Abstract
The rate of observed dose-limiting toxicities (DLTs) determines the maximum tolerated dose (MTD) in phase I trials. There are cases in which non-drug-related toxicities or other cause toxicities (OCTs) are flagged as DLTs, or vice versa, due to attribution errors. We aim to assess the impact of such errors on the final estimate of MTD. We compared the impact of attribution errors using two trial designs—the “3+3” dose-escalation scheme and the Continual Reassessment Method (CRM). Two attribution errors are considered: when a DLT is classified as an OCT (Type A error) and when an OCT is misclassified as a DLT (Type B error). The impact of these errors on accuracy, patient safety, sample size, and study duration was evaluated by varying the probability of occurrence of each error through simulated trials. Under no errors, CRM is on average 35% more accurate than 3+3 in finding the true MTD. This improved accuracy is maintained in the presence of errors. At a 15% Type B error rate, CRM recommends a dose within 2 levels of the true MTD 68% of the time, compared to 17% of the time using the 3+3 method. A DLT must be attributed as an OCT 30% of the time in order to increase the accuracy of 3+3, otherwise the method recommends a wrong dose approximately 75% of the time. CRM is more robust to toxicity attribution errors compared to the 3+3 since it uses information from all treated patients, leading to a more accurate MTD estimation at the frequency of attribution errors anticipated in phase I clinical trials.
INTRODUCTION
The objective of phase I studies is to establish the safety, dose, and schedule of a new drug or regimen for further clinical development. In general, it is assumed that for cytotoxic agents, higher drug exposure correlates with improved efficacy as measured by tumor responses. Higher drug exposure is also associated with increasing severity (grade) of adverse events (AEs), which are typically measured by standardized criteria such as CTCAE v 4.0. When patients experience a pre-specified, unacceptable rate of dose limiting toxicities (DLTs) at a particular dose level, typically 33% or higher, the trial design declares the level below as the maximum tolerated dose (MTD), which becomes the recommended phase II dose (RP2D) for further clinical development. Serious toxicities that otherwise would be counted as DLTs, if deemed non-drug-related, do not contribute equally in the determination of the MTD. Since the endpoint of phase I trials is the number of DLTs related to the experimental drug, it is essential that clinicians minimize errors when attributing toxicities.
Accurate attribution of toxicities to experimental drug versus other competing factors such as concomitant chemotherapy or medications, cumulative toxicities from previous treatment, disease progression, co-morbidities, and/or intercurrent illness is not always clear. The challenge arises since phase I trials are typically the first in-man studies of novel agents and investigators rely on the drug’s proposed mechanism of action, the toxicities observed in animal studies, and temporal associations. Clinical experience shows that it is sometimes beyond the clinicians’ ability to definitively determine if a given toxicity is due to the study drug, other cause, or combination [1-4]. In these situations, physicians may be inclined to attribute DLTs as possibly related to the study drug as a precaution, to reduce potential patient harm. This may bias DLT attribution against study drugs and lead to underestimation of the MTD. A recent report evaluated causality attribution for serious AEs (SAEs) during phase I oncology studies and concluded that a new causality assessment tool is needed [4]. Moreover, other reports suggest that there might have been over-reporting of SAEs [5] since until recently there were no specific guidelines for drug causality [6]. For this reason, the FDA recently issued a new regulation that clarifies the definition of AEs [7].
In this article, we estimate the impact of attribution errors on the outcome of phase I trials. Given the potential for attribution errors in toxicity assessment and the limited number of patients treated in phase I studies, the established MTD might not necessarily be the same as the true MTD, which corresponds to an acceptable toxicity rate. We address the question of how frequently attribution errors can occur without establishing an MTD that is significantly above or below the actual MTD and what are the implications of attribution errors on drug development? There are two types of errors that might occur in toxicity attribution: 1) when an investigator incorrectly attributes a DLT as an event due to other causes when in fact it is related to the experimental drug (Type A error), and 2) when an investigator incorrectly attributes toxicity to an experimental drug when in fact it is related to other causes (Type B error). A Type A error can result in additional patients being enrolled to higher dose levels and being exposed to toxic levels of the drug, thus adversely affecting patient morbidity and mortality. On the other hand, a Type B error will result in early termination of accrual and denote all levels above as unsafe, consequently recommending a subtherapeutic dose for further studies. This could ultimately result is abandonment of otherwise effective therapies. A Type B error can also lead to unnecessary dose expansion, resulting in an increase in trial duration and cost.
Attribution errors will affect the operational characteristics of various designs in different ways since different designs do not react in the same way in the presence of DLTs. Simulation studies allow us to compare the estimated MTD (RP2D) to the true MTD; thus, we simulated hypothetical rates of DLTs in the presence of attribution errors and evaluated the effect of errors on dose escalation and the RP2D. We compared the impact of attribution errors on two trial designs—the standard design (“3+3”) [8] and the Continual Reassessment Method (CRM) [9]. We hypothesize that adaptive designs that use the accumulated data from all patients are able to reduce the impact of attribution errors when they occur.
METHODS
Data collection
In practice, the true underlying cause of an AE is unknown; hence, investigators cannot know for sure whether the number of DLTs observed in a phase I trial truly corresponds to drug-related SAEs [4]. For this reason, a comparison of different phase I designs must be performed with simulated hypothetical data that are generated under the same circumstances. We followed two prospective dose-escalation algorithms as described below. Regardless of the design, each patient has the same probability of experiencing a DLT at different dose levels; therefore, the dose-escalation algorithm alone determines the trial enrollment and the final MTD [10].
