Abstract
Purpose
Patients with adolescent idiopathic scoliosis (AIS) often present with a disfiguring shoulder imbalance. Shoulder balance (Sh.B) is of significant importance to the patient’s self-perception. Previous studies have correlated Sh.B with respect to only the clinical posterior view correlated with radiographs. It is important, however, to address Sh.B with respect to anterior view of the patients’ shoulders as if patients were viewing in a mirror. In this study, we evaluated the anterior Sh.B and correlated it with posterior Sh.B clinically and radiographically in Lenke type 1 and 2 curves.
Method
An online scoliosis database was queried to identify 74 AIS patients with Lenke 1 (n = 55, age 15.28 ± 3.35) and 2 (n = 19, age 15.66 ± 3.72) curves with a complete set of PA radiographs and anterior and posterior photos. Radiographic measures for Sh.B included Cobb angles, T1 tilt, first rib angle, and clavicle-rib intersection angle. Clinical measures for Sh.B included inner shoulder angle, outer shoulder angle, and axillary fold angle. Regression analysis with Pearson’s correlation and ANOVA for statistical significance was used for analysis.
Results
For Lenke 1 curves, there was moderate statistically significant correlation between anterior and posterior clinical Sh.B (R = 0.35–0.41). There was only weak to moderate correlation between radiographic and clinical measures. For Lenke 2 curves, there was a weak to moderate correlation between anterior and posterior clinical Sh.B (R = 0.25–0.45), though not statistically significant. There was no statistically significant correlation between any radiographic measures and posterior Sh.B. There was, however, moderate and significant correlation between radiographic measures and anterior Sh.B.
Conclusion
There is no strong correlation between anterior and posterior clinical Sh.B, and surgeons should evaluate both sides in planning deformity correction, especially in Lenke 2 curves. None of the radiographic measures showed strong correlation (R > 0.8) with anterior or posterior clinical Sh.B. A stronger correlation existed between radiographic measures and anterior Sh.B measurements compared with posterior clinical Sh.B measurements in Lenke 2 curves further necessitating anterior evaluation in this group.
Keywords: Adolescent idiopathic scoliosis, Shoulder balance, Spinal deformity
Introduction
Patients with adolescent idiopathic scoliosis (AIS) often present with characteristic appearance including shoulder imbalance, waist line asymmetry, rib hump, and a prominent trunk shift. Cosmesis for the adolescent patient is an important factor for self-confidence, as studies have shown evidence of psychological distress in this population due to cosmetic concerns [1–4].
Of these cosmetic parameters, shoulder imbalance is easily noticed by the patient especially when viewed face-on in a mirror. Previous studies [5, 6] have shown that there is weak correlation between radiographic parameters and posterior clinical shoulder balance (Sh.B), and the principles of deformity correction involve consideration of not only the correction of radiographic measures but also that of clinical appearance. As an example, correction of only radiographic parameters in Lenke 2 curves may lead to a decompensated shoulder imbalance if the clinical appearance is not considered in surgical planning [7–9]. Anterior Sh.B may be more clinically relevant to the patient’s self-perception, although no study to date has evaluated if the commonly evaluated posterior Sh.B or radiographic parameters are reliable indicators of anterior Sh.B. In this study, we evaluated the anterior Sh.B and correlated it with posterior Sh.B clinically and radiographically in Lenke type 1 and 2 curves. The first purpose of this study is to evaluate the correlation between anterior and posterior clinical shoulder balance in AIS. The second purpose is to evaluate how well radiographic measures of shoulder balance predict clinical anterior shoulder balance in AIS.
Materials and methods
A retrospective review of surgical AIS cases was performed from a prospective online scoliosis database (Scolisoft). The database was queried with the following criteria: Adolescent idiopathic scoliosis, Lenke 1 and 2 curves. The query of the database returned 74 AIS patients with Lenke 1 (n = 55, age 15.28 ± 3.35) and 2 (n = 19, age 15.66 ± 3.72) curves with a complete set of posteroanterior (PA) radiographs, and clinical photographs of anterior and posterior views.
