Abstract
Objective
Imaging of the painful coccyx currently relies on standard and dynamic radiography. There are no literature data on MRI of the coccyx. This examination could provide information on the cause of pain.
Methods
172 patients with severe chronic coccydynia underwent MRI and dynamic radiography of the coccyx.
Results
Disc abnormalities (seen in 70 patients) were related to either the presence of intradiscal liquid effusion (17/70), or abnormality of the endplates similar to Modic 1 changes (38/70), or uncertain abnormalities (15/70). Abnormalities of the tip of the coccyx (seen in 41 patients) were located in the surrounding soft tissues: venous dilatations (18/41), soft tissue inflammation (13/41) and ambiguous images (9/41). Vertebral bone oedema was observed in five cases and a benign tumour was observed once. The type of imaging feature depend broadly on the mobility of the coccyx: the 105 cases with a mobile coccyx mainly presented abnormal features mainly in a disc (63 cases vs. 4 cases for the tip), whereas the 67 patients with a rigid coccyx mainly showed abnormal features at the tip (37 cases vs. 7 for the joints, p < 0.001).
Conclusions
We recommend MRI of the painful coccyx when dynamic radiography fails to reveal clearly a pathological lesion (i.e., normal or slightly increased mobility of the coccyx or a rigid coccyx lacking a spicule).
Keywords: Coccyx, Coccydynia, Coccygodynia, Dynamic films, MRI
Introduction
First-line imaging of the painful coccyx (coccydynia) involves both standard and dynamic radiography. Standard radiography (the oldest technique) enables morphological assessment of the coccyx and classification of the coccydynia into one of the four classes, depending on the shape of the coccyx (as described by Postacchini and Massobrio [11]). More recently, the development of dynamic radiography (also referred to as dynamic X-rays, stress films or weight-bearing X-rays) has enabled the direct measurement of the displacement of the coccyx by comparing a standard, standing position and a painful, sitting position [5]. Dynamic radiography also enables the coccydynia to be classified into one of the four following classes: rigid coccyx, normal mobility (5°–25° of flexion or extension), hypermobility (>25° of flexion) and luxation (rearwards displacement of the coccyx in the seated position, spontaneously reducible in the standing position) [8]. However, these four mobility classes do not have the same diagnostic importance. Luxation and marked hypermobility (>35°) are pathologic. Normal or slightly increased mobility do not enable the physician to draw conclusions as to the cause of the pain. Lastly, a rigid coccyx may bear a bony, pain-causing malformation at its tip called a spicule [4]. However, this malformation is observed in only 15% of cases of coccydynia [4].
Recently, MRI has been indicated as a second-line method for investigation of the coccyx. By analysing the concentration of hydrogen protons in the tissue, MRI can reveal oedema and inflammation—lesions that escape detection with X-rays—and can potentially add value to the aetiological diagnosis of coccydynia and improve our understanding of the mechanism(s) of pain. However, the few studies that report MRI evidence of oedema and inflammation have failed to specify the prevalence of these two features [1, 10]. The objective of the present study was thus to evaluate the value of MRI of the coccyx in a large sample of adult patients suffering from chronic coccydynia, to describe the observed abnormalities, determine their frequency of occurrence and specify the technique’s indications and thus clinical value in this situation.
Patients and methods
In five years, we included 172 patients presenting chronic coccydynia (i.e., lasting for at least two months) with a severe functional impact. All patients were aged 18 or over and had no contraindications to the performance of MRI. None had received cortisone injections in or around the coccyx in the 3 months preceding the MRI examination. Patients with a history of local surgery (resection of the coccyx or a pilonidal cyst) were not included in the study. Magnetic resonance imaging was performed on one of two 1.5-Tesla machines (GE and Siemens) with surface emitter and receiver coils. The patient lay on his/her back and was introduced into the bore head first. Straps were used to reduce body movement. Three different sequences were acquired in all cases: (1) a sagittal T1-weighted spin-echo sequence, (2) a sagittal short tau inversion recovery sequence and (3) an axial T2-weighted fat saturation sequence with contiguous 3-mm slices.
