Summary
We report a case of dural arteriovenous fistula (DAVF) within the left hypoglossal canal in a 64-year-old man who presented with tinnitus and ocular symptoms. Angiography revealed DAVF with the fistulous pouch medial to the left jugular bulb. The fistula was feeded by meningeal branches of the bilateral ascending pharyngeal arteries and the branches from the left vertebral artery. The fistula shunted into the left jugular bulb, with reflux into the left inferior petrosal (IPS) and cavernous sinuses (Cses), left superior ophthalmic vein (SOV) and cortical veins over the cerebral convexity. We performed transvenous coil embolization to occlude the fistula resulting in complete resolution of symptoms and signs.
Key words: arteriovenous fistula, transvenous embolization, hypoglossal canal
Introduction
Intracranial dural arteriovenous fistulas (DAVFs) are recognized as an abnormal channel from the artery(s) to the vein within the dura mater. Although the majority of DAVFs in the posterior fossa involve the transverse or sigmoid sinus, they must be observed in any portions of the dural structure. The symptoms relate to venous drainage and arterial phenomenon. We report a case who presented tinnitus and ocular symptoms due to a DAVF located in the left hypoglossal canal. The fistula was treated successfully by transvenous coil embolization.
Case Report
A 64-year-old man had complained of audible pulse-synchronous bruit around the left ear for a month. The patient revealed diplopia, bilateral exophthalmos and chemosis. Magnetic resonance imaging (MRI) revealed a signal void lesion within the left hypoglossal canal (figure 1).
Figure 1.
Axial contrast-enhanced Tl-weighted image reveals abnormal flow void in the left hypoglossal canal.
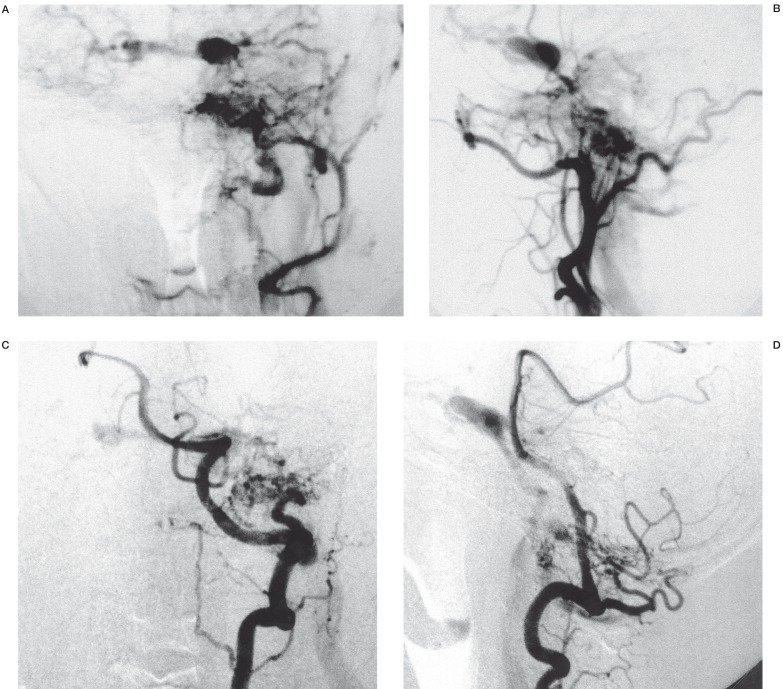
The angiography showed a DAVF with a fistulous pouch located inferomedial to the left jugular bulb. The DAVF was fed by meningeal branches of the bilateral ascending pharyngeal arteries and the arterial branches from the left vertebral artery (figure 2). The fistula drained through the left IPS and left CS into the left SOV and ipsilateral cortical veins over the cerebral convexity, and the contralateral CS (figure 2).
Figure 2.
Anteroposterior (A) and lateral projection (B) of Left external carotid arteriogram. Anteroposterior (C) and lateral projection (D) of left VA arteriogram. DAVF was supplied by meningeal branches of the left ascending pharyngeal artery and vertebral artery and drained the left internal jugular veins and IPS, then to the bilateral CS and cortical veins.