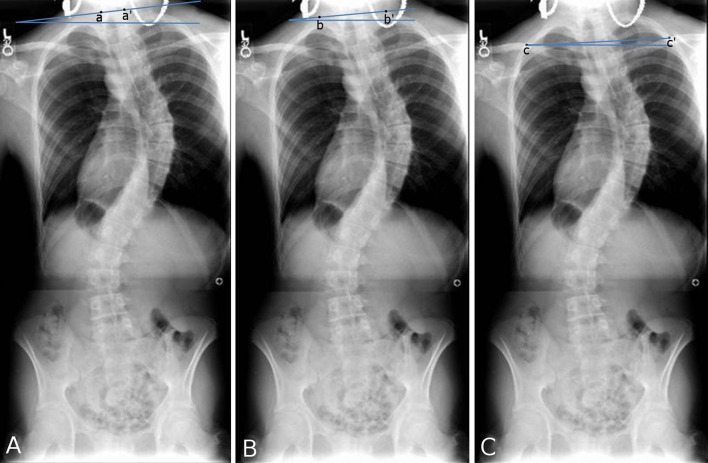
For each case, radiographic measures and clinical measures were evaluated for analysis. Two independent observers not involved in data analysis made all radiographic and clinical measures. Radiographic measures for Sh.B included proximal thoracic (PT) Cobb angle, main thoracic (MT) Cobb angle, T1 tilt, first rib angle (FRA), and clavicle-rib intersection angle (CRIA) (Fig. 1). Main thoracic Cobb angle, T1 tilt, and FRA were previously described measures by Bago et al. and Qiu et al. [5, 10]. T1 tilt is the angle between the line through the superior endplate of T1 and a horizontal line. In all measurements in this study, a positive value indicated a higher right side compared with the left. First rib angle is the angle between the line through the superior borders of the first ribs and a horizontal line. Clavicle rib intersection angle in this study is derived from previously described clavicle-rib cage intersection distance [10], modified to be measured as an angle to keep consistency from multicenter contribution of photographs. Herein, it is the angle between the line through the intersections of the clavicle and first ribs and the horizontal line. Clinical measures for Sh.B included inner shoulder angle (ISA), outer shoulder angle (OSA), and axillary fold angle (AFA) as viewed from anterior and posterior (Fig. 2). Outer shoulder angle is derived from previously described shoulder angle [5, 11], which is the angle between a line drawn through the superior aspect of each acromion and the horizontal line. Inner shoulder angle is defined as the angle between a line drawn through two points on the shoulder at which an initial line that approximates the slope of the distal shoulder intersects the trapezius and the horizontal line. Regression analysis with Pearson’s correlation was used to evaluate relationships between all measures. ANOVA was used to evaluate for statistical significance (P < 0.05).
Fig. 1.
Schematic of radiographic measurements. a T1 tilt angle (a–a′ and horizontal line), b first rib angle (b–b′ and horizontal line), c clavicle rib intersection angle (c–c′ and horizontal line)
Fig. 2.

Schematic of clinical measurements. a Anterior outer shoulder angle (a–a′ and horizontal line), anterior axillary fold angle (b–b′ and horizontal line); b anterior inner shoulder angle (c–c′ and horizontal line); c posterior outer shoulder angle (d–d′ and horizontal line), posterior axillary fold angle (e–e′ and horizontal line); d posterior inner shoulder angle (f–f′ and horizontal line)
Results
All descriptive statistics for clinical and radiographic measures are shown in Table 1. For Lenke 1 curves, there was statistically significant moderate correlation between all anterior and posterior clinical Sh.B measurements (ISA: R = 0.41, P = 2.0 × 10−3; OSA: R = 0.42, P = 0.02; AFA: R = 0.35, P = 0.01). For Lenke 2 curves, there was weak to moderate correlation between anterior and posterior clinical Sh.B measurements (ISA: R = 0.45, P = 0.06; OSA: R = 0.25, P = 0.29; AFA: R = 0.43, P = 0.07), with a trend towards significance in only in ISA and AFA (Table 2). Overall, there was only weak to moderate correlation between radiographic and clinical measures in both Lenke 1 and Lenke 2 curves (Table 3) indicating the unreliability of radiographic measurements as a guide to general appearance. In Lenke 1 curves, posterior clinical measures had moderate statistically significant correlation with the MT Cobb angle (range R = 0.53–0.57), while anterior clinical measures had weak statistically significant correlation with the FRA (range R = 0.32–0.39). In Lenke 2 curves, there was no statistically significant correlation between any radiographic measure and posterior Sh.B. Anterior clinical measures had strongest correlation trends with the MT Cobb angle (range R = 0.264–0.387), T1 tilt (range R = 0.419–0.484), and FRA (range R = 0.466–0.504) than posterior clinical measures.
Table 1.