Each MRI dataset was first examined separately by two radiologists with experience in musculoskeletal disorders and then by the attending clinician. In the event of disagreement over the final diagnosis (e.g., ambiguous or poor-quality images), the three physicians met and formed a final consensus diagnosis. Thanks to the availability of recent standard and dynamic radiographic X-ray data, each patient was classified into one of the four coccyx mobility classes described above. The MRI images were compared within a given mobility class and then between mobility classes.
Statistical analysis
Proportions were compared using the Chi-square test. Statistical significance was defined as p < 0.05.
Results
One hundred and seventy-two patients (130 women and 42 men; mean ± SD age: 44 ± 13) presenting chronic coccydynia with a severe functional impact underwent MRI, according to the protocol described above.
Dynamic X-rays
Our series included 105 cases with a mobile coccyx (normal mobility: 41 cases; hypermobility: 38 cases; luxation: 26 cases). The 67 other cases had a rigid coccyx. Thirty-five of the latter had a bony spicule at the tip of the spine, pointing rearwards and downwards; this spicule was also visible (and more clearly visible, in general) on MRI. The other cases of rigid coccyx did not have a spicule and the tip of the spine appeared to be normal.
Magnetic resonance imaging
Here, we report on specifically abnormal MRI features only. The shape of the coccyx, the number of vertebrae and the presence or absence of a spicule can be determined on standard X-rays and were not addressed by the present study.
The abnormal imaging features potentially concerned the sacrococcygeal or intercoccygeal disc and/or the adjacent vertebral endplates, the soft tissue around the lower extremity of the coccyx or the coccygeal vertebral bone.
Disc and/or adjacent vertebral endplates
