Abstract
Purpose
One of the downsides of spinal correction surgery for adolescent idiopathic scoliosis (AIS) is the cessation of spinal longitudinal growth within the fused levels in growing children. However, the surgery itself has the potential to increase spinal longitudinal length by correcting the curvature. The purpose of this study was to evaluate the correlation between curve correction and increased spinal longitudinal length by corrective surgery for AIS.
Methods
This study included 208 consecutive patients (14 male, 194 female) with AIS who underwent posterior or anterior correction and fusion surgeries. Mean age at the time of surgery was 15.7 ± 3.3 years (range 10–20 years). Patients with hyperkyphosis of more than 40° were excluded. All patients had main curves in the thoracic spine (Lenke type 1 or 2). Forty-three patients underwent anterior spinal correction and fusion (ASF) and 164 underwent posterior spinal correction and fusion (PSF). The mean preoperative height was 154.7 ± 6.9 cm (range 133–173 cm). Pre and postoperative PA standing X-ray films were used to measure the Cobb angle and spinal length between the end vertebrae of the main thoracic curve, and between T1 and L5. The patients were divided into ASF and PSF groups, within which correlations between the Cobb angle correction and spinal length increase were evaluated.
Results
In the ASF group, the mean preoperative Cobb angle of the main thoracic curve was 54.9 ± 8.3° (range 41–83°) and it was corrected to 19.7 ± 9.5° (range 0–47°) with a mean correction of 35.2 ± 11.1° (range 10–74°) after surgery. The mean increase in the length of the main thoracic curve was 1.5 ± 4.6 mm (range −8 to 13 mm), and the mean increase in T1–L5 length was 16.6 ± 7.7 mm (range −3 to 51 mm). Significant correlation between the correction of the Cobb angle and increase in T1–L5 length was observed, with a correlation coefficient of 0.44. In the PSF group, the mean preoperative Cobb angle of the main thoracic curve was 58.8 ± 11.6° (range 36–107°) and it was corrected to 17.1 ± 7.6° (range 10–49°), with a mean correction of 41.7 ± 10.2° (range 21–73°) after surgery. The mean increase in the length of the main thoracic curve was 14.0 ± 5.2 mm (range 0–42 mm), and the mean increase in T1–L5 length was 32.4 ± 10.8 mm (10–61 mm). Correlation between the correction of the Cobb angle and increase in T1–L5 length was high, with a correlation coefficient of 0.64. The increase in T1–L5 length could be calculated by the following formula based on linear regression analysis: increase in T1–L5 length (mm) = correction of the Cobb angle (º) × 0.77.
Conclusion
Spinal longitudinal length was significantly increased after surgery in both the ASF and PSF groups. Correction of the Cobb angle and increase in T1–L5 length were highly correlated with each other, especially in the PSF group.
Keywords: Adolescent idiopathic scoliosis, Posterior correction with fusion surgery, Anterior correction with fusion surgery, Spinal length
Background
In skeletally immature patients with scoliosis, one of the most important problems of correction by fusion surgery is the preclusion of longitudinal growth of the fused spine after surgery. This results in short stature and trunk at skeletal maturity [1, 2]. When considering spinal fusion surgery for skeletally immature patients, the potential loss of height has been estimated using an equation established by Winter [3]: shortening of the spine (cm) = 0.07 × number of segments fused × number of years of growth remaining. Meanwhile, it has also been recognized that correcting the spinal curvature can increase the longitudinal length of the spine. Thus, the estimates of final height should consider not only the loss of spinal growth by fusion but also the increase in spinal length by correction. However, to our knowledge, no study has reported the effect of correction and fusion surgery on the postoperative increase in longitudinal spinal length. The purpose of this study was to evaluate the correlation between curve correction by surgery and the increase in spinal longitudinal length in patients with adolescent idiopathic scoliosis (AIS).
