Summary
A 62-year-old man with a traumatic high-flow right carotid-cavernous fistula was treated by transarterial balloon occlusion technique. However, because of the relatively small size of the fistula, the balloon could not enter into the cavernous sinus via the fistula. During the procedure, the shunt flow decreased significantly, and we stopped the procedure. Follow-up angiography performed 14 days after the procedure showed complete occlusion of the fistula with a small residual pseudoaneurysm. One year later, the pseudoaneurysm had decreased in size. Repeated transient decrease and stagnancy of blood flow at the fistula during the balloon procedure may have played an important role in the thrombosis in this patient.
Key words: carotid-cavernous fistula, detachable balloon, spontaneous thrombosis, endovascular therapy, cerebral angiography
Introduction
The direct type of high-flow carotid-cavernous fistula (CCF) is traditionaly treated by transarterial detachable balloon occlusion technique 1,2. Recently, Guglielmi detachable coils (GDCs) were used for the treatment of direct CCF 3,4. The transvenous approach can also be used when the transarterial approach is unsuccessful 5,6. Direct CCF rarely closes spontaneously 7,8, and low-flow direct CCF is sometimes treatable by self-compression of the common carotid artery 9. We experienced a case of high-flow CCF that thrombosed spontaneously after failure of transarterial balloon occlusion technique.
Case Report
A 62-year-old man suffered a traffic accident resulting in multiple facial bone fractures. Five days after the accident, right abducens nerve palsy developed that caused double vision. Right chemosis, exophthalmos, and orbital bruit also developed gradually. Magnetic resonance images obtained 43 days after the head trauma showed right-side dominant bilateral chronic subdural hematomas with dilated right cavernous sinus and superior ophthalmic vein, indicative of the presence of a CCF. Subsequently, selective cerebral angiography was performed, and right high-flow direct CCF was confirmed (figure 1). Simultaneously performed balloon occlusion Matas test was positive (i.e., intolerable). Six days later, transarterial occlusion of the fistula with a detachable balloon was attempted under systemic heparinization through a 9F guiding catheter.
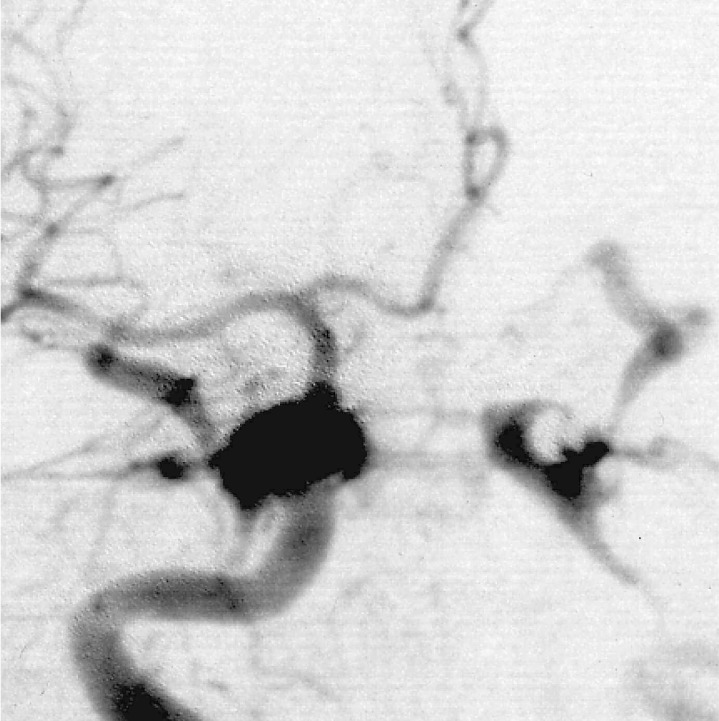
Figure 1.
Anteroposterior projection of selective right internal carotid arteriography shows a high-flow direct carotidcavernous fistula. The anterior cerebral arteries are compressed to the left by the right subdural haematoma.
The slightly inflated balloon (#9 Goldvalve, Nycomed, Paris, France) seated in the orifice many times but never entered the cavernous sinus via the fistula because the fistula was relatively small. During the procedure, blood flow in the internal carotid artery (ICA) decreased because of the large size of the guiding catheter and catheterization-related vasospasm, and we found that the shunt flow decreased significantly (figure 2). Therefore, we stopped the procedure. Over the following days, the orbital bruit disappeared, and right chemosis and exophthalmos improved. Follow-up angiography performed 14 days after the procedure showed occlusion of the fistula with a small residual pseudoaneurysm (figure 3). The size of the pseudoaneurysm had decreased one year later (figure 4). There is no evidence of recurrence of the CCF at three years after the procedure.
