Abstract
Background:
The objective of our study was to determine the safety and usefulness of performing surgery via occipital transtentorial approach to treat posterior cranial fossa tumors, which is well known as an approach to the pineal region (Poppen's approach).
Methods:
Fourteen patients with posterior cranial fossa tumors were successfully treated using occipital transtentorial approach between 2007 and 2012. The lesions included five meningiomas, three astrocytomas, two metastases, two hemangioblastomas, one cavernoma, and one dysgerminoma.
Results:
Lesions were <3 cm in 12 cases and ≥3 cm in two cases. Average Karnofsky Performance Status (KPS) scoring at admission was 88.5. Eleven patients scored ≥70 and seven patients <70. Average age was 43.1 years. All patients underwent surgical treatment by the same surgical team. All tumors were completely removed surgically without any injury to the venous complex and the adjoining structures. There was no incidence of mortality or morbidity in all patients, and all functional outcomes were good to excellent postoperatively. Postoperative computed tomography (CT) imaging revealed that none of the patients had suffered brain damage or infarction around the cerebellum, brainstem, or occipital lobe.
Conclusions:
We found that the use of occipital transtentorial approach is strongly supported by the successful removal of posterior cranial fossa tumors without serious complications. Open microneurosurgery is probably still the most effective therapy in improving survival and KPS in patients with posterior cranial fossa tumors, given that the proper surgical technique is used and complications do not occur. This case study has strongly suggested that this approach is very useful, safe, and accurate for removing the tumors of posterior fossa and evaluating the surrounding anatomy, as well as for determining operative strategy.
Keywords: Occipital transtentorial approach, Poppen's approach, posterior cranial fossa tumors
INTRODUCTION
The occipital interhemispheric transtentorial approach is commonly used for pineal region lesions and is well known as Poppen's approach. The pineal region contains certain tissues that have distinct histological characteristics, including the pineal gland and several parapineal structures such as the posterior third ventricle and the aqueduct, brain, dura, and vessels.[14] The list of tumors that can arise within the pineal region is extensive and encompasses germ cell tumors, pineal parenchymal cell tumors, gliomas, and meningiomas.[7] Among the prognostic factors, the cerebellar location was never considered, although this results in hydrocephalus, brain stem compression, ataxia, and intracranial hypertension.[18]
Recent reports of surgical interventions in the pineal region for meningiomas are mostly gained from independent studies that describe surgical approaches, such as Poppen's approach, Krause's approach, and combinations of the two approaches. It can be very difficult for the clinicians to choose the most appropriate treatment approach.[14]
Despite recent technological advances in the neurosurgical field, direct surgical approaches to the posterior cranial fossa and avoidance of unexpected complications in the relatively small space remain challenges for neurosurgeons. Occipital approaches offer the advantage of wide exposure, but have the disadvantage of the risk of injury to the normal cerebellar tissue around the tumor bed, thus interfering with good recovery following surgery.[16]
In our work, we have used Poppen's approach for the treatment of posterior cranial fossa tumors.
This study demonstrates that occipital transtentorial approach is clinically feasible for the treatment of posterior cranial fossa tumors and it provides a good prognosis for patients.
MATERIALS AND METHODS
Since 2007, we have treated 14 patients who presented with posterior cranial fossa tumors, using occipital transtentorial approach. The lesions included five meningiomas, three astrocytomas, two metastases, two hemangioblastomas, one cavernoma, and one dysgerminoma.
We used a modified “Concorde” position[6] with the patient's head in neutral position and upper body elevated approximately 15° above the horizontal level. The patient was operated with the need neutral and he was not turned to one side. The degree of head and neck flexion was guided by the angle of the tentorium, which was determined on the basis of sagittal Magnetic Resonance Images (MRI). In this position, the surgeon can move the microscope willingly in all directions and the tumor bed is usually observed just beneath the microscope. The choice of craniotomy was based on the side, location, and shape of the venous sinuses and feeding arteries of the tumor, and provided good orientation for the surgeon and sufficient space for placement of surgically assisted systems. A U-shaped skin incision was created over the confluence and the unilateral transverse sinus.