Materials and methods
This study included 208 consecutive patients with AIS (14 males, 194 females) who underwent posterior or anterior correction and fusion surgeries (Table 1). Mean age at the time of surgery was 15.7 ± 3.3 years (range 10–20 years). Mean preoperative height was 154.7 ± 6.9 cm (range 133–173 cm) and mean weight was 45.3 ± 6.5 kg (range 26–65 kg). The thoracic kyphosis angles (T5–T12) were between −10 and 40º, and the patients with hyperkyphosis more than 40º were excluded. The mean kyphosis angle was 15.5 ± 12.6º (−10 to 40º). All patients had main curves in the thoracic spine (Lenke type 1: 138 patients, type 2: 70 patients). A variety of lumbar modifiers were also assigned (A: 126 patients, B: 44 patients, C: 38 patients). Forty-three patients underwent anterior spinal correction and fusion (ASF), and 165 patients underwent posterior spinal correction and fusion (PSF). Among the patients who underwent PSF, hybrid constructs (combination of pedicle screws, hooks, and wires) were used in 106 and all-pedicle-screw constructs were used in 59. During ASF, thorough removal of the discs included in the correction and fusion area and the application of maximum compression force were performed during surgery.
Table 1.
Demographics of patients
| ASF | % | PSF | % | Total | % | |
|---|---|---|---|---|---|---|
| N | 43 | 165 | 208 | |||
| Male* | 1 | 2 | 13 | 8 | 14 | 7 |
| Female* | 42 | 98 | 152 | 92 | 194 | 93 |
| Height (cm)** | 155.5 ± 6.3 (138–168) | 154.5 ± 6.9 (133–173) | 154.7 ± 6.9 (133–173) | |||
| Weight (kg)** | 45.9 ± 5.7 (32–61) | 44.9 ± 6.7 (26–65) | 45.3 ± 6.5 (26–65) | |||
| Age (years)** | 15.5 ± 3.3 (12–27) | 15.7 ± 3.3 (10–29) | 15.7 ± 3.3 (10–29) | |||
| Lenke type1† | 36 | 84 | 102 | 62 | 138 | 63 |
| Lenke type2† | 7 | 16 | 63 | 38 | 70 | 32 |
| Lumbar modifier A†† | 24 | 56 | 102 | 62 | 126 | 60 |
| Lumbar modifier B†† | 9 | 21 | 35 | 21 | 44 | 21 |
| Lumbar modifier C†† | 10 | 23 | 28 | 17 | 38 | 18 |
ASF anterior spinal correction with fusion, PSF posterior spinal correction with fusion
* No significant difference by Chi-square test regarding proportion of gender
** No significant difference by Mann–Whitney U test
†p = 0.005 by Chi-square test regarding proportion of type 1 and 2
††No significant difference by one way factorial ANOVA regarding proportion of Lumbar modifier
Correlation between curve correction and increase in spinal length
The longitudinal length of the spine was measured both at the main thoracic curve and at the whole spine between T1 and L5. The length at the main thoracic curve was defined as the distance between the center of the upper and lower end vertebrae of the curve (main thoracic length) (Fig. 1), and the length between T1 and L5 was defined as the distance between the center of the T1 vertebra and the L5 vertebra (T1–L5 length). Measurements were made from standing X-rays before surgery and 1 month after surgery. The center of the vertebra was defined as the point of intersection of the vertebral diagonals. The Cobb angles of the main thoracic curve and lumbar curve were measured, and the number of fused vertebrae was counted. Correlations were then examined between the correction of the main thoracic curve and the increase in the main thoracic length, and between the correction of the main thoracic curve and the increase in T1–L5 length, by linear regression analysis. The patients were divided into ASF and PSF groups to evaluate the influence of the surgical approach on the increase in spinal length.
Fig. 1.
