Abstract
Dyspnea is the main symptom perceived by patients affected by chronic respiratory diseases. It derives from a complex interaction of signals arising in the central nervous system, which is connected through afferent pathway receptors to the peripheral respiratory system (airways, lung, and thorax). Notwithstanding the mechanism that generates the stimulus is always the same, the sensation of dyspnea is often described with different verbal descriptors: these descriptors, or linguistic 'clusters', are clearly influenced by socio-individual factors related to the patient. These factors can play an important role in identifying the etiopathogenesis of the underlying cardiopulmonary disease causing dyspnea. The main goal of rehabilitation is to improve dyspnea; hence, quantifying dyspnea through specific tools (scales) is essential in order to describe the level of chronic disability and to assess eventual changes after intervention. Improvements, even if modest, are likely to determine clinically relevant changes (minimal clinically important difference, MCID) in patients.
Currently there exist a large number of scales to classify and characterize dyspnea: the most frequently used in everyday clinical practice are the clinical scales (e.g. MRC or BDI/TDI, in which information is obtained directly from the patients through interview) and psychophysical scales (such as the Borg scale or VAS, which assess symptom intensity in response to a specific stimulus, e.g. exercise).
It is also possible to assess the individual's dyspnea in relation to specific situations, e.g. chronic dyspnea (with scales that classify patients according to different levels of respiratory disability); exertional dyspnea (with tools that can measure the level of dyspnea in response to a physical stimulus); and transitional (or 'follow up') dyspnea (with scales that measure the effect in time of a treatment intervention, such as rehabilitation).
Keywords: Chronic respiratory diseases, dyspnea, rehabilitation.
Dyspnea, the main symptom present in patients with chronic respiratory diseases, is a general term that characterizes a subjective sensation of difficulty in breathing [1]. In clinical practice, the quantitative assessment of this symptom can be useful for defining the patient's real level of respiratory disability; applied in pulmonary rehabilitation (PR) as an outcome measure it is useful to establish the efficacy - in terms of improvement of symptoms - of the intervention carried out, particularly in relation to programs that include general exercise training [2].
The Language of Dyspnea
Although it is an aspecific symptom generated through a common mechanism, dyspnea consists of qualitatively distinct sensations that vary in intensity and that, influencing the patient's personal perception, are closely dependent upon multiple personal factors such as socio-economic status, linguistic aspects, affective-cultural components and previous personal experience [3-5].
Hence, since dyspnea is perceived and described in different terms and modes, it is retained that there exist a series of 'descriptors' [1] indispensable for the expression of a specific language linked to efficacy of intervention and to defining the underlying pathophysiological causal mechanisms [4-6].
Regarding these multiple distinct sensations, diverse verbal descriptors have been grouped into distinctive "clusters" that have a high discriminating capacity [4-6]: a recent study [7], in fact, claims that the language used to describe the sensation of dysnea is capable of differentiating and thus classifying, through specific descriptors, individuals affected by chronic obstructive pulmonary diseases (COPD).
In the field of cardiopulmonary disease, the five descriptive clusters in the language of dyspnea most frequently selected are: 'chest tightness', 'increased effort of breathing', 'unsatisfied inspiratory effort', 'rapid or superficial breathing' and 'breathlessness' [1].
The sensation of 'chest tightness', frequently reported by asthmatic patients during acute bronchial obstruction, may derive from the stimulation of the pulmonary sensory receptors through vagal and autonomous pathways [8]: these slow adapting receptors, excited by the contraction of the airway muscle fibers, together with receptors from irritation (fast adapting) and C fibers could respond to the local airways inflammation [8]. Supporting this hypothesis would be the clinical observation that anesthesia of the airways with lidocaine induces the chest constriction associated to bronchial obstruction induced by histamine [9].
The cluster 'increased work or effort of breathing' includes instead descriptors often selected in conditions of increased mechanical load, such as occurs in COPD and in interstitial or neuromuscular diseases. The work/effort element, inadequate due to respiratory muscle fatigue or such as occurs during physical exercise, provokes an increase of the 'corollary discharge' [10] (central motor command to the sensitive cortex through small, highly localized interneurones in the central nervous system, that function as sensory receptors). The intensity of the command, alone or in combination with the force generation and contraction of the respiratory muscles, is appreciated at the conscious level as 'difficulty of breathing' [11].
The respiratory muscles are nevertheless important in the experience of dyspnea. 'Unsatisfied inspiratory effort' is a cluster that refers to conditions in which there is a disparity between central respiratory output and mechanical response of the respiratory system and it is considered to play a fundamental role in the increased perception of dyspnea during physical exercise in patients affected by COPD and interstitial diseases [12-14]. In COPD, in fact, dynamic hyperinflation during exercise contributes most to provoke mechanical limitations of the chest cage with a consequent increase of end-expiration lung volume and limitation to the increase of both flow volume and inspiratory capacity, responsible in their turn for the sensation of 'difficulty of breathing in' [12,15]. Reduced lung volumes and increased central respiratory drive explain the imbalance between increased central stimulus and probable reduction of the peripheral feedback between lung and rib cage [12,13]. The perception of this disparity is possible since the corollary discharge is modulated by a series of peripheral mechanoreceptors that provide precise information on the inspiratory muscles, on variations of flow-volume produced and on the calibre of the airways [11]. The disparity between this sensory feedback and the degree of effort in breathing is what underlies a pathogenetic mechanism of dyspnea recently proposed and defined as 'neuroventilatory dissociation' [12].
