Abstract
Purpose
To show the radiological results of adolescent idiopathic scoliosis (AIS) patients treated with posterior fusion using all-pedicle-screw construct with correction carried out using a convex rod reduction technique.
Methods
Between October 2004 and June 2007, 42 AIS patients were treated with posterior fusion using all-pedicle-screw construct with correction done through the convex side. Two patients were lost to follow-up and were not included in the study. Forty patients had a minimum follow-up of 2 years. Patients were evaluated for the deformity correction in coronal and sagittal planes and for spinal balance.
Results
The mean preoperative Cobb angle of the major curve and secondary minor curves was 60° and 41°, respectively. Immediate postoperative mean Cobb angle of the major curve and secondary minor curves was 17° and 13°, respectively. Postoperative 2-year average major curve loss of correction was 7 %. Postoperative 2-year average minor curve loss of correction was 5 %. Preoperative thoracic kyphosis of 28° was changed to 22° in 2-years follow-up. The loss of thoracic kyphosis was most noted in hyperkyphotic patients.
Conclusions
The correction of AIS by convex-sided pedicular screws yields a coronal correction comparable to what is described in the literature for segmental concave-sided screws.
Keywords: Adolescent idiopathic scoliosis, Convex side correction, Pedicular screws, Complications, Posterior fusion
Introduction
Since the introduction of Harrington rod instrumentation in 1960, in which correction was achieved by distraction forces, the correction techniques in scoliosis surgery have changed dramatically [1]. Curve correction was carried out by applying vertebral translation forces with sublaminar wires and later on according to the principles of Cotrel and Dubousset [2] by rod rotation of the concave rod to achieve de-rotation and slight distraction on the concave side and compression on the convex side. In all these surgical techniques, hooks and wires were used being the standard treatment for adolescent spinal deformities.
In the recent years, the use of thoracic pedicle screws has emerged in deformity surgery, providing a stable fixation system, opening new and more powerful possibilities to correct deformities [3–8]. Most of these correction maneuvers were utilizing the Cotrel and Dubousset principles of correction on screws, or hook and screws constructs.
Suk et al. [5] report on satisfactory radiographic and clinical outcomes with 203 thoracic idiopathic scoliosis patients subjected to selective thoracic fusion with segmental pedicle screw fixation. Other studies which compare the result of posterior segmental correction and fusion with pedicle screw instrumentations versus those with hooks or hybrid constructs in adolescent idiopathic scoliosis (AIS) describe a similar method of curve correction [6–9]. The concave rod is placed first in all patients except for patients with thoracic hyperkyphosis in whom the convex rod is placed first. Curve correction is achieved with concave rod maneuvers to optimize three-dimensional correction of the deformity. For thoracic hyperkyphosis, applied convex compression forces are used to correct the scoliosis and kyphosis simultaneously.
Use of the concave side for correction is traditional but associated with potential drawbacks. Liljenqvist et al. [10] studied the morphometry of thoracic and lumbar pedicles in idiopathic scoliosis. A significantly smaller pedicle width was observed on the concavity at the apical region of the thoracic curves. Other studies have shown higher incidence of cortical wall penetration on the concave side than the convex side in patients with scoliotic deformity [11].
Rauschning [12] presented dissections of human cadavers with scoliosis showing a shift of the dural sac to the concave side of the scoliotic curve with direct proximity to the pedicle. Meaning, neural elements lie directly adjacent to the concave pedicles and, as such, may not tolerate even minor compromise of the medial pedicle cortex. This implies that a medial pedicle screw penetration on the convex side might be tolerated better without injury to the spinal cord than a penetration on the concave side of a scoliotic curve, especially at the apex.
Our hypothesis was that comparable, safe and effective correction can be achieved using the convex side to anchor the construct and by applying the corrective maneuver on the convex rather the concave side.
The purpose of this prospective study is to evaluate radiographic results of AIS patients treated with posterior fusion using all-pedicle-screw construct with correction done through the convex side.