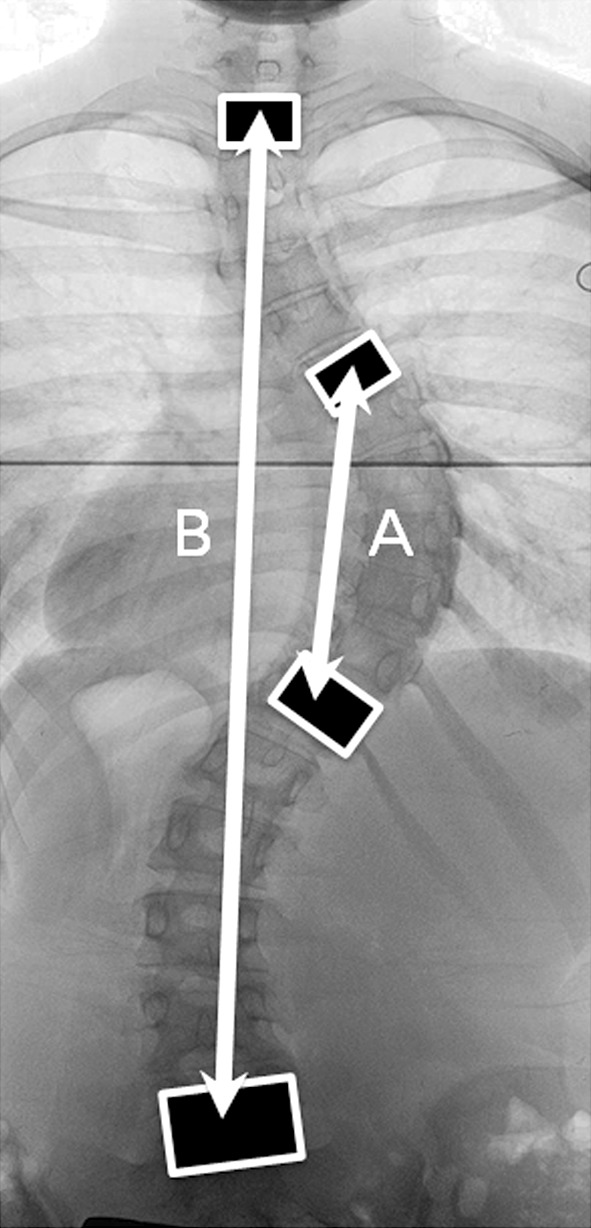
Spinal longitudinal length. Spinal longitudinal length was measured at the main thoracic curve (a) and at T1–L5 (b). The main thoracic length was the distance between the upper and lower end vertebrae of the main curve. The T1–L5 length was the distance between the T1 and L5 vertebrae
All measurements were performed on digitized X-ray films, using a computer workstation (CIS-Image/Viewer for Windows, version 2.6.13; IBM Japan, Tokyo, Japan). Coronal balance was indicated as a distance between C7 plumb line (C7PL) and center of sacral vertical line (CSVL). Deviation of the C7PL to the right side of the CSVL was indicated as plus value. The sagittal balance was indicated as a distance between C7PL and posterior upper endplate of sacrum. Forward deviation of the C7PL was indicated as plus value. Data were statistically analyzed using the SPSS 16.0 J statistical software package. The Chi-square test was used to compare the proportion of gender and curve type (types 1 and 2) between the ASF and PSF groups. One-way factorial ANOVA was used to compare the proportion of lumbar modifiers between the ASF and PSF groups. The Mann–Whitney U test was used to compare the mean height, weight, age, number of fused vertebrae, and radiographical parameters between the ASF and PSF groups. A paired t test was used to compare the mean correction of the Cobb angle and the mean increase in spinal length. Correlation between the correction of the Cobb angle and the increase in spinal length was evaluated using linear regression analysis. Statistical significance was defined as p < 0.05 for a two-sided hypothesis.
All measurements were performed by the first author. The intra-observer reliability was assessed by measuring the every parameter on the selected images from 10 patients at three different times on different days. The inter-observer reliability was assessed by comparing the measurement results of every parameter on the selected images from the 10 patients by the first and second (NH) authors.
Results
The mean height, weight, age, gender, and proportion of lumbar modifiers were equivalent between the ASF and PSF groups (Table 1). However, the proportion of Lenke type 1 patients was significantly higher in the ASF group (p = 0.005). The mean number of fused vertebrae was significantly greater in the PSF (6.6 ± 1.4 vs. 10.7 ± 1.4, p < 0.001), and the mean correction rate and mean correction of the main thoracic Cobb angle were superior in the PSF group (Table 2). The mean preoperative and postoperative Cobb angles of the lumbar curve were equivalent between the two groups.
Table 2.