Descriptive statistics of clinical and radiographic measures
| Clinical measure | Minimum | Maximum | Mean | SD |
|---|---|---|---|---|
| Lenke 1 | ||||
| Posterior inner shoulder | −1.99 | 9.87 | 2.54 | 2.42 |
| Posterior outer shoulder | −3.97 | 8.93 | 2.42 | 2.59 |
| Posterior axillary fold | −3.14 | 12.60 | 4.02 | 3.16 |
| Anterior inner shoulder | −8.75 | 8.83 | 0.89 | 2.65 |
| Anterior outer shoulder | −6.24 | 6.98 | 0.97 | 2.51 |
| Anterior axillary fold | −2.74 | 8.25 | 1.76 | 2.16 |
| Lenke 2 | ||||
| Posterior inner shoulder | −3.85 | 8.53 | 1.76 | 2.84 |
| Posterior outer shoulder | −2.99 | 5.14 | 1.46 | 2.21 |
| Posterior axillary fold | −2.22 | 9.50 | 3.29 | 2.81 |
| Anterior inner shoulder | −10.30 | 7.33 | 0.22 | 3.76 |
| Anterior outer shoulder | −10.05 | 7.18 | 0.23 | 3.48 |
| Anterior axillary fold | −8.39 | 4.87 | 1.09 | 3.23 |
| Radiographic measure | Minimum | Maximum | Mean | SD |
|---|---|---|---|---|
| Lenke 1 | ||||
| Main thoracic Cobb | 30.00 | 93.00 | 56.00 | 12.07 |
| Proximal thoracic Cobb | 9.00 | 50.00 | 24.08 | 8.49 |
| T1 tilt | −11.60 | 15.20 | 1.04 | 5.95 |
| First rib angle | −9.70 | 12.90 | 1.30 | 5.05 |
| CRIA angle | −5.90 | 7.70 | 1.79 | 3.53 |
| Lenke 2 | ||||
| Main thoracic Cobb | 42.00 | 116.00 | 66.74 | 18.93 |
| Proximal thoracic Cobb | 21.00 | 64.00 | 37.74 | 10.07 |
| T1 tilt | −13.00 | 9.50 | −3.25 | 6.36 |
| First rib angle | −9.20 | 12.00 | −0.51 | 6.10 |
| CRIA angle | −5.80 | 8.00 | 0.15 | 3.46 |
Table 2.
Correlation and significance of clinical posterior and anterior shoulder measurements
| Angle measure | Posterior inner shoulder | Posterior outer shoulder | Posterior axillary fold | |||
|---|---|---|---|---|---|---|
| R | P | R | P | R | P | |
| Lenke 1 | ||||||
| Anterior inner shoulder | 0.41 | 2.0E−3* | 0.43 | 1.0E−3* | 0.51 | 9.9E−5* |
| Anterior outer shoulder | 0.33 | 0.02* | 0.42 | 2.0E−3* | 0.50 | 1.5E−4* |
| Anterior axillary fold | 0.41 | 3.0E−3* | 0.42 | 2.0E−3* | 0.35 | 0.01* |
| Lenke 2 | ||||||
| Anterior inner shoulder | 0.45 | 0.06 | 0.24 | 0.32 | 0.29 | 0.23 |
| Anterior outer shoulder | 0.40 | 0.09 | 0.25 | 0.29 | 0.26 | 0.28 |
| Anterior axillary fold | 0.57 | 0.01* | 0.40 | 0.09 | 0.43 | 0.07 |
* p < 0.05
Table 3.
Correlation between clinical and radiographic measurements
| Clinical measure | MT Cobb | PT Cobb | T1 tilt | First rib angle | CRIA | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| R | P | R | P | R | P | R | P | R | P | |
| Lenke 1 | ||||||||||
| Posterior inner shoulder | 0.57 | 7.7E−6* | 0.24 | 0.09 | 0.35 | 0.01* | 0.28 | 0.05* | 0.31 | 0.02* |
| Posterior outer shoulder | 0.52 | 6.5E−5* | 0.25 | 0.08 | 0.21 | 0.12 | 0.22 | 0.11 | 0.30 | 0.03* |
| Posterior axillary fold | 0.53 | 4.9E−5* | 0.23 | 0.10 | 0.23 | 0.10 | 0.16 | 0.26 | 0.28 | 0.04* |
| Anterior inner shoulder | 0.40 | 3.0E−3* | 0.10 | 0.46 | 0.44 | 1.0E−3* | 0.39 | 4.0E−3* | 0.29 | 0.03* |
| Anterior outer shoulder | 0.26 | 0.06 | 0.04 | 0.79 | 0.30 | 0.03* | 0.32 | 0.02* | 0.31 | 0.02* |
| Anterior axillary fold | 0.06 | 0.66 | 0.22 | 0.11 | 0.21 | 0.13 | 0.35 | 0.01* | 0.33 | 0.02* |
| Lenke 2 | ||||||||||
| Posterior inner shoulder | 0.06 | 0.82 | 0.16 | 0.50 | 0.30 | 0.21 | 0.40 | 0.10 | 0.22 | 0.37 |
| Posterior outer shoulder | 0.15 | 0.55 | 0.07 | 0.77 | 0.03 | 0.89 | 0.18 | 0.48 | 0.14 | 0.57 |
| Posterior axillary fold | 0.11 | 0.66 | 0.24 | 0.32 | 0.20 | 0.43 | 0.01 | 0.96 | 0.16 | 0.52 |
| Anterior inner shoulder | 0.39 | 0.10 | 0.24 | 0.33 | 0.48 | 0.04* | 0.50 | 0.03* | 0.48 | 0.04* |
| Anterior outer shoulder | 0.38 | 0.11 | 0.27 | 0.27 | 0.43 | 0.08 | 0.47 | 0.05 | 0.49 | 0.04* |
| Anterior axillary fold | 0.26 | 0.27 | 0.03 | 0.92 | 0.42 | 0.08 | 0.50 | 0.03* | 0.44 | 0.07 |
MT main thoracic Cobb angle, PT proximal thoracic Cobb angle, CRIA clavicle rib intersection angle
* p < 0.05
Discussion
Shoulder balance is an important aspect of overall cosmetic balance in patients with AIS. Factors that contribute to the clinical aspects of shoulder deformity are not thoroughly understood. Attempts to evaluate shoulder balance via radiographic parameters are met with significant challenges due to generally less than moderate correlation between radiographic and clinical parameters [5]. Clinicians often focus on the appearance of the shoulders when viewed posteriorly, although patients may focus on anterior shoulder balance. This may even be more of an issue in countries where clinicians do not clinically examine the patients from the anterior aspect for patient modesty.
