Abstract
BACKGROUND
Transdiagnostic cognitive-behavioral treatments for anxiety disorders have been gaining increased attention and empirical study in recent years. Despite this, research on transdiagnostic anxiety treatments has, to date, relied on open trials, or comparisons to waitlist conditions, published benchmarks, or relaxation-based interventions.
METHODS
The current study was a randomized clinical trial examining the efficacy of a 12-week transdiagnostic cognitive-behavioral group treatment in comparison to 12-week diagnosis-specific group CBT protocols for panic disorder, social anxiety disorder and generalized anxiety disorder.
RESULTS
Results from 46 treatment initiators suggested significant improvement during treatment, strong evidence for treatment equivalence across transdiagnostic and diagnosis-specific CBT conditions, and no differences in treatment credibility.
CONCLUSIONS
This study provides evidence supporting the efficacy of transdiagnostic CBT by comparison to current gold-standard diagnosis-specific CBT for social anxiety disorder, generalized anxiety disorder, and panic disorder. Transdiagnostic group CBT has the benefit of potentially easing dissemination and increasing access to evidence based treatments for anxiety without sacrificing efficacy.
Keywords: Transdiagnostic, Cognitive-Behavioral Therapy, Non-Inferiority, Group Therapy
Transdiagnostic cognitive-behavioral treatments for anxiety disorders have been gaining increased attention and empirical study in recent years in response to amassing data suggesting more similarities among anxiety disorder diagnoses than differences [1,2,3]. Symptom overlap tends to be the norm rather than the exception, and several authors have suggested the existence of shared underlying pathology across the anxiety disorders [1, 4, 5]. Additionally, rates of co-occurring Axis I disorders are extremely high, with comorbidity among the anxiety and depressive disorders reaching approximately 55%[6]. Transdiagnostic treatments are designed to focus on the commonalities among the anxiety disorders, and recent studies have suggested that transdiagnostic CBT can be beneficial for clients with co-occurring anxiety and depressive disorders [7] and complex anxiety diagnoses such as anxiety disorder not otherwise specified [8].
Additional impetus to investigate transdiagnostic treatment protocols relates to practical issues that often arise in providing anxiety treatments in clinical settings. Transdiagnostic group CBT may be preferable in settings where it is not feasible to provide a variety of diagnostically homogeneous groups[9], such as sparsely populated regions where it would be difficult to populate diagnosis-specific groups in a timely manner, or settings with a high demand for services and limited resources for providing individual or diagnosis-specific group treatments. Furthermore, the dissemination of empirically supported treatments for anxiety may be eased with transdiagnostic CBT since therapists could receive training in a single CBT treatment for anxiety rather than multiple, disorder-specific treatments[10].
Transdiagnostic treatment models have generally shown evidence of efficacy, although the standards of comparison have been limited. Erickson[11], for example, reported the results of an uncontrolled trial of a transdiagnostic group CBT program for 70 individuals with an anxiety disorder diagnosis. His results suggested significant decreases in self-reported anxiety and depression among clients completing the 11-week treatment. Further, six-month follow-up data from 16 participants suggested maintenance of treatment gains. Norton[12] reported the results of an open trial of the transdiagnostic CBGT using mixed-effects regression modeling of session-by-session anxiety data from 52 participants with an anxiety disorder. Results indicated that participants tended to improve over treatment, with no differential outcome for any primary or comorbid diagnoses. Effect sizes (d = 1.68) were comparable to average treatment effects reported in meta-analyses of diagnosis-specific CBT for anxiety diagnoses (see[13,14]). Ellard and colleagues[15] reported data from 15 participants undergoing an open trial of individual transdiagnostic CBT for emotional disorders, reporting that 11 (73%) were treatment responders and 9 (60%) achieved high end-state functioning.
Norton and Hope[16] published the first randomized controlled trial of a 12-week transdiagnostic group treatment and found that approximately 67% of those receiving treatment, as compared to none of the waitlist controls, showed a reduction in diagnostic severity to subclinical levels. In a secondary analysis of the treatment data, Norton et al.[17] also noted significant decreases in depressive symptoms and the diagnostic severity of depressive disorders among those receiving treatment. Erickson et al.[18] also randomized 152 patients to either an 11-week CBGT program or a delayed treatment control condition. The immediate treatment group improved more than the delayed treatment controls at post-treatment. When diagnostic categories were examined separately, however, only patients with primary panic disorder showed greater improvement than controls, possibly due to the reduced sample sizes of these subgroup analyses. In a randomized clinical trial of a similar transdiagnostic anxiety treatment, Schmidt et al.[19] found that post-treatment outcomes on measures of anxiety (d's ranged from 1.31 to 1.62), depression (d = .70), and clinician-rated severity (d = 1.18) were also superior among patients receiving transdiagnostic anxiety treatment compared to waitlist controls. Importantly, these gains were maintained at six-month follow-up. Finally, Craske et al.[20,21] found evidence that a transdiagnostic computer-assisted CBT delivered in primary care settings was superior to usual care[20], and outcomes were similar across diagnoses[21]. Further, their data[21] suggested high acceptability and participation among both patients and practitioners.