Generally, three or four burr holes were placed adjacent to the venous sinuses, and a relatively small osteoplastic bone flap was created to expose the edge of the confluence, the lower part of the superior sagittal sinus, and the upper half of the transverse sinus to the operative field. The medial and inferior borders of the operative field were located under the transverse and sagittal sinuses, respectively. A cross dural incision was made [Figure 1]. Attention should be paid not to overextend the lateral boundary while creating the dural incision because the inferior cerebral veins are present beneath the lower portion of the lateral occipital lobe and drain into the tentorial sinus or transverse sinus.
Figure 1.
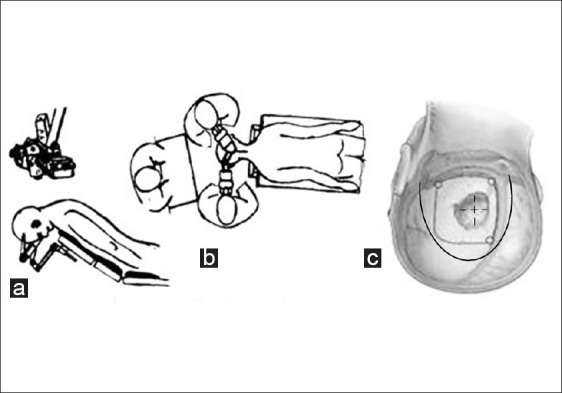
Surgical planning. (a) Concorde position. At (b) disposition of surgeons around the patient. (c) Schematic drawing of the U-shaped skin incision, cranial window, and dural incision
Retraction of the occipital pole rostrally was the most important step in preventing further complications during the approach to the tentorial edge. If the retraction force tends to extend from the lateral to medial direction, there may be a high risk of injury to the bridging veins in some cases.[13] Using a relatively small craniotomy, we usually observed no bridging veins around the occipital pole, but in some patients the internal occipital vein was present near the deep medial portion of the occipital pole. Therefore, care must be taken not to injure these bridging veins. After the occipital pole was retracted further, the boundary of the tentorial notch was visualized [Figure 2].
Figure 2.
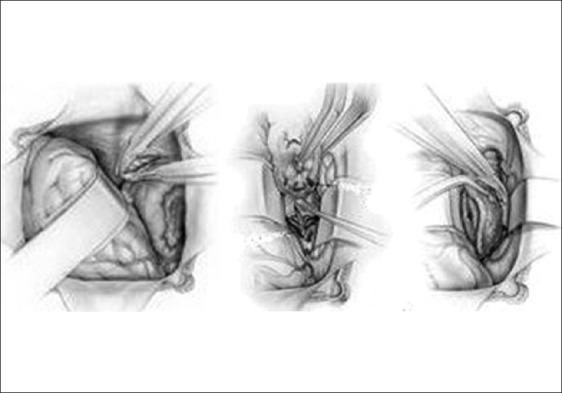
Tentorial notch visualization and incision after occipital pole retraction. Schematic drawing of the tumors’ dissection and removal
Tearing the arachnoid membrane to drain residual cerebrospinal fluid resulted in a wide surgical space. If the microoperative field was still insufficient to allow a tentorial incision, a ventricular catheter was placed into the occipital horn of the lateral ventricle, allowing the occipital pole to be retracted superiorly by a single brain retractor. Following careful observation of the edge of the tentorium, an incision parallel to the straight sinus was made. This tentorial incision was made by creating a small hole apart from the border of the transverse sinus by using a bipolar coagulator, following which a linear incision parallel to the straight sinus was made using a microscissor. The incised tentorium was then tented separately to allow the surface of the anterosuperior cerebellum to come into microsurgical view.
When the aforementioned portion of the examination had been concluded, tumor removal was then performed [Figure 3]. If the tumor was located in the distant anterior cerebellum, sharp incision of the quadrigeminal arachnoid membrane was essential.
Figure 3.