In this comparison we included the 3+3 dose escalation method because it is the most commonly used phase I design [11] and CRM, which is a model-based design. CRM determines whether to escalate, de-escalate or retain the level based on the accumulated data on all cohorts simultaneously and the best estimate of the MTD. Because CRM is an adaptive design, the dose escalation rules are not known in advance, but instead depend on the trial’s history. The design estimates a priori the toxicity rates for each dose level and refines these rates as the trial progresses and more patients are accrued [9].
Dose-Escalation Algorithms
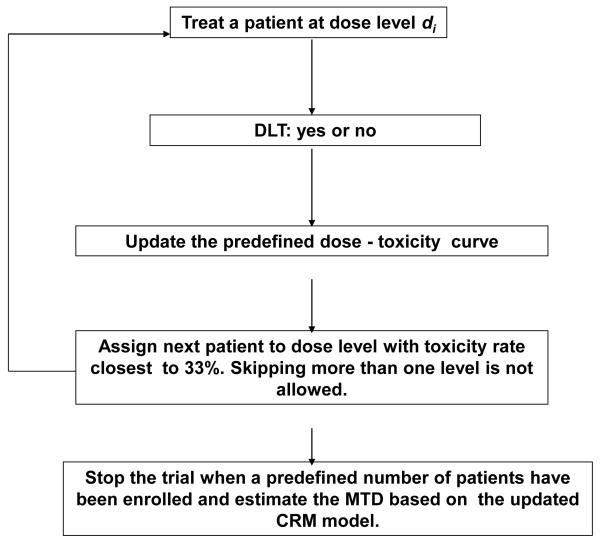
The rules that determine dose escalation for the 3+3 design are shown in Supplemental Table 1. The rules that determine dose escalation for CRM (Figure 1) are as follows:
Prior to the start of the trial, six dose levels are chosen and each dose level is pre-assigned a toxicity rate. For example investigators assign a toxicity rate of 5%, 10%, 20%, 30%, 40% and 50% for dose levels 1 through 6, respectively. As the trial progresses and data regarding DLTs are accumulated, the pre-assigned toxicity rates are refined by sequential estimation such that a dose level associated with a 33% DLT rate is identified [12].
The first dose is the lowest dose.
DLT is evaluated only during the first cycle, which is 21 days in duration.
Skipping dose levels is not allowed in dose escalation, but de-escalation by more than one dose level is permitted.
The trial stops when a pre-specified number of patients have been accrued. Here the sample size is 20 patients. The MTD is the dose recommended based on the updated estimates of toxicity rates based on all 20 patients’ outcomes.
Figure 1.
Dose-escalation algorithm for the Continual Reassessment Method.
Statistical Considerations
For both designs, we simulated 1000 hypothetical trials that tested six dose levels under six scenarios (Table 1) that varied the location of the MTD. We varied the parameter that controls the error rates from 0% to 30% by increments of 5% in different scenarios; however, in each scenario the error rate was constant across levels. [13]. Specifically, we varied the parameter that controls the error rates from 0% to 30% by increments of 5% in different scenarios; however, in each scenario the error rate was constant across levels. For example, Type A error rate is defined as a fixed probability that a true DLT is an other cause toxicity (OCT), irrespective of dose.
Table 1.
True toxicity rates used to simulate the probability of a DLT at each dose level
| d1 | d2 | d3 | d4 | d5 | d6 | |
|---|---|---|---|---|---|---|
| Scenario 1 | 0.10 | 0.17 | 0.22 | 0.30 | 0.45 | 0.50 |
| Scenario 2 | 0.05 | 0.07 | 0.10 | 0.12 | 0.20 | 0.30 |
| Scenario 3 | 0.05 | 0.20 | 0.35 | 0.45 | 0.50 | 0.55 |
| Scenario 4 | 0.01 | 0.05 | 0.10 | 0.30 | 0.50 | 0.70 |
| Scenario 5 | 0.05 | 0.15 | 0.20 | 0.25 | 0.30 | 0.50 |
| Scenario 6 | 0.10 | 0.17 | 0.26 | 0.40 | 0.42 | 0.45 |
We compared the performance of the above designs in terms of the following outcomes:
Accuracy of the final MTD by reporting the percentage of trials that found the correct MTD. If the trial recommended a wrong dose, we plotted how far away it was from the true MTD in terms of number of levels.
Safety (median number of DLTs)
Trial duration (in months)
Sample size (fixed at 20 for CRM, varying for 3+3 by definition)
Trial duration was calculated as described by Iasonos et al [14]. To be concise, in the next section we present simulation results based on two scenarios and accrual rates of 1 or 3 patients per month. Results with various accrual rates were similar to previous reports [14], and therefore were omitted from this paper.
