Abstract
Purpose
Case managers facilitate continuity of care for Persons Living with HIV (PLWH) by coordination of resources and referrals to social services and medical care. The complexity of HIV care and associated comorbidities drives the need for medical and psychosocial care coordination, which may be achieved through health information exchange (HIE) systems. However, the use of HIE has not been well studied in the context of HIV services. The purpose of this descriptive qualitative study is to explore factors influencing case managers adoption of electronic clinical data (ECD) summaries as an HIE strategy in HIV care through application of the “Fit between Individuals, Task and Technology” (FITT) framework.
Methods
Focus group methodology was used to gather perceptions from 48 participants who provided direct case management services for PLWH in New York City. Questions addressed current quality and efficiency challenges to HIE utilization in the context of case management of PLWH as well as barriers and enablers to use of an ECD summary. Analysis of the data was guided by the FITT framework.
Results
Major themes by interaction type were: 1) task-technology fit- resources, time and workflow; 2) individual-task fit - training and technical support; and 3) individual-technology fit - ECD summary functionality, technical difficulties and a the need of a computer for each end-user.
Conclusions
Our findings provide evidence for the applicability of the FITT framework to explore case managers’ perceptions of factors influencing the adoption of ECD summary systems for HIV care prior to actual implementation. Assessment of fit among individual, task, and technology and addressing the concerns identified prior to implementation is critical to successful adoption of health information technology as a strategy to improve quality and efficiency in health care.
Keywords: electronic clinical data summary, continuity of care, continuity of care record, continuity of care document, HIV/AIDS, FITT Framework
INTRODUCTION
For many people living with HIV (PLWH) advances in antiretroviral therapy have transformed a once fatal disease into a manageable chronic medical condition. Accordingly, the needs for comprehensive management of the disease have grown, now requiring a broad array of services [1]. In addition to high quality clinical care, PLWH often need additional disease prevention counseling, health education, care coordination and facilitated access to a variety of community resources [2]. Thus, the overall complexity of comprehensive HIV care has grown since it increasingly relies upon the coordinated efforts of a multidisciplinary workforce to achieve desired outcomes [3]. Case management has been a frequently used strategy for targeting and coordinating care [4]. HIV case management programs are designed to provide PLWH continuity of care by coordination of resources and referrals to community-based social services and medical care [5]. Nonetheless, HIV case managers frequently do not have access to information regarding their clients’ health status, medication information and clinician visits which would allow them to better coordinate their patients’ care. Health Information Exchange (HIE) is a key strategy for meeting case managers’ information needs.
The purpose of this paper is to explore factors influencing case managers’ adoption of electronic clinical data (ECD) summaries as an HIE strategy in HIV care through application of the “Fit between Individuals, Task and Technology” (FITT) framework [6].
BACKGROUND
Health Information Exchange (HIE)
Improved access to data through health information exchange (HIE) is likely to enhance the quality of care rendered and improve multidisciplinary coordination [7]. HIE refers to the process of reliable and interoperable electronic health-related information sharing across organizations conducted in a manner that protects the confidentiality, privacy, and security of the information [8]. The potential benefits of HIE include improved health care quality, lower health care costs, and improved tracking of chronic disease management [5]. Nevertheless, implementation and use of technologies that support HIE does not guarantee improved outcomes. Poor application of health information technology (HIT) can result in systems that are difficult to use, create additional workload for system users, or lead to tragic errors [9]. In contrast, well-designed systems can decrease the need for users to remember large amounts of information, which reduces the risk of errors [10]. There are a number of different strategies for supporting HIE including electronic health records (EHRs), Regional Health Information Organizations[11], CONNECT, and NHIN Direct [12]. Regardless of the strategy, a critical aspect of HIE is integration of standards that support functional interoperability (i.e., the ability to receive and interpret data) among systems. Health Level Seven (HL7) provides key standards for exchange of individual messages (e.g., a laboratory value), documents (e.g., a progress note), EHRs, and electronic clinical data (ECD) summaries (e.g., a continuity of care document [CCD]) [13].