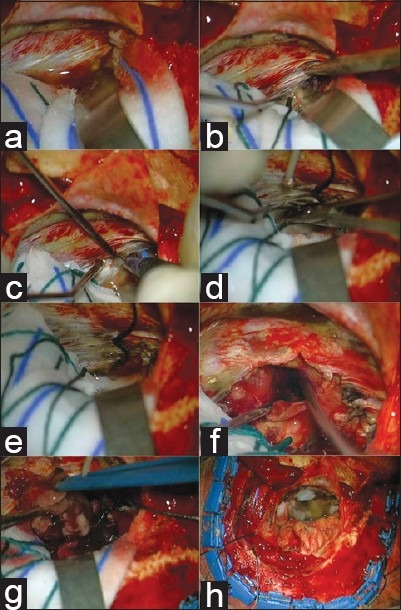
Intraoperative photographs. (a–d) A tentorial incision is made by creating a small hole apart from the border of the transverse sinus with the aid of a monopolar coagulator. (e, f) The incised tentorium is tented separately to allow the surface of the anterosuperior cerebellum to come into microsurgical view. (g, h) The tumor is dissected from the posterior fossa and removed
This procedure improved our field of vision for observation of the basal vein, the vein of Galen, and the precentral cerebellar vein. Histological samples were readily obtained directly from the superficial portion of the tumor. After verifying the pathological characteristics of the tumor, inner decompression was performed using both bipolar coagulation and suction to achieve accurate assessment of ranges of resectability. The ultrasonic aspirator was not always used because it may interfere with surgical procedures within a relatively narrow operative field, resulting in overretraction of the occipital lobe. For large and deep-seated tumors, avoidance of injury to the superior medullary velum, tectum, and posterior medial choroidal artery was necessary. In addition, an endoscope was used to access the remnant of the tumor, its relatively microanatomical structures, and the fourth ventricle.
Postoperatively, ventricular drainage was continued during the first 48 h regardless of whether a shunting operation was performed afterward.
RESULTS
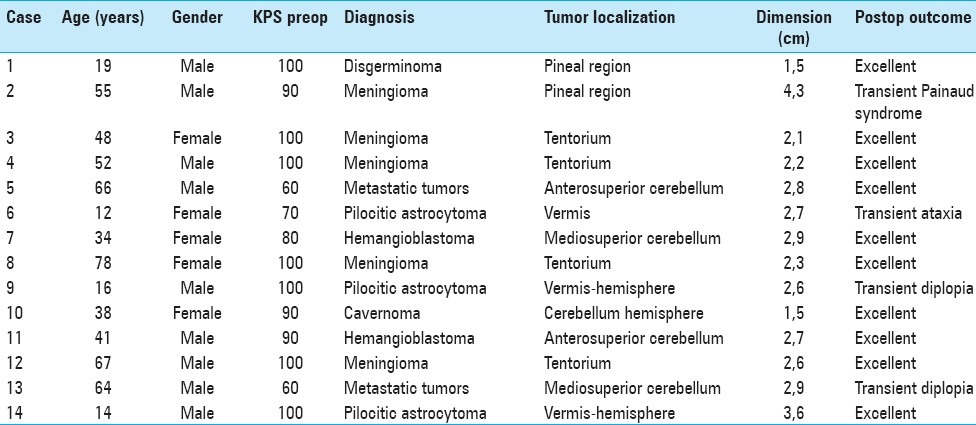
Since 2007, we have successfully used the occipital transtentorial approach for the treatment of posterior cranial fossa tumors in 14 patients (9 males and 5 females). These patients ranged in age from 12 to 78 years. Average age was 43.1 years. Tumor localization was cerebellum in eight cases, tentorium in four cases, and pineal region in two cases. Lesion dimensions were <3 cm in 12 cases and ≥3 cm in 2 cases. Average Karnofsky Performance Status (KPS) scoring at admission was 88.5. Eleven patients scored ≥70 and seven patients <70 [Table 1]. Clinical symptoms were often multiple at presentation and commonly were those caused by increased pressure. Presenting manifestations included headaches (78%), gait disturbances (64%), nausea/vomiting (57%), visual changes (35%), dizziness (28%), and altered mental status (14%). No case of seizures was registered.
Table 1.
Characteristics of 14 patients with posterior cranial fossa tumors who underwent surgery via the occipital transtentorial approach
Using this approach, combined with a neuronavigation system, microsurgeries were performed through relatively small bone windows. All tumors were completely removed surgically without any injury to the venous complex. There was no incidence of mortality or morbidity in our group of patients, and all functional outcomes were good to excellent postoperatively. No sacrifice of bridging veins occurred during any operation [Figures 4 and 5].
Figure 4.