Weak to moderate, though statistically significant, correlation was observed between anterior and posterior clinical measures only in Lenke 1 curves. There was no statistically significant correlation between posterior and anterior clinical measures in Lenke type 2 curves. These observations suggest that the perceived shoulder asymmetry viewed posteriorly cannot accurately predict that seen anteriorly in Lenke 2 curves. Previous studies have shown the difficulty of achieving balanced shoulders in Lenke type 2 curves due to the variability of the direction of shoulder imbalance, and specific instrumentation strategies have been proposed based on the direction of the shoulder imbalance in relation to the T1 tilt and main thoracic curve to achieve level shoulders to accommodate this issue [12]. Anterior shoulder balance should be evaluated as a separate component in the surgeon’s consideration of patient’s overall deformity, especially in Lenke type 2 curves.
None of the radiographic measures showed strong correlation (R > 0.8) with anterior or posterior clinical Sh.B. Radiographs are thus not a good indicator of clinical appearance both viewed from anterior and posterior. A stronger correlation existed between radiographic measures and anterior Sh.B measurements compared with posterior clinical Sh.B measurements in Lenke 2 curves. Bago et al. [10] showed moderate correlation between FRA (R = 0.63) and T1 tilt (R = 0.54) with clinical shoulder height and strong correlation of clavicle rib cage intersection, a variant of CRIA (R = 0.90) in series of King types II, III, and V curves. Such a strong correlation between CRIA and shoulder height could be reproduced neither by Qui et al. [5] who reported FRA (R = 0.53), T1 tilt (R = 0.51), and clavicle rib intersection (R = 0.74), nor by us in our study FRA [R = 0.22 (Lenke 1), R = 0.18 (Lenke 2)], T1 Tilt [R = 0.21 (Lenke 1), R = 0.03 (Lenke 2)], CRIA [R = 0.30 (Lenke 1), and R = 0.14 (Lenke 2)]. This is possibly due to the fact that Bago’s study did not include measurements of soft tissues. The lower correlation values in our study could be attributable to the methods of using angular measurements rather than height measurements, although this did not affect statistical significance. Our study is in agreement with Bago et al., and Qiu et al. [5, 10], in that there is a statistically significant correlation of CRIA to all posterior and anterior clinical shoulder measures in Lenke 1 curves and anterior clinical shoulder measures in Lenke 2 curves. Evaluation of anterior and posterior clinical shoulder measures should be considered separately in Lenke 2 curves. The fact that only anterior clinical shoulder measures correlated with radiographic measures in Lenke 2 curves is consistent with our finding that there is no statistically significant correlation between posterior and anterior clinical measures. Our results suggest that radiographic parameters in Lenke type 2 curves relate more closely with anterior shoulder balance than posterior shoulder balance, and a separate assessment of anterior shoulder balance is critical especially in patients with Lenke type 2 curves. Naturally for patients and the clinician, an important objective is to finish with balanced shoulders after the surgery. This study has therefore some surgical implications. From the patient’s perception, anterior shoulder balance seems to be logically the most important goal to achieve. Therefore, clinicians should focus on how to rebalance the shoulders irrespective of how the curve was classified in Lenke classification. In simple right thoracic curves, if the right shoulder is higher than the left from the anterior aspect, correction of the main thoracic curve should suffice. If the shoulders are level from the anterior aspect, care should be taken not to create a left shoulder elevation with too aggressive correction of the main thoracic curve. In the double thoracic curve, if the right shoulder is higher from the anterior aspect, it is in most cases not necessary to include the more proximal left thoracic curve irrespective of Lenke criteria. If the left shoulder is even or higher as seen from the front, the upper thoracic curve should be addressed and the correction should focus more on the upper thoracic curve than the main thoracic curve. Scoliosis correction is an art and starts with a thorough examination of the patient as seen from the posterior and also the anterior aspect.