Methods
Following Institutional Review Board approval, all patients who were operated for AIS were enrolled in the study in a single institution, excluding those patients with Lenke 5 type scoliosis treated by anterior approach. Preoperative, early postoperative, and 2-years follow-up postoperative data were recorded for all patients.
Data collection was carried out by a single observer (orthopedic spine surgeon) who was not involved in the surgical treatment. This single observer did all radiological measurement and collected data from medical records. All patients were treated at our institution between October 2004 and June 2007.
Demographic and radiological data
Forty-two patients with AIS were included in this study. Two patients were lost to follow-up, so the study included 40 patients with a mean follow-up of 24.9 months (range 24–42 months). There were 29 female and 11 male patients. Average age at surgery was 15.2 years (range 12–21 years).
The most frequent Risser grade observed in the cohort was Grade 4 (Average 3.75, range 0–5 grade). Table 1 describes the distribution of patients according to the surgical classification of AIS by Lenke et al. [13].
Table 1.
Distribution of patients according to the surgical classification of AIS by Lenke et al. (N) for normal thoracic kyphosis sagittal modifier (T4–T12, +10° to +40°)
| A+ | A− | AN | B+ | B− | BN | C+ | C− | CN | Total | |
|---|---|---|---|---|---|---|---|---|---|---|
| Type 1 main thoracic | – | 3 | 3 | 1 | 1 | 3 | – | 1 | 3 | 15 |
| Type 2 double thoracic | – | – | 4 | – | – | 4 | – | – | 2 | 10 |
| Type 3 double major | – | – | – | – | – | – | 2 | 1 | 4 | 7 |
| Type 4 triple major | – | – | – | 1 | – | – | – | – | 1 | 2 |
| Type 6 thoracolumbar/lumbar-main thoracic | – | – | – | – | – | – | 2 | – | 4 | 6 |
(+) for thoracic hyperkyphosis sagittal modifier (T4–T12 >+40°) and (−) for thoracic hypokyphosis sagittal modifier (T4–T12 <+10°)
Radiographic analysis
Posteroanterior and lateral three-foot standing preoperative radiographs were used to evaluate the coronal and sagittal planes. Curve flexibility was determined on the preoperative supine side bending films.
Radiographic analysis included Cobb angle measurements of the major curve which included the main thoracic curve in Lenke type 1–4, and the thoracolumbar/lumbar curve in Lenke type 6.
Radiographic analysis included also Cobb angle measurements of the minor curves which included the upper thoracic curve in Lenke type 2 and 4, the thoracolumbar/lumbar curve in Lenke type 3 and 4, and the main thoracic curve in Lenke type 6. All patients had early postoperative (within 1 week) films and postoperative 2-years radiographs.
The preoperative major and minor curves for each individual were identified and compared with the postoperative major and minor curves at the same location.
Coronal balance was measured using a radiological plumb line drawn from the center of the C7 endplate and the distance from the line was measured to the center sacral vertical line (CSVL). The patients were divided into three groups, “perfectly balanced,” “compensated” and “de-compensated”. In patients who were “perfectly balanced,” there was a 0-cm distance between the radiological plumb line and CSVL. Patients were considered “compensated” with less or 2 cm distance between the coronal plumb line and CSVL. Coronal de-compensation was defined as >2 cm distance from the radiological plumb line to the CSVL.
Thoracic kyphosis was measured from the upper endplate of T4 to the lower endplate of T12 on a standing lateral radiograph. Hypokyphosis, as defined by Lenke, was identified in a curve of less than +10°, normal kyphosis identified in a curve of +10° to +40° and hyperkyphosis was identified a curve of more than +40°.