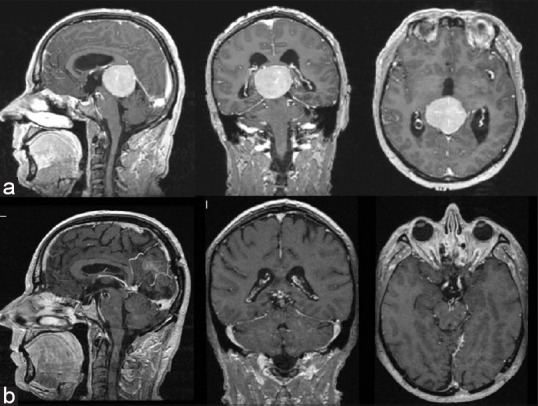
(a) Gadolinium-enhanced T1-weighted MR images obtained in a 55-year-old man (case 2), revealing a large meningioma of pineal region beneath the tentorium and extending to the midbrain. (b) Postoperative MRI after resection via an occipital transtentorial approach
Figure 5.
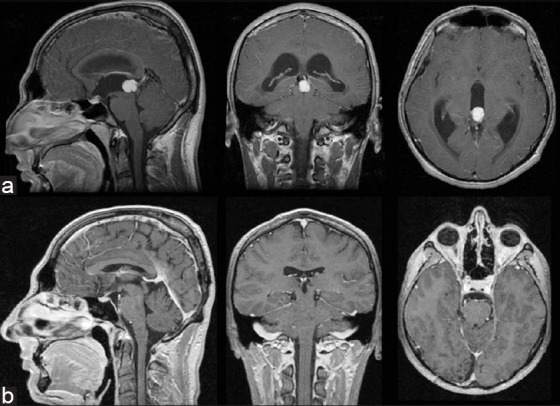
(a) Gadolinium-enhanced T1-weighted MR images obtained in a 19-year-old man (case 1), revealing a dysgerminoma of pineal region extending to the diencephalon. (b) Postoperative MRI after resection via an occipital transtentorial approach
Postoperative CT imaging revealed that none of the patients had suffered brain damage or infarction around the fourth ventricle, cerebellum, brainstem, or occipital lobe [Figure 6].
Figure 6.
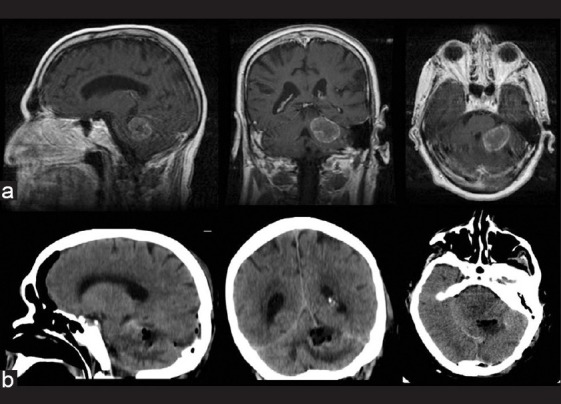
(a) Gadolinium-enhanced T1-weighted MR images obtained in a 64-year-old man (case 13), revealing a metastatic cerebellar tumor. (a) Postoperative CT after tumor resection via an occipital transtentorial approach
None of the patients experienced episodic seizures or hemianopsia postoperatively. Although transient diplopia related to a surgical intervention near the tectum, transient Parinaud syndrome in a pineal region meningioma, and transient ataxia in an anterosuperior cerebellum astrocytoma were observed, recovery was obtained within 2 weeks.
During the follow-up period, no patients exhibited aggravation of their cerebellar symptoms and signs.
DISCUSSION
Evaluations of the effectiveness of the occipital transtentorial approach in the treatment of posterior cranial fossa tumors have been absent from the literature, most likely as a consequence of the relatively low frequency of these lesions. In the present study, 14 patients with this type of disease underwent surgery performed via the occipital transtentorial approach with the aid of image-guided surgery (IGS) systems. Total removal was achieved in all patients, with excellent postoperative results.
The occipital transtentorial approach was originally devised for lesions close to the pineal body. It had been considered a no man's land until Jamieson[4] successfully approached tumors of the region using a variation of Poppen's method.[11,12]
The occipital transtentorial approach provides excellent exposure of midline and unilaterally paramedian lesions of the precentral cerebellar fissure, posterior incisural space, and adjoining structures.[5]
The occipital interhemispheric transtentorial approach proved to be very useful for mediosuperior lesions of the cerebellum, without causing any neural structural damage, and allowed for a wider operative field.[8] This approach was very useful, safe, and accurate for removing superior cerebellar tumors and evaluating the surrounding anatomy, as well as for determining operative strategy.[2,14]
In our study, we used the occipital transtentorial approach to treat posterior cranial fossa tumors that included five meningiomas, three astrocytomas, two metastases, two hemangioblastomas, one cavernoma, and one dysgerminoma.