ECD Summaries
The ECD summary is the HIE strategy of focus in this article [14]. ECD summaries can play a critical role in supporting chronic care management for PLWH, by providing access to health information and facilitating care coordination and continuity [15]. An easily accessible and accurate ECD summary offers many potential benefits for the overall care of patients, including reducing the risk of medical errors, decreasing pharmacy errors and providing just in time clinical information – all of which potentially could save lives [7]. ECD summaries have the potential to promote uncomplicated access to critical patient data and allow for care to be more complete by providing healthcare services that are less redundant, time intensive, and prone to error [16]. In particular, access to pharmacy utilization data via an ECD summary can inform healthcare providers with regard to possible medication adherence issues and can be a unique contribution to care for PLWH [17].
ECD summaries are derivatives of existing ECD such as that in EHRs or administrative databases and are created through different platforms such as those provided by EHR vendors or through more general standards-based approaches such as continuity of care records (CCRs) or CCDs. In contrast to the EHR, which is a longitudinal record of patient health information generated by patient encounters in any care delivery setting[ 18], vendor-specific ECD summaries, CCRs, and CCDs provide a more limited set of clinical data that is optimized to support continuity of care across settings [19]. The standard for the CCR was initially developed by the American Society for Testing and Materials (ASTM), which in collaboration with HL7, created the CCD standard which integrates additional guidance for implementation of standard data models into clinical information systems [20]. The CCD is designed to be accessible in multiple formats such as remote access via a secure Internet connection, direct secure electronic sharing among members of the healthcare team, and printed format [21].
FITT Framework
The FITT framework [22] is based on the idea that adoption of information technology (IT) “depends on the fit between the attributes of the users (e.g., motivation), the attributes of the technology (e.g., usability), and the attributes of the clinical tasks and processes (e.g., task complexity)”[6]. (Figure 1) The interaction of user and task is the decisive new element of this approach. The FITT framework supports analysis of the various interconnected factors that influence the success or failure of IT implementation, thus facilitating understanding of why an IT system can be a success or a failure [23, 24]. Like other technology acceptance frameworks, FITT is suitable for application prior to IT implementation to identify factors that may influence successful IT adoption so that issues can be addressed prior to the implementation phase [25]. In comparison to earlier models that informed its development such as the Technology Acceptance Model [26], the Information System Success Model [27], the Information Technology Adoption Model [28], and the Task-Technology-Fit model [29], the FITT framework has been used in relatively few studies [22, 25]. Thus, our application of the FITT framework for analysis of factors influencing case managers’ adoption of ECD summaries prior to implementation will contribute to the body of literature regarding the framework.
Figure 1.
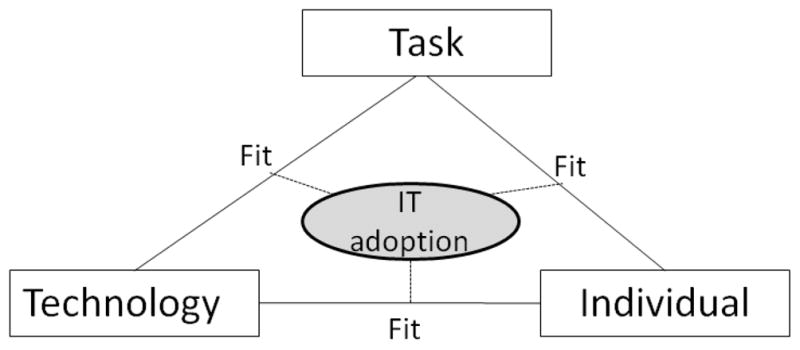
The FITT framework (FITT) by Ammenwerth et al.
METHODS
Settings
Study settings were two HIV case management sites affiliated with Bronx-Lebanon Hospital Comprehensive Care Center (BLH-CCC) and four HIV case management sites affiliated with NewYork-Presbyterian System SelectHealth (SH). BLH-CCC is a hospital-based outpatient clinic located in the Bronx, NY, which provides primary care and specialty care to approximately 3,100 PLWH. The patient population of BLH-CCC consists of predominantly ethnic minorities, including immigrants arriving from western Africa, the Caribbean and Central America. SH is a New York City based Medicaid Managed Care Special Needs Plan that coordinates care and a host of benefits to eligible PLWH. The patient population of SH comprises approximately 8,000 socioeconomically disadvantaged PLWH and their dependents; most are African American and about half are female.