In 70 of the 172 cases (40.7%), the vertebral endplates of the sacrococcygeal or intercoccygeal disc showed a hyperintense signal on T2 and isointense signal on T1-weighted images. In the majority of these cases (38 out of 70), the image was inhomogeneous, moderately intense, poorly delimited and sometimes associated with a slightly increased intradiscal signal on T2 (Figs. 1, 2). We interpreted this as oedema due to joint inflammation, by analogy with the situation described by Modic et al. [9] for the lumbar spine. In a smaller proportion of cases (17 out of 70), the imaging feature was homogeneous, intense and well delimited and thus suggested the presence of effusion into the disc space (Figs. 3, 4). In 15 of the 70 cases, the feature was too localised, too small or poorly defined and thus prevented us from differentiating between normal and pathological situations.
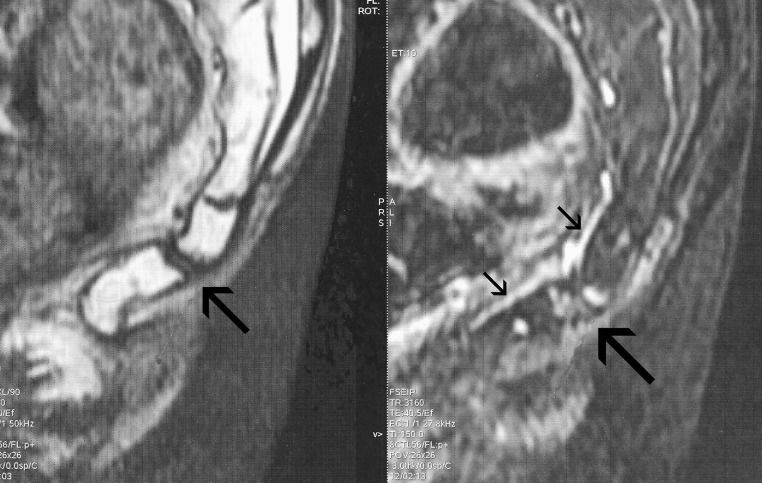
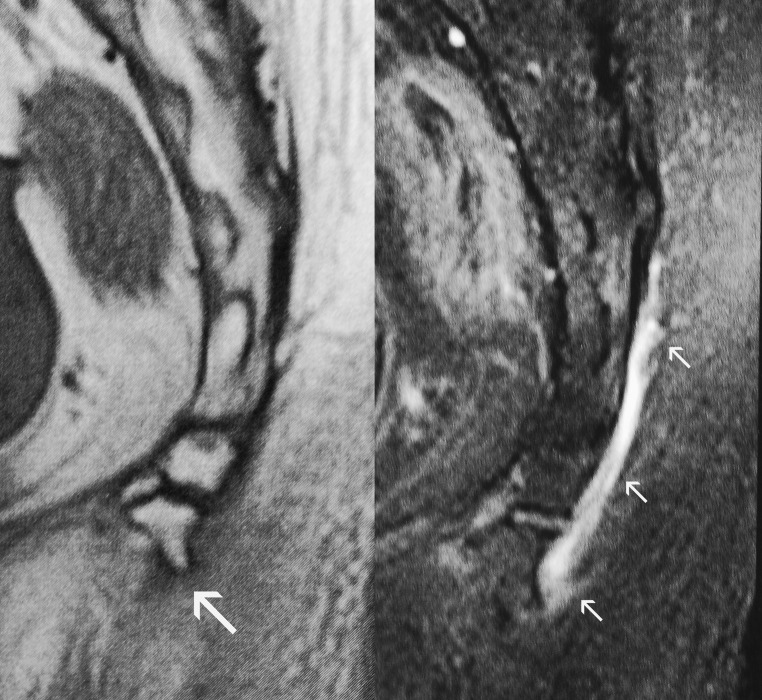
Fig. 1.
A 50-year-old man presenting hypermobility of the coccyx (30° of flexion in the seated position). Left: T1-weighted image showing the coccygeal anatomy. Right: T2-weighted hypersignal (with a short tau inversion recovery sequence) of the intercoccygeal joint and the adjacent vertebral end plates (image on the right, large arrow). Note the presence of a large drainage vein (image on the right, small arrows) on the ventral aspect of the coccyx
Fig. 2.
A 52-year-old man presenting hypermobility of the coccyx (45° of flexion in the seated position). T2-hypersignal of the anterior part of the sacrococcygeal joint and the upper end plate (image on the right). Note the presence of a vein on the ventral aspect of the coccyx
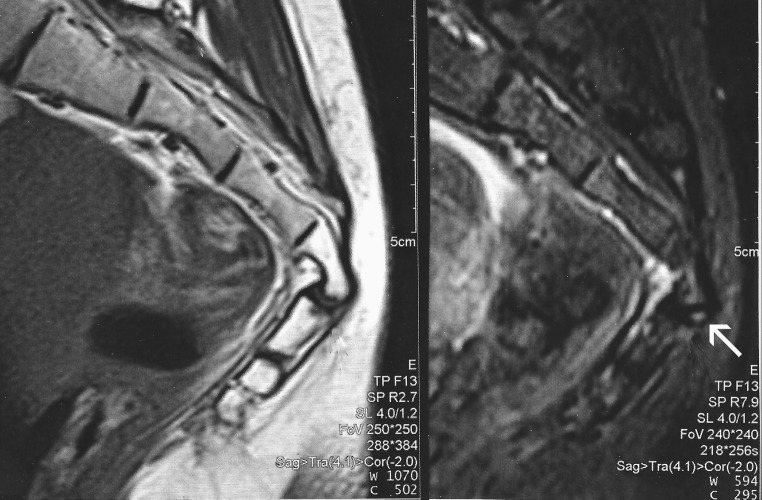
Fig. 3.
A 29-year-old women with hypermobility of the coccyx (35° of flexion in the seated position). Presence of round, well delimited, T2-STIR hyperintense feature situated on the dorsal part of the sacrococcygeal joint (image on the right, arrow). Note the possible liquid collection within the joint
Fig. 4.