Preoperative planning
All structural curves, not correcting to <25° on bending films, were included in the fusion. The lowest instrumented vertebra (LIV) was selected according to the following criteria: the disk below LIV reversed its tilt on bending films, the LIV was not at the apex of a curve at the coronal or sagittal plane, the LIV was not at the thoraco-lumbar junction or at an area of junctional kyphosis. For selective thoracic fusion, the L1 vertebra was the preferred LIV. The upper instrumented vertebrae (UIV) was selected according to the following criteria: if the left shoulder was higher than the right shoulder then the upper thoracic curve was included in the fusion, a stable vertebra was preferred as an UIV and the UIV avoids the apex of thoracic kyphosis or area of junctional kyphosis. Bilateral pedicular screws were used at the UIV, LIV and any end vertebrae that were included at the fusion. At the convex side, a screw was used at every second vertebrae. At the concave side one or two more screws were added to the screws that were applied to end vertebra to reinforce the construct. The apex at the concave side was never instrumented (Fig. 1).
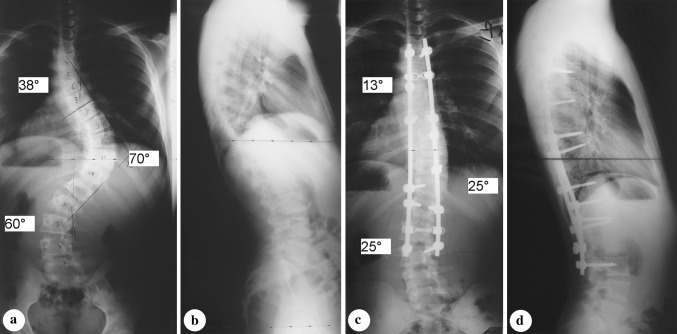
Fig. 1.
Triple major (upper thoracic, main thoracic and thoracolumbar/lumbar) curves of a 17-year-old boy. a Preoperative anteroposterior radiograph shows 38° upper thoracic curve, 70° main thoracic curve and 60° lumbar curve. b Preoperative lateral radiograph. c Anteroposterior radiograph taken 2 years after surgery. The upper thoracic curve was corrected to 13°, main thoracic curve was corrected to 25° and the lumbar curve was corrected to 25°. d In a lateral radiograph taken 2 years after surgery it can be seen that the thoracic kyphosis was not changed
Operative procedures
All patients had a posterior arthrodesis of the spine. Posterior surgery was performed on an open OSI frame. All the pedicle screws were inserted using a free-hand pedicle screw placement technique as described by Kim et al. [14]. Initially, thorough and meticulous exposure out to the tips of all transverse processes to be included in the instrumentation and fusion was performed. Next, 5 mm of the inferior facet was excised and cartilage on the dorsal side of the superior facet was removed. Lumbar facet joints were also excised.
The diameters of the screws were selected by careful evaluation of the preoperative radiographs. We used the screws with the diameters between 4.5 and 4.75 mm for the upper thoracic pedicles and between 5.5 and 6.5 mm for the lower thoracic and upper lumbar pedicles.
Screws were inserted according to a preoperative plan; all screws were monoaxial. Verification of placement was undertaken using fluoroscopy. Motor and somatosensory evoked potential spinal cord monitoring was used in all cases. All patients underwent a convex side thoracoplasty through the primary operative incision. An average of 4 ribs (range 3–5 ribs) was partially resected at the apex of the thoracic hump. We placed the 6.35 titanium convex rod first and applied de-rotation convex compression forces to correct the scoliosis. In double major curve, each curve was corrected at the convex side first, i.e., the right-sided rod was used for the major thoracic curve while the lumbar screws were left loose, then further correction was obtained by repeated in situ bending of the rod in the coronal plane of the apex of the curve, and then a left-sided rod was used at the lumbar curve. After locking the screws in the final corrected position, arthrodesis was carried out using a combination of autogenous ribs and locally harvested bone graft.
None of the patients were immobilized in a brace. Patients were allowed to ambulate the morning after operation.
During operation, operative time, blood loss and intra-operative complications were recorded.
Results
Coronal plane radiographic results
The mean preoperative Cobb angle of the major curve was 60° ± 11° (range 45°–85°) (Table 2). The flexibility of the major curve was 43 %. Immediate postoperative mean Cobb angle of the major curve was 17° ± 9° (range 0°–37°). Immediate postoperative major curve correction averaged 72 %. Postoperative 2-year Cobb angle of the major curve was 21° ± 9° (range 5°–39°). Postoperative 2-year major curve loss of correction was 7 % (Fig. 2a, b).