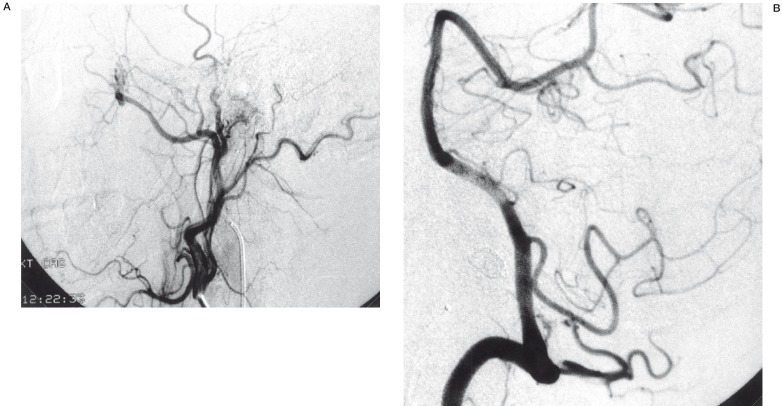
Transvenous coil embolization was tried to obliterate the fistula. Through a guiding catheter positioned in the left jugular vein, a microcatheter (Turbotracker 18, Boston Scientific) was advanced over a guidewire (0.016-in, GT wire, Terumo Co Ltd, Tokyo, Japan) into the fistulous pouch (figure 3). After placing one detachable coil (5 mm X 20 cm) (IDC-18; Boston Scientific) into the venous pouch, angiograms confirmed complete obliteration of the pouch and disappearance of venous drainage through the left IPS (figure 4).
Figure 3.
A microcatheter was advanced into the fistulous pouch inferomedial to the left jugular bulb.
Figure 4.
A) Lateral projection of left external carotid arteriogram. B) Lateral projection of left vertebral arteriogram. Immediately after endovascular treatment, both angiographys showed the disappearance of retrograde venous drainage and definite fistula.
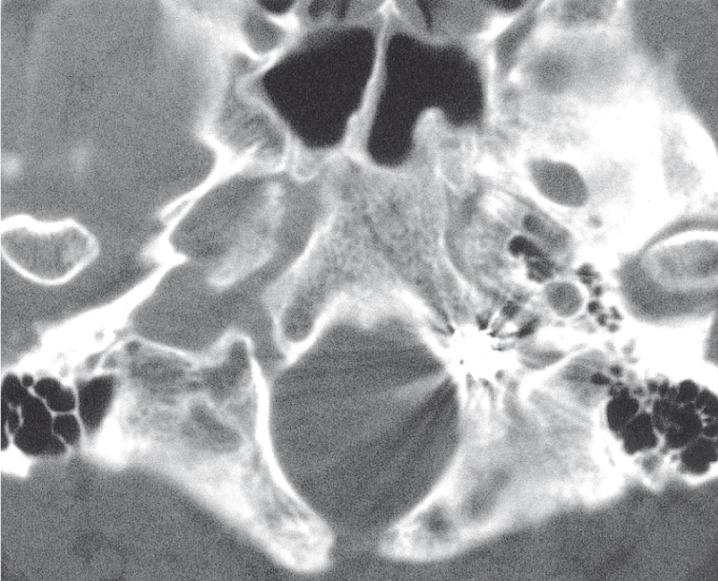
The patient reported the disappearance of bruit immediately after the endovascular treatment. The ocular symptoms were resolved gradually and completely by one month after coil embolization. Computerized tomography (CT) scan demonstrated a mass of coil within the left hypoglossal canal (figure 5). Follow-up angiograms one month after the endovascular treatment showed no recurrence of the arteriovenous fistula.
Figure 5.
CT scan following transvenous coil embolization shows a coil mass within the left hypoglossal canal.
