Summary
Background and objectives
Buttonhole needling is reported to be associated with less pain than standard needling. The purpose of this study was to compare patient perceived pain and fistula complications in buttonhole and standard needling.
Design, setting, participants, & measurements
In this study, 140 conventional hemodialysis patients were randomly assigned to buttonhole or standard needling. The primary outcome was patient perceived pain with needling at 8 weeks. Fistula complications of hematoma, bleeding postdialysis, and infection were tracked.
Results
Median pain score at 8 weeks using a visual analog scale from 0 to 10 cm was similar for standard and buttonhole needling (1.2 [0.4–2.4] versus 1.5 [0.5–3.4]; P=0.57). Rate of hematoma formation in standard needling was higher (436 versus 295 of 1000 hemodialysis sessions; P=0.03). Rate of no bleeding postdialysis was 23.6 and 28.3 per 1000 in standard and buttonhole needling, respectively (P=0.40). Rate of localized signs of infection in standard versus buttonhole needling was 22.4 versus 50 per 1000 (P=0.003). There was one episode of Staphylococcal aureus bacteremia during the 8 weeks with buttonhole needling and no episodes with standard needling (P=1.00). Within 12 months of follow-up, another two buttonhole needling episodes developed S. aureus bacteremia, and nine buttonhole needling episodes had needling site abscesses requiring intravenous antibiotics versus zero standard needling episodes (P=0.003).
Conclusions
Patients had no difference in pain between buttonhole and standard needling. Although fewer buttonhole needling patients developed a hematoma, there was an increased risk of bacteremia and localized signs of infection. Routine use of buttonhole needling is associated with increased infection risk.
Introduction
Vascular access remains the Achilles heel of hemodialysis (HD) patients. Complications of vascular access, including infection and thrombosis, are a significant source of patient morbidity and mortality, with considerable impact on quality of life (1–3). Although arteriovenous fistulae (AVF) have the lowest complication rate, apprehension and fear of painful needling may dissuade patients from choosing an AVF as an access.
Improvements in needling technique may reduce patient perceived pain and maintain AVF patency. The most common complication of cannulation (needle infiltration/hematoma) is associated with an increased risk of thrombosis and loss of AVF patency (4). The current standard of practice is to needle the AVF using the rope ladder technique, which rotates needling sites at each dialysis session (referred to as standard needling [SN]).
Buttonhole needling (BN), a technique adopted from nocturnal dialysis (5), uses a constant site for arterial and venous needles. Based primarily on observational evidence, BN is believed to be associated with less painful needling (6–9), fewer needle infiltrations (5,9,10), and reduction in aneurysm size (8). Two small randomized studies have evaluated BN, with the most recent study completed in a mixed population (n=70) of home and in-center patients (11). Although earlier studies showed a reduction in pain with BN, more recent studies show either no reduction in pain (12,13) or even an increase in pain (14). Given the potential increased risk of infection with BN (15), a better understanding of the actual benefit is needed.
We undertook this randomized controlled trial to compare BN and SN techniques on patient perceived pain and AVF complications in conventional HD patients. The primary objective was to determine if, after 8 weeks of buttonhole creation, there was a difference in patient perceived pain at the time of needling for BN compared with SN. Secondary objectives included collecting information on hematoma formation, time to hemostasis, risk of AVF infection, and nursing perceived difficulty in needling.
Materials and Methods
Study Design
We undertook this randomized controlled trial in 140 conventional (three times per week for 4 hours) in-center HD patients with AVF. After providing written informed consent, eligible patients were randomly assigned by a central service, in a 1:1 ratio, with the use of a permuted block design. Ethics approval was obtained from the University of Calgary Research Ethics Board. The trial adhered to the Declaration of Helsinki and was registered with Current Controlled Trials (ISRCTN94795553).