Table 2.
Comparison of coronal plane changes: preoperatively, immediate postoperatively and in 2-years follow-up
| Preoperative | Immediate postoperative | In 2-years follow-up | Immediate correction (%) | Loss of correction (%) | |
|---|---|---|---|---|---|
| Major curve Cobb (°) | 60 ± 11 | 17 ± 9 | 21 ± 9 | 71 | 7 |
| Minor curve Cobb (°) | 41 ± 12 | 13 ± 7 | 15 ± 11 | 68 | 5 |
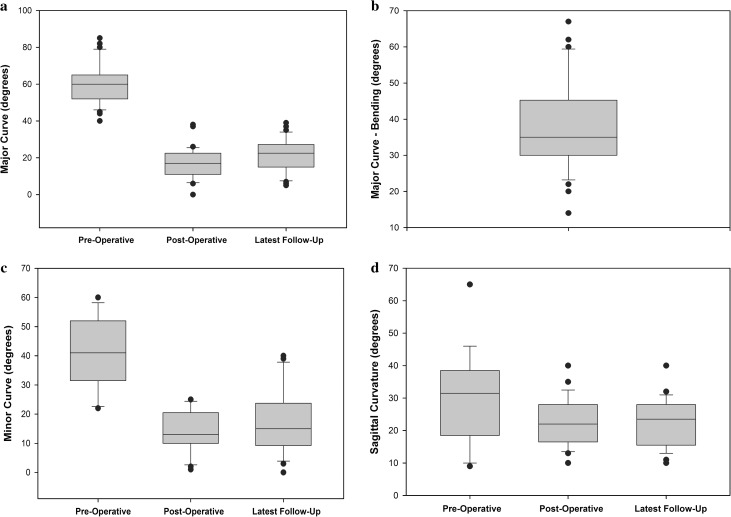
Fig. 2.
A Whisker type plot showing a major curve preoperative, early postoperative and late postoperative data; b major curve flexibility; c minor curve preoperative, early postoperative and late postoperative data; and d sagittal plane data
Preoperative Cobb angle of the secondary minor curves was 41° ± 12° (range 22°–60°). Immediate postoperative Cobb angle of the secondary minor curve was 13° ± 7° (range 1°–25°). Immediate postoperative secondary minor curves correction averaged 68 %.
Postoperative 2-year Cobb angle of the secondary minor curve was 15° ± 11° (range 0°–40°). Postoperative 2-year minor curve loss of correction was 5 % (Fig. 2c).
Global coronal balance, the distance between the C7 radiological plumb line and CSVL, was 10 mm before surgery, 16 mm immediate postoperative and 6 mm at 2-years follow-up. Preoperatively there were 13 patients whom we classified as “perfectly balanced” with 0-cm distance between the coronal plumb line (a radiological plumb line drawn from the center of the C7 endplate) and CSVL, 22 patients as “compensated” with less or 2 cm distance between the coronal plumb line and CSVL, and 5 patients as “de-compensated” with the same distance longer than 2 cm. In a 2-years follow-up, the “perfectly balance” group included 20 patients, the “compensated” group included 19 patients and only one patient was found in the “de-compensated” group (Table 3).
Table 3.
Distribution of patients as “perfectly balanced”, “compensated” and “de-compensated” in the coronal plane
| Preoperative | In 2-years follow-up | |
|---|---|---|
| Plumbline = 0 | 13 | 20 |
| Plumbline <2 | 22 | 19 |
| Plumbline >2 | 5 | 1 |
Patients were classified according to the distance between the coronal plumb line (a radiological plumb line drawn from the center of the C7 endplate) and CSVL. A 0-cm distance was defined as “perfectly balanced”, a distance of less or equal to 2 cm was defined as “compensated” and a distance of more than 2 cm was defined as “de-compensated”
Sagittal plane radiographic results
Preoperative thoracic kyphosis (T4–T12) of 28° (range −10° to 65°) was changed to 21° (range 8°–40°) at 1 week after surgery and to 22° (range 8°–40°) in 2-years follow-up (Fig. 2d).