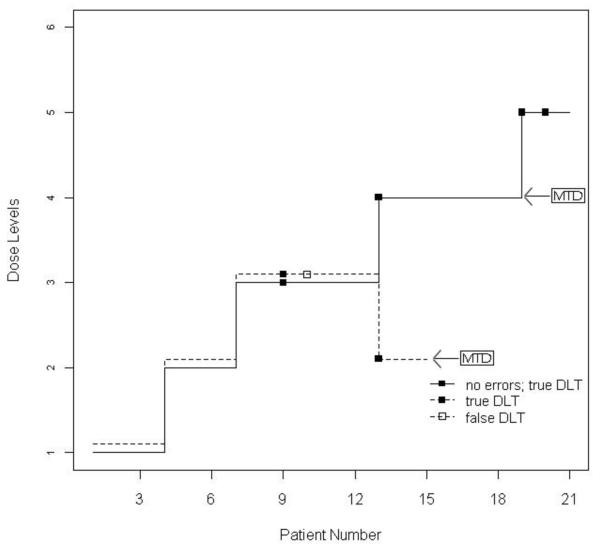
RESULTS
First we present two examples of hypothetical trials corresponding to the 3+3 and CRM designs in the presence of Type B error for illustration. For both designs, each patient treated at dose levels 1 to 6 had a DLT rate of 10%, 17%, 22%, 30%, 45%, and 50% (Scenario 1 in Table 1), respectively, and the true MTD was level 4. Figure 2A shows the trial progress with a 3+3 design in the presence of a Type B error in which one OCT was incorrectly attributed as a DLT (dashed line) at level 3. Since this is the second DLT at that level, the method recommends dose 2 as the MTD. The trial is terminated early with fewer patients; 15 versus 21 if it had reached dose 5. In the absence of error (solid line), level 3 would be the MTD. Note that the two types of errors act in opposite directions, so that one reduces the effect of the other. . However, we expect the Type B error rate to be greater than the Type A error rate in practice since investigators tend to attribute an event to the study drug when uncertain [4]. Similarly, Figure 2B shows the trial progress with a CRM design in the presence of a Type B error in which one OCT was incorrectly attributed as a DLT (dashed line) at level 3. For comparative purposes, a sample size of 21 patients was used in this example for CRM. Following the dashed line, after observing 2/3 DLTs at dose 3, CRM correctly de-escalated to dose level 2. Data from subsequent patients support that level 3 is not as toxic as initially thought, and allow the method to update the estimated rates and assign patients to higher levels. It takes longer to get to the MTD, since early DLTs drop the doses to lower levels and the method needs subsequent patients without DLTs in order to allow experimentation to higher levels, but the final MTD is the same, which is level 4.
Figure 2.
3+3 (Figure 2A) and CRM (Figure 2B) under no error (solid line) and under Type B error (dashed line) of incorrectly attributing other cause toxicity (OCT) as dose-limiting toxicity (DLT).
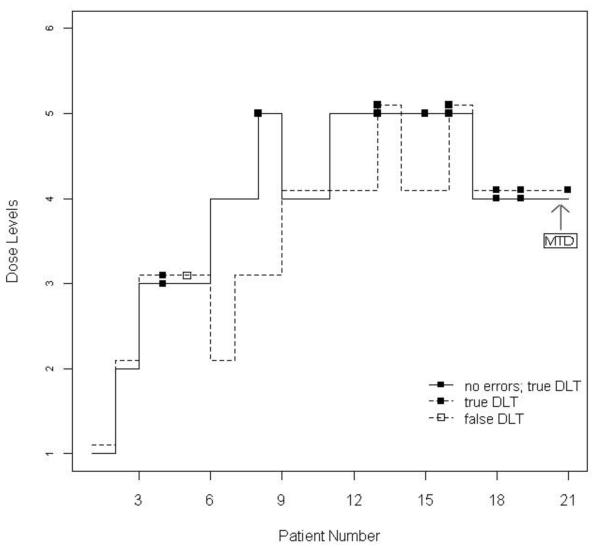
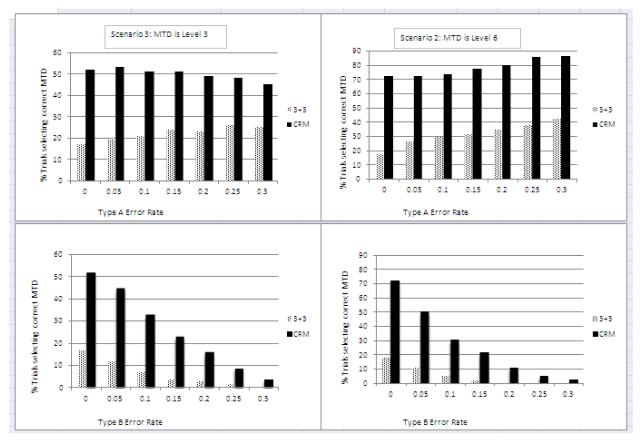
Figure 3 shows the summary results across 1000 simulated trials when dose level 3 (left panel shows Scenario 3) or dose 6 (right panel shows Scenario 2) was assumed to be the true MTD. In the absence of errors, the 3+3 scheme selects the correct MTD (dose 3) 17% of the time, while it selects dose 2 and 1 44% and 32% of the time, respectively. CRM has superior accuracy by selecting dose 3, 2, and 1 with a 52%, 29% and 1% chance, respectively. The right panels of Figure 3 show the scenario when the last dose is the true MTD. In the presence of type B errors, CRM selects a dose closest to the MTD 68% of the time, while 3+3 selects the same dose only 17% of the time.
Figure 3.
Percent of trials recommending each dose level based on simulated trials comparing 3+3 with CRM under Type A and B errors. In the left panel the true maximum tolerated dose (MTD) is level 3 (Scenario 3), and in the right panel the true MTD is level 6 (Scenario 2). NF: dose not found because level 1 was too toxic.