Results of radiographical parameters
| ASF | PSF | |
|---|---|---|
| Number of fused vertebrae† | 6.6 ± 1.4 (4–9) | 10.7 ± 1.4 (7–15) |
| Cobb angle of preop. main thoracic curve (º)* | 54.9 ± 8.3 (41–83) | 58.8 ± 11.6 (36–107) |
| Cobb angle of postop. main thoracic curve (º)* | 19.7 ± 9.5 (0–47) | 17.1 ± 7.6 (0–49) |
| Correction rate of main thoracic curve (%)† | 64.0 ± 16.8 (23–100) | 71.0 ± 11.2 (37–100) |
| Correction of Cobb angle (º)† | 35.2 ± 11.1 (10–74) | 41.7 ± 10.2 (21–73) |
| Preop. main thoracic curve length (mm)* | 154.3 ± 27.1 (98–217) | 143.6 ± 27.8 (83–223) |
| Postop. main thoracic curve length (mm)* | 155.9 ± 26.3 (105–219) | 157.6 ± 28.7 (90–238) |
| Increase in main thoracic curve length (mm)† | 1.5 ± 4.6 (−8 to 13) | 14.0 ± 5.2 (0–42) |
| Preop. T1–L5 length (mm)* | 376.9 ± 25.8 (313–431) | 371.9 ± 28.2 (286–448) |
| Postop. T1–L5 length (mm)* | 393.4 ± 23.2 (343–440) | 404.5 ± 27.7 (326–483) |
| Increase in T1–L5 length (mm)† | 16.6 ± 7.7 (−3 to 51) | 32.4 ± 10.8 (10–61) |
| Preop. lumbar curve Cobb angle (º)* | 34.1 ± 10.1 (20.0–63.8) | 34.1 ± 8.9 (17.1–60.6) |
| Postop. lumbar curve Cobb angle (º)* | 10.9 ± 8.7 (0.0–28.9) | 10.1 ± 7.3 (0.0–36.8) |
ASF anterior spinal correction and fusion, PSF posterior spinal correction and fusion
* No significant difference by Mann–Whitney U test between ASF and PSF group
†p < 0.001 by Mann–Whitney U test between ASF and PSF group
Increase in spinal longitudinal length after surgery (ASF group)
In the ASF group, the mean preoperative Cobb angle of the main thoracic curve was 54.9 ± 8.3°, and it was corrected to 19.7 ± 9.5°, with the mean correction of the Cobb angle of 35.2 ± 11.1°. The mean preoperative thoracic kyphosis was 16.7 ± 11.0° and the value significantly increased to 20.1 ± 7.6° after surgery with the mean increase of 3.5 ± 9.6° (p < 0.001). The preoperative coronal balance of the patients in the ASF group was −4 ± 15 mm and the value significantly increased to 4 ± 15 mm after surgery (p < 0.001). The preoperative sagittal balance was −5 ± 50 mm and the value significantly increased to 22 ± 63 mm after surgery.
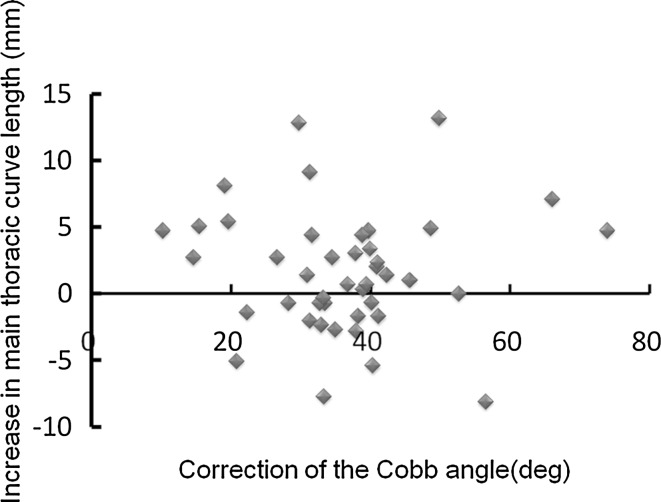
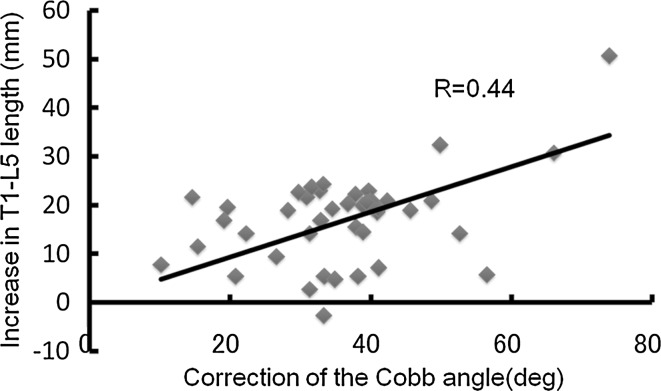
The mean preoperative main thoracic length was 154.3 ± 27.1 mm, and significantly increased after surgery, with a mean increase in length of 1.5 ± 4.6 mm (p = 0.026). Although the mean increase in length after surgery was statistically significant, regression analysis indicated no significant correlation between the correction of the Cobb angle and the increase in length (Fig. 2). The mean preoperative T1–L5 length was 376.9 ± 25.8 mm and the value significantly increased after surgery, with a mean increase of 16.6 ± 7.7 mm (p < 0.001). The regression analysis indicated that the correlation between the Cobb angle correction and increase in T1–L5 length was significant, with a correlation coefficient of 0.44 (Fig. 3).