We examined the changes in the sagittal plane based on three different subgroups: hypokyphotic patients, normal kyphosis patients and hyperkyphotic patients. Preoperatively six patients were hypokyphotic (average 5°, range −10° to 10°), 28 patients had normal kyphosis (average 28°, range 12°–40°) and six patients were hyperkyphotic (average 50°, range 45°–65°). At 2-years follow-up, in the hypokyphotic group, the average curve measured 12° (range 8°–20°), in normal kyphosis group, the average curve measured 23° (range 15°–32°) and in the hyperkyphotic group the average curve measured 27° (range 15°–40°) (Table 4).
Table 4.
Pre and postoperative sagittal alignment in the hypokyphotic, normal kyphosis and hyperkyphotic groups
| Preoperative | In 2-years follow-up | P value | |
|---|---|---|---|
| All patients (°) | 28 | 22 | |
| Hypokyphotic (°) | 5 | 12 | (<0.001) |
| Normal kyphosis (°) | 28 | 23 | (<0.001) |
| Hyperkyphotic (°) | 50 | 27 | (<0.001) |
There was a statistically significant difference between the hyperkyphotic group and the hypokyphotic and normal kyphotic groups regarding sagittal curve change (P < 0.001). While patients in the hypokyphotic group gained more kyphosis, patients in the hyperkyphotic group lost kyphosis.
Operation time, blood loss and complications
The average operative time was 276 min (range 180–360 min). Average intra-operative blood loss was 1,414 ml (range 800–2,700 mL).
There were no deep wound infections after surgery. There were no vascular or neurological complications related to the pedicle screws. One patient developed superior mesenteric artery syndrome and was treated accordingly. No patient has undergone revision surgery.
Discussion
Despite the excellent biomechanical advantages of pedicle screws over the other forms of spinal instrumentation, there is an increased risk of causing permanent neurological injuries during insertion of the device and during correction of the deformity. For the thoracic pedicle screws used in the treatment of spinal deformities, the incidence of screw misplacement ranges from 1.5 to 25 % with screw-related neurological complication in 0–0.9 % [5, 11, 15–18]. Several studies demonstrated a significantly smaller pedicle width on the concavity at the apical region of the thoracic curves [10, 19, 20]. Other studies demonstrated higher incidence of pedicle perforation in the concave side [11]. A systematic review of pedicle screw-related complication in scoliosis surgery noted that in all cases were the location of dural leaks was reported, it occurred on the concave thoracic pedicle [21]. Dissections of human cadavers with scoliosis showed a shift of the dural sac to the concave side of the scoliotic curve with direct proximity to the pedicle [12, 22]. The anatomical position of the spinal cord in the canal is also well demonstrated in MRI studies (Fig. 3). As a result, medial pedicle screw penetration on the convex side might be tolerated better without injury to the spinal cord than a penetration on the concave side of a scoliotic curve [12], explaining why our proposed method of deformity correction, theoretically reduces the risk for neurological injury.
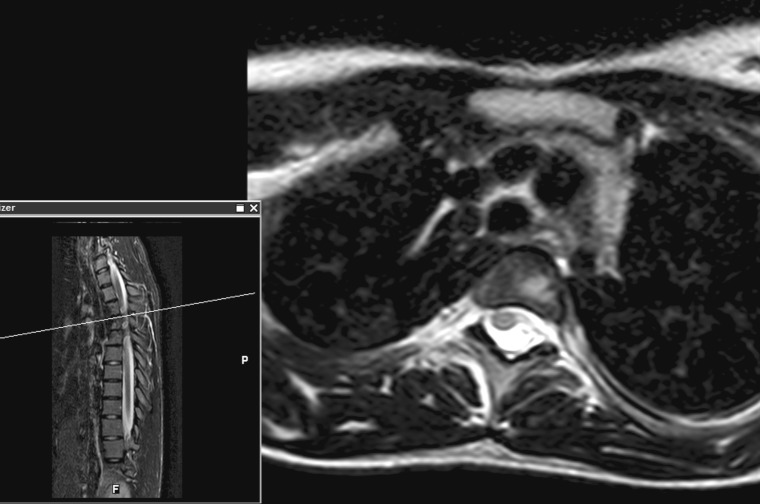
Fig. 3.