'Rapid or shallow breathing' is the respiratory cluster referred as a transitory experience by normal subjects during intense physical exercise or in the presence of external chest restriction [4-6]; it characterizes, in pathological terms, the response to exercise of patients with interstitial diseases [14]. The increased central drive provokes an increased breathing rate due to the reduced lung elastance: this mechanism would appear to be mediated by vagal receptors [16].
'Breathlessness', 'lack of breath' or 'a sense of suffocation' is a cluster that tends often to be associated to patients affected by congestive heart failure or other pathophysiological conditions (pregnancy, physical exercise, COPD). This dyspnea cluster is characterized by an increased respiratory drive, usually associated to increased ventilation [4]; it is in any case probable that the increased "impuse to breathe" comes directly from chemoreceptor afferents and from an increased alveolar partial pressure of carbon dioxide in the blood (PaCO2) [17]. In addition, this mechanism seems not to depend directly on the activation of the respiratory muscles or on an increase of pulmonary ventilation: in patients with a high cervical lesion on mechanical ventilation, in fact, the addition of PaCO2 to the inspired gas produces a "hard to breathe" sensation characterized by the "hunger for air" notwithstanding that ventilation is maintained at a constant level [17].
Dyspnea Scales and Their Clinical Significance
In patients with chronic respiratory disability improving exercise tolerance and the correlated symptom of dyspnea constitutes the main goal of rehabilitation. Assessment of dyspnea, thus, is essential as an outcome marker of efficacy. Moreover, in patients admitted to PR programs, the assessment of dyspnea during exercise makes it possible to tailor the training program to the patient's needs and capacities [18,19].
In reality, the difficulty of "measuring" a symptom implicates, as already stated, the need to be able to translate a subjective personal experience into a numeric parameter. Furthermore, the symptom of dyspnea represents a single and specific dimension of respiratory disease, measurable only through direct assessment: it is not, in fact, possible to evaluate it indirectly from other instrumental examinations such as, for example, lung function tests [20]. The use of specific tools (assessment scales) to quantify dyspnea thus permits to classify the severity of the symptom and the distress generated thereby, and to monitor it over time (Table 1).
Table 1.
Instruments for Measuring Dyspnea and their Field of Application in Clinical Practice and Rehabilitation
| Dyspnea assessment | |||
|---|---|---|---|
| Measurement tool | chronic | at exercise | at follow up |
| MRC | ++ | - | ++ |
| BDI | ++ | - | ++ |
| TDI | - | ++ | + |
| Modified Borg Scale | - | +++ | - |
| VAS | - | ++ | - |
| LCADL | ++ | - | ++ |
| PFSDQ | ++ | - | ++ |
| OCD | - | + | - |
Definition of abbreviations: BDI, Baseline Dyspnea Index; LCADL, London Chest Activity of Daily Living Scale; MRC, Medical Research Council; OCD, Oxygen Cost Diagram; PFSDQ, Pulmonary Functional Status and Dyspnea Questionnaire; TDI, Transitional Dyspnea Index; VAS, Visual Analogue Scale. +, ++, +++: different levels of specificity; -: absence of specificity.
Numerous clinical studies have thus utilized dyspnea - through variations of the assessment scales - as a clinical outcome useful for evaluating the response to muscle training interventions: these changes in symptoms, even if of a modest size, can produce clinically significant variations in the patients (minimally clinically important difference, MCID) (Figure 1) [2]. A statistical criterion useful for analyzing the sensitivity of the dyspnea assessment tool in terms of the effect of rehabilitation can be obtained by determining the "Effect Size" (ES), mathematically calculable as the variation of the score after a rehabilitation intervention divided by the standard deviation of the baseline value [21]: a greater variation of dyspnea linked to PR evidences a high value of ES.
Figure 1.
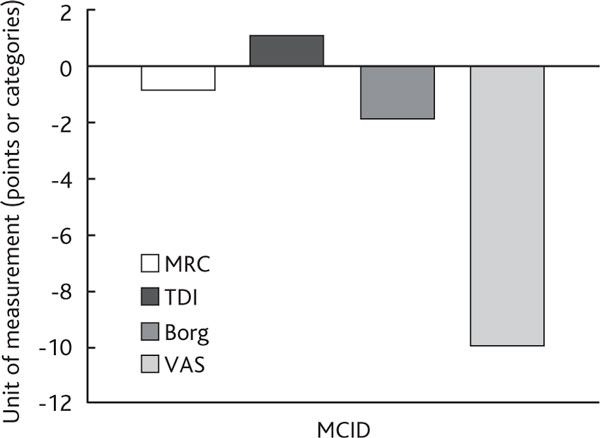
Dyspnea Measurement Tools and Relative Changes (Post-Rehabilitation) According to the MCID. Definition of abbreviations: MCID, minimal clinically important difference; MRC, Medical Research Council; TDI, Transitional Dyspnea Index; VAS, Visual Analogue Scale.
At present, there exist numerous modes for classifying and characterizing the tools used to assess dyspnea. Substantially, one can distinguish "discriminative" scales (that differentiate study populations based on the level of perceived dyspnea) from "evaluative" tools (that identify variations with respect to a baseline condition). In addition one can distinguish "categorical" scales, that quantify the symptom according to categories (mild, moderate and severe dyspnea, as in the Borg Scale), from "analogical" scales (e.g. the Visual Analogue Scale or VAS, where the determination of the severity of dyspnea is of an analogical type). Furthermore, depending on the relationship that exists between assessment scale and the symptom it is possible to distinguish "direct" scales (that investigate directly the level of the symptom perceived) and "indirect" (that evaluate, for example, the activities that dyspnea limits in daily life). Finally, based on whether the assessment tool identifies a single or several dimensions of the sensation of dyspnea it is possible to distinguish "unidimensional" scales (which consider only the type of activity that provokes the dyspnea) from "multidimensional" scales (which also take other aspects into account, such as functional impairment, the size of the task that evokes dyspnea and the degree of exertion associated to the sensation).