Discussion
To our knowledge, there are only five cases with dural AVFs involving the hypoglossal canal in the previous literature 1-3. The hypoglossal nerve, neuromeningeal branch of the ascending pharyngeal artery with the surrounding venous plexus go through the hypoglossal. The venous plexus within the hypoglossal canal is referred to as the anterior condylar vein. The anterior condylar vein traverses the hypoglossal canal joining the inferomedial aspect of the IPS to the suboccipital venous plexus, vertebral or paravertebral veins, marginal sinus, or the internal vertebral venous plexus 4. DAVFs localized to the anterior condylar vein can be confused with fistulas involving the marginal sinus because of the similarity on angiograms. Hence, Ernst et Al 1 and Kiyosue et Al 2 reported that precise observation on MRI and contralateral carotid angiography were useful in identifying the exact location of the fistula within the hypoglossal canal. In the present case, MRI clearly demonstrated a findings of abnormal flow signal within the hypoglossal canal (figure 1). The CT scan following endovascular treatment demonstrated the exact coil placement in the possible venous pouch located within the canal (figure 5).
Clinical symptoms of DAVFs depend on the pattern of fistulous venous drainage. Although the common manifestations of posterior cranial fossa DAVFs are tinnitus, bruit and vertigo, they often present ocular symptoms mimicking a dural carotid-cavernous sinus fistula (CCF). In the present case, we observed retrograde venous drainage to the IPS, CSes, SOV and cortical veins, suggesting the possible increasing venous pressure in these venous channels. A DAVF with retrograde cortical venous drainage as shown in the present case (figure 2) has a high risk for cerebral haemorrhage 5 and such a case must be treated as soon as possible. In the present case, we used transvenous approach to embolize and occlude the fistula, resulting in angiographical improvement as well as complete resolution of the symptoms. Previous report 1 revealed that transvenous coil embolization was curative in two of three cases of DAVF related to the hypoglossal canal. According to McDougall et Al 6, DAVFs of the marginal sinus are potentially life-threatening lesion that must be treated with endovascular techniques with a high rate of cure and low morbidity. They cured 13 of 14 patients with endovascular techniques alone and one by preoperative embolization followed by surgical obliteration of the fistula. They performed transvenous coil embolization in all patients and transarterial embolization with particles or liquid was preceded in seven patients. Because of the inability to embolize the exact site of the fistula and all its feeding artery pedicles, transarterial treatment is unlikely to result in permanent cure. However it can be useful in reducing the rate of flow through a fistula before attempting definitive treatment.
In conclusion, DAVFs within the hypoglossal canal are relatively rare and may be confused with marginal sinus DAVFs on angiography. MRI is useful in diagnosing the precise localization of the fistula to the hypoglossal canal. Transvenous coil embolization must be tried initially to cure the lesion.
References
- 1.Ernst R, Bulas R, et al. Three cases of dural arteriovenous fistula of the anterior condylar vein within the hypoglossal canal. Am J Neuroradiol. 1999;20:2016–2020. [PMC free article] [PubMed] [Google Scholar]
- 2.Kiyosue H, Tanoue S, et al. Ocular symptoms associated with a dural arteriovenous fistula involving the hypoglossal canal: Selective transvenous coil embolization: Case report. J Neurosurg. 2001;94:630–632. doi: 10.3171/jns.2001.94.4.0630. [DOI] [PubMed] [Google Scholar]
- 3.Komiyama M, Ishiguro T, et al. Intense pulse-synchronous tinnitus caused by dural arteriovenous fistula at the hypoglossal canal. No to Shinkei. 2002;54:830–831. [PubMed] [Google Scholar]
- 4.Katsuta T, Rhoton A, Jr, Matsushima T. The jugular foramen: microsurgical anatomy and operative approaches. Neurosurgery. 1997;41:149–202. doi: 10.1097/00006123-199707000-00030. [DOI] [PubMed] [Google Scholar]
- 5.Lasjaunias P, Berenstein A. Surgical Neuroangiography. Vol. 2. New York: Springer-Verlag; 1987. pp. 273–315. [Google Scholar]
- 6.McDougall C, Halbach V, et al. Dural arteriovenous fistulas of the marginal sinus. Am J Neuroradiol. 1997;18:1565–1572. [PMC free article] [PubMed] [Google Scholar]