Abstract
Lymphangioleiomyomatosis (LAM) is a rare lung disease affecting almost exclusively young women, characterised by abnormal proliferation of atypical smooth muscle cells. We describe a young woman presenting with chyluria secondary to the presence of a large retroperitoneal lymphangioleiomyoma. Immunohistochemical analysis revealed HMB45-negative LAM cells (HMB45 staining is absent only in rare cases) expressing low levels of estrogen receptors. Estrogen suppressive treatment with triptoreline, a synthetic analogue of Gn-RH, resulted in dramatic reduction of the retroperitoneal mass size. The role of estrogens in the pathogenesis of LAM remains poorly understood, and hormonal therapy is still debated, but this case suggests that at least in some LAM patients, possibly those with HMB45-negative disease and estrogen receptor expression, hormonal therapy may be effective in controlling the disease process.
Keywords: Chyluria, lymphangioleiomyoma, lymphangioleiomyomatosis, triptoreline
Lymphangioleiomyomatosis (LAM) is a rare, progressive, frequently fatal lung disease. It affects almost exclusively pre-menopausal women and is exacerbated by pregnancy and exogenous estrogens, thus suggesting a role for estrogens in its etiology and pathology. LAM is predominantly sporadic, owing to somatic mutations in tuberous sclerosis genes, but it may also manifest in the context of tuberous sclerosis complex (TSC), an autosomal dominant disorder of highly variable penetrance [1,2]. The pathologic hallmark of LAM is the abnormal and potentially metastatic growth of atypical smooth muscle (SM)-like cells (LAM cells) within the lungs and axial lymphatics. LAM cells typically express the melanoma-related antigen HMB-45 [3].
In the lung, the typical lesions are thin-walled parenchymal cysts, which cause destruction of the interstitium and progressive air-flow obstruction [4]. In addition to the lung cysts, LAM is also characterized by renal or abdominal angiomyolipomas, perivascular tumors consisting of a mixture of LAM cells, fat cells and blood vessels [5]. A recent report including both patients with TSC and sporadic LAM showed that sirolimus monotherapy reduced angiomyolipoma volume by nearly 50%. Conversely, improvements in airflow and gas trapping were limited to patients with LAM [6]. However, the rate of adverse effects was high, and only a small number of patients had renal and pulmonary benefits that persisted after the drug was stopped. Another recent report [7] shows that treatment with sirolimus for 1 year has beneficial effects in patients with LAM, including the stabilization of forced expiratory volume in 1 second (FEV1) and improvement in forced vital capacity (FVC), quality of life, and some func-tional performance measures. But sirolimus therapy positively affected lung function only during the treatment period and it was associated with a large number of different adverse events.
Despite these somewhat promising results, and despite the recently reported effect of hormonal manipulation [8], effective treatment for patients with LAM is still lacking.