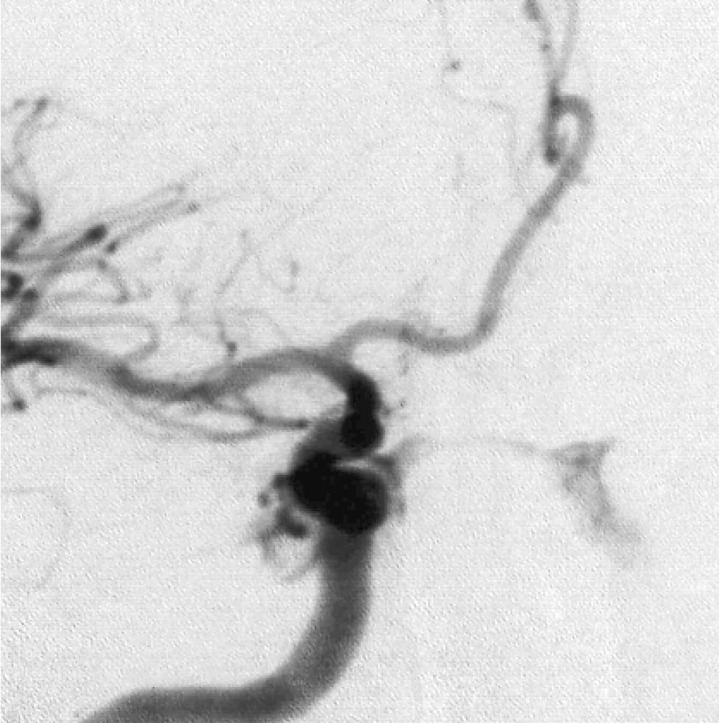
Figure 2.
Anteroposterior projection of selective right internal carotid arteriography during transarterial balloon occlusion shows significant decrease of the shunt flow.
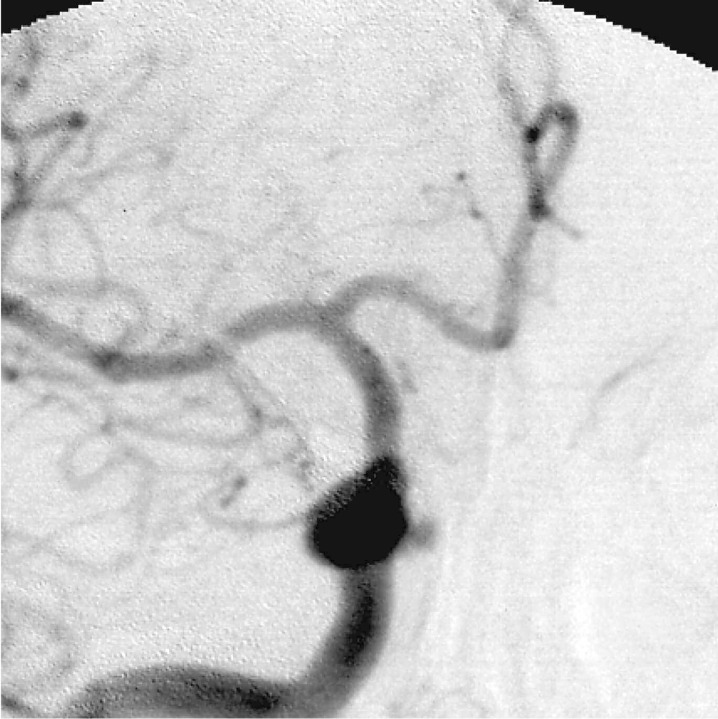
Figure 3.
Anteroposterior projection of right common carotid arteriography performed 14 days after the balloon occlusion procedure shows occlusion of the fistula and a small residual pseudoaneurysm at the medial wall of the cavernous internal carotid artery.