Norton[22] described a randomized clinical trial examining the efficacy of a 12-week transdiagnostic group CBT program in comparison to a 12-week comprehensive relaxation training program. Results from 87 treatment initiators suggested significant and statistically equivalent/non-inferior outcomes across conditions, although relaxation was associated with a greater rate of dropout despite no differences in treatment credibility. No evidence was found for any differential effects of transdiagnostic CBT for any primary or comorbid diagnoses.
McEvoy and Nathan[23] utilized a benchmarking strategy—comparing observed effect sizes to those obtained from methodologically-similar studies—to compare the efficacy of their transdiagnostic CBT intervention for anxiety and depression to similar published efficacy trials. Data from 143 participants attending at least three sessions (30 with anxiety disorders, 38 with depressive disorders, 75 with comorbid anxiety and depressive disorders) indicated treatment effect sizes, reliable change indices, and clinically significant change indices that were highly similar to those obtained in methodologically similar diagnosis-specific treatment studies for major depressive disorder or specific anxiety disorder diagnoses.
Finally, Norton and Philipp[24] reported a meta-analysis on the efficacy of transdiagnostic anxiety treatments, and noted a strong average within-group effect (d = 1.29) across studies. Although these previous studies demonstrate the efficacy of transdiagnostic treatments in reducing anxiety symptoms, what is not established is the comparative efficacy of transdiagnostic anxiety treatments to well-established diagnosis-specific group CBT protocols for specific anxiety disorders. The primary aim of the current study was to investigate the efficacy of a transdiagnostic anxiety treatment by comparison to group CBT treatments that specifically target individual diagnoses of panic disorder, social anxiety disorder, and generalized anxiety disorder using a treatment non-inferiority methodology[25]. Non-inferiority methods differ from traditional null hypothesis significance testing in that the null hypothesis tested is of treatment inferiority and the alternative hypothesis, should the null be rejected at α = .05, is of treatment non-inferiority. It was hypothesized that all participants would show a significant reduction in anxiety over the course of treatment, and that outcomes in the transdiagnostic and diagnosis-specific conditions would be non-inferior.
Method
Participants
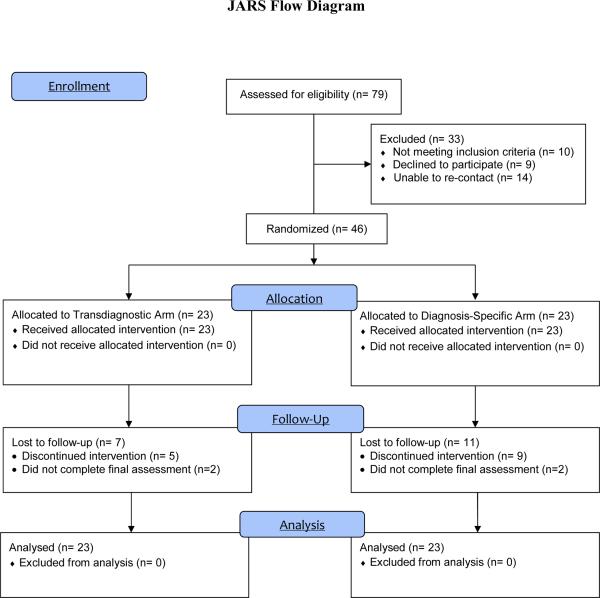
Participants were drawn from 79 individuals who presented to the University of Houston Anxiety Disorder Clinic between April 2009 and August 2010 for treatment services. Inclusion criteria were: (a) age 18 or older, (b) principal DSM-IV diagnosis of panic disorder, social anxiety disorder, or generalized anxiety disorder, (c) adequate proficiency in English, (d) no evidence of dementia or other neurocognitive conditions, (e) absence of serious suicidality, substance use disorder, or other conditions that would require immediate intervention, and (f) willingness to be randomized to treatment condition. Thirty-three of the assessed participants did not participate in the study: 10 were excluded due to not meeting diagnostic inclusion criteria, 9 declined to participant in the trial, and 14 did not return following the assessment and were unable to be reached. Figure 1 presents the JARS flowchart of patient disposition.