In daily clinical practice there exist thus "clinical" scales (completed by the patient during the medical interview) and "psycho-physical" scales (that evaluate the intensity of the symptom as a response to a stimulus, such as physical exercise or pharmacologically induced bronchodilatation).
Clinical scales
Medical Research Council (MRC) scale
Defined in 1959 by Fletcher et al. [22] the MRC scale, the first clinical scale for the determination of dyspnea, is a 5-point scale based on the sensation of breathing difficulty experienced by the patient during daily life activities (Table 2). Patients, reading the scale, are invited to recognize their own level of respiratory fatigue or, as is more often the case, the MRC can be directly administered.
Table 2.
Modified Medical Research Council (MRC) Scale
| 0. | I only get breathless with strenuous exercise |
|---|---|
| 1. | I get short of breath when hurrying on the level or walking up a slight hill |
| 2. | I walk slower than people of the same age on the level because of breathlessness or have to stop for breath when walking at my own pace on the level |
| 3. | I stop for breath after walking about 100 yards or after a few minutes on the level |
| 4. | I am too breathless to leave the house or I am breathless when dressing |
From [23] mod.
Level 0 represents the lowest level of dyspnea impairment perceived, level 4 the greatest dyspnea impairment. While for level 0 and 1 the MRC is considered as a symptomatic scale, in that the effort that produces the symptom is defined, levels 2, 3 and 4 yield indications concerning personal capacities and social impact (see Table 2). As regards the activity theshold able to evoke the sensation of dyspnea, the MRC is not able to evaluate the mode of performing the task, nor the effort or time required to complete it.
Hence, while it is widely used in the field of rehabilitation, mostly as a discriminative tool to characterize study populations or stratify patients with diverse lung function impairment [23], the use of the MRC scale, due to the limited number of levels present, may not be specific enough to detect moderate changes. Variations of 1 point in the scale nevertheless signify a perceived clinical improvement [24].
Baseline Dyspnea Index (BDI) - Transitional Dyspnea Index (TDI)
These two tools [25] are often used in rehabilitation both as a measure of treatment outcome and to assess daily living activities (see below). While the BDI, as its name indicates, constitutes the initial baseline assessment (discriminative tool), the TDI is administered at a certain point after the rehabilitation intervention has been carried out and it provides a measure of change with respect to the baseline value.
The unique feature of the BDI and TDI is that they are composed of three categories (functional impairment, magnitude of task and magnitude of effort) that are useful for quantifying the limitation due to dyspnea or the patient's capacities that have been impaired [25].
In the BDI each of the three categories has 5 levels of symptom severity from 0 to 4 where 0 corresponds to the most severe level: summing the scores for each category, a lower total score indicates a worse clinical condition (12 is the maximum possible score which corresponds to the least physical limitation the patient can experience). The scale can be administered informally by the doctor, nurse or physiotherapist during the patient's medical interview and takes from 4 to 5 minutes to complete: recently, a computerized version of the BDI has been introduced in order to compare the total scores obtained by different interviewers.
In the area of 'functional impairment' (due to respiratory disease), functional loss is evaluated in the sphere of both daily living and occupational activities, which are often completely suspended. 'Magnitude of task' on the other hand assesses what daily living tasks can provoke dyspnea, presenting activities of increasing intensity with 5 available response levels, 0 indicating always the greatest degree of impairment (dyspnea at rest). Finally, 'magnitude of effort' evaluates specifically how much effort needs to be sustained by the patient to evoke dyspnea. This last aspect of the BDI is perhaps the most singular in that it differentiates patients who, while performing the same activities, sustain efforts that are extremely diverse; the variable "time needed to perform the activity" is also explored together with the type of activity (more or less strenuous).
Concerning the reliability of the BDI, several reports have shown a good correlation between the BDI total score and follow up assessments [26], good inter-observer agreement [27] and good correlation with total scores of other dyspnea scales [28,29]. Regarding use of the TDI, in order to explore with respect to the baseline condition any functional changes (including type and degree) it is necessary to use the scores of the BDI as a reference point and remind the patient about the comments and choices made during the initial interview. The patient accordingly can choose the score 0 (no change) or report a slight, moderate or marked change, worse or improved with respect to baseline (3 levels above or below zero) and this gives the scale great sensitivity in determining changes in dyspnea. The scores of the 3 categories are thus summed to obtain the total score (variation) of the TDI which ranges between - 9 and + 9.
Used in studies with COPD patients in clinically stable condition, the TDI has shown to be sensitive in measuring changes in dyspnea after use of pharmacological drugs (e.g. tiotropium) [30] and in measuring the progressive decline in lung function [31]: variations of + 1 represent the threshold of MCID at which the patient can perceive an improvement of dyspnea (from BDI) [32]. However, in the rehabilitation of COPD patients, use of the TDI to assess outcome with respect to muscle training has shown this scale to be not particularly adequate or sensitive to perceived improvement in dyspnea [33].
Psychophysical scales
Psychophyscial evaluation is a branch of psychology that studies the laws that regulate the perception of sensations in response to variations of stimulus. Experimental studies of Stevens [34] in 1957 made it possible to quantify perceptions by means of methods and techniques regarding the estimation of magnitude (the subject attributes a numerical score to a workload added) and the reproduction of magnitudes (the subject increases or reduces the stimulus until the sensation is equal to a multiple or fraction, as requested, of the baseline stimulus). In this type of scale an absolute zero can be identified (absense of perception of the symptom) and the intervals in the score are equidistant.