A 41-year-old women with hypermobility of the coccyx (35° of flexion in the seated position). The intercoccygeal joint is hypointense with a T1-weighted sequence (image on the left) and hyperintense with a T2-STIR sequence (image on right). The MRI feature is compatible with liquid collection within the joint
When cross-correlating this T2 hyperintense signal with the coccyx mobility pattern, the feature was present in 63 of the 105 cases of mobile coccyx (normal mobility + hypermobility + luxation) versus 7 of the 67 cases of rigid coccyx (p < 0.001). It was most frequent in cases of luxation (18 out of 26). In cases of mobile coccyx, only the mobile disc showed T2 hyperintense signal. If two discs were mobile, only the more mobile of the two showed T2 hyperintense signal. In one case, this feature was visible in a non-mobile disc, whereas the disc above (the sacrococcygeal disc) had normal mobility.
Soft tissues around the lower extremity of the coccyx
In 40 of the 172 cases (23.3%), there was a hyperintense signal on T2-weighted imaging and a isointense signal on T1-weighted imaging in the soft tissues around the lower tip of the coccyx. These signal abnormalities presented two different features. In most cases, the features were tube-like (with significant, well-delimited T2 hyperintensity) and appeared to be linked to the drainage system because of their topography or continuity with the vascular system (18 cases). These structures were most probably veins (Fig. 5). More rarely, the features were not tube-like and had more localised T2 hyperintensity. Some extended upwards along the dorsal face of the coccyx, whereas others extended to the tip (13 cases) (Fig. 6). We interpreted this as inflammation of the soft tissues (moderately hyperintense T2-weighted signal with poorly delimited boundaries) or bursitis (a very intense T2-weighted hypersignal that was well delimited and appear to be separated from adjacent blood vessels). In nine cases, it was impossible to distinguish between these two situations.
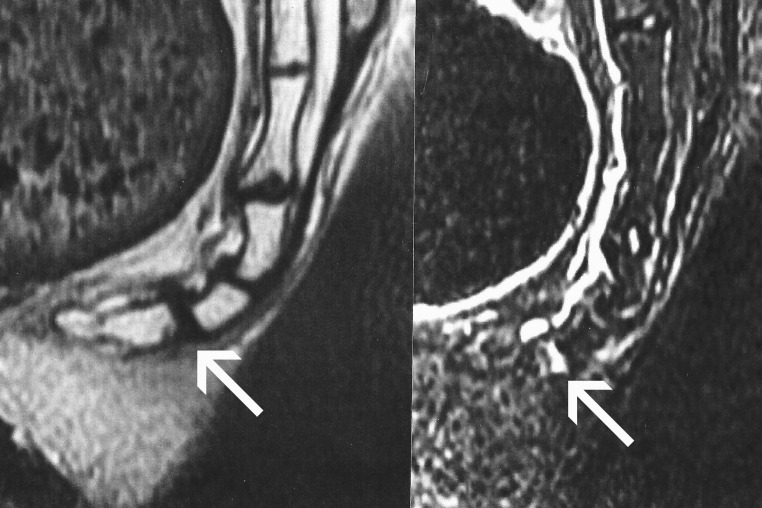
Fig. 5.
A 37-year-old women with a rigid coccyx and no spicule. A T2-hyperintense structure is situated at the tip of the coccyx (image on the right). It is probably of vascular origin because it appears to be joined to a vein situated on the ventral face of the coccyx
Fig. 6.
A 33-year-old women with a rigid coccyx and a small spicule at the tip, visible with a T1-weighted sequence (image on the left). There was also an inhomogeneous hyperintense feature bear the lower tip of the coccyx when a T2 STIR sequence was used (image on the right). The MRI feature is compatible with inflammation of the soft tissues
These features in the soft tissue around the lower tip of the coccyx were only found in 4 of the 105 cases of mobile coccyx (normal mobility, hypermobility or luxation). When the coccyx was rigid (67 cases), they were found 37 times (Chi-square test, p < 0.001).
