Summary
Internal maxillary arterial or branch transection is a potential complication of maxillofacial surgery. We describe one such patient who developed acute massive nasal haemorrhage, an episode of which was controlled clinically just prior to performing endovascular embolization by employing the simple but effective clinical manoeuvre of manual carotid arterial compression. Six weeks later the haemorrhage recurred despite a seemingly adequate embolization of the affected arteries with microcoils and Spongistan due to re-establishment of flow through the coils.
Key words: epistaxis, iatrogenic pseudoaneurysm, maxillary artery
Case Report
An 18-year-old male had undergone a bi-maxillary osteotomy to correct an overbite. No immediate postoperative complications were encountered. Six weeks later he developed an acute massive right-sided epistaxis. He was resuscitated and transfused with 4 units of whole blood whilst being transferred by ambulance to our unit for arteriography and possible embolization. He remained stable during the three-hour journey, but shortly after arrival in our hospital developed another massive haemorrhage. One of the authors went immediately to the ward and applied external compression to the right common carotid artery to control the haemorrhage. This compression was maintained until the patient began to loose consciousness and was then released until he recovered whereupon the compression was reapplied. In the meantime the interventional theatre was cleared and prepared for the patient's arrival. Assisted by the carotid compression the bleeding stopped long enough to allow administration of an anaesthetic and endotracheal intubation. Direct selective catheterization of the right external carotid artery was then performed using a 5F Headhunter Type I catheter (Glidecath, Terumo Corporation, Tokyo). External carotid arteriography demonstrated the presence of a large pseudoaneurysm filling from the distal right internal maxillary artery (IMAX).
A Renegade microcatheter (Target Therapeutics/Boston Scientific Corporation, Fremont, CA) was placed through the diagnostic catheter over a Transcend Soft-tip 0,014" microwire (Target Therapeutics) into the distal IMAX which was then occluded with six fibered platinum microcoils (Target Therapeutics). A small quantity of Spongistan (Cordis Johnson and Johnson, Miami, FL) was also injected into the distal IMAX through the Headhunter catheter after removal of the microcatheter. Check arteriography of the contralateral external carotid artery showed no filling of the pseudoaneurysm via any collateral arteries. No further bleeding was encountered and the patient was discharged three days later.
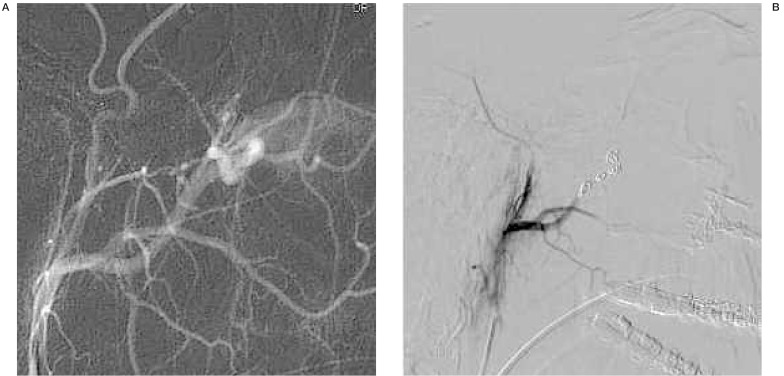
Figure 1.
A) Selective right external carotid digital subtraction arteriogram, lateral projection, showing filling of a large pseudoaneurysm from the distal IMAX. B) Selective external carotid arteriogram following occlusion of the distal IMAX with coils and Spogistan.
Six weeks later he presented again with another acute massive right sided epistaxis. He was transferred back to our hospital by helicopter whereupon an urgent arteriogram was repeated under general anaesthesia. A selective right external carotid arteriogram showed recurrent filling of the pseudoaneurysm through the right IMAX and through the previously deposited microcoils. One of the microcoils had displaced distally into the pseudoaneurysm lumen whereas the other five were still in-situ in the distal IMAX as placed previously. Selective catheterization of the IMAX was performed through the coils and the artery re-embolized with another single microcoil and with cyanoacrylate (Histoacryl, B.Braun, Helsungen, Germany). Again no filling of the pseudoaneurysm was confirmed from collateral arteries prior to terminating the procedure. No further bleeding occurred and the patient was discharged again several days later.
A follow-up arteriogram was performed six weeks later which now showed occlusion of the distal IMAX and its terminal branches and no filling of the pseudoaneurysm. The patient has remained clinically well to date (21 months) with no further epistaxis.
Discussion
Vascular injuries during craniofacial surgery are uncommon but well described complications 1,2. Embolization of traumatized craniofacial vessels is also a well-recognized method of treatment 3-6. The purpose of this report is to emphasize two points related to this case: firstly the life-saving manoeuvre of direct carotid compression, and secondly recanalization of an artery originally thought to be adequately embolized with fibered platinum microcoils in the absence of any thrombolytic or antiplatelet agents being used.