Our findings indicate that the occipital transtentorial approach can provide a sufficient operative field with minimal retraction of the occipital lobes and the peritumoral venous system in the treatment of these lesions.
This approach may offer the advantage of wide exposure, but it has the disadvantage of encountering the tumor beneath the deep venous system, which interferes with additional surgical removal or injures the deep feeding arteries of the tumor.[14] This approach provides a good view of the floor of the quadrigeminal region without strong flexion of the patient's neck and head. In this position, the surgeon can move the microscope comfortably in all directions and the tumor bed is usually observed just beneath the microscope.
The occipital transtentorial approach also provides direct vision into the depths of the precentral cerebellar fissure near the fourth ventricular roof, inferior colliculus, and anterior vermis. In contrast, the supracerebellar infratentorial approach provides a midline trajectory to midline lesions situated from the upper part of the precentral cerebellar fissure up to the tentorial incisura and below the deep venous system.[2,5,15,17]
The occipital transtentorial approach was described by Poppen[9,11,12] utilizing parasagittal occipital craniotomy exposing the lateral sinus, ventricular drainage, paramedian occipital lobe elevation, and resection of a wedge of tentorium through the suboccipital corridor.
In some reports, the occipital lobe is described as protruding alarmingly during the exposure until the basal cisterns near the tentorial notch are opened. Undoubtedly, these maneuvers risk tearing variably present draining veins and perturb the visual pathways near the occipital pole. Early postoperative visual field loss has been reported in 19–100% of patients, and long-term visual field loss has been reported in up to 17% of patients.[2,3,10]
The prone position to approach the pineal region allows comfortable access by the surgeon and an assistant, but still requires some occipital lobe retraction and has the disadvantage in the disorienting perspective the surgeon receives with the patient in the prone position. The “Concorde” position is at first view more comfortable for the surgeon, but is very disadvantageous for an assistant. The three-quarter prone position described by Ausman et al. in the Poppen and supracerebellar approaches has the advantages of all the previous positions without the disadvantages.[1] With the patient on the side, the risk of air embolus should be reduced over the seated position even though the head might be slightly tilted up. Occipital lobe retraction is markedly reduced because with the operated side down and a cannula in the lateral ventricle, the occipital lobe will fall away from the operative field and require very little retraction.
However, none of patients have had a postoperative hemianopsia in our series, so the “Concorde” position was found to be very useful and safe. The patient was operated with the need neutral and he was not turned to one side.
As for treatment of pineal region tumors, which has been described in recent reports,[7,9,17,19] the occipital transtentorial approach can extend the wide operative view to the thalamus and to the anterosuperior portion of the cerebellum.[8]
CONCLUSIONS
The occipital transtentorial approach provides excellent exposure for tumors of the posterior cranial fossa. This approach allows preservation of the superficial bridging veins and the deep veins around the pineal–tentorial region.
With careful study of the preoperative MRI scans, the approach can be tailored to the surgical lesion and individualized venous anatomy. This allows for a small, strategically placed craniotomy that avoids excessive occipital pole retraction, with improved neurological outcomes. Furthermore, the optimized exposure maximizes the chances of gross total resection of lesions in these locations. The results of this study demonstrate that the occipital transtentorial approach is an accurate, safe, and minimally invasive means of treating posterior cranial fossa tumors.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2012/3/1/85/99911
Contributor Information
Giuliano Maselli, Email: giuliano.maselli@tin.it.
Danilo De Paulis, Email: d.depaulis@alice.it.
Alessandro Ricci, Email: alex.ricci@email.it.
Renato J. Galzio, Email: renato.galzio@cc.univaq.it.