Case report
We describe a 42-year old Italian pre-menopausal woman, current smoker. She reported the use of hormonal therapy as a contraceptive measure, discontinued 2 years before presenting at our hospital, with irrelevant familiar and past medical history, apart from a voluntary abortion at age 25. No history of tuberous sclerosis was present. In July 2006 she reported an acute flu-like syndrome with fever and diffuse abdominal pain, relieved by paracetamol administration. One month later, chyluria associated to mild left flank pain appeared, in the absence of urinary symptoms; echographic examination of the abdomen revealed a tubular mass with a maximum diameter of 2 cm, as well as pseudocystic lesions around the right ureter with mild left hydronephrosis. A computerized tomography (CT) scan confirmed the presence of a large retroperitoneal mass, initially interpreted as conglomerated lymph nodes, dislocating both ureters, the lower tract of the vena cava and the abdominal tract of the aorta (Figure 1, panel A). In the left kidney a 1.4 cm renal cyst was identified, while the uterus was enlarged by an endoluminal 2 cm nodule (later diagnosed as a myoma by transvaginal echography). Radiographic examination of the urinary tract by urography confirmed that the left ureter was compressed and dislocated by the neoformation. During a cystoscopic examination, white, milk-like urine from the left ureteral ostium was identified and a permanent left ureteral stent was inserted. In October 2006 the patient was admitted to the Oncology department, where a laparoscopy and biopsy of the retroperitoneal tissue were performed. Histologic examination revealed nodular infiltration by SM cells: immunohistochemical analysis showed that these muscle cells stained positive with antibodies specific for desmin (clone D240) and α-actin (clone HHF35), while they were negative for anti-CD34 (clone QBEND10), S100 protein (polyclonal), melanoma-associated antigen (clones HMB-45 and MART-1) and cytokeratin (clones MNF116, 35βH11 and 34βE12) antibodies. Staining for α and β estrogen receptors (ERs) was almost completely negative. A brain MRI was normal. Chest examination was normal as were arterial blood gases. Body plethysmography was within normal values (FEV1 3.2 L, 116% predicted; FVC 3.9 L, 121% predicted; total lung capacity [TLC] 6.3 L, 127% predicted; residual volume [RV] 1.7 L, 102% predicted), whereas carbon monoxide diffusion was slightly reduced (DLCO 77% predicted). Chest high-resolution computed tomography (HRCT) showed thin-walled cysts with an average diameter of 5 mm, diffused to both upper lobes (Figure 2); the thoracic duct was moderately enlarged. Trans-bronchial biopsies were obtained and revealed the presence of aggregates of LAM cells with the same phenotypic pattern detected at retroperitoneal biopsy, i.e. HMB-45-negative LAM cells. ERs-β were expressed at low levels in the lung specimens only.
Figure 1.
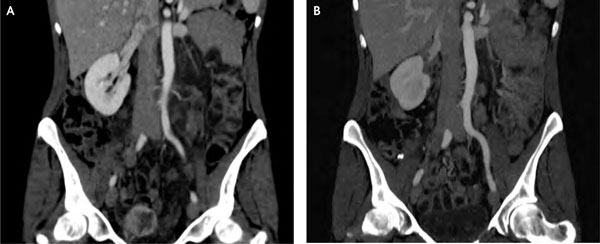
Multi-slice Spiral Computed Tomography (CT), Coronal Reformatted Image Showing a Retroperitoneal Mass Located in Close Proximity to the Thoracic Duct Before (Panel a) and After (Panel b) Treatment With Triptoreline.
Figure 2.
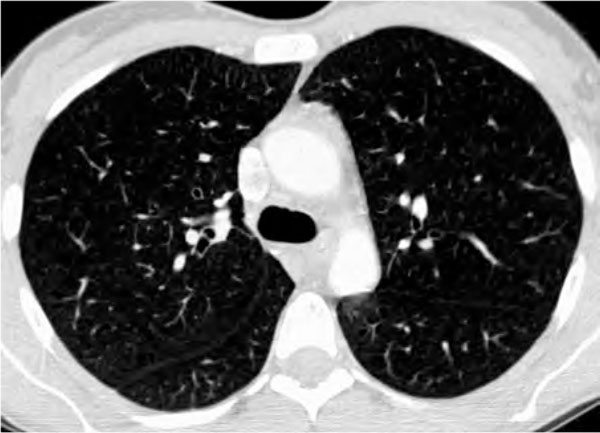
High Resolution Computed Tomography of the Lung Showing 5 to 7 mm Bilateral Cysts.