Conclusions
This is the first study that compared anterior and posterior Sh.B in AIS. Due to the lack of a strong correlation between clinical findings and X-ray parameters, surgeons should not only rely on the latter to evaluate Sh.B in Lenke 1 and 2 curves, but also on the clinical anterior and posterior examination. The Lenke classification and its implications on shoulder balance do not stand in view of this study comparing anterior and posterior shoulder balance and should be further investigated. In double major thoracic curves, the anterior shoulder balance may be a more reliable clinical measure of structural deformity and also correlate better with radiographic parameters.
Acknowledgments
This study was funded in part by Synthes through a research salary grant.
Conflict of interest
None.
References
- 1.Orvomaa E. Psychological evaluations of patients operated for idiopathic scoliosis by the Harrington method. Int J Rehabil Res. 1998;21(2):169–178. doi: 10.1097/00004356-199806000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Danielsson AJ, Wiklund I, Pehrsson K, et al. Health-related quality of life in patients with adolescent idiopathic scoliosis: a matched follow-up at least 20 years after treatment with brace or surgery. Eur Spine J. 2001;10(4):278–288. doi: 10.1007/s005860100309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Payne WK III, Ogilvie JW, Resnick MD et al (1997) Does scoliosis have a psychological impact and does gender make a difference? Spine 22(12):1380–1384 [DOI] [PubMed]
- 4.Asher MA, Burton DC. Adolescent idiopathic scoliosis: natural history and long term treatment effects. Scoliosis. 2006;1(1):2. doi: 10.1186/1748-7161-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qiu XS, Ma WW, Li WG, Wang B, et al. Discrepancy between radiographic shoulder balance and cosmetic shoulder balance in adolescent idiopathic scoliosis patients with double thoracic curve. Eur Spine. 2009;18(1):45–51. doi: 10.1007/s00586-008-0833-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akel I, Pekmezci M, Hayran M, Genc Y, et al. Evaluation of shoulder balance in the normal adolescent population and its correlation with radiological parameters. Eur Spine J. 2008;3:348–354. doi: 10.1007/s00586-007-0546-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Margulies JY, Floman Y, Robin GC, et al. An algorithm for selection of instrumentation levels in scoliosis. Eur Spine J. 1998;7(2):88–94. doi: 10.1007/s005860050036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.King HA. Selection of fusion levels for posterior instrumentation and fusion in idiopathic scoliosis. Orthop Clin North Am. 1988;19(2):247–255. [PubMed] [Google Scholar]
- 9.Arlet V, Reddi V. Adolescent idiopathic scoliosis: Lenke type I–VI case studies. Neurosurg Clin N Am. 2007;18(2):e1–e24. doi: 10.1016/j.nec.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 10.Bago J, Carrera L, March B, et al. Four radiological measures to estimate shoulder balance in scoliosis. J Pediatr Orthop B. 1996;5(1):31–34. doi: 10.1097/01202412-199605010-00006. [DOI] [PubMed] [Google Scholar]
- 11.Yang S, Jones-Quaidoo SM, Eager M, Griffin JW, et al. Right adolescent idiopathic thoracic curve (Lenke 1 A and B): does cost of instrumentation and implant density improve radiographic and cosmetic parameters? Eur Spine J. 2011;20(7):1039–1047. doi: 10.1007/s00586-011-1808-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ilharreborde B, Even J, Lefevre Y, et al. How to determine the upper level of instrumentation in Lenke types 1 and 2 adolescent idiopathic scoliosis: a prospective study of 132 patients. J Pediatr Orthop. 2008;28(7):733–739. doi: 10.1097/BPO.0b013e318185a36b. [DOI] [PubMed] [Google Scholar]