Image of isolated, diffuse bone oedema
In five cases, a coccygeal vertebra showed a moderately hyperintense signal on T2-weighted images and a isointense signal on T1-weighted images for the whole vertebral body, with no associated joint abnormalities. This image was interpreted as (possibly post-traumatic) bone oedema.
Other features observed
In 35 cases, we observed (either alone or combined with one of the imaging features described above) the presence of a hyperintense signal on T2-weighted images, isointense on T1-weighted images, of variable extent situated on the dorsal face of the coccyx and covering the entire coccyx in some cases (Fig. 7). These MRI characteristics argue in favour of a layer of liquid. Lastly, in one case, we discovered a precoccygeal epidermal inclusion cyst.
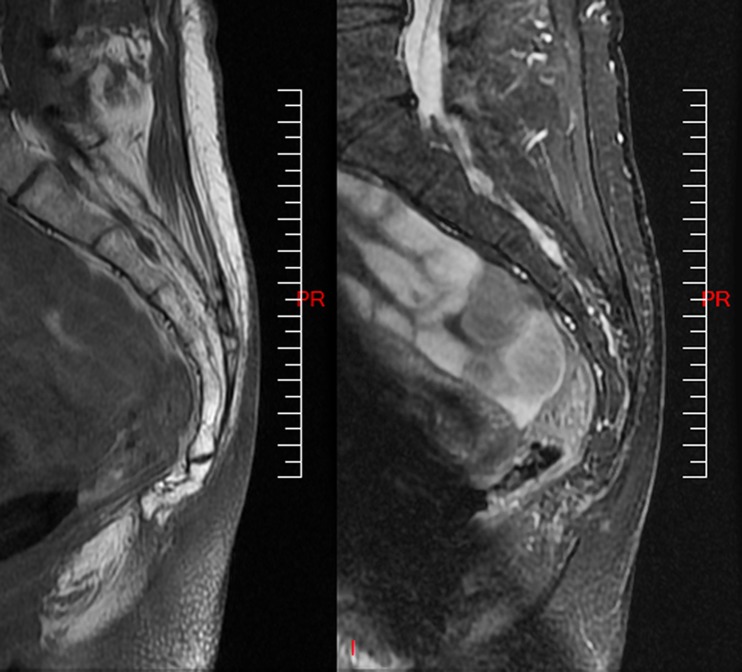
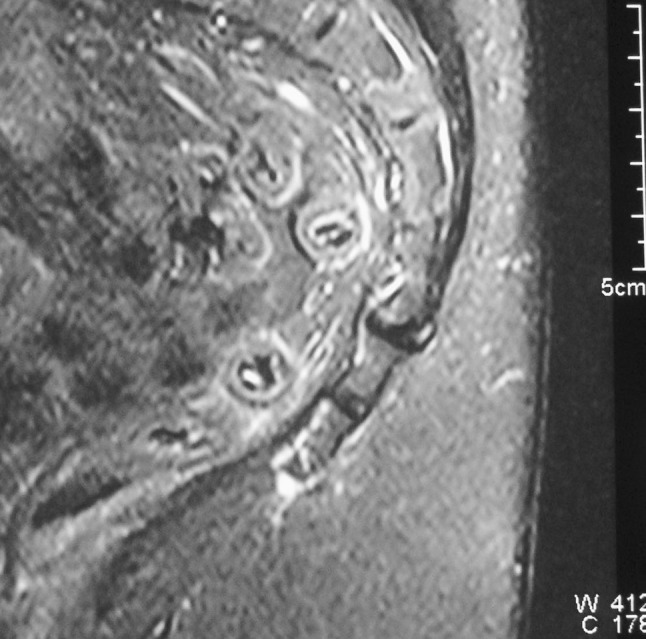
Fig. 7.