Based on these findings a diagnosis of pulmonary and extrapulmonary LAM was established. In December 2006 treatment with triptoreline, a synthetic analogue of Gn-RH (at the dose of 3.75 mg every 4 weeks), was started; subsequent blood hormone dosages confirmed the induction of iatrogenic menopause. Seven months later, a CT scan revealed that the size of the retroperitoneal lymph angioleiomyoma was reduced by approximately 80% (Figure 1, panel B); the caliber of the thoracic duct was also reduced, while lung cysts were unchanged. During this period the patient presented a mild, self-limiting chyluria on two occasions. Therefore, she underwent a retrograde bilateral ureteropyelography revealing a normal left urinary tract and absence of hydronephrosis, whereas, on the right side, extensive and dilated fistulous connections between the urinary tract and retroperitoneal lymphatics were present (Figure 3); the ureter stent was removed. In December 2007 the patient was clinically re-evaluated and was still asymptomatic; at that time, 18 months after initial presentation, lung function was basically unchanged (FEV1 3.1 L, FVC 3.9 L, TLC 5.28 L, RV 1.32 L). Chyluria was absent and triptoreline treatment was continued.
Figure 3.
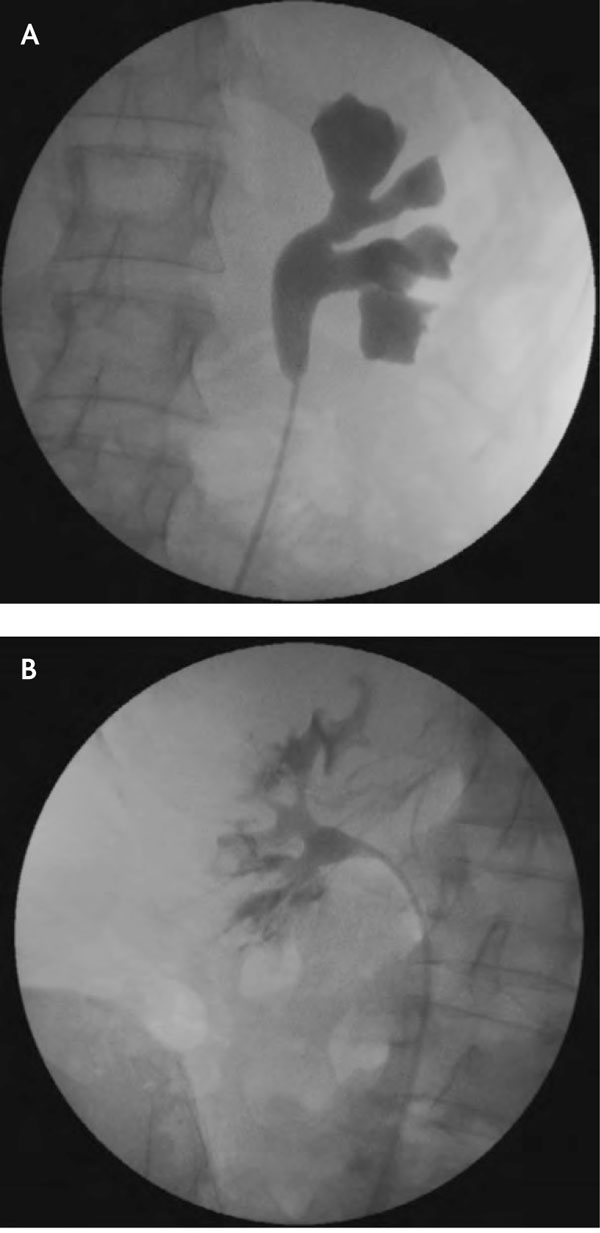
Retrograde Bilateral Ureteropyelography. Right upper urinary tract showing extensive fistulous connections between urinary system and retroperitoneal lymphatics (panel a) and normally shaped left urinary tract (panel b).