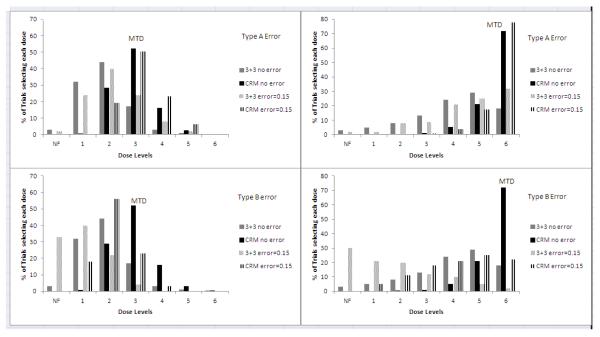
Figure 4 shows how both methods behave as the error rates increase from 0% to 30%. We can see that CRM’s accuracy remains in the presence of Type A error regardless of the location of the MTD, while as the Type B error rate increases, both methods correctly shift recommendation to lower levels below the MTD as they adapt by rejecting levels with a higher than expected number of DLTs. Simulations in which the true MTD was dose 4 and 5 confirmed these findings (data not shown). Misattributing a DLT as an OCT helps the 3+3 method by increasing its accuracy from 18% to 43% (right panel presents Scenario 2) as the error rate is increased. This is because, in certain cases, it can allow the method to proceed to higher levels where activity occurs. Traditionally, the 3+3 design recommends a dose level with an observed rate of less than 33% [15, 16]. By misattributing a DLT as an OCT, the number of DLTs no longer meets the cutoff of 2/6, and the method continues to escalate. The reduced accuracy of the 3+3 is also a result of a smaller sample size and consistently treating patients at lower dose levels as measured by a smaller number of DLTs. When the MTD turns out to be among the higher levels (as in Scenario 2), sample size is larger (21-24 as opposed to 20) and trial duration is longer with the 3+3 (21 vs 20 months), whereas accuracy is much lower compared to CRM (18% vs 73% in the absence of errors). If the MTD is among the first three levels, then trial duration is approximately 5 months shorter with the 3+3, since the trial can be completed with 12-15 patients on average (as opposed to 20 patients needed with CRM), although it recommends the correct MTD in fewer than 1 of 4 trials. Hence, this increase in sample size and resources enables the method to correct its estimate of the MTD, leading to a more accurate and robust RP2D.
Figure 4.
Percent of trials recommending the correct phase II dose based on simulated trials. In the left panel the true maximum tolerated dose (MTD) is level 3 (Scenario 3), and in the right panel the true MTD is level 6 (Scenario 2). Type A Error: incorrectly attributing a dose-limiting toxicity (DLT) as other cause toxicity (OCT); Type B Error: incorrectly attributing an OCT as a DLT.
Thus far, the CRM design was set to target a 33% rate of observed DLTs as an acceptable rate. Since the 3+3 design tends to select doses with much lower rates of toxicity, we also include simulations in which CRM targets a level with a 25% (1 in 4) rate of DLTs. Table 2 shows the percent of trials selecting each level as well as the percentage of patients being treated at each level. The results support the previous findings, although the absolute improvement changes (it is not as high). This is expected since the accuracy of any design depends on the true underlying rates and the dose-toxicity curve. The target rate is considered an external parameter, and it offers the flexibility to fine tune the design depending on the disease setting and the respective acceptable toxicity rate.
Table 2.
Results of 1000 simulated trials under true toxicity rates equal to 0.1, 0.17, 0.26, 0.4, 0.42, 0.45 for the 6 levels, respectively, and a target acceptable toxicity rate of 25%. Each error rate varied from 0 to 0.3 by increments of 0.05. Level -1: one level below level 1; NF: dose not found because level 1 was too toxic. Numbers in bold indicate true MTD.
| % Trials selecting each dose | Patients Treated | DLTs | Duration | Sample Size |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||||||||
| Level | NF | −1 | 1 | 2 | 3 | 4 | 5 | 6 | −1 | 1 | 2 | 3 | 4 | 5 | 6 | |||
|
| ||||||||||||||||||
| accrual rate: 1/mos |
||||||||||||||||||
|
| ||||||||||||||||||
| CRM | ||||||||||||||||||
| Error A: 0 | 5 | 24 | 43 | 21 | 5 | 2 | 16 | 28 | 32 | 17 | 5 | 2 | 5 (4,6) | 19.9 | 20 | |||
| 0.05 | 3 | 22 | 41 | 23 | 8 | 3 | 14 | 26 | 33 | 18 | 7 | 3 | 5 (4,6) | 19.9 | 20 | |||