The psychophysical approach has made an important contribution to the quantification of dyspnea, in particular to dyspnea arising during physical exercise and which can be evaluated by means of laboratory tests (cardiopulmonary exercise test, CPX) or field tests (6-min walking test, 6MWT).
Gunnar Borg in the '70s, building on these premises, elaborated a categorical scale, the Rating of Perceived Exertion (RPE) [35], and the subsequent modified version of the 10 Category-Ratio (CR 10) [36], both used to assess the sensation of exertional dyspnea and fatigue perceived during physical activity.
From the methodological point of view, however, the Borg scales require particular care and attention in their administration. The operator must a priori evaluate the patient's emotive disposition (since patients can over- or under-estimate the perception and quantification of the symptom) in order to be certain that they have understood all the information required to complete the scale and also that the score they give to the symptom as they perceive it regards "their sensation", i.e. it will not be judged or corrected.
Rating of Perceived Exertion (RPE)
The RPE [35] is a categorical scale with verbal descriptors (termed anchors) associated to a score that rates the perceived level of exertion. The author designed this dyspnea scale to overcome the limits of comparing scores between different subjects: for the same numerical score attributed to a sensation, in fact, one cannot be sure that for two different subjects the sensation is the same, and it is thus not possible to compare scores across subjects.
The verbal anchors thus create categories of sensation with which subjects can easily identify: "moderate intensity" is placed at the center of the scale, "strong" and "weak" symmetrically at the two ends of the scale.
The principle of the scale - composed of 15 levels, from 6 to 20 - is based on the notion that during physical exercise a close correlation exists between heart rate (HR) and workload: the scores of the RPE have in fact been translated from values of HR during exercise tests in a normal subject, where the score 6 corresponds to 60 beats/min (medium resting HR) and the score 20 to the other extreme, i.e. 200 beats/min (considered as the maximum HR attainable at exercise peak).
10 Category-Ratio (CR 10)
The CR 10 [36] is a categorical scale with a score from 0 to 10, where 0 (as a measure of dyspnea) corresponds to the sensation of normal breathing (absence of dyspnea) and 10 corresponds to the subject's maximum possible sensation of dyspnea. Also with this assessment tool the reference values are always linked to verbal anchors, chosen from commonly used terms, to facilitate the evaluation and recall the sensation to the patient's mind. Above the value of 10 it is possible for the patient to give a higher score, if they wish: this allows patients to connotate with still greater precision their own sensation (it is thus an open scale).
The version of the CR 10 that is usually administered in respiratory patients is the version modified by Mahler and Horowitz in 1994 [37] known as the "Modified Borg Scale" (Table 3) which uses specific descriptors of dyspnea. In the field of rehabilitation, the modified Borg scale is widely used as an instrument to prescribe workload during muscle training sessions [18], and the clinical significance of the rehabilitation outcome (in terms of perceived dyspnea during physical exercise) has been validated [38]. Now, since the perception of exercise induced dyspnea depends on the stimulus to which the patient has been subjected, the evaluation by means of the Borg scale should ideally be carried out at the same workload.
Table 3.
Modified Borg Scale
| 0 | (Dyspnea) NONE |
|---|---|
| 0.5 | (Dyspnea) EXTREMELY MILD |
| 1 | (Dyspnea) VERY MILD |
| 2 | (Dyspnea) MILD |
| 3 | (Dyspnea) MODERATE |
| 4 | (Dyspnea) INTENSE |
| 5 | (Dyspnea) RATHER INTENSE |
| 6 | |
| 7 | (Dyspnea) VERY INTENSE |
| 8 | |
| 9 | (Dyspnea) ALMOST UNBEARABLE |
| 10 | (Dyspnea) UNBEARABLE |
From [37], mod.
Numerous studies in COPD patients have used this scale as an outcome measure [39-41]. In reference to CPX, for the measurement of dyspnea in muscle training pre- and post- intervention, variations of -1.8 units (ES = 1.0) [39] and -2 units (ES = 1.5) [41] have been documented in iso-workload assessments at incremental CPX, while changes of -1.6 units (ES = 0.8) have been reported in iso-time evaluations at endurance CPX [39].
Concerning use of the 6MWT as a stimulus test for dyspnea in COPD patients on oxygen therapy (with respect to a group of COPD patients not on oxygen therapy), one study [41] showed a non significant reduction of dyspnea according to the Borg scale (4.1 vs. 4.8; ES = 0.5). Significant findings were reported instead (mean reduction of 3.6 units, ES = 1.8) in emphysematous patients undergoing lung reduction surgery (iso-work load at incremental exercise testing) [42].
In general, however, it is known that variations of 2 units with respect to baseline are associated to a sensation of perceived improvement [43], this being more evident in patients with a higher baseline respiratory disability.
Visual Analogue Scale (VAS)
First described by Aitken in 1969 [44], the VAS (Figure 2) found its first field of application in evaluating different sensations, and only subsequently was it applied to determine dyspnea. It is a closed scale (delimited at its two ends) composed graphically of a vertical or horizontal line 10 or 20 cm long and at the two ends of which (often indicated with dots) correspond two "pictures or verbal descriptors", one depicting the maximum intensity of dyspnea sensation and the other the absence of perception.
Figure 2.
Visual Analogue Scale (VAS). From [44], mod.
