC. Management of sepsis: a 47-year-old woman with an indwelling intravenous catheter and sepsis. JAMA. 2011;305:1469–1477. doi: 10.1001/jama.2011.438. [DOI] [PubMed] [Google Scholar]
- 28.Annane D, Bellissant E, Cacvaillon J-M. Septic Shock. Lancet. 2005;365:63–78. doi: 10.1016/S0140-6736(04)17667-8. [DOI] [PubMed] [Google Scholar]
- 29.Dellinger RP, Levy MM, Carlet JM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med Jan. 2008;36:296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- 30.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 31.Bernard GR, Vincent JL, Laterre PF, et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 2001;344:699–709. doi: 10.1056/NEJM200103083441001. [DOI] [PubMed] [Google Scholar]
- 32.Zahar J-R, Timsit J-F, Garrouste-Orgeas M, et al. Outcomes in severe sepsis and patients with septic shock: pathogen species and infection sites are not associated with mortality. Crit Care Med. 2011;39:1886–1895. doi: 10.1097/CCM.0b013e31821b827c. [DOI] [PubMed] [Google Scholar]
- 33.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 34.Soldo BJ, Hurd MD, Rodgers WL, et al. Asset and health dynamics of the oldest old: an overview of the AHEAD study. J Gerontol B Psychol Soc Sci. 1997;52:1–20. doi: 10.1093/geronb/52b.special_issue.1. [DOI] [PubMed] [Google Scholar]
- 35.Kohout FJ, Berkman LF, Evans DA, et al. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993;5:179–183. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 36.Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. Int Psychogeriatr. 1999;11:139–148. doi: 10.1017/s1041610299005694. [DOI] [PubMed] [Google Scholar]
- 37.Steffick D. Documentation of affective functioning measures in the Health and Retirement Study. Survey Research Center; Ann Arbor, Michigan: 2000. [Google Scholar]
- 38.Langa KM, Valenstein MA, Fendrick AM, et al. Extent and cost of informal caregiving for older Americans with symptoms of depression. Am J Psychiatry. 2004;161:857–863. doi: 10.1176/appi.ajp.161.5.857. [DOI] [PubMed] [Google Scholar]
- 39.Zivin K, Llewellyn DJ, Lang IA, et al. Depression among older adults in the United States and England. Am J Geriatr Psychiatry. 2010;18:1036–1044. doi: 10.1097/JGP.0b013e3181dba6d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mezuk B, Bohnert ASB, Ratliff S, et al. Job strain, depressive symptoms, and drinking behavior among older adults: results from the Health and Retirement Study. J Gerontol B Psychol Sci Sco Sci. 2011;66:426–434. doi: 10.1093/geronb/gbr021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Langa KM, Larson EB, Karlawish JH, et al. Trends in the prevalence and mortality of cognitive impairment in the United States: is there evidence of a compression of cognitive morbidity? Alzheimers Dement. 2008;4:134–144. doi: 10.1016/j.jalz.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Allison PD. Fixed Effects Regression Models. Sage; Thousand Oaks: 2009. [Google Scholar]
- 43.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 44. [Accessed January 30, 2012];Health and Retirement Study: Sample evolution: 1992–1998. http://hrsonline.isr.umich.edu/sitedocs/surveydesign.pdf.