A 45-year-old women with a rigid coccyx and a large spicule at the tip, visible with a T1-weighted sequence (image on the left, arrow). Note the presence of a T2 STIR hyperintense feature running along the dorsal face of the coccyx for 4 cm (image on the right, arrows). This MRI feature is compatible with a bursa
Discussion
Few publications have reported on the utility of MRI in coccydynia. A few case reports have demonstrated its value, notably for discovering an epidermal inclusion cyst or a tumour. However, the latter are unusual causes of coccyx pain [2, 3, 12]. In 2004, Fogel et al. [1] reported on the value of MRI of the coccyx in a small series, with the images of oedema of the distal coccygeal segments on the sagittal T2-weighted spin-echo sequences. The only MRI series published in adults is that of Mouhsine et al. [10], who imaged 15 patients suffering from post-traumatic coccygeal instability (luxation). There was intrajoint effusion in all cases and subchondral marrow oedema of the unstable segment in seven cases, which agree with our present observations. However, instability of the coccyx is only one cause of coccydynia. A recent series of 27 adolescents having undergone MRI of the coccyx has been published, with lesions similar to those seen here in adults [7].
Our work had two main limitations. Firstly, the series was not fully representative of chronic coccydynia because we performed MRI only in cases considered to be severe or difficult to treat. This explains why cases of rigid coccyx were over-represented and luxations were under-represented, since each condition usually accounts for about a quarter of cases of chronic coccydynia. Even though luxation may be severe, the fact that it is easy to diagnose and treat makes additional assessment with MRI less important. Secondly, some imaging features were very small or poorly defined. The absence of MRI data on the normal coccyx makes these features more difficult to interpret. However, the large number of reported cases and the correlation with the coccygeal mobility class enabled us to draw some useful conclusions.
To the best of our knowledge, the soft tissue lesions at the lower tip of the coccyx have never previously been described. If this is bursitis, the fact that the coccyx is rigid in most cases is surely related. In the seated position and due to the absence of flexion, tip of the coccyx can exert pressure and friction on the subcutaneous tissues and thus initiate chronic inflammation of the soft tissues. This is probably why this type of lesion is much rarer in patients with a flexible coccyx, which decreases the pressure exerted on the perineum. The same is true for drainage veins, which were found almost exclusively in patients with a rigid coccyx. Likewise, the presence of drainage veins may indicate slight inflammation at the tip of the coccyx and explains the frequency of a blood reflux when a needle is introduced into the area around the tip of the coccyx under fluoroscopic guidance (in our opinion, the latter technique of therapeutic injection is indicated when the coccyx is rigid and the tip is painful).
Disc lesions must be assessed with reference to anatomical knowledge. In fact, the coccygeal disc can be replaced by a synovial joint or by an intermediate structure consisting of a disc traversed by a horizontal cleft of varying length, the walls of which being covered with synovial cells. An anatomical study of ten coccyges of aged subjects revealed a disc structure in six cases (including four with a more or less pronounced cleft) and a synovial joint in four cases [6]. One can thus legitimately expect to see effusion in the coccygeal disc. When the inflammatory reaction affects the over- and underlying vertebral end plates, the MRI feature can be likened to a type 1 Modic sign (decreased signal on T1, and increased signal on T2). Bone oedema is a standard imaging feature after trauma but was rarely found in our series of chronic coccydynia.
We have no definite explanation for the presence of a liquid layer at the dorsal aspect of the coccyx, which we found in 35 cases. Our hypothesis is that it could be a bursa, although it is not described in the anatomical textbooks. This hypothesis is sustained by peroperative findings during coccygeal surgery (Doursounian L. Personal communication).