FIGURE 1.
JARS flowchart of patient disposition.
Following diagnostic assessment, participants were randomly assigned by the first author to treatment condition blocked by primary diagnosis to ensure similar rates of group enrollment. When a sufficient number (e.g., 3–6) of participants had completed diagnostic assessments and been randomized to treatment condition, they were enrolled in a group. In two instances, Diagnosis-Specific CBT groups were initiated with 3 group members due to slow recruitment of that diagnosis and our unwillingness to unnecessarily delay treatment for these participants. In all, clients from 4 Transdiagnostic (n =23; 12 principal social phobia, 6 generalized anxiety disorder, 5 panic disorder) and 6 Diagnosis-Specific (n = 23; 13 principal social anxiety disorder, 6 panic disorder, and 4 generalized anxiety disorder) groups participated in the study.
The randomized initiator sample consisted of 23 men and 23 women, and was racially diverse (54.3% Caucasian, 23.9% Hispanic/Latino(a), 10.9% African American, 6.5% Asian American, and 4.3% Other or Mixed). The sample ranged in age from 19 to 53 years old, with a mean of 31.46 (SD = 8.93). Most participants were single (60.9%) or married (26.1%), and were fairly well educated (28.3% some undergraduate, 26.1% Bachelors degree or equivalent, 2.2% some professional/graduate school, 17.4% graduate/professional degree).
Measures
All participants were assessed using both clinician-rated measures and self-report measures. Participants received a structured diagnostic assessment at intake, the Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV)[26] including Clinician Severity Ratings for each diagnosis (CSR) and an overall Clinical Global Impressions (CGI), and completed a battery of self-report questionnaires. Participants also completed the State-Trait Anxiety Inventory – state version immediately prior to each session, and a treatment credibility measure following Session 2 of each treatment.
Anxiety Disorders Interview Schedule for DSM-IV
The Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV Adult Version)[26] is a semi-structured diagnostic interview designed to assess the presence, nature, and severity of DSM-IV anxiety and mood disorders. All ADIS-IV interviewers were doctoral students trained to reliability standards and were held blind to treatment condition. Where possible, the same interviewer evaluated the same participant at pre and post-treatment. Post-treatment assessments were conducted by an interviewer who was not involved in providing therapy for that participant or treatment group. Reliability Assessors, who were blind to the original diagnosis, coded DVDs of a random subset of diagnostic interviews and noted very high diagnostic agreement across principal and comorbid diagnoses (86%; κ = .759).
Clinician Severity Ratings (CSR), a component of the ADIS-IV, are subjective ratings applied by diagnosticians to quantify the severity of each disorder diagnosis from 0 (not at all severe) to 8 (extremely severe/distressing). A CSR of 4 (moderate) is considered the cut-off for a disorder of clinical significance[27]. Diagnosticians also completed the Clinical Global Impressions (CGI)[28] scale, a clinician-rated measure of overall severity and therapeutic improvement. As with the ADIS-TV diagnoses, CSR and CGI ratings were made blind to treatment condition. Reliability assessors showed a high degree of consistency in CSR (ICC = .774) and CGI-S (ICC = .727) ratings with the original assessor. CSR and CGI ratings were made at both the pre- and post-treatment assessment points.
State-Trait Anxiety Inventory – State Version
The state form of the State-Trait Anxiety Inventory (STAI)[29] is a 20-item measure designed to assess state anxiety. The psychometric properties of the STAI-S are strong across multiple populations[29] and the measure has demonstrated sensitivity to treatment effects[30]. At Session 1, the STAI was highly internally consistent (α = .92) in the current sample.
Self-report outcome measures
At pre, mid (week 6), and post-treatment assessment points participant completed a battery of self-report questionnaires, including the Panic Disorder Severity Scale (PDSS[31] pre-treatment α = .88), Social Phobia Diagnostic Questionnaire (SPDQ[32] pre-treatment α = .95), Generalized Anxiety Disorder Questionnaire for DSM-IV (GAD-Q-IV[33] pre-treatment α = .80), and Beck Depression Inventory (BDI[34] pre-treatment α = .94). All of these measures have demonstrated excellent reliability and validity, and have sensitivity to clinical change in CBT trials.