| 0.10 | 4 | 20 | 42 | 23 | 8 | 4 | 14 | 26 | 31 | 18 | 7 | 3 | 5 (4,6) | 19.8 | 20 | |||
| 0.15 | 2 | 15 | 38 | 27 | 12 | 6 | 13 | 23 | 30 | 20 | 9 | 4 | 5 (4,5) | 20.2 | 20 | |||
| 0.20 | 1 | 15 | 35 | 28 | 13 | 7 | 11 | 23 | 30 | 21 | 10 | 6 | 4 (4,5) | 19.8 | 20 | |||
| 0.25 | 1 | 12 | 32 | 30 | 15 | 9 | 11 | 21 | 29 | 21 | 12 | 6 | 4 (3,5) | 20.2 | 20 | |||
| 0.30 | 1 | 7 | 28 | 32 | 18 | # | 10 | 19 | 27 | 23 | 13 | 8 | 4 (3,5) | 19.8 | 20 | |||
| 3+3 | 1 | 8 | 25 | 31 | 27 | 7 | 1 | 1 | 31 | 30 | 21 | 9 | 2 | 0 | 3 (2,3) | 15.1 | 15 | |
| 2 | 7 | 21 | 32 | 27 | 8 | 3 | 1 | 30 | 30 | 22 | 10 | 3 | 0 | 3 (2,3) | 15.7 | 15 | ||
| 0 | 6 | 19 | 30 | 32 | 9 | 3 | 1 | 28 | 29 | 23 | 12 | 3 | 1 | 3 (2,3) | 15.6 | 15 | ||
| 1 | 8 | 16 | 31 | 28 | 11 | 4 | 2 | 27 | 28 | 23 | 11 | 4 | 1 | 3 (2,3) | 16.0 | 15 | ||
| 1 | 7 | 15 | 25 | 31 | 13 | 7 | 2 | 27 | 26 | 22 | 14 | 5 | 2 | 3 (2,3) | 16.9 | 15 | ||
| 1 | 6 | 13 | 25 | 30 | 14 | 8 | 4 | 25 | 26 | 23 | 14 | 6 | 3 | 3 (2,3) | 17.0 | 18 | ||
| 0 | 5 | 13 | 24 | 29 | 17 | 7 | 6 | 25 | 25 | 22 | 15 | 6 | 3 | 3 (2,3) | 17.6 | 18 | ||
| accrual rate: 3/mos |
||||||||||||||||||
| CRM | 5 | 27 | 43 | 19 | 4 | 2 | 17 | 36 | 30 | 12 | 4 | 1 | 5 (3,6) | 7.8 | 20 | |||
| 4 | 24 | 39 | 25 | 6 | 2 | 19 | 36 | 29 | 13 | 3 | 1 | 4 (3,5) | 7.9 | 20 | ||||
| 5 | 22 | 37 | 27 | 6 | 2 | 17 | 35 | 29 | 14 | 4 | 1 | 4 (3,5) | 7.8 | 20 | ||||
| 3 | 18 | 39 | 29 | 8 | 4 | 16 | 33 | 30 | 15 | 5 | 2 | 4 (3,5) | 7.8 | 20 | ||||
| 1 | 15 | 35 | 30 | 12 | 7 | 14 | 32 | 30 | 16 | 5 | 2 | 4 (3,5) | 7.8 | 20 | ||||
| 1 | 11 | 33 | 33 | 13 | 8 | 13 | 31 | 29 | 18 | 7 | 3 | 4 (3,5) | 7.8 | 20 | ||||
| 1 | 11 | 33 | 31 | 15 | 10 | 12 | 31 | 30 | 18 | 7 | 3 | 4 (3,5) (,) | 7.9 | 20 | ||||
| 3+3 | 1 | 8 | 25 | 31 | 27 | 7 | 1 | 1 | 31 | 30 | 21 | 9 | 2 | 0 | 3 (2,3) | 5.6 | 15 | |
| 2 | 7 | 21 | 32 | 27 | 8 | 3 | 1 | 30 | 30 | 22 | 10 | 3 | 0 | 3 (2,3) | 5.8 | 15 | ||
| 0 | 6 | 19 | 30 | 32 | 9 | 3 | 1 | 28 | 29 | 23 | 12 | 3 | 1 | 3 (2,3) | 5.7 | 15 | ||
| 1 | 8 | 16 | 31 | 28 | 11 | 4 | 2 | 28 | 28 | 23 | 11 | 4 | 1 | 3 (2,3) | 5.9 | 15 | ||
| 1 | 7 | 15 | 25 | 31 | 13 | 7 | 2 | 27 | 26 | 22 | 14 | 5 | 2 | 3 (2,3) | 6.2 | 15 | ||
| 1 | 6 | 13 | 25 | 30 | 14 | 8 | 4 | 25 | 26 | 23 | 14 | 6 | 2 | 3 (2,3) | 6.3 | 9 | ||
| 0 | 5 | 13 | 24 | 29 | 17 | 7 | 6 | 25 | 26 | 22 | 15 | 6 | 3 | 3 (2,3) | 6.4 | 18 | ||
| accrual rate: 1/mos |
||||||||||||||||||
| CRM | ||||||||||||||||||
| Error B: 0 | 5 | 24 | 43 | 21 | 5 | 2 | 16 | 28 | 32 | 17 | 5 | 2 | 5 (4,6) | 19.9 | 20 | |||
| 0.05 | 14 | 33 | 35 | 13 | 3 | 1 | 23 | 31 | 28 | 13 | 4 | 1 | 5 (4,6) | 20.0 | 20 | |||
| 0.10 | 29 | 35 | 26 | 9 | 2 | 1 | 32 | 32 | 24 | 10 | 3 | 1 | 6 (5,7) | 19.6 | 20 | |||
| 0.15 | 44 | 34 | 17 | 4 | 1 | 1 | 44 | 30 | 17 | 7 | 2 | 1 | 6 (5,7) | 20.3 | 20 | |||
| 0.20 | 58 | 25 | 14 | 3 | 0 | 0 | 51 | 26 | 16 | 5 | 2 | 0 | 6 (6,8) | 20.0 | 20 | |||
| 0.25 | 74 | 17 | 7 | 1 | 0 | 0 | 62 | 23 | 11 | 3 | 1 | 0 | 7 (6,8) | 19.9 | 20 | |||
| 0.30 | 82 | 12 | 4 | 1 | 0 | 0 | 70 | 19 | 9 | 3 | 1 | 0 | 8 (7,9) | 19.8 | 20 | |||
| 3+3 | accrual rate: 1/mos |
|||||||||||||||||
| 1 | 8 | 25 | 31 | 27 | 7 | 1 | 1 | 5 | 31 | 30 | 21 | 9 | 2 | 0 | 3 (2,3) | 15.1 | 15 | |
| 5 | 14 | 26 | 32 | 17 | 4 | 1 | 0 | 10 | 36 | 29 | 17 | 6 | 1 | 0 | 2 (2,3) | 14.0 | 12 | |
| 8 | 20 | 32 | 24 | 13 | 3 | 0 | 0 | 15 | 40 | 27 | 13 | 4 | 0 | 0 | 2 (2,3) | 13.0 | 12 | |
| 18 | 21 | 33 | 19 | 8 | 1 | 0 | 0 | 21 | 43 | 24 | 9 | 3 | 0 | 0 | 2 (2,3) | 12.3 | 12 | |
| 26 | 23 | 31 | 15 | 5 | 0 | 0 | 0 | 25 | 45 | 21 | 7 | 1 | 0 | 0 | 2 (2,3) | 11.8 | 12 | |
| 38 | 23 | 26 | 10 | 2 | 0 | 0 | 0 | 31 | 46 | 17 | 4 | 0 | 0 | 0 | 2 (2,3) | 11.0 | 12 | |
| 51 | 19 | 22 | 7 | 0 | 0 | 0 | 0 | 36 | 47 | 14 | 3 | 0 | 0 | 0 | 2 (2,3) | 10.5 | 9 | |
| CRM | accrual rate: 3/mos |
|||||||||||||||||
| 5 | 27 | 43 | 19 | 4 | 2 | 17 | 36 | 30 | 12 | 4 | 1 | 5 (3,6) | 7.8 | 20 | ||||