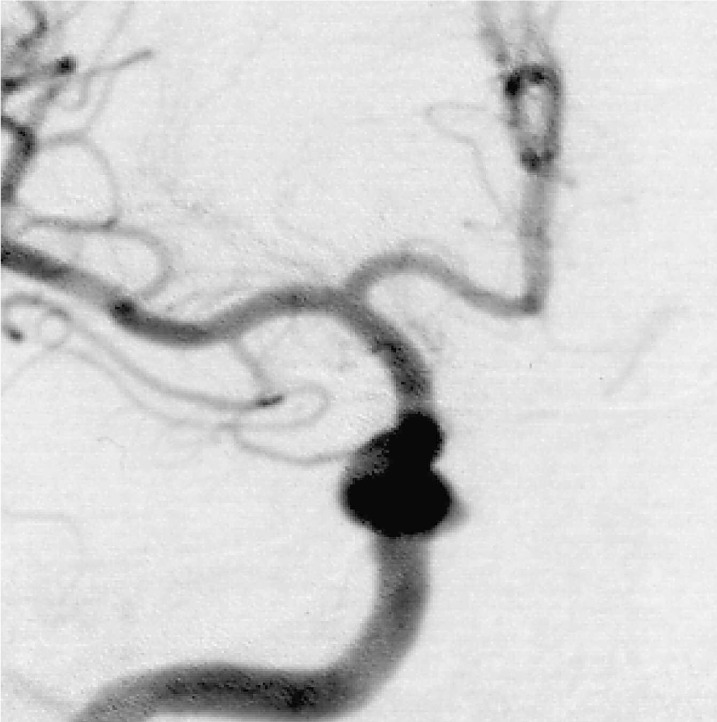
Figure 4.
Anteroposterior projection of right common carotid arteriography performed approximately one year after the procedure shows the residual pseudoaneurysm has decreased in size.
Discussion
According to Barrow et Al 10, CCF is classified into four types: type A involves a direct shunt between the intracavernous ICA and the cavernous sinus (CS); types B, C, and D involve indirect transdural shunts between the CS and dural branches of the ICA, external carotid artery or both. The majority of type A (direct) CCFs occur as a rare complication of head injury with basal skull fracture, and a minority occur because of rupture of an intracavernous ICA aneurysm, resulting in a high-flow shunt 11. Another risk factor for direct CCF is connective tissue disorders 12. Spontaneous dissection is also a rare cause of direct CCF 13. In the present patient, the CCF was caused by trauma. Rupture of a preexisting small aneurysm, triggered by the rupture caused by the trauma, may also have occurred. However, the small aneurysm decreased in size one year later, indicating that it was not a true aneurysm but a pseudoaneurysm 14.
Endovascular closure is the treatment of choice in direct CCF. Endovascular balloon occlusion was first described by Serbinenko 1 and popularized by Debrun et Al 2. Usually, a transarterial approach is attempted. If it fails, a transvenous approach is the alternative 5. Recently, GDCs have been used for the treatment of direct CCF via both the transarterial and transvenous approaches 4. Even though a fistula is small in caliber, it can be treated with GDCs because it is technically easier to guide a microcatheter and microguidewire combination through a small fistula than it is to guide a balloon 3. Thus, in hindsight, we should have used GDCs rather than a balloon to treat the direct CCF in our patient.
Direct CCFs sometimes thrombose spontaneously 7,8. Mechanisms thought to be responsible for the spontaneous thrombosis of direct CCF are slow flow due to ICA dissection leading to venostasis and damage to the vascular lining of the CS caused by venous hypertension 8. Nishijima et Al 7 reported a case of spontaneously healed direct CCF immediately after orbital venography and speculated that a temporary decrease in the pressure gradient between the cavernous sinus and the ICA caused formation of a thrombus. Spinnato et Al 9 reported a case of a direct slow-flow CCF successfully treated by self-compression of the common carotid artery. Compression induces simultaneous arterial hypotension and venous hypertension, which result in a transient decrease of the pressure gradient across the shunt, thus promoting thrombosis. The present patient had a high-flow shunt, but the blood flow in the ICA decreased during the intraarterial procedure because we used a 9F guiding catheter and because of vasospasm related to the catheterization.
Moreover, the slightly inflated balloon seated in the orifice of the fistula many times, resulting in intermittent occlusion of the fistula. These transient reductions in blood flow and the resulting stagnancy may have played an important role in the thrombosis of the CCF in the present patient. Thus, had it been performed, self-compression of the common carotid artery, which produces a similar reduction in blood flow, might also have been useful for the treatment of the direct CCF in the present patient. Another explanation of spontaneous thrombosis in this patient may be that the injection of iodinated contrast media exaggerated leukocytic accumulation, promoted red blood cell aggregation, and directly affected the vascular endothelium 8.