Fig. 2.
Increase in main thoracic length and correction of the Cobb angle by ASF. Linear regression analysis indicated no significant correlation between the correction of the Cobb angle and increase in the main thoracic length
Fig. 3.
Increase in T1–L5 length and correction of the Cobb angle by ASF. Linear regression analysis indicated a moderate correlation between the correction of the Cobb angle and increase in T1–L5 length, with a correlation coefficient of 0.44
Increase in spinal longitudinal length after surgery (PSF group)
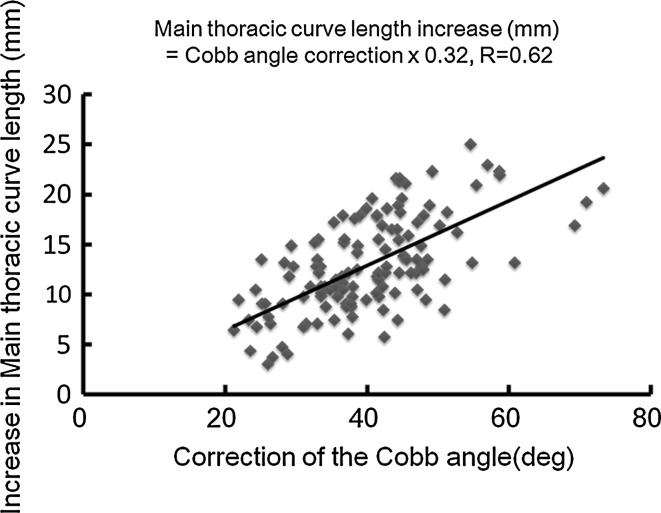
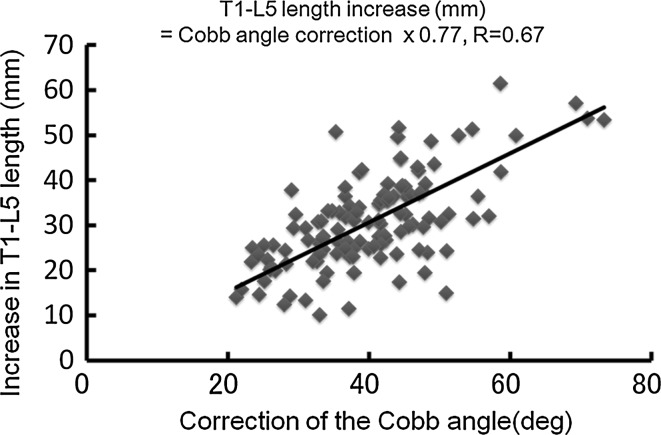
In the PSF group, the mean preoperative Cobb angle of the main thoracic curve was 58.8 ± 11.6°, and it was corrected to 17.1 ± 7.6° with the mean correction of the Cobb angle of 41.7 ± 10.2° (range 21–73°). The mean preoperative thoracic kyphosis was 15.2 ± 13.1°, and no significant change was recognized after surgery (16.8 ± 6.8°). The preoperative coronal balance of the patients in the PSF group was −5 ± 16 mm and the value significantly increased to 5 ± 21 mm after surgery. The preoperative sagittal balance was −8 ± 38 mm and the value significantly increased to 22 ± 74 mm after surgery (p < 0.001). The mean preoperative main thoracic length was 143.6 ± 27.8 mm, and it increased significantly after surgery with a mean increase in length of 14.0 ± 5.2 mm (p < 0.001). Regression analysis indicated that the correlation between the correction of the Cobb angle and the increase in main thoracic length was significant, with a correlation coefficient of 0.63 (Fig. 4). The mean preoperative T1–L5 length was 371.9 ± 28.2 mm, and it increased significantly after surgery with a mean increase of 32.4 ± 10.8 mm (p < 0.001). Correlation between the correction of the Cobb angle and the increase in T1–L5 was significant as well, with a correlation coefficient of 0.64 (Fig. 5). The relationship between the increase in T1–L5 length and correction of the Cobb angle was indicated by linear regression analysis as follows: increase in T1–L5 length (mm) = correction of the Cobb angle (º) × 0.77.