Treatment credibility measure
Treatment credibility was assessed using the Borkovec and Nau[35] 4-item measure of treatment rationale credibility immediately following the first session (when the treatment rationale is presented). This measure has been used in several anxiety treatment outcome trials to assess the credibility of competing treatments and psychological placebos[27,36].
Procedure
Assessment and treatment were conducted at the University of Houston Anxiety Disorder Clinic. Participants were recruited for participation via advertisements and articles in local and neighborhood newspapers, referrals from health and mental health professions, and public service media announcements. All methods and procedures were reviewed by the Institutional Review Board of the University of Houston and informed consent was obtained from all participants. Potential participants underwent a telephone screen to assess suitability for the study. Participants who appeared eligible were scheduled for diagnostic evaluation. Following evaluation, eligible participants were randomly assigned to transdiagnostic or diagnosis-specific CBGT.
Treatment protocols and therapists
Treatment in the transdiagnostic CBT condition consisted of 12 weekly two-hour sessions following a manualized treatment protocol[37] (for a description and group case example, see[38]). This protocol deemphasizes diagnostic labels, and focuses instead on challenging and confronting feared stimuli. Below is a brief description of the focus of each session:
-
Session 1.
Psychoeducation, including discussion of genetic and learning factors implicated in the development of anxiety disorders, and the physiological, cognitive, and behavioral manifestations of anxiety.
-
Session 2.
Introduction to cognitive restructuring, including discussion of automatic thoughts.
-
Session 3.
Cognitive restructuring, including identifying thinking errors, challenging thoughts with disputing questions, and developing rational responses.
-
Session 4–Session 9.
Exposure, which is conducted in vivo or through role-played, imaginal, or interoceptive methods depending on client needs and the nature of the feared stimuli, is conducted in session and assigned as part of weekly homework exercises. Where possible, simultaneous exposures are conducted by grouping clients whose exposures may be complementary. In one group, for example, the clients walked to a neighboring office tower that held a busy cafeteria. A socially anxious client asked multiple strangers for directions; a client with claustrophobic fears rode the office elevator multiple floors by herself; a third client, who had concerns about being observed sat by herself for 10 minutes at a table in the middle of the cafeteria; a fourth client who had contamination fears touched surfaces in the cafeteria and refrained from hand washing.
-
Session 10–Session 11.
Advanced cognitive restructuring focusing on global schemas.
-
Session 12.
Conclusion of therapy, dealing with stressors and lapses, and setting post-treatment action plans.
Treatments in the Diagnosis-Specific CBT condition were Craske and Barlow's[39] Mastery of your Anxiety and Panic protocol for panic disorder, Heimberg and Becker's[40] Cognitive-Behavioral Group Therapy for Social Phobia protocol for social anxiety disorder, and Dugas and Robichaud's[41] Cognitive-Behavioral Treatment for Generalized Anxiety Disorder protocol for GAD. These protocols were chosen because they are widely used and were either developed for delivery in a group format or have been previously utilized in trials of group anxiety treatment (e.g.,[27,42,43]). All treatments were adapted for group format according to each authors' recommendations, and were delivered in two-hour group sessions over the course of 12 weeks.
Each group was led by two doctoral-level graduate students who were experienced in providing CBT treatments for anxiety disorders. Therapists were trained in the treatment protocols through video observation of previous groups, and were then paired with senior graduate student co-therapists who had previously delivered the treatments. All sessions were video-taped, and weekly supervision was provided by the first author.
Treatment fidelity
Therapist adherence to the treatment protocols was assessed using the Therapist Adherence Scales created by each protocol's developer. Independent raters evaluated the extent to which several therapy components described in the treatment manual were implemented effectively. Ratings from the different instruments were standardized such that 1.00 represented perfect fidelity and 0.00 represented complete non-fidelity. Overall, raters judged the therapists to be consistent with each of the treatment protocols (Transdiagnostic: Mean = 0.92, sd = .05, range = 0.87 – 1.00; Diagnosis-Specific: Mean = 0.94, sd = .07, range = 0.83 – 1.00; t (8) = 0.42, p = .686), with no single session from any treatment protocol rated out of protocol.
Analytic strategy
Treatment non-inferiority methodologies differ from traditional null hypothesis significance testing approaches in that not significantly different is not synonymous with equivalent or non-inferior. Many factors, including sample size, alpha corrections, and within-group variability, could influence whether or not the null hypothesis was retained despite potentially clinically-significant differences in outcome. Non-inferiority models set a “prestated margin of noninferiority (Δ)” (p. 1153)[25] to determine a maximum difference in outcomes that would be considered as not clinically significant. Mean differences, and 95% confidence intervals (95% CI) around those means, are then utilized to test the null hypothesis of differences across treatment conditions and identify if mean differences in outcomes suggest non-inferiority (rejecting the null hypothesis at α = .05), inconclusive results (failure to reject the null hypothesis as the 95% confidence interval includes Δ), or clear inferiority (failure to reject the null hypothesis and the 95% confidence intervals do not include Δ; see[25,44] for more thorough discussions).