Conclusions
Repeat transient decrease and stagnancy of blood flow at the fistula may have played an important role in the thrombosis of the CCF in the present patient. Thus, we suggest that temporary occlusion of the orifice of the CCF with a balloon may produce permanent thrombosis of the fistula. For a similar reason, self-compression of the common carotid artery may possibly be useful for the treatment of the direct CCF with a relatively small fistula. If endovascular therapy is considered, GDCs appear to be a better choice than are balloons for the treatment of a direct CCF.
References
- 1.Serbinenko FA. Balloon catheterization and occlusion of major cerebral vessels. J Neurosurg. 1974;41:125–145. doi: 10.3171/jns.1974.41.2.0125. [DOI] [PubMed] [Google Scholar]
- 2.Debrun G, Lacour P, et al. Treatment of 54 traumatic carotid-cavernous fistulas. J Neurosurg. 1981;55:678–692. doi: 10.3171/jns.1981.55.5.0678. [DOI] [PubMed] [Google Scholar]
- 3.Guglielmi G, Viñuela F, et al. High-flow, small-hole arteriovenous fistulas: treatment with electrodetachable coils. Am J Neuroradiol. 1995;16:325–328. [PMC free article] [PubMed] [Google Scholar]
- 4.Bavinzski G, Killer M, et al. Treatment of post-traumatic carotico-cavernous fistulae using electrolytically detachable coils: technical aspects and preliminary experience. Neuroradiology. 1997;39:81–85. doi: 10.1007/s002340050371. [DOI] [PubMed] [Google Scholar]
- 5.Halbach VV, Higashida RT, et al. Transvenous embolization of direct carotid cavernous fistulas. Am J Neuroradiol. 1988;9:741–747. [PMC free article] [PubMed] [Google Scholar]
- 6.Chun GF, Tomsick TA. Transvenous embolization of a direct carotid cavernous fistula through the pterygoid plexus. Am J Neuroradiol. 2002;23:1156–1159. [PMC free article] [PubMed] [Google Scholar]
- 7.Nishijima M, Iwai R, et al. Spontaneous occlusion of traumatic carotid cavernous fistula after orbital venography. Surg Neurol. 1985;23:489–492. doi: 10.1016/0090-3019(85)90244-7. [DOI] [PubMed] [Google Scholar]
- 8.Castillo M, Silverstein M, et al. Spontaneous thrombosis of a direct carotid cavernous sinus fistula: confirmation by Gd-DTPA-enhanced MR. Am J Neuroradiol. 1989;10:S75–S76. [PMC free article] [PubMed] [Google Scholar]
- 9.Spinnato S, Talacchi A, et al. Conservative treatment of a traumatic direct low-flow carotid-cavernous sinus fistula: a case report. Acta Neurochir (Wien) 1997;139:1181–1184. doi: 10.1007/BF01410980. [DOI] [PubMed] [Google Scholar]
- 10.Barrow DL, Spector RH, et al. Classification and treatment of spontaneous carotid-cavernous fistulas. J Neurosurg. 1985;62:284–256. doi: 10.3171/jns.1985.62.2.0248. [DOI] [PubMed] [Google Scholar]
- 11.Kobayashi N, Miyachi S, et al. Endovascular treatment strategy for direct carotid-cavernous fistulas resulting from rupture of intracavernous carotid aneurysms. Am J Neuroradiol. 2003;24:1789–1796. [PMC free article] [PubMed] [Google Scholar]
- 12.Forlodou P, de Kersaint-Gilly A, et al. Ehlers-Danlos syndrome with a spontaneous caroticocavernous fistula occluded by detachable balloon: case report and review of the literature. Neuroradiology. 1996;38:595–597. doi: 10.1007/BF00626107. [DOI] [PubMed] [Google Scholar]
- 13.Bradac GB, Bender A, et al. Report of two cases of spontaneous direct carotid-cavernous fistula. Diagnostic and therapeutic considerations. Neuroradiology. 1985;27:436–439. doi: 10.1007/BF00327610. [DOI] [PubMed] [Google Scholar]
- 14.Mori S, Feliciani M, et al. Regression of an internal carotid artery pseudoaneurysm after therapeutic embolization of a post-traumatic carotid-cavernous fistula secondary to gunshot injury. Neuroradiology. 1990;32:226–228. doi: 10.1007/BF00589117. [DOI] [PubMed] [Google Scholar]