Compression of a blood vessel either by direct pressure of by means of a tourniquet is a standard accepted practice for the control of bleeding in trauma and surgery. Current wisdom holds that direct pressure applied to the bleeding site is preferable to more proximal occlusion of a vessel. However, there are some areas of the body where direct pressure cannot be applied in order to control acute bleeding, and upstream vessel occlusion then becomes essential. This is particularly true of the head and neck region where many vital vascular structures are hidden by the facial skeleton and skull base. Embolization of traumatized craniofacial vessels is in many instances the preferred first-line method of treatment 5.
The performance of such procedures requires that the patients be stabilized as fast as possible before transfer to the interventional unit. In many instances immediate surgical back-up may not be available when a sudden catastrophic haemorrhage in the head and neck region occurs, and the interventionalist may be left to his or her own devices as how best to control such a situation. Based on our own experience our first priority when faced with any situation involving haemorrhage in the head and neck region is airway protection, regardless of whether acute bleeding is present or not. All such patients are anaesthetized and intubated in our unit prior to any angiographic and interventional procedure.
Acute massive haemorrhage can occur at any stage before adequate endovascular control can be achieved. Extracorporeal carotid compression can thus buy valuable time whilst preparing a patient for anaesthesia and intervention. Obviously a major potential complication of carotid compression is stroke and care must be taken to re-establish temporary flow through the internal carotid artery from time to time (e.g. releasing the pressure every two to three minutes for several seconds) as the situation allows.
Platinum microcoils are available form a number of sources. Although the platinum itself is thrombotic, the addition of Dacron fibres enhances their thrombogenicity 7,8 as with their larger stainless steel (Gianturco) counterparts 9,10. When adequate packing of a vessel with coils has been achieved, the vessel generally remains occluded, although flow may become re-established through the coils in either a high-flow situation (as in an arteriovenous fistula) or due to the use of anticoagulants or thrombolytics 6,11. Our patient was never given thrombolytic agents, and did not use antiplatelet agents or drugs such as non-steroidal anti-inflammatory agents (with anti-platelet properties) at any stage after the first embolization.
We have never before seen such late re-establishment of flow through coils other than in a high-flow situation. We deemed the initial embolization with coil packing and Spogistan in the distal IMAX during the first procedure to be quite adequate and can only conclude that denser packing of the coils together into a focal nest during the first procedure may have proven more efficacious although the pattern of coil placement that was used had never failed before.
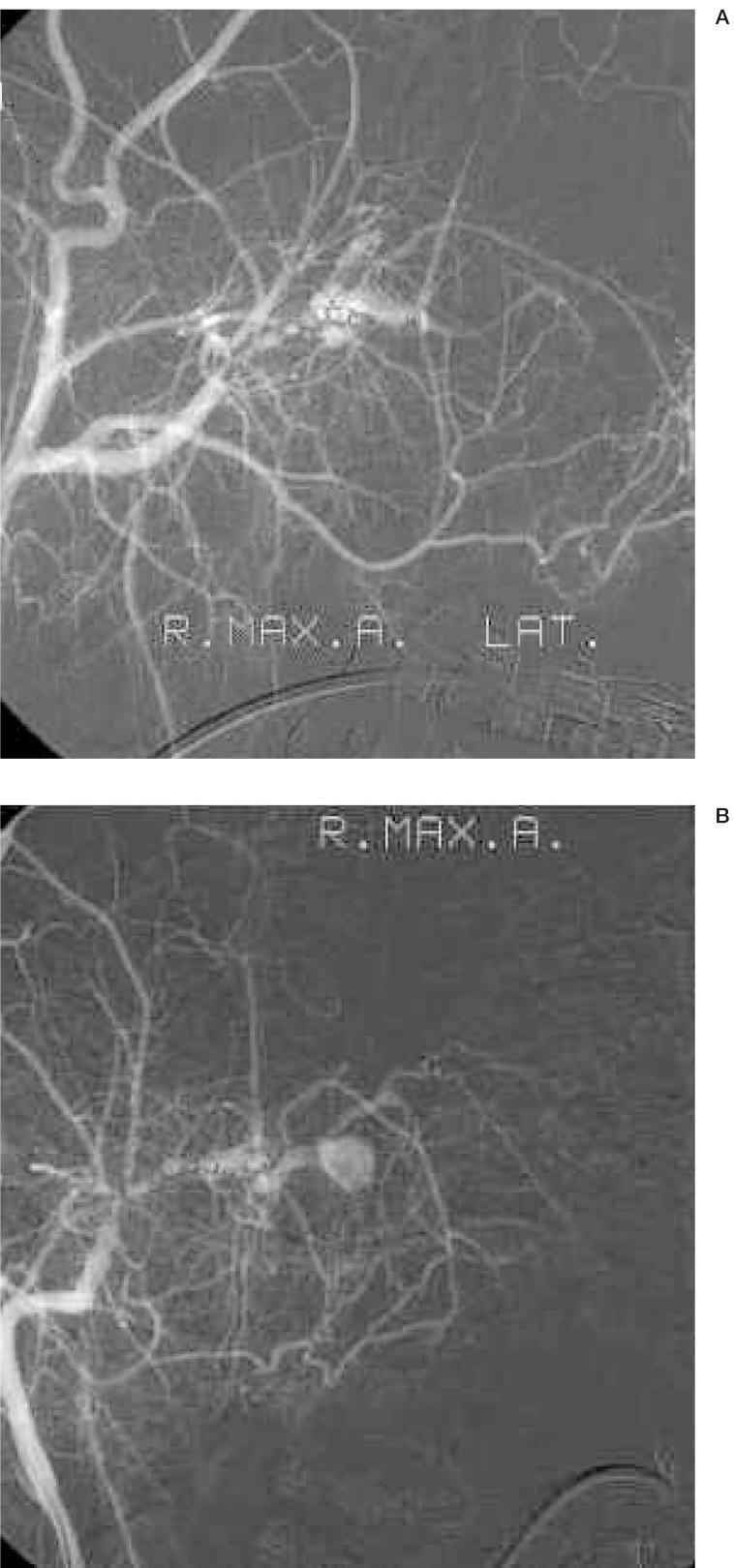
Figure 2.