Fig. 4.
Increase in main thoracic length and correction of the Cobb angle by PSF. Linear regression analysis indicated a high correlation between the correction of the Cobb angle and increase in main thoracic length, with a correlation coefficient of 0.63
Fig. 5.
Increase in T1–L5 length and correction of the Cobb angle by PSF. The correlation between the correction of the Cobb angle and increase in T1–L5 length was high, with a correlation coefficient of 0.64. Linear regression analysis indicated the relationship between the increase in T1–L5 length and correction of the Cobb angle to be: increase in T1–L5 length (mm) = correction of the Cobb angle (º) × 0.77
Regarding the intra-observer reliability, the interclass correlation coefficient was 0.995 for the Cobb angle of MT curve, 0.969 for thoracic kyphosis, 1.00 for main thoracic length, and 1.00 for T1–L5 length. While regarding the inter-observer reliability, the interclass correlation coefficient was 0.992 for the Cobb angle of MT curve, 0.920 for thoracic kyphosis, 0.996 for main thoracic length, and 0.998 for T1–L5 length. The interclass correlation coefficient of more than 0.8 indicates almost perfect agreement.
Discussion
The prediction of original body height or height loss for patients with scoliosis has been reported previously [4–11], but most studies have not considered the lengthening effect by corrective surgery. The present study showed that the correction and fusion surgery for AIS significantly increased the spinal longitudinal length, and the increase was highly correlated with the correction of the Cobb angle, especially in the PSF group (R = 0.64). In the PSF group, the increase in T1–L5 length could be approximated by the following equation: increase in T1–L5 length (mm) = correction of the Cobb angle (º) × 0.77. In the ASF group, although the length significantly increased after surgery, the correlation between the increase in length and correction of the Cobb angle was lower than in the PSF group, and the increase in T1–L5 length was approximately half that of the PSF group (17 ± 9 vs. 32 ± 11 mm). The lower correlation and smaller length increase in the ASF group may have been due to the shortening effect of the disc removal and compression occurring during the anterior procedures.
In the PSF group, we decided not to adjust the equation considering the influence of thoracic kyphosis since the mean preoperative thoracic kyphosis did not significantly change after surgery. While in the ASF group, the mean preoperative thoracic kyphosis of 16.7 ± 11.0° significantly increased to 20.1 ± 7.6° after surgery. Although the changes might have influenced the increases in the longitudinal length, we decided not to adjust the equation since the mean increase in kyphosis was relatively small (3.5 ± 9.6°).
The correlation between increase in T1–L5 length and correction of the Cobb angle was relatively high with the correlation coefficient of 0.67, however, there were still wide variations in correlation. We speculate that the variation may be caused by several factors including height of the patient, curve length, curve magnitude, magnitude and flexibility of compensatory curve, and correction maneuver.
Although the correction of the Cobb angle and increase in spinal length with PSF were highly correlated, we still cannot precisely predict the length increase, because the equation includes the postoperative Cobb angle as one of its variables. However, it is reported that the postoperative Cobb angle can be predicted using stress X-rays, such as side bending [12], fulcrum bending [13], traction [14, 15], and push-prone X-rays [12]. Thus, we can approximately predict the postoperative correction of the curve to be obtained, and therefore estimate the postoperative increase in spinal length.
There are several limitations in the present study. First, the equations were established based not on the real heights of the patients but on longitudinal spinal lengths on standing X-rays. The coronal and sagittal balances of the spine were not included in the equation, because the height was measure between T1 and L5 in the coronal plane. Thus, it is not clear how much the increased longitudinal lengths on X-rays are correlated with the real height increases partially obtained by improvement of balances. However, the changes in the balances were relatively small and the majority of AIS patients was coronally and sagittally balanced, and the impact of the balances may not be large. Second, we cannot predict the long-term increase in the spinal length, although the growth of unfused vertebrae, the correction loss due to crankshaft phenomenon or loosening of the instrumentations may have some impact in the spinal length. Another longitudinal study that evaluates the final height of the patient after correction and fusion surgery should be performed.