Discussion
Estrogens have been implicated in the pathogenesis of LAM based on a number of convincing signs of evidence, including the identification of estrogen receptors (ERs) in the context of LAM cells [9-11], and the occurrence of the disease primarily in women of childbearing age. However, hormonal modulation (using a number of different approaches) has failed to provide consistent, reproducible proof of efficacy [4,8,12,13]. In this regard, a recent report suggested limited efficacy of triptoreline therapy [14]. However, in this study on 11 patients (9 of which had pathologic confirmation of their disease) no data were reported concerning the expression of estrogen receptors and HMB-45, and it is unknown whether these 9 patients represented cases of LAM in which LAMD-SM cells played a role. Importantly, ER expression has been documented in HMB-45positive, but not in HMB-45-negative LAM cells [9], although these data have not been confirmed.
LAM is rare so there have been no controlled trials of its management. Effective treatment for patients with LAM is still lacking and European Respiratory Society (ERS) guidelines for LAM do not have conclusive indications about effective therapeutic strategies [15].
Another recent report [7] shows that treatment with sirolimus for 1 year has beneficial effects in patients with LAM, including the stabilization of FEV1 and improvement in FVC, quality of life, and some functional performance measures. But sirolimus therapy positively affected lung function only during the treatment period and it was associated with a large number of different adverse events.
Here we report the identification of LAM cells negative for HMB-45 and expressing very low levels of ERs in a young woman with a retroperitoneal mass and lung cysts. The LAM cells found in our patient closely resemble the spindle-shaped (LAMD-SM) cells. Both in the lung specimens and in the retroperitoneal mass ER levels were almost undetectable. Similarly, Glassberg and colleagues reported that the amounts of ER-α and ER-β protein were lower in LAM tissue and LAMD-SM cell lines compared to control lung tissue and cell lines [11]. In this regard, it has been demonstrated that unbound ERs undergo a rapid proteosome degradation in LAMD-SM cells [16,17]. However, despite very low ER protein levels, LAMD-SM are more responsive to estrogens compared to control cells. This is not surprising, because estrogen sensitivity and responsiveness only partially depend on the levels of functional ERs [18]. In turn, the estrogen-ER interaction drives matrix metalloproteinase (MMP)-2 and -9 synthesis and activation in LAMD-SM, thus leading to tissue invasion and destruction [11]. HMB-45negative spindle cells have been shown to possess a high proliferating-cell nuclear antigen expression and have been implicated in the progression of LAM [19]. The HMB-45-negative LAM cell occurrence is rare and we hypothesize that HMB-45negative LAM may represent a distinct disease phenotype, more aggressive but highly responsive to hormonal therapy. In the case reported here, the pharmacologic suppression of estrogen levels rapidly reduced the size of a large retroperitoneal mass, with consequent relief of urinary symptoms, and stabilized the extension of the pulmonary cysts. We therefore consider this case as indirect in vivo evidence in support of the so-called "estrogen hypothesis" in LAM. The fact that pregnancy and use of oral contraceptives are associated with a higher frequency of exacerbations and a more aggressive disease course, along with reports of LAM in postmenopausal women taking hormone replacement, reinforce this theory [20-22]. The patient described here displayed other peculiar features meriting further discussion. Chyluria was the presenting symptom and we hypothesize that the presence of a fistulous connection between the urinary system and the retroperitoneal lymphatic system might have been responsible for this unusual presentation of LAM. Interestingly, chyluria completely disappeared after hormonal treatment, due to the dramatic reduction in size of the retroperitoneal mass. In this patient the early occurrence of such an atypical urinary presentation prompted adequate treatment that might have been able to stop disease progression at a time when pulmonary function was only mildly impaired, but after confirmation of LAM cells in the lung tissue. Taken together, these findings underscore the importance of a high diagnostic suspicion of LAM in young women presenting with atypical clinical manifestations.
The role of estrogens in the pathogenesis of LAM remains poorly understood, and hormonal therapy (based on the antagonism of estrogen effects) is empiric and unproven. Nevertheless, our in vivo findings, coupled with recent evidence of limited efficacy of other therapeutic options, strongly suggest that hormonal therapy may still hold promise at least in some LAM patients.
Conflict of interest statement
None of the authors has any conflict of interest to declare in relation to the subject matter of this manuscript.