Sample and Recruitment
Data were collected from March 2008 – February 2010. Convenience samples of case managers affiliated with BLH-CCC and SH were recruited to participate in focus groups. Inclusion criteria for focus group participation included English speaking and the ability to provide informed consent. Recruitment of participants included direct contact by clinic directors and distribution of fliers. A total of 48 case managers participated in six focus groups: 11 BLH-CC case managers in two focus groups and 37 SH case managers in four focus groups. Participants across focus groups were predominantly female and African American or Latino
Procedures
All study materials and procedures were approved by the Institutional Review Boards of Bronx-Lebanon Hospital (for BLH-CCC) and Columbia University (for SH). Each focus group session was facilitated by a member of the research team, a second member recorded field notes.
Following completion of the informed consent process, the facilitator described the ECD summary system. For BLH-CCC focus groups, the facilitator described a plan to implement a feature within Bronx Lebanon’s EHR, Eclipsys, to support exchanging ECD between community service providers and clinicians. Through the newly created ePartner Report, case managers would be able to log in to view a subset of EHR data for their respective patients including visits, vaccinations, laboratory results, and medications. For SH, the facilitator described a secure, web-based CCD containing ECD from SH’s administrative databases including provider contact information, laboratory data, procedures, and pharmacy refills. Although the focus group discussions were centered on case manager use, case managers were also told that the ECD summary would be viewable by clinicians and SH members (i.e., PLWH) from any computer with an Internet connection.
Development of the focus group guide was informed by the PRECEDE portion of the PRECEDE/PROCEED framework and designed to elicit predisposing, enabling, and reinforcing factors for case manager use of an ECD summary [30]. Questions addressed current quality and efficiency challenges to HIE in the context of case management of PLWH as well as barriers and enablers to use of an ECD summary.
Each focus group session lasted approximately one hour and was audio recorded. The facilitator summarized the key points at the end of each question and sought verification or clarification from participants. Participants from SH were reimbursed for their time. BLH participants did not receive reimbursement for their time but were provided with food appropriate for the time of day.
Data Analysis
Coding of the data began after reading each transcript at least twice; codes were created based on a line-by-line analysis using paper and pen. Principles of content analysis [31] were used in an iterative fashion to identify descriptive codes, then more general categories, and finally major themes in the data. Data were summarized thematically through an iterative process by two of the authors (RS, SB) and organized according to the FITT framework. Discrepancies during data analysis were discussed until consensus was reached.
RESULTS
We organized our findings according to the components of the FITT framework. Our main findings suggest that the quality of fit depends on the fit between the: 1) task and the technology such as system functionality and workflow; 2) individual and the task such as efficient training sessions and end-user attitude 3) individual and the technology such as computers available to end-users and existing IT skills.
Fit between task and technology
Overall, participants expressed that the web-based CCD had the ability to save resources and time. One case manager thought it would enable a workflow where there would be “less writing for us.” Multiple case managers explained that they thought a web-based CCD would be a time-saving tool because they spend a great deal of time accessing information about their patients. “I think you also will give us more time because we are running around looking for providers to give us information.”
Additionally, participants thought that the system would save resources. More specifically, a few case managers mentioned that labs and tests are ordered multiple times for the same diagnostic condition because the documentation is not available or readily accessible. One participant explained that the web-based CCD would be “cost effective because it would allow not for repetitive tests to be done when not necessary like when sometimes they [providers] will order labwork if I won’t call for 2 weeks then they will think oh I didn’t have that labwork or I need that labwork…” Another case manager described how providers just assume that “PPDs [tuberculosis skin test] are outdated and we probably wouldn’t look into [the] date of the last one, we’ll say he is already due for the next one.” In this case, there is often an overuse of resources because important health information is not available.
For the ePartner Report, case managers at BLH expressed concerns that the system would not fulfill its intended use of improving HIE. More specifically, there were concerns that physicians may not participate in using the system. “Are the doctors viewing this as a benefit or a barrier? …Because that would be a barrier for us. Because we might love it and be all in there and then they don’t respond.” As a result, the case managers were concerned that the information contained within the ePartner Report would not include updated information because of lack of use of the system by the physicians. In addition, there were concerns about the technological stability of the system and how often it would “go down.” Participants described how their whole work day can become worthless if an electronic system, on which they depend, is not functional.