Inclusion/Exclusion Criteria
Eligible patients were adults 18 years and older dialyzing with a stable AVF (access flow constant over the previous 4 months without surgical or radiologic interventions) or needled consistently for at least 4 weeks with an access flow>500 ml/min. All AVFs were a minimum length of 10 cm to allow placement of two needles 3 cm apart and 3 cm from the arteriovenous anastamosis. Patients planning to move or having impending transplant or transfer to peritoneal dialysis were excluded. Patients who self-needled, refused to stop intradermal lidocaine, or were unable to complete the visual analog scale (VAS) were also excluded.
Data Collection and Outcome Variables
Baseline data, including age, sex, history of diabetes, cardiovascular disease, and details regarding the AVF (type and location, date of creation, recent access flow, and fistulogram results), were obtained.
At each HD session over the 8-week period, data were obtained on presence and size of hematomas, nursing perceived degree of difficulty needling, signs of localized infection, and time to hemostasis after removal of the HD needles. After the 8-week study period, patients were followed for a 1-year period for AVF patency and assessment of infectious complications.
Outcomes
The primary outcome, patient perceived pain postneedling, was assessed by an individual blinded to needling type using a validated 10-cm VAS (16–18). Assessment of pain was collected for the three HD runs at baseline and again during week 8. The median pain score based on these three runs determined patient perceived pain. To ensure balanced treatment of the AVF in both groups and given the frequent use of anesthetic before study start, all patients received a topical 5% lidocaine gel applied to their AVF for 5 minutes during weeks 1 and 8. During the rest of the study period, patients were allowed to use their usual anesthetic (Table 1), except that BN patients did not use intradermal lidocaine as per standard technique (5).
Table 1.
Characteristics of patients randomized to buttonhole or standard needling groups
| Characteristic | Standard Needling (n=70) | Buttonhole Needling (n=70) |
|---|---|---|
| Mean age (SD) in years | 66.7 (14.4) | 70.3 (12.3) |
| Male sex (n; %) | 46 (65.7) | 51 (72.9) |
| Comorbid illnesses (n; %) | ||
| Diabetes mellitus | 39 (55.7) | 33 (47.1) |
| Coronary artery disease | 28 (40.0) | 31 (44.3) |
| Years on hemodialysis (median) | 3.0 (1.6–5.4) | 2.8 (1.6–5.6) |
| Coumadin (n; %) | 9 (12.9) | 5 (7.1) |
| Mean international normalized ratio (SD) | 2.2 (0.3) | 2.4 (0.4) |
| Type of arteriovenous fistula (n; %) | ||
| Radiocephalic | 13 (18.6) | 11 (15.7) |
| Brachiocephalic | 32 (45.7) | 43 (61.4) |
| Brachial basilic | 24 (34.3) | 16 (22.9) |
| Other | 1 (1.4) | 0 |
| Previous fistulogram/fistuloplasty (n; %) | 48 (68.6) | 43 (61.4) |
| Anesthesia used (n; %) | 20 (28.6) | 17 (24.3) |
| Type of anesthesia if used | ||
| Eutectic mixture of local anesthetics topical | 9 (45.0) | 13 (76.5) |
| Lidocaine topical | 9 (45.0) | 2 (11.8) |
| Intradermal lidocaine | 2 (10.0) | 2 (11.8) |
Data are expressed as mean ± SD, median (25th to 75th percentile), or number (percentage).
The secondary outcomes, documented at each run, included hematoma formation, time to hemostasis postneedle removal, localized signs of AVF infection (erythema, pus, or swelling), AVF infection defined by abscess or bacteremia, and ease of needling from a nursing perspective. Hematoma was categorized based on size as 0–4.9, 5–10, or >10 cm. Time to hemostasis postdialysis was categorized (8) as no bleeding, <5 minutes, 5–10 minutes, or >10 minutes bleeding post-HD. Ease of needling from the nurse perspective was assessed on a scale from zero to five, with zero being no difficulty and five being high difficulty or unable to needle.
The presence of cellulitis or abscess at the AVF site as well as bacteremia or metastatic infectious complications were monitored at each HD session. If erythema or pus was present on the AVF, a swab for culture and sensitivity was taken; a positive culture was defined as presence of neutrophils with cultured bacteria. According to center protocol, any patient with fever, rigors, malaise, or suspected infection had two sets of blood cultures drawn. If an AVF infection developed, the AVF was needled at a site not affiliated with the infection (for both SN and BN). Intravenous antibiotics were given if the culture and sensitivity were positive, the patient developed a fever, or an abscess or overt cellulitis developed.