In setting Δ, prior equivalence and non-inferiority trials of CBT for anxiety disorders were consulted[22,45,46]. Margins of noninferiority in these trials, each of which was based on meta-analytic data, ranged from Δ = 0.50 to 0.67 SD below the mean effect of the established treatment arm for each measure (Mean Δ = 0.59). For the current study, Δ was therefore set at 0.6 SD below the Diagnosis-Specific condition mean for each analysis. For example, if the Diagnosis-Specific condition showed a post-treatment score on a hypothetical Measure X (controlling for pre-treatment scores) of Mean = 10, SD = 4, for non-inferiority to be assumed the Transdiagnostic condition would need to show a post-treatment effect, and 95% CI around that effect, on Measure X of +/− [SD = 4 * 0.6] 2.4, or a mean post-treatment score and 95% CI ranging from 7.6 to 12.4. Given that ITT analyses can artificially increase the perception of treatment non-inferiority by reducing variability and narrowing the confidence intervals, the self-report data were analyzed carrying forward data only if the participant completed the mid-treatment assessment.
To fully utilize the entire sample of treatment initiators, session-by-session STAI measures were examined using Mixed-effect Regression Modeling (MRM). MRM can be conceptualized as an extension of linear regression, but with the incorporation of individual-level effects in addition to group-level effects. In essence, individual regression lines are modeled for each participant, such that their severity and change can be expressed as a combination of individual intercept and slope parameters, thereby providing estimates of both the intercept and slope of the sample as well as estimates of the average deviations of individual participants from these intercepts and slopes. Individual data are nested within treatment groups to partial out group-level effects, if any. Missing data are accommodated, as the individual regression lines are fitted to the available longitudinal data, assuming at least two time points are available (for an accessible introduction see[47]). All participants attending at least two sessions were included in the sample. Non-inferiority analyses were conducted to examine whether both the Transdiagnostic mean slope (and 95% CI around the parameter) differ by more than 0.6 SD from that of the Diagnosis-Specific condition.
Analysis of therapist and patient ratings of anxiety was conducted using Analysis of Variance, as opposed to an MRM model, as nested group correlations were small and the design effects (0.03 to 0.36) were well below the 2.0 threshold reported by Muthén and Satorra[48] as indicative of needing to be modeled. Variables were analyzed using between groups ANOVAs (Transdiagnostic vs. Diagnosis-Specific CBT) with pre-treatment scores as covariates. Mean differences and 95% CI were then examined to see if they fell within 0.6 SD of the Diagnosis-Specific mean. Treatment Responder status was defined, consistent with Ellard et al[15], as achieving a 30% or greater reduction of the CSR of their primary diagnosis or a post-treatment primary diagnosis CSR of 3 or lower.
Results
Preliminary Analyses
Fifty-eight participants were randomized to treatment condition. Of those randomized, 12 did not initiate treatment. Rates of pre-treatment attrition did not differ by condition χ2 (1, n = 58) = 0.27, V = .068, p = .607. Given ethical obligations not to delay treatment, group size tended to be smaller for diagnosis-specific (M = 3.29, sd = 1.38) groups than transdiagnostic (M = 5.75, sd = 0.50) groups t(9) = 3.38, p = .008, as populating transdiagnostic groups was faster (i.e., 4 to 6 clients of any diagnosis) than for diagnosis-specific groups (4 to 6 clients of a specific diagnosis) despite the imbalanced randomization.