SH case managers expressed concerns over the web-based CCD’s functionality. For instance, a participant voiced concerns over the data being unreliable. “I have a concern if everybody is doing the input into the computer what if somebody makes a mistake and how accurate would it be.” Another case manager asked, “How often the information can be updated or is it going to be like certain websites where you go to and the information there from 2–3 years ago.”
Fit between individual and task
Case managers in both groups thought that training and instructions were critical for successful use of the systems. One participant commented, “we definitely need training as case managers.” [Web-based, SH] Another case manager recommended “setting up …a to do sheet as to how to log on, what to do, step by step.”[ePartner Report, BLH ] Case managers reflecting on each ECD summary suggested the ‘super-user’ or train- the trainer model. “Well, I think it will be the training for us… You know how to use it and maybe have someone who knows more than we do … So if it doesn’t work we can call on [that person]. It’s like, kind of a support person, you know.”[ePartner Report]
In terms of the fit between the individual and the task, case managers explained that the system would improve their work efficiency, “I think you also will give us more time because we are running around… looking for providers to give us information and sometimes they don’t even want to see case manager. [CCD]” Another case manager said, “Yeah, I think it’s going to facilitate our workload better…. Cause last week I was trying to track a client and they were sending me back and forth. At first they told me the client was not in the system and after that when I told them the doctor’s name they transferred me to another floor and they told me he doesn’t work there. [USB]” Yet, other potential users of the ePartner Report system were unsure of how this would help with their current tasks “ I really haven’t processed this thing, what it’s going to do for me, to help me with the patient.”
Fit between individual and technology
Of note, at three of the four SH focus group sites, each case manager had her own computer with Internet access. However at one site, there was only one computer for all of the case managers. Participants explained that it would make it almost impossible for them to use the web-based CCD while caring for their clients.
Finally, a participant explained the need “to make sure that it is user friendly.” Another SH case manager said, “I think to make the website as user friendly as possible for the clinicians and case managers.” Overall, participants felt very strongly that the system needed to be friendly, simple, stable and reliable.
Case managers at BLH also expressed concerns over potential technical difficulties for the e-Partner Report, “Technical difficulties always come up… no offense.” Other case managers did not think that this system would provide them with the necessary information and had a low perception of the potential usefulness of the system. For example, they thought that there was a need to include demographic information, such as emergency contacts and diagnosis for emergency visits. “Why the patient came in this time. What happened? What was the treatment? So this, there is quite a bit we are still going to need the paper charts to review. Because there is a lot we need to know so that we can set up this case for home care.”
DISCUSSION
In this paper, we applied the FITT framework to analyze the fit between individual, technology and task upon the introduction of two ECD summary systems for HIV care. The FITT framework focuses on the significance of the optimal interaction (fit) of individual user, technology, and task. In this framework, The fit between the attributes is more important than the attributes themselves. The framework provided a structured way to identify and understand case managers perceptions about adoption of the ECD summary systems prior to actual implementation and provided critical information necessary to tailor and successfully implement these systems.
Findings from this study indicate that there are commonalities regarding potential IT adoption issues across potential end-users but also differences in potential IT adoption issues depending on whether case managers were potential users of the web-based CCD group at SH or the ePartner Report system at BLH. In terms of the fit between the individual and the task, we found that case managers in the web-based CCD groups explained that the system would save them time and resources and thought the system would facilitate positive end-user responses. In contrast, some potential users of the ePartner Report system were concerned that the system would be a barrier to their workflow and in fact interrupt their current productivity. Barriers related to increased workload [32] and use of the system being time-consuming have been reported in earlier studies [33, 34]. In analyzing the fit between the individual and the technology, respondents in the web-based CCD group were more likely to be concerned about the systems’ functionality with specific concerns about data integrity. Since this system relied on data being collected from outside sources such as the insurance claims related to visits and New York State data feeds of drug refill information, it is understandable that case managers were concerned that the data may not be regularly updated or reliable.
In contrast, respondents in the ePartner Report groups were more worried about having technical difficulties. Since many of the case managers had used Eclipsys and knew that the data was already contained in an existing system, they were less concerned about data integrity and more afraid of technical difficulties. This is not surprising since they may have already encountered technical difficulties when they had used Eclipsys on earlier occasions.