BN and SN Descriptions
Patients randomized to the BN group were needled using a standard sharp needle for the first six to nine HD runs (2–3 weeks; until the BN track was established) by a nurse trained in this technique. BN sites were created using a 20°–30° angle at least 3 cm from the arterial or venous anastamosis. The distance from the wrist and/or distance from the antecubital fossa (whichever was closer) to the BH site was recorded as well as the angle of insertion. All venous needles were inserted in antegrade fashion, and arterial needles were inserted preferentially in antegrade fashion according to standard care. Consistent with the practice that Twardowski (5) initiated, intradermal lidocaine was not allowed during the course of the study because of concerns regarding distortion of anatomy and interference with establishment of the BN track. Topical anesthetic creams were allowed except during baseline and week 8 (when pain scores were tested); at those times, a 5-minute application of topical lidocaine was applied before needling for all patients. The same nurse was used to maintain the BN track for 1 additional week using the dull needles until the BN site was established. An established BN site was defined as a track created over six to nine HD runs using sharp needles that easily accepts a blunt needle after the third consecutive blunt needling. After the BN site was established, the regular nursing staff needled the BN patients with BN technique and dull needles.
Patients randomized to SN continued to receive SN throughout the 8-week study period. Both BN and SN AVFs were disinfected with chlorhexidine/alcohol 70% before cannulation in accordance with Kidney Disease Outcomes Quality Initiative guidelines (19). Individuals that did not tolerate this disinfectant received a 60-second application of 70% alcohol. In BN patients, the AVF was disinfected before and after scab removal (using a sterile dull needle). Topical exit site prophylaxis was not used.
Statistical Analyses
All analyses followed the intent-to-treat principle. Baseline data were described as mean ± SD, median (25th to 75th percentile), or frequencies as appropriate. Nonparametric comparisons were performed using the Wilcoxon rank sum test. Categorical measures were compared using the chi-squared or Fisher exact test. All analyses were performed using Stata/IC 11.2. Analyses were based on the difference between groups for the outcome after 8 weeks. For the primary objective, the Wilcoxon rank sum test was used to determine if there was a difference in median pain scores (based on three HD sessions) at week 8 for the BN group compared with the SN group. For patients who did not have pain scores at 8 weeks, we carried forward the last pain score obtained. We assessed the impact of this imputation in a sensitivity analyses, where we replaced the missing values for the BN group with a conservative approach (using the highest pain score achieved within that group) and we replaced missing values for the SN group with an anticonservative imputation (using the lowest pain score achieved). Additional analysis limited to subjects with complete data at 8 weeks was done.
For the secondary objectives, the rate of hematoma formation (per 1000 dialysis sessions) for BN and SN was determined. We also compared the proportion of BN and SN patients with a time to hemostasis of >5 minutes, signs of localized infection (erythema, pus, or swelling), and AVF infection (defined by cellulitis, abscess, or bacteremia) using the chi-squared test. An unpaired t test was used to compare mean nursing needling difficulty for the two study groups. All tests of significance are two-sided, with a P value<0.05 considered statistically significant.
Sample Size
Based on pilot data from randomly selected patients with an AVF in our HD unit, we determined a mean (SD) pain score postneedling using the 10-cm VAS of 3.0 (±1.5). Assuming an effect size of 50% (i.e., a decrease in perceived pain from 3.0 to 1.5) based on previously published studies (8,9) using BN, with an α=0.05 and 80% power, we determined that a sample size of 63 patients per group or a total of 126 patients was required. We calculated our sample size based on an approximate 10% dropout rate to account for potential dropout or loss to follow-up, and thus, we planned to recruit 70 patients per arm (140 patients).