| 12 | 38 | 34 | 13 | 3 | 0 | 25 | 38 | 25 | 9 | 3 | 1 | 5 (4,6) | 7.8 | 20 | ||||
| 27 | 38 | 27 | 6 | 1 | 0 | 34 | 37 | 21 | 6 | 1 | 0 | 5 (4,6) | 7.8 | 20 | ||||
| 45 | 32 | 18 | 5 | 1 | 0 | 45 | 33 | 16 | 4 | 1 | 0 | 6 (5,7) | 7.8 | 20 | ||||
| 58 | 29 | 11 | 2 | 0 | 0 | 51 | 31 | 14 | 3 | 0 | 0 | 6 (5,8) | 7.7 | 20 | ||||
| 74 | 19 | 6 | 0 | 0 | 0 | 61 | 26 | 11 | 2 | 0 | 0 | 7 (6,8) | 7.6 | 20 | ||||
| 85 | 12 | 3 | 0 | 0 | 0 | 69 | 23 | 7 | 1 | 0 | 0 | 8 (7,9) | 7.6 20 | |||||
| 3+3 | accrual rate: 3/mos |
|||||||||||||||||
| 1 | 8 | 25 | 31 | 27 | 7 | 1 | 1 | 5 | 31 | 30 | 21 | 9 | 2 | 0 | 3 (2,3) | 5.6 | 15 | |
| 5 | 14 | 26 | 32 | 17 | 4 | 1 | 0 | 10 | 36 | 29 | 17 | 6 | 1 | 0 | 2 (2,3) | 5.3 | 12 | |
| 8 | 20 | 32 | 24 | 13 | 3 | 0 | 0 | 15 | 40 | 27 | 13 | 4 | 0 | 0 | 2 (2,3) | 4.9 | 12 | |
| 18 | 21 | 33 | 19 | 8 | 1 | 0 | 0 | 21 | 43 | 24 | 9 | 3 | 0 | 0 | 2 (2,3) | 4.6 | 12 | |
| 26 | 23 | 31 | 15 | 5 | 0 | 0 | 0 | 25 | 45 | 21 | 7 | 1 | 0 | 0 | 2 (2,3) | 4.5 | 12 | |
| 38 | 23 | 26 | 10 | 2 | 0 | 0 | 0 | 31 | 46 | 17 | 4 | 0 | 0 | 0 | 2 (2,3) | 4.2 | 12 | |
| 51 | 19 | 22 | 7 | 0 | 0 | 0 | 0 | 36 | 47 | 14 | 3 | 0 | 0 | 0 | 2 (2,3) | 4.0 | 9 | |
DISCUSSION
In this paper, we have integrated the impact of clinicians’ errors in toxicity attribution and the choice of trial design on the estimation of the MTD in phase I trials. We have shown that mistaking a DLT for an OCT, when it occurs less than 15% of the time, will not put patients at significant risk as estimated by the number of DLTs under either method. This is in agreement with reports that have shown that patients participating in phase I trials are not exposed to an increased risk for life-threatening events, having a <0.5% risk of a drug-related fatality [17-22]. We refer to an individual harm when a single patient or a cohort of patients is assigned to a higher dose as a result of an error in toxicity attribution. In the 3+3 design, individual harm is minimal overall because the number of patients treated at a level higher than the MTD will not be more than 3 unless these errors occur very frequently. Under CRM, when DLTs are mistaken as OCTs, the dose may escalate to a level above the true MTD, but additional patients with DLTs will certainly result in de-escalation [23]. Our simulations confirmed that overall only a small number of patients would be exposed to levels higher than the MTD with CRM (20% and 3% at 1 and 2 levels above the MTD, respectively; Table 2).
The two trial designs do behave significantly differently when OCTs are mistakenly attributed as DLTs. Type B errors are probably more common than Type A errors in phase I trials because physicians are less familiar with the side effect profile of new agents and are eager to avoid potential patient harm. A Type B error rate of 30% will stall the 3+3 design at dose 1 (or dose −1 if that is permitted) with high probability (93%), as opposed to 35% when there are no errors (Scenario 3). This illustrates how early DLTs cannot be overridden in the 3+3 design. This is consistent with the findings of other authors who have shown that the 3+3 design is conservative and tends to stop early [24], recommending an incorrect dose on average 75% of the time [14-16, 25, 26]. This is due to the fact that the 3+3 does not utilize the cumulating experience of all the patients accrued in a trial, and instead it only utilizes the DLTs seen in the present cohort. CRM is consistently superior, on average 35% more accurate than the 3+3 in finding the true MTD, and this superior accuracy remains in the presence of attribution errors. This is a result of the adaptive nature of CRM, which allows de-escalation in the presence of DLTs but subsequent re-escalation if acceptable. CRM is a design with memory [27], thus it can quickly correct the estimated rates and acceptable doses even in the presence of attribution error, as long as the error rate is less than 20%.