The fit between individual and the task is particularly important since it is influenced by the organizational behavior that influence HIT implementation [35]. One factor which influenced the fit between individual and the task emerged from both groups. Similar to previous studies, training and technical support was elucidated as one of the most influential factors for the success of the systems implementation [36].
Interestingly, the SH case managers who were the intended end-users of the web-based CCD group made special note that a computer would be needed for each end-user in the case management agency for successful implementation of the system. This was a unique concern among some intended end-users in the web-based CCD group since there are case management agencies where there is reportedly a single computer which all case managers need to share. BLH case managers who reflected on the ePartner Report system did not express this barrier since their agencies were better equipped with computers. Therefore, this barrier is less reflective of the technology and more likely an organizational barrier due to lack of sufficient resources. This attribute is important to address prior to implementation because it is often overlooked when organizational factors are disregarded, there is often low user even user boycott.[37]
The appropriateness of the FITT framework [6] for our study purposes can be assessed by comparing it with other models. An application of the Technology Acceptance Model would have revealed the issues in fit between the individual and technology but not the fit between the task and the technology.[38] The Task-Technology Fit model would have identified issues with the fit between task and technology but not the fit between the individual and task or the individual and technology [29]. Finally the Information Systems Success model concentrates on interactions of factors like system quality, information quality and user satisfaction [27] Even so, it would not have allowed for this level of analysis since the FITT framework supported exploration of setting and technology on IT adoption [6]. Ultimately the findings from our study demonstrate how application of the FITT framework explicated aspects the fit between the individual, technology and task needed to be modified prior to implementation of the systems.
Limitations to this study include the generalizability of the findings to all case managers as well as to other settings. Since our study took place at only two settings and only included two ECD summary systems, the findings are not generalizable to all ECD summary systems. Finally, participants in our study did not see or use the actual ECD summary system and were only responding to the focus group facilitator’s description of the system.
Conclusion
Our findings provide evidence for the applicability of the FITT framework to explore case managers perceptions of factors influencing the adoption of ECD summary systems for HIV care prior to actual implementation. Assessment of fit among individual, task, and technology and addressing the concerns identified prior to implementation is critical to successful adoption of HIT as a strategy to improve quality and efficiency in health care.
Summary points.
What is already known on the topic?
ECD summaries have become a key strategy in supporting patient care by promoting the use of electronic information to transfer critical health information between patients and their providers
Understanding HIT project implementation characteristics is critical for understanding determinants of success
What this study added to our knowledge?
Training and technical support was elucidated as one of the most influential factors for the success of the systems’ implementation
Perceptions about factors influencing adoption of HIT are common across systems
The FITT framework is a useful model to identify and understand perceived barriers and facilitators to system implementation and explain the potential reasons for its success.
Highlights.
The FITT framework is a useful model to identify and understand perceived barriers and facilitators to system implementation and explain the potential reasons for its success
Training and technical support was elucidated as one of the most influential factors for the success of the systems’ implementation
Perceptions about factors influencing adoption of HIT are common across systems
Acknowledgments
The authors would like to acknowledge the case managers who participated in the focus groups. In addition, we would like to thank Michelle Odlum, Martha Rodriguez and Esmerlin Valdez who assisted in organizing and conducting the project and evaluation.
Support for this research was provided by H97HA08481 (Tim Kanter, Principal Investigator, H97HA08483 (Peter Gordon, Principal Investigator), and P30NR010677 (Suzanne Bakken, Principal Investigator).