Results
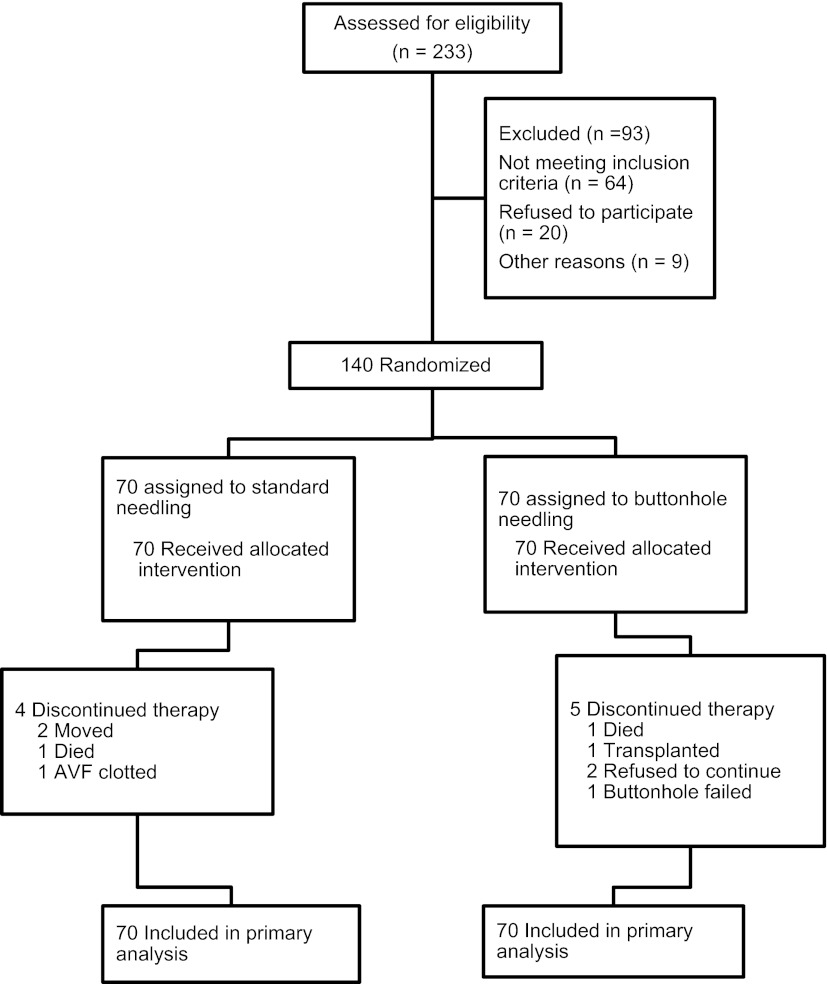
Of the 140 patients randomized, 131 patients completed the study: 66 patients in the SN group and 65 patients in the BN group (Figure 1). All patients were included in intention to treat analyses. Baseline characteristics (Table 1) were similar; the patients were older and on dialysis for over 2.5 years, and approximately one-quarter of them used anesthetic with needling.
Figure 1.
Patient flow diagram depicting enrollment, randomization, and follow-up of study patients.
The median pain score at 8 weeks was similar (SN=1.2 [0.4–2.4] versus BN=1.5 [0.5–3.4], P=0.57) (Table 2). The median pain score did not change over the 8 weeks: SN baseline=1.5 (0.4–3.2) to 1.2 (0.4–2.4) at 8 weeks (P=0.24) and BN baseline=1.6 (0.5–3.2) to 1.5 (0.5–3.4) at 8 weeks (P=0.86). Similar results were obtained in a sensitivity analysis limited to patients who completed the study (data not shown).
Table 2.
Pain scores at baseline and 8 weeks with standard and buttonhole needling
| Standard Needling (n=70) | Buttonhole Needling (n=70) | P Value (Between Group) | |
|---|---|---|---|
| Baseline (week 1) median (25th to 75th percentile) | 1.5 (0.4–3.2) | 1.6 (0.5–3.2) | 0.78 |
| Study end (week 8) median (25th to 75th percentile) | 1.2 (0.4–2.4) | 1.5 (0.5–3.4) | 0.57 |
| P value (within group) | 0.24 | 0.86 |
The median value is based on the three pain scores per patient each week and expressed as median (25th to 75th percentile).