REFERENCES
- 1.Ausman JI, Malik GM, Dujovny M, Mann R. Three-quarter prone approach to the pineal-tentorial region. Surg Neurol. 1988;29:298–306. doi: 10.1016/0090-3019(88)90161-9. [DOI] [PubMed] [Google Scholar]
- 2.Cardenas RJ, Javalkar V, Ezer H, Burnham J, Nanda A. Occipital interhemispheric transtentorial approach to the superior cerebellum. J Clin Neurosci. 2011;18:128–30. doi: 10.1016/j.jocn.2010.04.053. [DOI] [PubMed] [Google Scholar]
- 3.Chi JH, Lawton MT. Posterior interhemispheric approach: Surgical technique, application to vascular lesions, and benefits of gravity retraction. Neurosurgery. 2006;59(Suppl 1):ONS41–9. doi: 10.1227/01.NEU.0000219880.66309.85. [DOI] [PubMed] [Google Scholar]
- 4.Jamieson KG. Excision of pineal tumors. J Neurosurg. 1971;35:550–3. doi: 10.3171/jns.1971.35.5.0550. [DOI] [PubMed] [Google Scholar]
- 5.Kawashima M, Rhoton AL, Jr, Matsushima T. Comparison of posterior approaches to the posterior incisural space: Microsurgical anatomy and proposal of a new method, the occipital bi-transtentorial/falcine approach. Neurosurgery. 2002;51(Suppl 3):S1208–21. [Google Scholar]
- 6.Kobayashi S, Sugita K, Tanaka Y, Kyoshima K. Infratentorial approach to the pineal region in the prone position: Concorde position. Technical note. J Neurosurg. 1983;58:141–3. doi: 10.3171/jns.1983.58.1.0141. [DOI] [PubMed] [Google Scholar]
- 7.Konovalov AN, Spallone A, Pitzkhelauri DI. Meningioma of the pineal region: A surgical series of 10 cases. J Neurosurg. 1996;85:586–90. doi: 10.3171/jns.1996.85.4.0586. [DOI] [PubMed] [Google Scholar]
- 8.Kurokawa Y, Uede T, Hashi K. Operative approach to mediosuperior cerebellar tumors: Occipital interhemispheric transtentorial approach. Surg Neurol. 1999;51:421–5. doi: 10.1016/s0090-3019(98)00123-2. [DOI] [PubMed] [Google Scholar]
- 9.Li Y, Zhao G, Wang H, Zhu W, Qu L, Li Y, et al. Use of 3D-computed tomography angiography for planning the surgical removal of pineal region meningiomas using Poppen's approach: A report of ten cases and a literature review. World J of Surg Oncol. 2011;9:64. doi: 10.1186/1477-7819-9-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nazzaro JM, Shults WT, Neuwelt EA. Neuro-ophthalmological function of patients with pineal region tumors approached transtentorially in the semisitting position. J Neurosurg. 1992;76:746–51. doi: 10.3171/jns.1992.76.5.0746. [DOI] [PubMed] [Google Scholar]
- 11.Poppen JL. The right occipital approach to a pinealoma. J Neurosurg. 1966;25:706–10. doi: 10.3171/jns.1966.25.6.0706. [DOI] [PubMed] [Google Scholar]
- 12.Poppen JL, Marino R., Jr Pinealomas and tumors of the posterior portion of the third ventricle. J Neurosurg. 1968;28:357–64. doi: 10.3171/jns.1968.28.4.0357. [DOI] [PubMed] [Google Scholar]
- 13.Reid WS, Clark WK. Comparison of the infratentorial and transtentorial approaches to the pineal region. Neurosurgery. 1978;3:1–8. doi: 10.1227/00006123-197807000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Rhoton AL., Jr The lateral and third ventricles. Neurosurgery. 2002;51(4 Suppl):S207–71. [PubMed] [Google Scholar]
- 15.Rhoton AL, Jr, Yamamoto I, Peace DA. Microsurgery of the third ventricle: Part 2—Operative approaches. Neurosurgery. 1981;8:357–73. doi: 10.1227/00006123-198103000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Sato O. Transoccipital transtentorial approach for removal of cerebellar haemangioblastoma. Acta Neurochir. 1981;59:195–208. doi: 10.1007/BF01406349. [DOI] [PubMed] [Google Scholar]
- 17.Stein BM. The infratentorial supracerebellar approach to pineal lesions. J Neurosurg. 1971;35:197–202. doi: 10.3171/jns.1971.35.2.0197. [DOI] [PubMed] [Google Scholar]
- 18.Yoshida S, Takahashi H. Cerebellar metastases in patients with cancer. Surg Neurol. 2009;71:184–7. doi: 10.1016/j.surneu.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 19.Yu JL, Zhao G, Qu LM, Li Y, Li YQ. Suboccipital transtentorial approach to pineal region meningiomas by 3D-CTA assistance: Surgical considerations. Zhonghua Wai Ke Za Zhi. 2011;49:245–9. [PubMed] [Google Scholar]