The choice of verbal descriptors at the two extremes must take into account the semantic value that these terms may have for the individual and the terms thus must be carefully evaluated: e.g. the term "unbearable" to describe the maximum sensation of dyspnea could be understood by the patient as more absolute than the term "maximum".
In quantifying dyspnea, the patient is asked to indicate on the VAS the point which corresponds to his/her own perception, evaluated as the distance from the zero extreme (non dyspnea) and expressed as a percentage of the total length of the line. The VAS is thus an instrument of an analogical type since the line on which patients mark their reference point corresponds to the "continuum of dyspnea perception".
The VAS is economic and easy to use, but the mental operation required of the subject is certainly complex and calls for a good capacity for abstract thinking, difficult to achieve at extremes of age. It is thus of little value applied in children and very elderly subjects.
Like the Borg scale, the VAS - with a well established validity and reliability [1] - is a scale commonly used in rehabilitation, especially to measure dyspnea in response to physical exercise [1]. It is thus used in numerous studies [24,40,45] as a subjective outcome marker: its value decreases by approximately 20% compared to baseline in the cardiopulmonary exercise test, [40,45] while it decreases by 12% in the 6MWT [24].
In emphysema patients undergoing lung reduction surgery [42] VAS evaluation of dyspnea at iso-workload during CPX has shown a notable reduction of the individual's perception of the symptom (on average from 79.6 to 49.3, with 30.3% variation). In general, even if few studies have considered the VAS from the point of view of the MCID as a post-exercise index of rehabilitation outcome, a minimum variation of 10% is considered indicative of clinical improvement [43].
Dyspnea Measurement in Daily Living Activities
Dyspnea and muscle fatigue, common symptoms in respiratory disease patients, often cause interference with many occupational activities and in the disease progression can limit the individual's participation in social and/or recreational activities. In more advanced phases of the disease, in fact, respiratory patients are not infrequently impaired also in their ability to perform autonomously personal and domestic tasks defined as activities of daily living (ADL).
When "basic activities of daily living" (BADL) are impaired, the patient needs others to help them fulfill their own personal primary care functions: in severe cases, support is necessary also for elementary functions such as eating, washing, dressing or moving about inside the house. Since promoting the patient's autonomy in carrying out ADLs is a primary goal of PR, the measurement of dyspnea as a symptom during these very activities is an aspect that should not be overlooked [46].
A "centralized" assessment of the needs and motivations of the individual will thus require both "subjective" analysis (by means of interview or questionnaire) and "objective" analysis (validated measurement scales capable of precisely assessing the functional status and the individual's living environment).
Subjective elements of evaluation
Self-evaluation questionnaires enter into this category. They give qualitative information about how the individual perceives their own capacity to cope with their personal care and domestic care requirements, as well as their need for physical and recreational activities.
There exist, however, few valid instruments capable of measuring in a simple manner the perception that patients have concerning the effects that their dyspnea and muscle fatigue have on ADL. Among the most important are the London Chest Activity of Daily Living Scale (LCADL) [47], the Pulmonary Functional Status and Dyspnea Questionnaire (PFSDQ) [48] and the Oxygen Cost Diagram (OCD) [49].
The LCADL [47] is a standardized scale, easy to administer and specific for patients with severe COPD. The primary goal of this scale is to offer a measurement of the patient's ability to carry out ADLs through an estimation of the level of perceived dyspnea during performance of the investigated activities. The theory on which the instrument is based is that dyspnea, during the common daily life activities of the patient, induces a condition of significant limitation in the individual's functional capacity and social participation.
The scale investigates the level of disability induced by dyspnea associated to 15 common activities, subdivided into 4 areas (personal care, domestic activities, physical and social activities) that are mostly carried out on a daily basis in the home: recent studies have in fact shown that the LCADL is a reliable tool for evaluating dyspnea during ADLs [47,50]. Excluding the part related to domestic activities, the LCADL has been shown to be useful in identifying changes in lifestyle (also at follow up) in patients admitted to a rehabilitation program [51].
The PFSDQ [48] is a self-completed questionnaire consisting of 164 questions investigating the individual's functional status and level of dyspnea during the performance of activities. It is subdivided into 6 categories: personal care, mobility, home management, nutrition, recreational activities and social activities. Despite the fact it was designed specifically for use in patients with respiratory diseases, it is not very widely used, perhaps because many of the questions present are not applicable to patients with severe disease. Hence, in patients with very severe COPD a modified, abridged version (40 questions only, taking 7 minutes to complete) has been developed and it has shown an excellent validity, reliability and ease of use [52].
The Oxygen Cost Diagram (OCD) [49] is, on the other hand, a self-evaluation tool designed to provide an estimate of physical exercise limitation. Conceptually similar to the VAS, the OCD is designed as a vertical linear scale 10 cm long with common ADLs listed on both sides: at the bottom end of the list are activities with a small oxygen demand (sleep); as one climbs the list, physical activities make a progressively growing energy demand culminating, at the upper end of the scale, in "walking fast uphill". Patients are invited to indicate with a line the point corresponding to the physical task that provokes in them a sensation of dyspnea such as to require the suspension of the activity. The administration of the OCD is very rapid (takes about 1-2 minutes), and in patients with COPD the OCD has been found able to distinguish different levels of disease severity [53]. However, longitudinal studies testing the instrument's sensitivity with respect to variations in physical condition have shown a poor capacity of this scale to detect both improvement and decline post-rehabilitation [54,55].