T2-weighted MRI axial view of a patient with adolescent idiopathic scoliosis. The axial view is at the T5–T6 level where there is a left upper thoracic curve. The spinal cord deviates toward the concavity side of the curve where even minimal medial penetration of the pedicle may injure the spinal cord
Kim et al. [7] using pedicle screws inserted at all levels on the concave side of the thoracic curve and every second or every third vertebra on the convex side and reported an average major curve correction of 70 % and a secondary curve correction of 65 %. In our patients a correction of 71 and 68 % was achieved in the major and minor curves, respectively. Suk et al. [5] using similar methods showed a correction of 72 % in the main thoracic curve and a 71 % correction in the lumbar curve. However, we inserted screws bilaterally on both end vertebra and unilateral every second segment on the convex side. On the concave side, we added only one or two more screws, avoiding the apex. Thus, we demonstrated that the use of screws in every second level does not compromise correction and theoretically allow shorter procedure at a lower cost.
Thoracic kyphosis demonstrated a 6° decrease after surgery. The positioning of the patient, in extension on the Jackson’s OSI table may contribute to the loss of kyphosis [23]. Nevertheless, it is hypothesized that compressive force applied to the convexity of the curve during the corrections maneuver is the main cause for the decrease in kyphosis. Loss of thoracic kyphosis ranging 10°–14° [7, 24, 25] was also described following the use of concave segmental screws for deformity correction. Other studies showed an increase in thoracic kyphosis [5, 26]. These studies, however, did not evaluate separately the hypokyphotic, normal kyphotic and hyperkyphotic curves. When comparing the three groups, a statistically significant difference was found with the hyperkyphotic curves loosing thoracic kyphosis and the normal kyphotic and hypokyphotic curves showing a minimal change in kyphotic position. We currently avoid compression maneuver on the convex side and try to gain more kyphosis by in situ bending the convex rod before inserting the concave side rod. However, in cases of severe hypokyphosis or lordotic spine it will be very difficult to gain kyphosis, so other method of correction might be used.
One can claim that the vast usage of thoracoplasty on all of our patients was too aggressive. However, thoracoplasty has been shown to give better rib hump correction and satisfactory clinical outcomes without pulmonary function compromise, even in patients who underwent DVR [27]. None of our patients required thoracic tube or had any other complication related to thoracoplasty.
In recent years there is a trend toward new correction techniques, the direct vertebral rotation (DVR) and direct vertebral de-rotation (DVD). The DVR applies a de-rotation maneuver on the apical vertebra in the opposite direction to the rod de-rotation and DVD applies vertebral de-rotation maneuvers on each vertebral level in the instrumented segment. Both methods require the insertion of bilateral screws in every manipulated segment. Some studies comparing direct vertebral rotation to simple rod de-rotation maneuvers, found a better coronal and rotational correction using these new methods [28–30]. Others have shown mixed results with a better correction in the main and proximal thoracic curve with the direct vertebral de-rotation system but not as good results with regards to the lumbar curve [31]. The combination of these relatively new correction techniques and CT-guided navigation pedicles screw insertion which significantly enhances accuracy and safety placement of thoracic pedicle screws [32] is promising. However, Hicks et al. [21], in their systematic review of complications associated with pedicle screw fixation in scoliosis surgery, state that the high incidence of patients with mal-positioned screw obligate us to use techniques that can decrease screw mal-positioning including inserting only the number of screws necessary for a given curve at the strategic levels.
The method which is presented in this study serves as such an alternative with similar effectiveness regarding the correction and in theory should result in lower risk and costs.