Of the 23 treatment initiators in the transdiagnostic CBT condition, 12 were assigned principal diagnoses of social anxiety disorder, 6 generalized anxiety disorder, and 5 panic disorder. Similarly, of the 23 treatment initiators assigned to the diagnosis-specific CBT condition, 13 were assigned principal diagnoses of social anxiety disorder, 6 panic disorder, and 4 generalized anxiety disorder. No significant pattern of association was observed between primary diagnosis and treatment condition, χ2 (2, n = 46) = 0.53, p = .767. Similar to other samples in clinical trials of transdiagnostic CBT[21], the treatment initiator sample showed considerable comorbidity, with 58.7% having additional diagnoses including major depressive disorder or dysthymia (n = 17), GAD (n = 8), social anxiety disorder (n = 5), panic disorder with or without agoraphobia (n = 4), specific phobia (n = 3), obsessive-compulsive disorder (n = 3), substance abuse (n = 1), post-traumatic stress disorder (n = 1), tic disorder (n = 1), and bipolar disorder NOS (n = 1). At pre-treatment, no differences emerged between the conditions in terms of demographic variables such as age, sex, race, education, or marital status (Fs = 0.05 – 0.08, ps = .77 – .88; χ2s = 0.09 – 4.06, ps = .40 – .77). Similarly, no differences between conditions emerged at pretreatment on clinician-rated (Fs = 1.61 – 3.25, ps = .08 – .21) or self-report outcome measures (Fs = 0.15 – 1.94, ps = .17 – .71), nor were there differences between conditions in the percent of treatment initiators with comorbid diagnoses, χ2 (1, n=46) = 0.09, V = .044, p = .77.
Attrition
Treatment initiators attended an average of 8.46 sessions (SD = 3.40), with a median of 10 and the modal number being 11. Half of those who discontinued treatment (7 of 14 discontinuers) did so within the first three sessions. No differences in number of sessions attended were observed between transdiagnostic (M = 8.78, sd = 3.34) and diagnosis-specific conditions (M = 8.13, sd = 3.49), F(1,46) = 0.42, p = .52, partial η2 = .009. Similarly, no differences were observed among initiators in treatment discontinuation by condition χ2 (1, n=46) = 1.64, V = .189, p = .20. The attrition rate in this study (30%) is comparable to that reported in other trials of transdiagnostic CBGT (34%)[23] and diagnosis-specific CBGT (20% – 47%)[27,49].
Collapsing diagnosis-specific CBT data
Analyses were next conducted to evaluate the comparability data from participants receiving treatment for panic disorder, social anxiety disorder, or generalized anxiety disorder in the diagnosis-specific CBT condition. No significant differences emerged across diagnoses on primary outcomes (Primary CSR: F(1,13) = 1.33, p = .312; CGI-S: F(1,12) = 0.05, p = .948; CGI-I: F(1,12) = 1.02, p = .393). Data from the diagnosis-specific treatments were therefore collapsed into a single diagnosis-specific condition.
Treatment credibility
Analysis of the Treatment Credibility Measure suggest that those in the transdiagnostic CBGT condition (M = 25.13, sd = 3.60) and those in the diagnosis-specific CBGT condition (M = 24.71, sd = 3.76) did not differ significantly in their perceptions of treatment credibility, F(1,37) = 0.11, p = .74, partial η2 = .003.
Analysis of Session-by-Session Change
To fully utilize the entire sample of treatment initiators, session-by-session STAI measures were examined using Mixed-effect Regression Modeling (MRM). Using a Restricted Maximum Likelihood (REML) estimator, the data were fitted to a random intercepts and slopes model with session-by-session STAI scores serving as a time variant regressor and condition as a time invariant factor. Results indicated that the intercept of the STAI scores (i.e., prior to Session 1) were within the clinical range for both treatment conditions [Transdiagnostic CBGT: Maximum Likelihood Estimate (MLE) = 45.52, Wald z = 18.01, p < .001; Diagnosis-Specific CBT: MLE = 48.70, Wald z = 18.74, p < .001], and, consistent with the hypothesis, similarly decreasing STAI scores were observed over treatment, (Transdiagnostic: MLE = −0.93, Wald z = −4.08, p < .001; Diagnosis-Specific: MLE = −1.06, Wald z = −4.12, p < .001). Constraining the intercepts and slopes to be equal across conditions did not result in decreased model fit (Bayesian Information Criteria constrained: 2934.28; freely estimated: 2941.15) indicating that intercepts (MLE = 47.11) and slopes (MLE = 0.98) were invariant across treatment conditions. Non-inferiority analysis of the slopes, controlling for session 1 intercepts, indicated that the confidence interval of the mean difference in slopes of the STAI did not intersect 0.6 SD (MDiff = −0.029, 95% CI = −0.298 to 0.239, −0.6 SD = −.418), suggesting that transdiagnostic CBT showed non-inferior outcomes in comparison to diagnosis-specific CBT (see Table 1).
Table 1.