A greater proportion of patients in the BN group (20/70, 28.6%) had excess pain, which was defined by a mean pain score>3 at 8 weeks, compared with the SN group (11/70, 15.7%, P=0.07; odds ratio [OR]=2.15; 95% confidence interval [CI]=0.87–5.44).
The rate of hematoma formation in the SN group was higher (436 per 1000 dialysis sessions) than in the BN group (295 per 1000 sessions, P=0.03). A greater proportion of patients in the SN group had at least one hematoma (25/70, 36%) versus the BN group (12/70, 17%, P=0.01; OR=0.37; 95% CI=0.15–0.87). The proportion of patients with a large hematoma (>5 cm diameter) was higher in the SN group, although this result did not reach statistical significance (11/70 SN versus 5/70 BN, P=0.18; OR=0.41; 95% CI=0.11–1.39). The results were similar in an analysis limited to patients who completed the study.
The time to hemostasis postdialysis was similar for SN and BN (Table 3). The rate of no bleeding postdialysis was 23.6 and 28.3 per 1000 dialysis sessions in SN and BN groups, respectively (P=0.40), whereas the rate of any bleeding was 97.6 and 97.2 per 1000 dialysis sessions in SN and BN groups, respectively (P=0.90). There was no difference in the proportion of patients who had a bleeding time>10 minutes (25/70 SN and 22/70 BN, P=0.59; OR=0.83; 95% CI=0.38–1.77).
Table 3.
Rates of secondary outcomes (per 1000 dialysis sessions) for standard and buttonhole needling
| Outcomes | Standard Needling Rate per 1000 Dialysis Sessions | Buttonhole Needling Rate per 1000 Dialysis Sessions | P Value |
|---|---|---|---|
| Hematoma formation | 436 | 295 | 0.003 |
| Bleeding postdialysis | |||
| No bleeding | 23.6 | 28.3 | |
| Any bleeding | 97.6 | 97.2 | 0.40 |
| Signs of localized infection | 22.4 | 50.0 | 0.003 |
Signs of localized infection included erythema, pus, or swelling at the fistula site.
The rate of localized infections in the SN group was 22.4 per 1000 dialysis sessions versus 50 per 1000 dialysis sessions in the BN group (P=0.003). The median (25th to 75th percentile) number of localized infections was 1 (1–1.5) in the SN group versus 2 (1–3) in the BN group.
During the 8-week study period, there was one episode of Staphylococcal aureus (SA) bacteremia (week 6) in the BN group and no episodes in the SN group (P=1.00). Subsequently, after study completion (but within 12 months of the study start), another two BN patients developed SA bacteremia, and nine BN patients had an abscess at the needling site requiring intravenous antibiotics compared with zero SN patients (P=0.003). Two of the study patients had already abandoned BN when they developed their infections, whereas the remaining nine patients were still using BN at the time of infection.
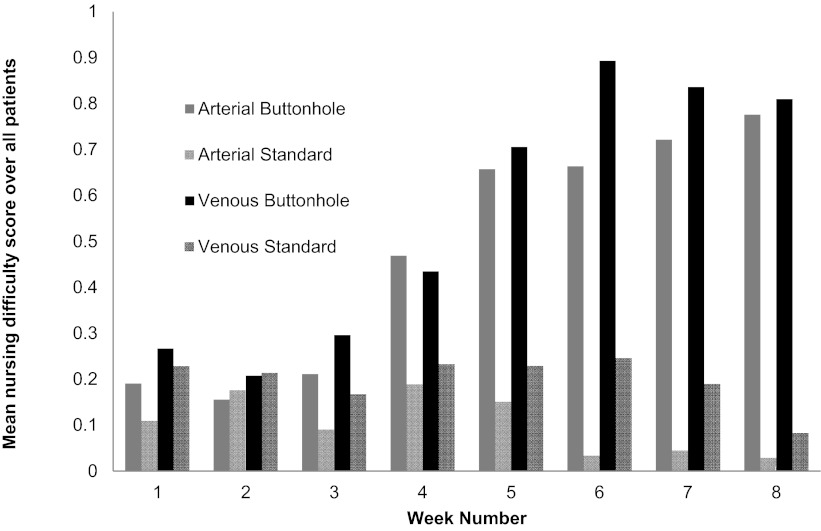
Overall, BN had higher median (25th to 75th percentile) difficulty needling scores for both arterial (0.33 [0.17–0.56]) and venous (0.5 [0.17–0.79]) sites compared with SN (arterial=0.0.4 [0–0.13] and venous=0.10 [0–0.29], P<0.001). The difficulty of needling increased over the course of the study for BN and remained relatively stable for SN (Figure 2). The proportion of patients with a difficulty score of more than two was consistently higher starting at week 4 in the BN group (20/69) compared with the SN group (6/69, P=0.002).