The above two errors have different implications on the process of drug development. Collective harm refers to the harm we impose on all future patients by recommending a wrong dose for future studies. A phase I trial can only estimate the MTD; the true effective dose has to be determined in a phase II efficacy study, in which trials are powered both for efficacy and toxicity. Unfortunately, different phase I designs would often lead us to different MTDs, and the correct dose can be provided only through theoretical simulations. Two recent reviews [11, 28] showed that there is still reluctance among the investigators to use model-based designs, possibly because they are considered complex. The 3+3 is easy to implement, it requires very few patients if the MTD turns out to be among the first 3 levels, and in a particular setting of a 12-patient study, it can be a short trial. The major limitation, however, is that it leads to a wrong dose approximately 75% of the time, and attribution errors further increase the likelihood that the entire phase II program will be conducted with a suboptimal, possibly invalid dose. Given the narrow therapeutic window for many drugs, the result on drug development may be unrecoverable and would only be mitigated by either (i) including a consistent dose-escalation clause in phase II, which is very rarely done, and/or (ii) by using adaptive dose finding designs. Another alternative is to develop phase I designs that do not group different attribution levels, especially groups that suggest uncertainty such as unlikely, possibly, or probably, into a dichotomous outcome of presence/absence of DLT. However, current designs use DLTs as their endpoint with the assumption that there is no misclassification of drug-related SAEs as DLTs.
We have illustrated that the impact of attribution errors depends on the magnitude of error rates and the rates of true DLTs. Our results depend on the numerical properties of the simulated cases we studied [29, 30], and they are not based on prospective trials. The attribution error rate that occurs in practice in phase I trials is not known. Attribution errors have been noted in the phase III randomized setting [31-33]; however, the reported error rates are likely less than those observed in the phase I setting [4]. For this reason, we evaluated the methods under a number of different parameters and scenarios. However, error rates that change dynamically within a trial and from patient to patient are not addressed in this simulation.
Model-based designs are more accurate and more robust in the presence of clinician attribution errors. The problem of toxicity attribution becomes more relevant as we move into drug combinations of more than one novel agent with neither agent previously being tested in humans [34]. In such a setting, the question of toxicity attribution has no clear answer. Although the expected clinical benefit cannot be known in such early testing, recent work suggests that phase I patients expect some benefit [35]. If we were to justify their participation in a clinical trial that might be more likely to harm them than to provide benefit, then the justification must be that at least the trial will determine the correct dose for future patients. Moreover, if the drug turns out to be efficacious in later testing, then the majority of phase I patients treated under CRM will have received an efficacious dose without the need to expand accrual at the MTD [27].
Supplementary Material
Acknowledgments
Funding: This was work was partially supported by the National Institutes of Health (U01 CA069856 to AI and DS)
Footnotes
Conflicts of interest: The authors have no conflicts of interest to disclose
REFERENCES
- 1.Crowe BJ, Xia HA, Berlin JA, Watson DJ, Shi H, Lin SL, et al. Recommendations for safety planning, data collection, evaluation and reporting during drug, biologic and vaccine development: a report of the safety planning, evaluation, and reporting team. Clin Trials. 2009;6:430–40. doi: 10.1177/1740774509344101. [DOI] [PubMed] [Google Scholar]
- 2.Ellenberg SS, Fleming TR, DL D. Data monitoring committees in clinical trials: A practical perspective. John Wiley & Sons Ltd.; West Sussex, England: 2003. [Google Scholar]
- Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research Guidance for industry and investigators: safety reporting 13 requirements for INDs and BA/BE studies. http://wwwfdagov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM227351pdf.
- 4.Mukherjee SD, Coombes ME, Levine M, Cosby J, Kowaleski B, Arnold A. A qualitative study evaluating causality attribution for serious adverse events during early phase oncology clinical trials. Invest New Drugs. 2011;29:1013–20. doi: 10.1007/s10637-010-9456-9. [DOI] [PubMed] [Google Scholar]
- 5.Sargent DJ, George SL. Clinical trials data collection: when less is more. J Clin Oncol. 2010;28:5019–21. doi: 10.1200/JCO.2010.31.7024. [DOI] [PubMed] [Google Scholar]
- 6.FDA Guideline for industry: clinical safety data management: definitions and standards for expedited reporting. 1995 [Google Scholar]
- 7.FDA Investigational new drug safety reporting requirements for human drug and biological products and safety reporting requirements for bioavailability and bioequivalence studies in humans. Final rule. Fed Regist. 2010;75:59935–63. [PubMed] [Google Scholar]
- 8.Storer BE. Design and analysis of Phase I clinical trials. Biometrics. 1989;45:925–37. [PubMed] [Google Scholar]
- 9.O’Quigley J, Pepe M, Fisher L. Continual Reassessment Method: a practical design for phase 1 clinical trials in cancer. Biometrics. 1990;46:33–48. [PubMed] [Google Scholar]