Objective elements of evaluation
Objective instruments useful both in individual measurement and in monitoring basic functional capacity during the performance of multiple ADLs are the BDI/TDI [25] and the Borg scale [37], both, as described above, widely validated and currently adopted to assess patients affected by chronic respiratory diseases. The level of physical activity necessary to provoke the sensation of dyspnea is, on the other hand, the goal of the MRC [22].
As a stimulus to detect dyspnea in ADLs, one may consider the test of simulation of 4 common ADLs performed by the upper limbs (putting plates back on a shelf after washing; simulating window cleaning on a blackboard; putting groceries in the cupboard; changing a light bulb) [56]; this test has already been reproduced [51] and validated in COPD patients showing a good correlation with ventilatory and metabolic responses to conventional exercise tests [56].
Conclusions
Dyspnea is a very common and frequent symptom in chronic respiratory diseases, reported by patients through specific descriptors and clusters. From the point of view of an objective estimate of this symptom, it is fundamental to have instruments and measurement scales that are able to characterize at baseline patients with different levels of respiratory disability (MRC, BDI) and observe the evolution in time (TDI, LCADL).
In patients undergoing rehabilitation these instruments can moreover perform the function of outcome markers (Borg scale and VAS, in particular). Use of the MCID as an instrument for orienting the significance of the outcome, even if specific to the measurement scale used, does not yet seem systemically reliable as a method to evalutate changes in dyspnea in this clinical setting, in particular on account of the limited number of studies and data available. In our opinion future studies need to focus on this precise issue.
Conflict of Interest Statement
The authors have no conflict of interest to declare in relation to the subject of this manuscript.
References
- American Thoracic Society. Dyspnea. Mechanisms, assessment, and management: a consensus statement. Am J Respir Crit Care Med. 1999;159:321–340. doi: 10.1164/ajrccm.159.1.ats898. [DOI] [PubMed] [Google Scholar]
- Nici L, Donner C, Wouters E, Zuwallack R, Ambrosino N, Bourbeau J, Carone M, Celli B, Engelen M, Fahy B, Garvey C, Goldstein R, Gosselink R, Lareau S, MacIntyre N, Maltais F, Morgan M, O'Donnell D, Prefault C, Reardon J, Rochester C, Schols A, Singh S, Troosters T. ATS/ERS Pulmonary Rehabilitation Writing Committee. American Thoracic Society/European Respiratory Society Statement on Pulmonary Rehabilitation. Am J Respir Crit Care Med. 2006;173:1390–1413. doi: 10.1164/rccm.200508-1211ST. [DOI] [PubMed] [Google Scholar]
- Jones PW, Wilson RC. In: Respiratory sensations. Adams L, Guz A, editor. New York: Marcel Dekker; 1996. Cognitive aspects of breathlessness; pp. 311–339. [Google Scholar]
- Simon PM, Schwartzstein RM, Weiss JW, Fencl V, Teghtsoonian M, Weinberger SE. Distinguishable types of dyspnea in patients with shortness of breath. Am Rev Respir Dis. 1990;142:1009–1014. doi: 10.1164/ajrccm/142.5.1009. [DOI] [PubMed] [Google Scholar]
- Elliott MW, Adams L, Cockcroft A, Macrae KD, Murphy K, Guz A. The language of breathlessness. Use of verbal descriptors by patients with cardiopulmonary disease. Am Rev Respir Dis. 1991;144:826–832. doi: 10.1164/ajrccm/144.4.826. [DOI] [PubMed] [Google Scholar]
- Mahler DA, Harver A, Lentine T, Scott JA, Beck K, Schwartzstein RM. Descriptors of breathlessness in cardiorespiratory diseases. Am J Respir Crit Care Med. 1996;154:1357–1363. doi: 10.1164/ajrccm.154.5.8912748. [DOI] [PubMed] [Google Scholar]
- Williams M, Cafarella P, Olds T, Petkov J, Frith P. The language of breathlessness differentiates between patients with COPD and age-matched adults. Chest. 2008;134:489–496. doi: 10.1378/chest.07-2916. [DOI] [PubMed] [Google Scholar]
- Paintal AS. Vagal sensory receptors and their reflex effects. Physiol Rev. 1973;53:159–227. doi: 10.1152/physrev.1973.53.1.159. [DOI] [PubMed] [Google Scholar]
- Taguchi O, Kikuchi Y, Hida W, Iwase N, Satoh M, Chonan T, Takishima T. Effects of bronchoconstriction and external resistive loading on the sensation of dyspnea. J Appl Physiol. 1991;71:2183–2190. doi: 10.1152/jappl.1991.71.6.2183. [DOI] [PubMed] [Google Scholar]
- Mc Closkey DI. In: The nervous system. Handbook of physiology. Brookhart JM, Mouncastle VB, editor. Vol. 2. Bethesda: American Physiological Society; 1981. Corollary discharges: motor commands and perception; pp. 1415–1447. [Google Scholar]
- Killian KJ, Campbell EJ. In: The Thorax, Part B. Roussos C, editor. New York: Marcel Dekker; 1995. Dyspnea; pp. 1709–1747. [Google Scholar]
- O'Donnell DE, Revill SM, Webb KA. Dynamic hyperinflation and exercise intolerance in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;164:770–777. doi: 10.1164/ajrccm.164.5.2012122. [DOI] [PubMed] [Google Scholar]