Footnotes
Authors’ contributions
Rebecca Schnall, RN, PhD, 1a) the conception and design of the study; (1b) acquisition of data; (1c) analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Ann B. Smith, MPH, 1a) the conception and design of the study; (1b) acquisition of data; (1c) analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Manik Sikka, MBA (1b) acquisition of data; (1c) analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Peter Gordon, MD: (1b) acquisition of data; (1c) analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Eli Camhi, MSSW: (1b) acquisition of data; (1c) analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Tim Kanter, MD: (1b) acquisition of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Suzanne Bakken, RN, DNSc: (1a) the conception and design of the study (Evaluation Director); (1b) acquisition of data; (1c) analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Conflict of interest statement
None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Indyk D, Belville R, Lachapelle S, Gordon G, Dewart T. A community-based approach to HIV case management: systematizing the unmanageable. Soc Work. 1993;38(4):380–7. [PubMed] [Google Scholar]
- 2.Rodriguez HP, Marsden PV, Landon BE, Wilson IB, Cleary PD. The effect of care team composition on the quality of HIV care. Med Care Res Rev. 2008;65(1):88–113. doi: 10.1177/1077558707310258. [DOI] [PubMed] [Google Scholar]
- 3.Hecht FM, Wilson IB, Wu AW, Cook RL, Turner BJ. Optimizing care for persons with HIV infection. Society of General Internal Medicine AIDS Task Force. Ann Intern Med. 1999;131(2):136–43. doi: 10.7326/0003-4819-131-2-199907200-00011. [DOI] [PubMed] [Google Scholar]
- 4.Wright J, Henry SB, Holzemer WL, Falknor P. Evaluation of community-based nurse case management activities for symptomatic HIV/AIDS clients. J Assoc Nurses AIDS Care. 1993;4(2):37–47. [PubMed] [Google Scholar]
- 5.Institute of Medicine. Patient Safety: Achieving a New Standard for Care. Washington, DC: 2003. Contract No.: Document Number|. [Google Scholar]
- 6.Ammenwerth E, Iller C, Mahler C. IT-adoption and the interaction of task, technology and individuals: a fit framework and a case study. BMC Med Inform Decis Mak. 2006;6:3. doi: 10.1186/1472-6947-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kibbe DC, Phillips RL, Jr, Green LA. The continuity of care record. Am Fam Physician. 2004;70(7):1220, 2–3. [PubMed] [Google Scholar]
- 8.Office of the National Coordinator for Health Information Technology. Defining Key Health Information Technology Terms: Department of Health and Human Services. 2008. Contract No.: Document Number|. [Google Scholar]
- 9.Johnson TR, Tang X, Graham MJ, Brixey J, Turley JP, Zhang J, et al. Attitudes toward medical device use errors and the prevention of adverse events. Jt Comm J Qual Patient Saf. 2007;33(11):689–94. doi: 10.1016/s1553-7250(07)33079-1. [DOI] [PubMed] [Google Scholar]
- 10.Norman DA. User Centered System Design: New Perspectives on Human-computer Interaction. Hillsdale, NJ: Lawrence Erlbaum Associates; 1986. [Google Scholar]
- 11.Adler-Milstein J, Bates DW, Jha AK. A Survey of Health Information Exchange Organizations in the United States: Implications for Meaningful Use. Annals of Internal Medicine. 2011;154(10):666–71. doi: 10.7326/0003-4819-154-10-201105170-00006. [DOI] [PubMed] [Google Scholar]
- 12.The Office of the National Coordinator for Health Information Technology. The Nationwide Health Information Network, Direct Project, and CONNECT Software. Washington, DC: US Department of Health and Human Services; 2011. [updated 2011; cited 2012 June 11]; Available from: http://healthit.hhs.gov/portal/server.pt?open=512&mode=2&objID=3340. [Google Scholar]
- 13.Health Level Seven International. HL7 Standards - Section 4: EHR Profiles. Ann Arbor, MI: 2012. [updated 2012; cited 2012 February 29]; Available from: http://www.hl7.org/implement/standards/product_section.cfm?section=4. [Google Scholar]
- 14.Arzt NH. Clinical Summaries and Meaningful Use. J Healthc Inf Manag. 2011;25(1):62–9. [Google Scholar]
- 15.Cesta A, Bajcar JM, Ong SW, Fernandes OA. The EMITT study: development and evaluation of a medication information transfer tool. Ann Pharmacother. 2006;40(6):1074–81. doi: 10.1345/aph.1G707. [DOI] [PubMed] [Google Scholar]