A) Selective external carotid digital subtraction arteriogram, lateral projection, performed six weeks after recurrence of the epistaxis, showing flow of contrast through the coils with refilling of the pseudoaneurysm. B) Same study, frontal projection, showing contrast flowing through the coils in the distal IMAX.
In conclusion, two valuable lessons were learnt form this case. Firstly the technique of extracorporeal carotid compression when faced with severe uncontrollable haemorrhage in the head and neck region arising from trauma to the carotid arteries on their main branches can buy time during resuscitation and prior to any definitive treatment, be it surgical or endovascular intervention. Secondly, although uncommon, the potential exists for the recanalization of a vessel thought to be adequately occluded by metallic coils, which should always be considered in any setting of recurrence of haemorrhage from a vessel or lesion previously embolized with coils.
References
- 1.Bradley JP, Elahi M, Kawamoto HK. Delayed presentation of pseudoaneurysm after Le Fort I osteotomy. J Craniofacial Surg. 2002;13:746–750. doi: 10.1097/00001665-200211000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Panula K, Finne K, Oikarinen K. Incidence of complication and problems related to orthognathic surgery: A review of 655 patients. J Oral Maxillofacial Surg. 2001;59:1128–1136. doi: 10.1053/joms.2001.26704. [DOI] [PubMed] [Google Scholar]
- 3.Zachariades N, Rallis G, et al. Embolization for the treatment of pseudoaneurysm and transection of facial vessels. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:491–494. doi: 10.1067/moe.2001.117453. [DOI] [PubMed] [Google Scholar]
- 4.Kagetsu NJ, Berenstein A, Choi IS. Interventional radiology of the extracranial head and neck. Cardiovasc Interv Radiol. 1991;14:325–333. doi: 10.1007/BF02577890. [DOI] [PubMed] [Google Scholar]
- 5.Gittleman A, Oritz AO, et al. Emergency Endovascular Interventions of Traumatic Cranial and Extracranial Injuries. Semin Intervent Radiol. 2003;20:151–167. [Google Scholar]
- 6.Connors JJ, Wojak JC. Arteriovenous fistulae and traumatic vascular lesions. In: Connors JJ, Wojak JC, editors. Interventional Neuroradiology: Strategies and practical techniques. Philadelphia: WB Saunders Co; 1999. pp. 160–179. [Google Scholar]
- 7.Yang PJ, Halbach VV, et al. Platinum wire: a new transvascular embolic agent. Am J Neuroradiol. 1988;9:547–550. [PMC free article] [PubMed] [Google Scholar]
- 8.Hilal SK, Khandji AG, et al. Synthetic fiber-coated platinum coils successfully used for endovascular treatment of arteriovenous malformation, aneurysm and direct arteriovenous fistulas of CNS (abstract) Am J Neuroradiol. 1988;9:1030. [Google Scholar]
- 9.Gianturco C, Anderson JH, Wallace S. Mechanical devices for arterial occlusion. Am J Roentgenol. 1975;124:428–435. doi: 10.2214/ajr.124.3.428. [DOI] [PubMed] [Google Scholar]
- 10.Wallace S, Gianturco C, et al. Therapeutic vascular occlusion utilizing steel coil technique: Clinical applications. Am J Roentgenol. 1977;129:795–798. doi: 10.2214/ajr.127.3.381. [DOI] [PubMed] [Google Scholar]
- 11.Young AT, Murthy Tadavarthy S, et al. Vascular embolotherapy. In: Castañeda-Zúñiga WR, Murthy Tadavarthy S, editors. Interventional Radiology. Baltimore: Williams and Wilkins; 1992. pp. 9–73. [Google Scholar]