Acknowledgements
We would like to thank Jan-Åke Gustafsson, Margaret Warner and Paloma Alonso Magdalena (Karolinska Institutet, Stockholm, Sweden) for the ER staining.
References
- Taveira-DaSilva AM, Steagall WK, Moss J. Lymphangioleiomyomatosis. Cancer Control. 2006;13:276–285. doi: 10.1177/107327480601300405. [DOI] [PubMed] [Google Scholar]
- Schiavina M, Contini P, Guerrieri A, Tavalazzi F, Fabiani A. Lymphangioleiomyomatosis: a rare disease. Multidiscip Resp Med. 2009;4:203–207. [Google Scholar]
- Tanaka H, Imada A, Morikawa T, Shibusa T, Satoh M, Sekine K, Abe S. Diagnosis of pulmonary lymphangioleiomyomatosis by HMB45 in surgically treated spontaneous pneumothorax. Eur Respir J. 1995;8:1879–1882. doi: 10.1183/09031936.95.08111879. [DOI] [PubMed] [Google Scholar]
- Johnson SR. Lymphangioleiomyomatosis. Eur Respir J. 2006;27:1056–1065. doi: 10.1183/09031936.06.00113303. [DOI] [PubMed] [Google Scholar]
- Krymskaya VP. Smooth muscle-like cells in pulmonary lymphangioleiomyomatosis. Proc Am Thorac Soc. 2008;5:119–126. doi: 10.1513/pats.200705-061VS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bissler JJ, McCormack FX, Young LR, Elwing JM, Chuck G, Leonard JM, Schmithorst VJ, Laor T, Brody AS, Bean J, Salisbury S, Franz DN. Sirolimus for angiomyolipoma in tuberous sclerosis complex or lymphangioleiomyomatosis. N Engl J Med. 2008;358:140–151. doi: 10.1056/NEJMoa063564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack FX, Inoue Y, Moss J, Singer LG, Strange C, Nakata K, Barker AF, Chapman JT, Brantly ML, Stocks JM, Brown KK, Lynch JP, Goldberg HJ, Young LR, Kinder BW, Downey GP, Sullivan EJ, Colby TV, McKay RT, Cohen MM, Korbee L, Taveira-DaSilva AM, Lee HS, Krischer JP, Trapnell BC. National Institutes of Health Rare Lung Diseases Consortium; MILES Trial Group. Efficacy and safety of sirolimus in lymphangioleiomyomatosis. N Engl J Med. 2011;364:1595–1606. doi: 10.1056/NEJMoa1100391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiavina M, Contini P, Fabiani A, Cinelli F, Di Scioscio V, Zompatori M, Campidelli C, Pileri SA. Efficacy of hormonal manipulation in lymphangioleiomyomatosis. A 20-year experience in 36 patients. Sarcoidosis Vasc Diffuse Lung Dis. 2007;24:39–50. doi: 10.1007/s11083-007-9058-0. [DOI] [PubMed] [Google Scholar]
- Matsui K, Takeda K, Yu ZX, Valencia J, Travis WD, Moss J, Ferrans VJ. Downregulation of estrogen and progesterone receptors in the abnormal smooth muscle cells in pulmonary lymphangioleiomyomatosis following therapy. An immunohistochemical study. Am J Respir Crit Care Med. 2000;161(3 Pt 1):1002–1009. doi: 10.1164/ajrccm.161.3.9904009. [DOI] [PubMed] [Google Scholar]
- Berger U, Khaghani A, Pomerance A, Yacoub MH, Coombes RC. Pulmonary lymphangioleiomyomatosis and steroid receptors. An immunocytochemical study. Am J Clin Pathol. 1990;93:609–614. doi: 10.1093/ajcp/93.5.609. [DOI] [PubMed] [Google Scholar]