These results prompt one to question of the role of MRI in the diagnostic work-up for chronic coccydynia. In our experience, MRI is a second-line examination that can follow on from dynamic X-rays, which provide undeniable benefit when correctly acquired from a technical point of view. When dynamic X-rays reveal luxation, marked hypermobility (>35°) or a spicule with undoubtedly pathological features, MRI is not essential. In contrast, for coccyx with normal mobility or limited hypermobility or a rigid coccyx lacking a spicule, MRI can be useful by evidencing an inflammatory reaction around a disc or the pericoccygeal soft tissue or bone oedema. The discovery of these disease-related features can also underpin a hypothesis in which coccygeal injury leads to pain. Lastly, the physician must bear in mind the possible occurrence of a coccygeal tumour.
Conclusion
Our radiographic and MRI-based clinical study enabled us to gain a better understanding of the aetiological mechanisms of pain in chronic coccydynia. The lesions observed by MRI vary depending on the type of coccygeal mobility, which underlines the importance of performing dynamic X-rays. With a rigid coccyx, abnormal MRI features predominate at the tip, whereas lesions are predominantly found in joints in patients with a mobile coccyx. Future studies should attempt to (1) establish a scientific basis for the observed symptoms by determining the MRI appearance of the normal coccyx and then (2) look for prognostic MRI features for predicting the clinical course of coccydynia.
Conflict of interest
None.
References
- 1.Fogel GR, Cunningham PY, 3rd, Esses SI. Coccygodynia: evaluation and management. J Am Acad Orthop Surg. 2004;12:49–54. doi: 10.5435/00124635-200401000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Foye PM. Coccyx pain diagnostic workup: necessity of mri in detecting malignancy presenting with tailbone pain. Am J Phys Med Rehabil. 2002;89:S33. [Google Scholar]
- 3.Jaiswal A, Shetty AP, Rajasekaran S. Precoccygeal epidermal inclusion cyst presenting as coccygodynia. Singapore Med J. 2008;49:e212–e214. [PubMed] [Google Scholar]
- 4.Maigne JY, Doursounian L, Chatellier G. Causes and mechanisms of common coccydynia: role of body mass index and coccygeal trauma. Spine. 2000;25:3072–3079. doi: 10.1097/00007632-200012010-00015. [DOI] [PubMed] [Google Scholar]
- 5.Maigne JY, Guedj S, Straus C. Idiopathic coccygodynia: lateral roentgenograms in the sitting position and coccygeal discography. Spine. 1994;19:930–934. doi: 10.1097/00007632-199404150-00011. [DOI] [PubMed] [Google Scholar]
- 6.Maigne JY, Molinié V, Fautrel B. Anatomie des disques coccygiens. Revue Médecine Orthopédique. 1992;28:34–35. [Google Scholar]
- 7.Maigne JY, Pigeau I, Aguer N, et al. Chronic coccydynia in adolescents: a series of 53 patients. Eur J Phys Rehabil Med. 2011;47:245–251. [PubMed] [Google Scholar]
- 8.Maigne JY, Tamalet B. Standardized radiologic protocol for the study of common coccygodynia and characteristics of the lesions observed in the sitting position: clinical elements differentiating luxation, hypermobility, and normal mobility. Spine. 1996;21:2588–2593. doi: 10.1097/00007632-199611150-00008. [DOI] [PubMed] [Google Scholar]
- 9.Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166:193–199. doi: 10.1148/radiology.166.1.3336678. [DOI] [PubMed] [Google Scholar]
- 10.Mouhsine E, Garofalo R, Chevalley F, et al. Posttraumatic coccygeal instability. Spine J. 2006;6:544–549. doi: 10.1016/j.spinee.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 11.Postacchini F, Massobrio M. Idiopathic coccygodynia: analysis of fifty-one operative cases and a radiographic study of the normal coccyx. J Bone Jt Surg Am. 1983;65(8):1116–1124. [PubMed] [Google Scholar]
- 12.Uglialoro AD, Beebe KS, Hameed M, Benevenia J. A rare case of intraosseous benign notochordal cell tumor of the coccyx. Orthopedics. 2009;32:445. doi: 10.3928/01477447-20090511-22. [DOI] [PubMed] [Google Scholar]