Conclusion
A posterior correction and fusion using all-pedicle-screw constructs carried out using the convex rod de-rotation maneuver offers similar major and minor curve correction when compared to concave rod reduction techniques. There are theoretical advantages in reducing the risk of neurological harm and cost when using the convex rod reduction techniques.
Conflict of interest
None.
Footnotes
The study was approved by the Institutional Review Board of Assaf Harofeh Medical Center.
References
- 1.Harrington PR. Treatment of scoliosis: correction and internal fixation by spine instrumentation. J Bone Joint Surg Am. 1962;44:591–610. [PubMed] [Google Scholar]
- 2.Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop. 1988;227:10–23. [PubMed] [Google Scholar]
- 3.Suk SI, Lee CK, Kim WJ, et al. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. [PubMed] [Google Scholar]
- 4.Suk SI, Kim WJ, Kim JH, et al. Restoration of thoracic kyphosis in the hypokyphotic spine: a comparison between multiple-hook and segmental pedicle screw fixation in adolescent idiopathic scoliosis. J Spinal Disord. 1999;12:489–495. doi: 10.1097/00002517-199912000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Suk SI, Lee SM, Chung ER, Kim JH, Kim SS. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine. 2005;30:1602–1609. doi: 10.1097/01.brs.0000169452.50705.61. [DOI] [PubMed] [Google Scholar]
- 6.Dobbs MB, Lenke LG, Kim YJ, Kamath G, Peelle MW, Bridwell KH. Selective posterior thoracic fusions for adolescent idiopathic scoliosis: comparison of hooks versus pedicle screws. Spine. 2006;31:2400–2404. doi: 10.1097/01.brs.0000240212.31241.8e. [DOI] [PubMed] [Google Scholar]
- 7.Kim YJ, Lenke LG, Kim J, Bridwell KH, Cho SK, Cheh G, Sides B. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2006;31:291–298. doi: 10.1097/01.brs.0000197865.20803.d4. [DOI] [PubMed] [Google Scholar]
- 8.Lowenstein JE, Matsumoto H, Vitale MG, Weidenbaum M, Gomez JA, Lee FY, Hyman JE, Roye DP., Jr Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine. 2007;32:448–452. doi: 10.1097/01.brs.0000255030.78293.fd. [DOI] [PubMed] [Google Scholar]
- 9.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine. 2004;29:333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 10.Liljenqvist UR, Link TM, Halm HF. Morphometric analysis of thoracic and lumbar vertebrae in idiopathic scoliosis. Spine. 2000;25:1247–1253. doi: 10.1097/00007632-200005150-00008. [DOI] [PubMed] [Google Scholar]
- 11.Smorgick Y, Millgram MA, Anekstein Y, Floman Y, Mirovsky Y. Accuracy and safety of thoracic pedicle screw placement in spinal deformities. J Spinal Disord Tech. 2005;18:522–526. doi: 10.1097/01.bsd.0000154448.90707.a8. [DOI] [PubMed] [Google Scholar]
- 12.Rauschning W (1995) Anterior surgery of the thoracolumbar junction and the lumbar spine. Anatomy, complications, safeguards. Presented at the meeting anterior spine surgery: standards and new techniques. Berlin, October 25–27
- 13.Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83:1169–1181. [PubMed] [Google Scholar]
- 14.Kim YJ, Lenke LG, Keith HB, et al. Free hand pedicle screw placement in the thoracic spine: is it safe? (Spine SRS Specialty Issue) Spine. 2004;29:333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 15.Suk SI, Lee CK, Kim WJ, et al. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. [PubMed] [Google Scholar]
- 16.Brown CA, Lenke LG, Bridwell KH, et al. Complications of pedicle thoracolumbar and lumbar pedicle screws. Spine. 1998;23:1566–1571. doi: 10.1097/00007632-199807150-00012. [DOI] [PubMed] [Google Scholar]