- Glassberg MK, Elliot SJ, Fritz J, Catanuto P, Potier M, Donahue R, Stetler-Stevenson W, Karl M. Activation of the estrogen receptor contributes to the progression of pulmonary lymphangioleiomyomatosis via matrix metalloproteinase-induced cell invasiveness. J Clin Endocrinol Metab. 2008;93:1625–1633. doi: 10.1210/jc.2007-1283. [DOI] [PubMed] [Google Scholar]
- Tomasian A, Greenberg MS, Rumerman H. Tamoxifen for lymphangioleiomyomatosis. N Engl J Med. 1982;306:745–746. doi: 10.1056/NEJM198203253061215. [DOI] [PubMed] [Google Scholar]
- Glassberg MK. Lymphangioleiomyomatosis. Clin Chest Med. 2004;25:573–82. doi: 10.1016/j.ccm.2004.05.003. vii. [DOI] [PubMed] [Google Scholar]
- Harari S, Cassandro R, Chiodini J, Taveira-DaSilva AM, Moss J. Effect of a gonadotrophin-releasing hormone analogue on lung function in lymphangioleiomyomatosis. Chest. 2008;133:448–454. doi: 10.1378/chest.07-2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SR, Cordier JF, Lazor R, Cottin V, Costabel U, Harari S, Reynaud-Gaubert M, Boehler A, Brauner M, Popper H, Bonetti F, Kingswood C. Review Panel of the ERS LAM Task Force. European Respiratory Society guidelines for the diagnosis and management of lymphangioleiomyomatosis. Eur Respir J. 2010;35:14–26. doi: 10.1183/09031936.00076209. [DOI] [PubMed] [Google Scholar]
- Nawaz Z, Lonard DM, Dennis AP, Smith CL, O'Malley BW. Proteasome-dependent degradation of the human estrogen receptor. Proc Natl Acad Sci USA. 1999;96:1858–1862. doi: 10.1073/pnas.96.5.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrel TA, Brueggemeier RW. Increased proteasome-dependent degradation of estrogen receptor-alpha by TGF-beta1 in breast cancer cell lines. J Cell Biochem. 2003;88:181–190. doi: 10.1002/jcb.10353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb P, Lopez GN, Greene GL, Baxter JD, Kushner PJ. The limits of the cellular capacity to mediate an estrogen response. Mol Endocrinol. 1992;6:157–167. doi: 10.1210/me.6.2.157. [DOI] [PubMed] [Google Scholar]
- Jaiswal VR, Baird J, Fleming J, Miller DS, Sharma S, Molberg K. Localized retroperitoneal lymphangioleiomyomatosis mimicking malignancy. A case report and review of the literature. Arch Pathol Lab Med. 2003;127:879–882. doi: 10.5858/2003-127-879-LRLMM. [DOI] [PubMed] [Google Scholar]
- Ryu JH, Moss J, Beck GI, Lee JC, Brown KK, Chapman JT, Finlay GA, Olson EJ, Ruoss SJ, Maurer JR, Raffin TA, Peavy HH, McCarthy K, Taveira-Dasilva A, McCormack FX, Avila NA, Decastro RM, Jacobs SS, Stylianou M, Fanburg BL. The NHLBI lymphangioleiomyomatosis registry: characteristics of 230 patients at enrollment. Am J Respir Crit Care Med. 2006;173:105–111. doi: 10.1164/rccm.200409-1298OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunelli A, Catalini G, Fianchini A. Pregnancy exacerbating unsuspected mediastinal lymphangioleiomyomatosis and chylothorax. Int J Gynaecol Obstet. 1996;52:289–290. doi: 10.1016/0020-7292(95)02619-3. [DOI] [PubMed] [Google Scholar]
- Yano S. Exacerbation of pulmonary lymphangioleiomyomatosis by exogenous oestrogen used for infertility treatment. Thorax. 2002;57:1085–1086. doi: 10.1136/thorax.57.12.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]