- 45.Levy PS, Lemeshow S. Sampling of populations. John Wiley & Sons; New York: 1999. [Google Scholar]
- 46.Rao RS, Sigurdson AJ, Doody MM, et al. An application of a weighting method to adjust for non-response in standardized incidence-ratio analysis of cohort studies. Ann Epidemiol. 2005;15:129–136. doi: 10.1016/j.annepidem.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 47.Steffens DC, Fisher GG, Langa KM, et al. Prevalence of depression among older Americans: the Aging, Demographics, and Memory Study. Int Psychogeriatr. 2009;21:879–888. doi: 10.1017/S1041610209990044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Peters KR, Rockwood K, Black SE, et al. Characterizing neuropsychiatric symptoms in subjects referred to dementia clinics. Neurology. 2006;66:523–528. doi: 10.1212/01.wnl.0000198255.84842.06. [DOI] [PubMed] [Google Scholar]
- 49.Peters KR, Rockwood K, Black SE, et al. Neuropsychiatric symptom clusters and functional disability in cognitively-impaired-not-demented individuals. Am J Geriatr Psychiatry. 2008;16:136–144. doi: 10.1097/JGP.0b013e3181462288. [DOI] [PubMed] [Google Scholar]
- 50.Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in men. Am J Psychiatry. 2006;163:115–124. doi: 10.1176/appi.ajp.163.1.115. [DOI] [PubMed] [Google Scholar]
- 51.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry. 2003;54:216–226. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- 52.Polsky HR, Doshi JA, Marcus S, et al. Long-term risk for depressive symptoms after a medical diagnosis. Arch Intern Med. 2005;165:1260–1266. doi: 10.1001/archinte.165.11.1260. [DOI] [PubMed] [Google Scholar]
- 53.Han B. The impact of age, gender, and race on the relationship between depression and self-rated health in community-dwelling older adults: a longitudinal study. Home Health Care Serv Q. 2001;20:27–43. doi: 10.1300/J027v20n03_02. [DOI] [PubMed] [Google Scholar]
- 54.Himelhoch S, Weller WE, Wu AW, et al. Chronic medical illness, depression, and use of acute medical services among Medicare beneficiaries. Med Care. 2004;42:512–521. doi: 10.1097/01.mlr.0000127998.89246.ef. [DOI] [PubMed] [Google Scholar]
- 55.Davydow DS, Russo JE, Ludman E, et al. The association of comorbid depression and intensive care unit admission in patients with diabetes: a prospective cohort study. Psychosomatics. 2011;52:117–126. doi: 10.1016/j.psym.2010.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Spitzer RL, Kroenke K, Linzer M, et al. Health-related quality of life in primary care patients with mental disorders. Results from the PRIME-MD 1000 Study. JAMA. 1995;274:1511–1517. [PubMed] [Google Scholar]
- 57.Steffens DC, Snowden M, Fan MY, et al. Cognitive impairment and depression outcomes in the IMPACT Study. Am J Geriatr Psychiatry. 2006;14:401–409. doi: 10.1097/01.JGP.0000194646.65031.3f. [DOI] [PubMed] [Google Scholar]
- 58.DiPietro L. Physical activity in aging: changes in patterns and their relationships to health and function. J Gerontol A Biol Sci Med Sci. 2001;56:S13–S22. doi: 10.1093/gerona/56.suppl_2.13. [DOI] [PubMed] [Google Scholar]
- 59.Hough CL, Steinberg KP, Thompson BT, et al. Intensive care unit-acquired neuromyopathy and corticosteroids in survivors of persistent ARDS. Intensive Care Med. 2009;35:63–68. doi: 10.1007/s00134-008-1304-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Callahan LA, Supinski GS. Sepsis-induced myopathy. Crit Care Med. 2009;37:S354–S367. doi: 10.1097/CCM.0b013e3181b6e439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients. Lancet. 2009;373:1874–1882. doi: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Katon WJ, Lin EHB, Von Korff M, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363:2611–2620. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Callahan CM, Kroenke K, Counsell SR, et al. Treatment of depression improves physical functioning in older adults. J Am Geriatr Soc. 2005;53:367–373. doi: 10.1111/j.1532-5415.2005.53151.x. [DOI] [PubMed] [Google Scholar]
- 64.Milbrandt EB, Eldadah B, Nayfield S, et al. Toward an integrated research agenda for critical illness in aging. Am J Respir Crit Care Med. 2010;182:995–1003. doi: 10.1164/rccm.200904-0630CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.