- 17.Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine. 1997;22:2239–2245. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 18.Suk SI, Kim WJ, Lee SM, et al. Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine. 2001;26:2049–2057. doi: 10.1097/00007632-200109150-00022. [DOI] [PubMed] [Google Scholar]
- 19.Xiong B, Sevastik B, Willers U, Sevastik J, Hedlund R. Structural vertebral changes in the horizontal plane in idiopathic scoliosis and the long-term corrective effect of spine instrumentation. Eur Spine J. 1995;4:11–14. doi: 10.1007/BF00298411. [DOI] [PubMed] [Google Scholar]
- 20.Smith RM, Pool RD, Butt WP, Dickson RA. The transverse plane deformity of structural scoliosis. Spine. 1991;16:1126–1129. doi: 10.1097/00007632-199109000-00020. [DOI] [PubMed] [Google Scholar]
- 21.Hicks JM, Singla A, Shen FH, Arlet V. Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine. 2010;35:E465–E470. doi: 10.1097/BRS.0b013e3181d1021a. [DOI] [PubMed] [Google Scholar]
- 22.Bridwell KH, Kuklo TR, Lewis SJ, Sweet FA, Lenke LG, Baldus C. String test measurement to assess the effect of spinal deformity correction on spinal canal length. Spine. 2001;26:2013–2019. doi: 10.1097/00007632-200109150-00015. [DOI] [PubMed] [Google Scholar]
- 23.Marsicano JG, Lenke LG, Bridwell KH, Chapman M, Gupta P, Weston J. The lordotic effect of the OSI frame on operative adolescent idiopathic scoliosis patients. Spine. 1998;23:1341–1348. doi: 10.1097/00007632-199806150-00009. [DOI] [PubMed] [Google Scholar]
- 24.Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2004;29:2040–2048. doi: 10.1097/01.brs.0000138268.12324.1a. [DOI] [PubMed] [Google Scholar]
- 25.Lowenstein JE, Matsumoto H, Vitale MG, et al. Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine. 2007;32:448–452. doi: 10.1097/01.brs.0000255030.78293.fd. [DOI] [PubMed] [Google Scholar]
- 26.Suk SI, Kim WJ, Kim JH, Lee SM. Restoration of thoracic kyphosis in the hypokyphotic spine: a comparison between multiple-hook and segmental pedicle screw fixation in adolescent idiopathic scoliosis. J Spinal Disord. 1999;12:489–495. doi: 10.1097/00002517-199912000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Suk SI, Kim JH, Kim SS, Lee JJ, Han YT. Thoracoplasty in thoracic adolescent idiopathic scoliosis. Spine. 2008;33:1061–1067. doi: 10.1097/BRS.0b013e31816f2888. [DOI] [PubMed] [Google Scholar]
- 28.Asghar J, Samdani AF, Pahys JM, et al. Computed tomography evaluation of rotation correction in adolescent idiopathic scoliosis: a comparison of an all pedicle screw construct versus a hook-rod system. Spine. 2009;34:804–807. doi: 10.1097/BRS.0b013e3181996c1b. [DOI] [PubMed] [Google Scholar]
- 29.Lee SM, Suk SI, Chung ER. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine. 2004;29:343–349. doi: 10.1097/01.BRS.0000109991.88149.19. [DOI] [PubMed] [Google Scholar]
- 30.Suk SI, Kim JH, Kim SS, Lim DJ. Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS) Eur Spine J. 2012;21:13–22. doi: 10.1007/s00586-011-1986-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kadoury S, Cheriet F, Beauséjour M, Stokes IA, Parent S, Labelle H. A three-dimensional retrospective analysis of the evolution of spinal instrumentation for the correction of adolescent idiopathic scoliosis. Eur Spine J. 2009;18:23–37. doi: 10.1007/s00586-008-0817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ughwanogho E, Patel NM, Baldwin KD, Sampson NR, Flynn JM (2011) CT-guided navigation of thoracic pedicle screws for ais results in more accurate placement and less screw removal. Spine. Oct 24 (Epub ahead of print) [DOI] [PubMed]