In conclusion, we found a correlation between correction of the Cobb angle and the increase in spinal longitudinal length after correction and fusion surgery for AIS. In posterior surgery, the high correlation between the Cobb angle correction and the increase in T1–L5 distance may enable the increase in length to be estimated using the equation: increase in T1–L5 distance (mm) = correction of the Cobb angle (º) × 0.77. This equation could provide spine surgeons, patients, and their parents with valuable information about the possible increase in height brought about by correction and fusion surgery for AIS.
Conflict of interest
None.
References
- 1.Letts RM, Bobechko WP (1974) Fusion of the scoliotic spine in young children. Clin Orthop Relat Res:136–145 [PubMed]
- 2.Hefti FL, McMaster MJ. The effect of the adolescent growth spurt on early posterior spinal fusion in infantile and juvenile idiopathic scoliosis. J Bone Joint Surg Br. 1983;65:247–254. doi: 10.1302/0301-620X.65B3.6841390. [DOI] [PubMed] [Google Scholar]
- 3.Winter R. Scoliosis and spinal growth. Orthop Rev. 1977;6:17–20. [Google Scholar]
- 4.Ylikoski M. Height of girls with adolescent idiopathic scoliosis. Eur Spine J. 2003;12:288–291. doi: 10.1007/s00586-003-0527-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stokes IA. Stature and growth compensation for spinal curvature. Stud Health Technol Inform. 2008;140:48–51. [PubMed] [Google Scholar]
- 6.Bjure J, Grimby G, Nachemson A. Correction of body height in predicting spirometric values in scoliotic patients. Scand J Clin Lab Invest. 1968;21:191–192. doi: 10.3109/00365516809084283. [DOI] [PubMed] [Google Scholar]
- 7.Helms P, Bain SH, Warner JO. Foot and hand length for prediction of vital capacity in scoliotic children. Spine (Phila Pa 1976) 1986;11:746–748. doi: 10.1097/00007632-198609000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Hepper NG, Black LF, Fowler WS. Relationships of lung volume to height and arm span in normal subjects and in patients with spinal deformity. Am Rev Respir Dis. 1965;91:356–362. doi: 10.1164/arrd.1965.91.3.356. [DOI] [PubMed] [Google Scholar]
- 9.Linderholm H, Lindgren U. Prediction of spirometric values in patients with scoliosis. Acta Orthop Scand. 1978;49:469–474. doi: 10.3109/17453677808993264. [DOI] [PubMed] [Google Scholar]
- 10.Torres LA, Martinez FE, Manco JC. Correlation between standing height, sitting height, and arm span as an index of pulmonary function in 6 to10-year-old children. Pediatr Pulmonol. 2003;36:202–208. doi: 10.1002/ppul.10239. [DOI] [PubMed] [Google Scholar]
- 11.Brookenthal KR (2002) Loss of height in scoliosis due to degree of curvature. Scoliosis Res Soc:Exhibit 15
- 12.Vedantam R, Lenke LG, Bridwell KH, Haas J, Linville DA. A prospective evaluation of pulmonary function in patients with adolescent idiopathic scoliosis relative to the surgical approach used for spinal arthrodesis. Spine (Phila Pa 1976) 2000;25:82–90. doi: 10.1097/00007632-200001010-00015. [DOI] [PubMed] [Google Scholar]
- 13.Cheung KM, Luk KD. Prediction of correction of scoliosis with use of the fulcrum bending radiograph. J Bone Joint Surg Am. 1997;79:1144–1150. doi: 10.2106/00004623-199708000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Takahashi S, Passuti N, Delecrin J. Interpretation and utility of traction radiography in scoliosis surgery. Analysis of patients treated with Cotrel–Dubousset instrumentation. Spine (Phila Pa 1976) 1997;22:2542–2546. doi: 10.1097/00007632-199711010-00015. [DOI] [PubMed] [Google Scholar]
- 15.Watanabe K, Kawakami N, Nishiwaki Y, Goto M, Tsuji T, Obara T, Imagama S, Matsumoto M (2007) Traction versus supine side-bending radiographs in determining flexibility: what factors influence these techniques? Spine (Phila Pa 1976) 32:2604–2609. doi:10.1097/BRS.0b013e318158cbcb [DOI] [PubMed]