- 10.O’Quigley J, Paoletti X, Maccario J. Non-parametric optimal design in dose finding studies. Biostatistics. 2002;3:51–6. doi: 10.1093/biostatistics/3.1.51. [DOI] [PubMed] [Google Scholar]
- 11.Rogatko A, Schoeneck D, Jonas W, Tighiouart M, Khuri FR, Porter A. Translation of innovative designs into phase I trials. J Clin Oncol. 2007;25:4982–6. doi: 10.1200/JCO.2007.12.1012. [DOI] [PubMed] [Google Scholar]
- 12.O’Quigley J, Shen L. Continual Reassessment Method: a likelihood approach. Biometrics. 1996;52:673–84. [PubMed] [Google Scholar]
- 13.Zohar S, O’Quigley J. Sensitivity of dose-finding studies to observation errors. Contemp Clin Trials. 2009;30:523–30. doi: 10.1016/j.cct.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 14.Iasonos A, Wilton AS, Riedel ER, Seshan VE, Spriggs DR. A comprehensive comparison of the continual reassessment method to the standard 3+3 dose escalation scheme in Phase I dose-finding studies. Clin Trials. 2008;5:465–77. doi: 10.1177/1740774508096474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garrett-Mayer E. The continual reassessment method for dose-finding studies: a tutorial. Clin Trials. 2006;3:57–71. doi: 10.1191/1740774506cn134oa. [DOI] [PubMed] [Google Scholar]
- 16.He W, Liu J, Binkowitz B, Quan H. A model-based approach in the estimation of the maximum tolerated dose in phase I cancer clinical trials. Stat Med. 2006;25:2027–42. doi: 10.1002/sim.2334. [DOI] [PubMed] [Google Scholar]
- 17.Horng S, Emanuel EJ, Wilfond B, Rackoff J, Martz K, Grady C. Descriptions of benefits and risks in consent forms for phase 1 oncology trials. N Engl J Med. 2002;347:2134–40. doi: 10.1056/NEJMsa021182. [DOI] [PubMed] [Google Scholar]
- 18.Horstmann E, McCabe MS, Grochow L, Yamamoto S, Rubinstein L, Budd T, et al. Risks and benefits of phase 1 oncology trials, 1991 through 2002. N Engl J Med. 2005;352:895–904. doi: 10.1056/NEJMsa042220. [DOI] [PubMed] [Google Scholar]
- 19.Kurzrock R, Benjamin RS. Risks and benefits of phase 1 oncology trials, revisited. N Engl J Med. 2005;352:930–2. doi: 10.1056/NEJMe058007. [DOI] [PubMed] [Google Scholar]
- 20.Muggia FM. Phase 1 clinical trials in oncology. N Engl J Med. 2005;352:2451–3. author reply 2451-3. [PubMed] [Google Scholar]
- 21.Roberts TG, Jr., Goulart BH, Squitieri L, Stallings SC, Halpern EF, Chabner BA, et al. Trends in the risks and benefits to patients with cancer participating in phase 1 clinical trials. JAMA. 2004;292:2130–40. doi: 10.1001/jama.292.17.2130. [DOI] [PubMed] [Google Scholar]
- 22.Sekine I, Yamamoto N, Kunitoh H, Ohe Y, Tamura T, Kodama T, et al. Relationship between objective responses in phase I trials and potential efficacy of non-specific cytotoxic investigational new drugs. Ann Oncol. 2002;13:1300–6. doi: 10.1093/annonc/mdf202. [DOI] [PubMed] [Google Scholar]
- 23.Cheung Y. Coherence principles in dose-finding studies. Biometrika. 2005;92:863–73. [Google Scholar]
- 24.Hamberg P, Ratain MJ, Lesaffre E, Verweij J. Dose-escalation models for combinations phaseI trials in oncology. Eur J Cancer. 2010;46:2870–8. doi: 10.1016/j.ejca.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 25.Zhao L, Lee J, Mody R, Braun TM. The superiority of the time-to-event continual reassessment method to the rolling six design in pediatric oncology Phase I trials. Clin Trials. 2011;8:361–9. doi: 10.1177/1740774511407533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reiner E, Paoletti X, O’Quigley J. Operating characteristics of the standard phase I clinical trial design. J Computational Statistics and Data Analysis. 1999;30:303–15. [Google Scholar]
- 27.O’Quigley J, Zohar S. Experimental designs for phase I and phase I/II dose-finding studies. Br J Cancer. 2006;94:609–13. doi: 10.1038/sj.bjc.6602969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Le Tourneau C, Lee JJ, Siu LL. Dose escalation methods in phase I cancer clinical trials. J Natl Cancer Inst. 2009;101:708–20. doi: 10.1093/jnci/djp079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Conaway MR, Dunbar S, Peddada SD. Designs for single- or multiple-agent phase I trials. Biometrics. 2004;60:661–9. doi: 10.1111/j.0006-341X.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- 30.O’Quigley J, Iasonos A. Handbook of statistics in clinical oncology. CRC Press; 2011. [Google Scholar]
- 31.Hillman SL, Mandrekar SJ, Bot B, DeMatteo RP, Perez EA, Ballman KV, et al. Evaluation of the value of attribution in the interpretation of adverse event data: a North Central Cancer Treatment Group and American College of Surgeons Oncology Group investigation. J Clin Oncol. 2010;28:3002–7. doi: 10.1200/JCO.2009.27.4282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaiser LD, Melemed AS, Preston AJ, Chaudri Ross HA, Niedzwiecki D, Fyfe GA, et al. Optimizing collection of adverse event data in cancer clinical trials supporting supplemental indications. J Clin Oncol. 2010;28:5046–53. doi: 10.1200/JCO.2010.29.6608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mahoney MR, Sargent DJ, O’Connell MJ, Goldberg RM, Schaefer P, Buckner JC. Dealing with a deluge of data: an assessment of adverse event data on North Central Cancer Treatment Group trials. J Clin Oncol. 2005;23:9275–81. doi: 10.1200/JCO.2004.00.0588. [DOI] [PubMed] [Google Scholar]
- 34.Woodcock J, Griffin JP, Behrman RE. Development of novel combination therapies. N Engl J Med. 2011;364:985–7. doi: 10.1056/NEJMp1101548. [DOI] [PubMed] [Google Scholar]
- 35.Locock L, Smith L. Personal benefit, or benefiting others? Deciding whether to take part in clinical trials. Clin Trials. 2011;8:85–93. doi: 10.1177/1740774510392257. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.