Comparison of treatment effects.
| Post-Treatment Mean (se) | ANOVA (Condition) | ||||
|---|---|---|---|---|---|
|
|
|||||
| Measure | Transdiagnostic | Dx-Specific | F | p | partial η2 |
| CSR | 3.15 (0.38) | 2.97 (0.42) | 0.12 | .73 | .004 |
| CGI-S | 2.91 (0.26) | 3.20 (0.29) | 0.44 | .51 | .017 |
| CGI-I | 2.25 (0.19) | 2.08 (0.21) | 0.32 | .57 | .011 |
| PDSS | 5.25 (1.00) | 7.28 (1.00) | 1.47 | .24 | .052 |
| SPDQ | 11.96 (1.48) | 9.90 (1.29) | 1.10 | .31 | .052 |
| GADQ | 15.01 (1.95) | 16.19 (1.81) | 0.19 | .67 | .008 |
| BDI | 8.69 (2.06) | 11.24 (2.06) | 0.76 | .39 | .027 |
| STAI (Slope) | −0.98 (0.09) | −1.01 (0.10) | 0.05 | .83 | .001 |
Notes: Means represent post-treatment estimated marginal means (standard error) after controlling for pre-treatment scores for each condition. For each measure, more positive scores represent greater anxiety severity.
CSR: Clinician Severity Ratings of principal diagnosis; CGI-S: Clinical Global Impressions scale – Severity; CGI-I: Clinical Global Impressions scale – Improvement; PDSS: Panic Disorder Severity Scale; SPDQ: Social Phobia Diagnostic Questionnaire; GADQ: Generalized Anxiety Disorder Questionnaire; STAI (Slope): State-Trait Anxiety Inventory (State version) slopes from mixed-effect regression model.
Pre-Post Outcomes
As noted earlier, Pre-Post outcomes were analyzed in ANOVA models without nesting individual data within treatment groups, as nested group correlations were extremely small and the design effects (0.03 to 0.36) were well below the 2.0 threshold reported by Muthén and Satorra[48] as indicative of needing to be modeled.
Self-report measures
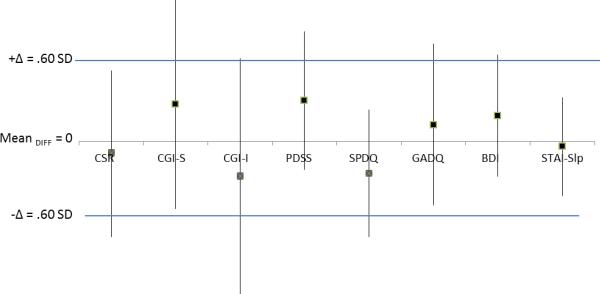
Self-report measures were next analyzed using between-groups ANOVA with respective pre-treatment variables as covariates. Given that ITT analyses can artificially increase the perception of treatment non-inferiority, the self-report data were analyzed carrying forward data only if the participant completed the mid-treatment assessment. These analyses showed no significant differences in outcome by Condition, Fs (1,30) = 0.13 – 1.47, ps = .23 – .72, partial η2s = .005 – .052. Non-inferiority analyses revealed that PDSS, GADQ, IUS, and BDI outcomes in Transdiagnostic CBT were equivalent/non-inferior to Diagnosis-Specific CBT outcomes, while SPDQ scores yielded inconclusive results as the 95% CI of the mean difference intersected Δ of −0.6 SD (Figure 2).
FIGURE 2.
Non-inferiority analyses of mean outcome differences at post-treatment. Note: Square boxes represent mean differences in outcomes, with squares above “Mean DIFF = 0” representing outcomes favoring Transdiagnostic CBT and squares below “Mean DIFF = 0” representing outcomes favoring Diagnosis-Specific CBT. Whiskers represent 95% Confidence Intervals around the mean differences. Boxes represented with an X signify measures where the 95% Confidence Intervals exceed Δ and are thus considered “inconclusive”.
CSR: Clinician Severity Ratings (clinician-rated), CGI-S: Clinical Global Impressions-Severity Scale (clinician-rated), CGI-I: Clinical Global Impression-Improvement scale (clinician-rated), PDSS: Panic Disorder Severity Scale (self-report), SPDQ: Social Phobia Diagnostic Questionnaire (self-report), GADQ: Generalized Anxiety Disorder Questionnaire for DSM-IV (self-report), BDI: Beck Depression Inventory (self-report), STAI-Slp: slope of change for State-Trait Anxiety Inventory-State form (self-report).