Figure 2.
Nursing perceived difficulty of needling over the course of the study. The difficulty score was calculated on a weekly basis as the mean of the three hemodialysis sessions per week. The difficulty scores were significantly higher for buttonhole needling (for both arterial and venous needles) compared with standard needling starting at week 4.
Discussion
Our study, the first to compare BN with SN in a large randomized controlled trial in conventional HD patients, did not find a reduction in pain with BN. Although we did find a significant reduction in hematoma for BN, whether this finding translates to improved fistula longevity remains to be determined. A concerning finding, however, was that signs of erythema, pus, or swelling were doubled in the BN group (50 per 1000 dialysis runs) compared with the SN group (22.4 per 1000 dialysis runs). In addition, there was an increased risk of SA bacteremia (three patients) or abscess (nine patients) within 12 months of starting BN.
There were no differences in pain scores at baseline between SN and BN groups or at the end of our study. We used a 10-cm VAS that has been validated in chronic disease (18) and used in hemodialysis patients (13). Prior studies reporting a reduction of painful needling with the BN technique were limited by their observation- (5,8,9) or survey-based design (7,10) without an adequate comparison group (20).
Two recent randomized trials have compared BN with SN (11,13). Consistent with our results, the work by Chow et al. (11) found no difference in pain scores (determined with a VAS from zero to five) in 69 patients, although this study included both in-center and home dialysis patients. The other randomized trial (13) was completed in 56 in-center HD patients and also did not find a difference in median pain scores using a 10-cm VAS (1.0 SN versus 2.5 BN; no P value reported). However, patients were allowed to use local anesthetic, if needed, throughout the study, making the pain scores difficult to interpret.
The increased risk of infectious complications with BN is particularly important. Similar results have been reported in both in-center (8,21) and extended dialysis patients (9,15,22). The work by Chow et al. (11) reported four patients with an infection at the BN site and one patient with an infection at the SN site (although this patient had previously used BN). The work by Struthers et al. (13) reported one fistula infection in the BN group and zero fistula infections in the SN group. The work by Labriola et al. (21) reported an increase in infectious complications (bacteremia and/or local AVF infection) after switching to BN in a large in-center HD unit from 0.17 (95% CI=0.086–0.31) to 0.43 (95% CI=0.29–0.61) events per 1000 AVF days (P=0.003). Of particular concern was that this increase in infectious complications did not occur until the second full year of BN, implying that follow-up of many of the reported studies may be too short to notice the true increases in infectious complications with BN.
A retrospective review of SA bacteremia over a 10-year period in home dialysis patients suggested a high risk of infection with BN, with 10 SA bacteremia cases in 55 home dialysis patients (OR=35.3, 95% CI=2–626, P=0.01) (15). Based on expert opinion (15), it has been suggested that topical mupirocin be applied to the buttonhole sites to reduce the risk of infections. However, even with this approach, the risk of SA bacteremia is still higher with BN (OR=6.4, 95% CI=1.3–32.3) (15). Additional studies are required to determine the optimal methods to reduce the risk of infection.