- O'Donnell DE, Bertley JC, Chau LK, Webb KA. Qualitative aspects of exertional breathlessness in chronic airflow limitation: pathophysiologic mechanisms. Am J Respir Crit Care Med. 1997;155:109–115. doi: 10.1164/ajrccm.155.1.9001298. [DOI] [PubMed] [Google Scholar]
- O'Donnell DE, Chau LK, Webb KA. Qualitative aspects of exertional dyspnea in patients with interstitial lung disease. J Appl Physiol. 1998;84:2000–2009. doi: 10.1152/jappl.1998.84.6.2000. [DOI] [PubMed] [Google Scholar]
- O'Donnell DE, Webb KA. Exertional breathlessness in patients with chronic airflow limitation. The role of lung hyperinflation. Am Rev Respir Dis. 1993;148:1351–1357. doi: 10.1164/ajrccm/148.5.1351. [DOI] [PubMed] [Google Scholar]
- Scano G, Stendardi L, Grazzini M. Understanding dyspnoea by its language. Eur Respir J. 2005;25:380–385. doi: 10.1183/09031936.05.00059404. [DOI] [PubMed] [Google Scholar]
- Banzett RB, Lansing RW, Reid MB, Adams L, Brown R. "Air hunger" arising from increased PCO2 in mechanically ventilated quadriplegics. Respir Physiol. 1989;76:53–67. doi: 10.1016/0034-5687(89)90017-0. [DOI] [PubMed] [Google Scholar]
- Chida M, Inase N, Ichioka M, Miyazato I, Marumo F. Ratings of perceived exertion in chronic obstructive pulmonary disease: a possible indicator for exercise training in patients with this disease. Eur J Appl Physiol Occup Physiol. 1991;62:390–393. doi: 10.1007/BF00626608. [DOI] [PubMed] [Google Scholar]
- Mahler DA, Ward J, Mejia-Alfaro R. Stability of dyspnea ratings after exercise training in patients with COPD. Med Sci Sports Exerc. 2003;35:1083–1087. doi: 10.1249/01.MSS.0000074456.10983.CF. [DOI] [PubMed] [Google Scholar]
- Mahler DA, Harver A. A factor analysis of dyspnea ratings, respiratory muscle strength, and lung function in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1992;145:467–470. doi: 10.1164/ajrccm/145.2_Pt_1.467. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Fletcher CM, Elmes PC, Fairbairn AS, Wood CH. The significance of respiratory symptoms and the diagnosis of chronic bronchitis in a working population. Br Med J. 1959;2:257–266. doi: 10.1136/bmj.2.5147.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54:581–586. doi: 10.1136/thx.54.7.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Torres JP, Pinto-Plata V, Ingenito E, Bagley P, Gray A, Berger R, Celli B. Power of outcome measurements to detect clinically significant changes in pulmonary rehabilitation of patients with COPD. Chest. 2002;121:1092–1098. doi: 10.1378/chest.121.4.1092. [DOI] [PubMed] [Google Scholar]
- Mahler DA, Weinberg DH, Wells CK, Feinstein AR. The measurement of dyspnea. Contents, interobserver agreement, and physiologic correlates of two new clinical indexes. Chest. 1984;85:751–758. doi: 10.1378/chest.85.6.751. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Berman LB, Townsend M, Pugsley SO, Chambers LW. A measure of quality of life for clinical trials in chronic lung disease. Thorax. 1987;42:773–778. doi: 10.1136/thx.42.10.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahler DA, Ward J, Fierro-Carrion G, Waterman L, Lentine TF, Mejia-Alfaro R, Baird JC. Development of self-administered versions of modified baseline and transition dyspnea indexes in COPD. COPD. 2004;1:165–172. doi: 10.1081/COPD-120030829. [DOI] [PubMed] [Google Scholar]
- Mahler DA, Wells CK. Evaluation of clinical methods for rating dyspnea. Chest. 1988;93:580–586. doi: 10.1378/chest.93.3.580. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Thompson PJ, Berman LB, Sullivan MJ, Townsend M, Jones NL, Pugsley SO. How should we measure function in patients with chronic heart and lung disease? J Chronic Dis. 1985;38:517–524. doi: 10.1016/0021-9681(85)90035-9. [DOI] [PubMed] [Google Scholar]
- Brusasco V, Hodder R, Miravitlles M, Korducki L, Towse L, Kesten S. Health outcomes following treatment for six months with once daily tiotropium compared with twice daily salmeterol in patients with COPD. Thorax. 2003;58:399–404. doi: 10.1136/thorax.58.5.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahler DA, Tomlinson D, Olmstead EM, Tosteson AN, O'Connor GT. Changes in dyspnea, health status, and lung function in chronic airway disease. Am J Respir Crit Care Med. 1995;151:61–65. doi: 10.1164/ajrccm.151.1.7812573. [DOI] [PubMed] [Google Scholar]
- Witek TJ Jr, Mahler DA. Minimal important difference of the transition dyspnoea index in a multinational clinical trial. Eur Respir J. 2003;21:267–272. doi: 10.1183/09031936.03.00068503a. [DOI] [PubMed] [Google Scholar]
- Mahler DA, Witek TJ Jr. The MCID of the transition dyspnea index is a total score of one unit. COPD. 2005;2:99–103. doi: 10.1081/COPD-200050666. [DOI] [PubMed] [Google Scholar]
- Stevens SS. On the psychophysical law. Psychol Rev. 1957;64:153–181. doi: 10.1037/h0046162. [DOI] [PubMed] [Google Scholar]
- Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med. 1970;2:92–98. [PubMed] [Google Scholar]
- Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–381. [PubMed] [Google Scholar]
- Mahler DA, Horowitz MB. Perception of breathlessness during exercise in patients with respiratory disease. Med Sci Sports Exerc. 1994;26:1078–1081. [PubMed] [Google Scholar]
- Mador MJ, Rodis A, Magalang UJ. Reproducibility of Borg scale measurements of dyspnea during exercise in patients with COPD. Chest. 1995;107:1590–1597. doi: 10.1378/chest.107.6.1590. [DOI] [PubMed] [Google Scholar]
- Stulbarg MS, Carrieri-Kohlman V, Demir-Deviren S, Nguyen HQ, Adams L, Tsang AH, Duda J, Gold WM, Paul S. Exercise training improves outcomes of a dyspnea self-management program. J Cardiopulm Rehab. 2002;22:109–121. doi: 10.1097/00008483-200203000-00010. [DOI] [PubMed] [Google Scholar]
- Foglio K, Bianchi L, Bruletti G, Battista L, Pagani M, Ambrosino N. Long-term effectiveness of pulmonary rehabilitation in patients with chronic airway obstruction. Eur Respir J. 1999;13:125–132. doi: 10.1183/09031936.99.13112599. [DOI] [PubMed] [Google Scholar]
- Eaton T, Garrett JE, Young P, Fergusson W, Kolbe J, Rudkin S, Whyte K. Ambulatory oxygen improves quality of life of COPD patients: a randomised controlled study. Eur Respir J. 2002;20:306–312. doi: 10.1183/09031936.02.00301002. [DOI] [PubMed] [Google Scholar]
- Martinez FJ, de Oca MM, Whyte RI, Stetz J, Gay SE, Celli BR. Lung-volume reduction improves dyspnea, dynamic hyperinflation, and respiratory muscle function. Am J Respir Crit Care Med. 1997;155:1984–1990. doi: 10.1164/ajrccm.155.6.9196106. [DOI] [PubMed] [Google Scholar]
- Ries AL. Minimally clinically important difference for the UCSD Shortness of Breath Questionnaire, Borg Scale, and Visual Analog Scale. COPD. 2005;2:105–110. doi: 10.1081/COPD-200050655. [DOI] [PubMed] [Google Scholar]
- Aitken RC. Measurement of feelings using visual analogue scales. Proc R Soc Med. 1969;62:989–993. doi: 10.1177/003591576906201005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon J, Awad E, Normandin E, Vale F, Clark B, ZuWallack RL. The effect of comprehensive outpatient pulmonary rehabilitation on dyspnea. Chest. 1994;105:1046–1052. doi: 10.1378/chest.105.4.1046. [DOI] [PubMed] [Google Scholar]
- Horne D, Corsello P. Physical and occupational therapy for patients with chronic lung disease. Semin Respir Med. 1993;14:466–481. doi: 10.1055/s-2007-1006342. [DOI] [Google Scholar]
- Garrod R, Bestall JC, Paul EA, Wedzicha JA, Jones PW. Development and validation of a standardized measure of activity of daily living in patients with severe COPD: the London Chest Activity of Daily Living scale (LCADL) Respir Med. 2000;94:589–596. doi: 10.1053/rmed.2000.0786. [DOI] [PubMed] [Google Scholar]
- Lareau SC, Carrieri-Kohlman V, Janson-Bjerklie S, Roos PJ. Development and testing of the Pulmonary Functional Status and Dyspnea Questionnaire (PFSDQ) Heart Lung. 1994;23:242–250. [PubMed] [Google Scholar]
- McGavin CR, Artvinli M, Naoe H, McHardy GJ. Dyspnoea, disability, and distance walked: comparison of estimates of exercise performance in respiratory disease. Br Med J. 1978;2:241–243. doi: 10.1136/bmj.2.6132.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrod R, Paul EA, Wedzicha JA. An evaluation of the reliability and sensitivity of the London Chest Activity of Daily Living Scale (LCADL) Respir Med. 2002;96:725–730. doi: 10.1053/rmed.2002.1338. [DOI] [PubMed] [Google Scholar]
- Costi S, Crisafulli E, Antoni FD, Beneventi C, Fabbri LM, Clini EM. Effects of unsupported upper extremity exercise training in patients with COPD: a randomized clinical trial. Chest. 2009;136:387–395. doi: 10.1378/chest.09-0165. [DOI] [PubMed] [Google Scholar]
- Lareau SC, Meek PM, Roos PJ. Development and testing of the modified version of the pulmonary functional status and dyspnea questionnaire (PFSDQ-M) Heart Lung. 1998;27:159–168. doi: 10.1016/S0147-9563(98)90003-6. [DOI] [PubMed] [Google Scholar]
- O'Brien B, Viramontes JL. Willingness to pay: a valid and reliable measure of health state preference? Med Decis Making. 1994;14:289–297. doi: 10.1177/0272989X9401400311. [DOI] [PubMed] [Google Scholar]
- Janssens JP, Breitenstein E, Rochat T, Fitting JW. Does the 'oxygen cost diagram' reflect changes in six minute walking distance in follow up studies? Respir Med. 1999;93:810–815. doi: 10.1016/S0954-6111(99)90266-4. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, King DR, Feeny DH, Stubbing D, Goldstein RS. Generic and specific measurement of health-related quality of life in a clinical trial of respiratory rehabilitation. J Clin Epidemiol. 1999;52:187–192. doi: 10.1016/S0895-4356(98)00157-7. [DOI] [PubMed] [Google Scholar]
- Velloso M, Stella SG, Cendon S, Silva AC, Jardim JR. Metabolic and ventilatory parameters of four activities of daily living accomplished with arms in COPD patients. Chest. 2003;123:1047–1053. doi: 10.1378/chest.123.4.1047. [DOI] [PubMed] [Google Scholar]