- 16.Siika AM, Rotich JK, Simiyu CJ, Kigotho EM, Smith FE, Sidle JE, et al. An electronic medical record system for ambulatory care of HIV-infected patients in Kenya. Int J Med Inform. 2005;74(5):345–55. doi: 10.1016/j.ijmedinf.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Grossberg R, Gross R. Use of pharmacy refill data as a measure of antiretroviral adherence. Current HIV/AIDS Reports. 2007;4(4):187–91. doi: 10.1007/s11904-007-0027-4. [DOI] [PubMed] [Google Scholar]
- 18.HIMSS. Electronic Health Record. Chicago, IL: 2012. [updated 2012; cited 2012 February 29]; Available from: http://www.himss.org/ASP/topics_ehr.asp. [Google Scholar]
- 19.ASTM WK4363. Draft Standard Specification for the Continuity of Care Record, Version 1. ASTM International; 2004. [Google Scholar]
- 20.ASTM E31.28. E- Standard Specification for Continuity of Care Record (CCR) ASTM International; 2005. [Google Scholar]
- 21.Jerant AF, Hill DB. Does the use of electronic medical records improve surrogate patient outcomes in outpatient settings? J Fam Pract. 2000;49(4):349–57. [PubMed] [Google Scholar]
- 22.Tsiknakis M, Kouroubali A. Organizational factors affecting successful adoption of innovative eHealth services: a case study employing the FITT framework. Int J Med Inform. 2009;78(1):39–52. doi: 10.1016/j.ijmedinf.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 23.Berg M. Implementing information systems in health care organizations: myths and challenges. Int J Med Inform. 2001;64(2–3):143–56. doi: 10.1016/s1386-5056(01)00200-3. [DOI] [PubMed] [Google Scholar]
- 24.May C, Ellis NT. When protocols fail: technical evaluation, biomedical knowledge, and the social production of facts about a telemedicine clinic. Social Science & Medicine. 2001;53(8):989–1002. doi: 10.1016/s0277-9536(00)00394-4. [DOI] [PubMed] [Google Scholar]
- 25.Honekamp W, Ostermann H. Evaluation of a prototype health information system using the FITT framework. Inform Prim Care. 2011;19(1):47–9. doi: 10.14236/jhi.v19i1.793. [DOI] [PubMed] [Google Scholar]
- 26.Davis FD. User acceptance of information technology: system characteristics, user perceptions and behavioral impacts. International Journal of Man-Machine Studies. 1993;38(3):475–87. [Google Scholar]
- 27.DeLone W, McLean E. Information systems success: the quest for the dependent variable. Inform Systems Res. 1992;3(1):60–95. [Google Scholar]
- 28.Dixon DR. The behavioral side of information technology. International journal of medical informatics. 1999;56(1–3):117–23. doi: 10.1016/s1386-5056(99)00037-4. [DOI] [PubMed] [Google Scholar]
- 29.Goodhue DL, Klein BD, March ST. User evaluations of IS as surrogates for objective performance. Information & Management. 2000;38(2):87–101. [Google Scholar]
- 30.Green LW, Kreuter MW. Health program planning: An educational and ecological approach. 4. Boston: McGraw Hill; 2005. [Google Scholar]
- 31.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004;24(2):105–12. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 32.Yasunaga H, Imamura T, Yamaki S, Endo H. Computerizing medical records in Japan. Int J Med Inform. 2008;77(10):708–13. doi: 10.1016/j.ijmedinf.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 33.Likourezos A, Chalfin DB, Murphy DG, Sommer B, Darcy K, Davidson SJ. Physician and nurse satisfaction with an Electronic Medical Record system. J Emerg Med. 2004;27(4):419–24. doi: 10.1016/j.jemermed.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 34.Randeree E. Exploring physician adoption of EMRs: a multi-case analysis. J Med Syst. 2007;31(6):489–96. doi: 10.1007/s10916-007-9089-5. [DOI] [PubMed] [Google Scholar]
- 35.Lesselroth BJ, Yang J, McConnachie J, Brenk T, Winterbottom L. Addressing the sociotechnical drivers of quality improvement: a case study of post-operative DVT prophylaxis computerised decision support. BMJ Qual Saf. 2011;20(5):381–9. doi: 10.1136/bmjqs.2010.042689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McGinn CA, Grenier S, Duplantie J, Shaw N, Sicotte C, Mathieu L, et al. Comparison of user groups’ perspectives of barriers and facilitators to implementing electronic health records: a systematic review. BMC Med. 2011;9:46. doi: 10.1186/1741-7015-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chau PYK, Hu PJ-H. Investigating healthcare professionals’ decisions to accept telemedicine technology: an empirical test of competing theories. Information & Management. 2002;39(4):297–311. [Google Scholar]
- 38.Davis F, Bagozzi R, Warshaw P. User acceptance of computer technology: a comparison of two theoretical models. Management Science. 1989;35(8):982–1003. [Google Scholar]