The results of our study show that BN is a difficult technique when done by multiple HD nurses in a traditional dialysis unit. Our nurses found it difficult to maintain the buttonhole track; the difficulty scores in the BN patients started to increase in week 4, which corresponded to the use of the blunt needle, and continued to increase throughout the remainder of the study. Increasing difficulty with BN is likely to result in increased complications at the needling site, and it may negate any potential benefit anticipated with the BN technique. Longer-term follow-up of these patients is required to evaluate the impact of the difficulty in needling.
A reduction in hematoma formation with BN has been reported (5,14). The work by Chow et al. (11) reported more hematomas in BN patients in a randomized trial, although this finding was attributed to lack of experience by the nurses. It is plausible that the blunt needle used in BN is less traumatic and subsequently, has a lower risk of hematoma. We did not explore the effect of BN on aneurysm formation or growth, but other studies have reported a reduction in aneurysm size with initiation of BN (8,14).
Our study has strengths and limitations. Our findings are limited to the conventional dialysis population needled by dialysis nurses. Although pain with needling might be less when done by the patient themselves, our results can be generalized to the majority of patients who are dialyzed in a dialysis center. Another potential limitation was the use of topical anesthetic during the 1 week that the pain assessment was completed, which may have reduced pain scores in both groups. However, this use was necessary, because approximately 25% of patients used an anesthetic with needling at baseline, and we anticipated difficulty recruiting and maintaining patients in the study if anesthetic use was discontinued. Thus, we standardized treatment across groups and applied 5 minutes of topical lidocaine cream before needling. One could argue that 5 minutes is unlikely to produce a significant effect on pain perception. Another limitation is that the study was designed and initiated before the publication of the work by Nesrallah et al. (15), which showed a reduction in bacteremia with topical antibiotic prophylaxis. A randomized trial comparing SN with BN with topical prophylaxis is required. Our study was done in a rigorous manner with an adequate sample size and pain scores obtained by an individual blinded to treatment assignment. Our results show no reduction in pain with BN and an increased risk of systemic and localized infections compared with SN. Although there were fewer hematomas, whether this finding translates to a reduction in fistula interventions and improved patency remains to be determined. Careful consideration should be given before routine use of BN in in-center HD patients.
Disclosures
None.
Acknowledgments
This work was supported by the Kidney Foundation of Canada (Biomedical Research Grant).
This work was presented in abstract form at the American Society of Nephrology Annual Meeting, November 12, 2011, Philadelphia, Pennsylvania, and the Canadian Society of Nephrology Annual Meeting, April 26, 2012, Newfoundland, Canada.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Accessing the Access,” on pages 1548–1550.
References
- 1.Wasse H, Kutner N, Zhang R, Huang Y: Association of initial hemodialysis vascular access with patient-reported health status and quality of life. Clin J Am Soc Nephrol 2: 708–714, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allon M: Current management of vascular access. Clin J Am Soc Nephrol 2: 786–800, 2007 [DOI] [PubMed] [Google Scholar]
- 3.Polkinghorne KR, McDonald SP, Marshall MR, Atkins RC, Kerr PG: Vascular access practice patterns in the New Zealand hemodialysis population. Am J Kidney Dis 43: 696–704, 2004 [DOI] [PubMed] [Google Scholar]
- 4.Lee T, Barker J, Allon M: Needle infiltration of arteriovenous fistulae in hemodialysis: Risk factors and consequences. Am J Kidney Dis 47: 1020–1026, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Twardowski Z, Kubar H: Different sites versus constant sites of needle insertion into arteriovenou fistulas for treatment by repeated dialysis. Dial Transplant 8: 978–980, 1979 [Google Scholar]
- 6.Ball LK: The buttonhole technique for arteriovenous fistula cannulation. Nephrol Nurs J 33: 299–304, 2006 [PubMed] [Google Scholar]
- 7.Toma S, Shinzato T, Fukui H, Nakai S, Miwa M, Takai I, Maeda K: A timesaving method to create a fixed puncture route for the buttonhole technique. Nephrol Dial Transplant 18: 2118–2121, 2003 [DOI] [PubMed] [Google Scholar]
- 8.Marticorena RM, Hunter J, Macleod S, Petershofer E, Dacouris N, Donnelly S, Goldstein MB: The salvage of aneurysmal fistulae utilizing a modified buttonhole cannulation technique and multiple cannulators. Hemodial Int 10: 193–200, 2006 [DOI] [PubMed] [Google Scholar]
- 9.Verhallen AM, Kooistra MP, van Jaarsveld BC: Cannulating in haemodialysis: Rope-ladder or buttonhole technique? Nephrol Dial Transplant 22:2601–2604, 2007 [DOI] [PubMed] [Google Scholar]
- 10.Ball LK, Treat L, Riffle V, Scherting D, Swift L: A multi-center perspective of the Buttonhole Technique in the Pacific Northwest. Nephrol Nurs J 34: 234–241, 2007 [PubMed] [Google Scholar]
- 11.Chow J, Rayment G, San Miguel S, Gilbert M: A randomised controlled trial of buttonhole cannulation for the prevention of fistula access complications. J Ren Care 37: 85–93, 2011 [DOI] [PubMed] [Google Scholar]
- 12.Figueiredo AE, Viegas A, Monteiro M, Poli-de-Figueiredo CE: Research into pain perception with arteriovenous fistula (avf) cannulation. J Ren Care 34: 169–172, 2008 [DOI] [PubMed] [Google Scholar]
- 13.Struthers J, Allan A, Peel RK, Lambie SH: Buttonhole needling of ateriovenous fistulae: A randomized controlled trial. ASAIO J 56: 319–322, 2010 [DOI] [PubMed] [Google Scholar]
- 14.van Loon MM, Goovaerts T, Kessels AGH, van der Sande FM, Tordoir JHM: Buttonhole needling of haemodialysis arteriovenous fistulae results in less complications and interventions compared to the rope-ladder technique. Nephrol Dial Transplant 25:225–230, 2010 [DOI] [PubMed] [Google Scholar]
- 15.Nesrallah GE, Cuerden M, Wong JH, Pierratos A: Staphylococcus aureus bacteremia and buttonhole cannulation: Long-term safety and efficacy of mupirocin prophylaxis. Clin J Am Soc Nephrol 5: 1047–1053, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dexter F, Chestnut DH: Analysis of statistical tests to compare visual analog scale measurements among groups. Anesthesiology 82: 896–902, 1995 [DOI] [PubMed] [Google Scholar]
- 17.Reading AE: A comparison of pain rating scales. J Psychosom Res 24: 119–124, 1980 [DOI] [PubMed] [Google Scholar]
- 18.Olsen SNM, Nolan MF, Kori S: Pain measurement. An overview of two commonly used methods. Anesthesiol Rev 19: 11–15, 1992 [PubMed] [Google Scholar]
- 19.Vascular Access 2006 Work Group : Clinical practice guidelines for vascular access. Am J Kidney Dis 48 [Suppl 1]: S176–S247, 2006 [DOI] [PubMed] [Google Scholar]
- 20.Castro MCM, Silva CD, Souza JMR, Assis MCSB, Auki MVS, Xagoraris M, Centeno JR, Souza JAC: Arteriovenous fistula cannulation by buttonhole technique using dull needle. Braz J Nephrol 32: 281–285, 2010 [PubMed] [Google Scholar]
- 21.Labriola L, Crott R, Desmet C, André G, Jadoul M: Infectious complications following conversion to buttonhole cannulation of native arteriovenous fistulas: A quality improvement report. Am J Kidney Dis 57: 442–448, 2011 [DOI] [PubMed] [Google Scholar]
- 22.Van Eps CL, Jones M, Ng T, Johnson DW, Campbell SB, Isbel NM, Mudge DW, Beller E, Hawley CM: The impact of extended-hours home hemodialysis and buttonhole cannulation technique on hospitalization rates for septic events related to dialysis access. Hemodial Int 14: 451–463, 2010 [DOI] [PubMed] [Google Scholar]