Clinician-rated measures
Independent assessors who were blind to treatment condition rated both the severity of primary diagnoses (CSR) and provided an overall assessment of patient severity (CGI-S) and improvement (CGI-I). Each variable was analyzed using between-groups (Condition) ANOVAs with the respective pre-treatment score as a covariate. Improvement following treatment (CGI-I) was also analyzed using a between-groups ANOVA. For primary diagnosis CSR, no effect of condition was observed, F(1,29) = 0.09, p = .766, partial η2 = .003, and no differences in the Percent Responders between those receiving transdiagnostic (64.7%) and diagnosis-specific CBT (69.2%) was observed, χ2 (2, n = 30) = 0.07, p = .794. Non-inferiority analyses, however, were inconclusive as the 95% confidence interval around the mean difference exceeded the pre-stated margin of non-inferiority (MDiff = −0.171, 95% CI = −1.342 to 1.00, −0.6 SD = −1.081). No difference by condition was found for overall CGI severity, F(1,27) = 0.55, p = .465, partial η2 = .022, and non-inferiority analyses indicated that the 95% confidence interval around the mean difference did not overlap the −0.6 SD margin of non-inferiority (MDiff = 0.290, 95% CI = −0.516 to 1.096, −0.6 SD = −0.591). Finally, overall CGI improvement showed no mean difference, F(1,29) = 0.36, p = .551, partial η2 = .013, although non-inferiority analyses were inconclusive (MDiff = −0.173, 95% CI = −0.761 to 0.415, −0.6 SD = −0.384). (Table 1).
Discussion
Transdiagnostic models and treatments appear to be gaining interest for anxiety disorders[11,12,19]. Impetus for transdiagnostic treatments stems from research showing shared clinical features and underlying processes among the anxiety disorders[1], and the argument that the primary difference between individual anxiety disorders is the content of the perceived threat[50]. Previous studies suggest considerable symptom improvement among those receiving transdiagnostic CBT for anxiety. The current study is the first to directly compare the efficacy of transdiagnostic CBT to diagnosis-specific CBT for panic disorder, social anxiety disorder, and GAD. The results of this study provide support for the efficacy of transdiagnostic CBT for anxiety disorders, as it showed effects at least as strong as those of established diagnosis-specific CBT on most outcome measures. Further, post-treatment CSR ratings for the overall sample (3.07) were, for example, highly similar to those reported in other recent transdiagnostic (CSR = 3.20)[15], and diagnosis-specific CBT trials (CSR = 3.29)[51]. On the remaining measures, 95% confidence intervals around the mean differences included Δ = 0.60 SD leading to “inconclusive” results or an inability to reject the null hypothesis of different outcomes by condition. The extent to which this is a function of actual differences or limited study power should therefore be examined in larger comparative outcome trials.
In addition to the theoretical assumptions of shared pathology among the anxiety disorders, there are also pragmatic reasons to consider transdiagnostic treatment approaches for anxiety. As noted by Clark[52] (see also[8,53]), “having a single transdiagnostic CBT that is applicable to a broader range of disorders might increase the adoption rate of evidence-based CBT by mental health practitioners and improve access and availability of effective psychological treatment in the health care sector” (p. 31). The results from the current study also lend support to the efficiency of transdiagnostic group therapy. Due to the lack of restrictions on group enrollment based on diagnosis, populating new transdiagnostic groups was more efficient and yielded larger group sizes than did diagnosis-specific groups without delaying the initiation of the treatment. This advantage of transdiagnostic group therapy could have substantial impact on the provision of services for anxiety disorders while reducing delays and burden on practitioners.
While steps were taken to maximize the validity of the current trial, several limitations must be considered. First, no “attention placebo” condition was implemented. It, therefore, cannot be ruled out that the lack of difference in outcomes between the two treatment conditions arose due to common factors. Given the large effect sizes, well-documented superiority of cognitive-behavioral treatments for anxiety disorders over most other treatment approaches and the high percentage of participants classified as responders in both conditions, this appears unlikely. Second, the sample in the current study was small, particularly for non-inferiority analyses, and as such the results warrant replication. Third, no follow-up data were available, so the long-term comparability of the treatment effects could not be assessed. Finally, the sample included a limited profile of primary diagnoses, with the sample having primary diagnoses of social anxiety disorder, panic disorder, or GAD. While specific phobia, OCD, and PTSD were represented among comorbid diagnoses, care should be taken in generalizing these results to individuals with these diagnoses.
Despite the limitations, our results provide important support for transdiagnostic CBT as an efficacious and efficient treatment for anxiety disorders. Strengths of a transdiagnostic approach include focus on the shared pathology among the anxiety disorders and on the underlying processes maintaining each individual's psychopathology, which is sometimes lost in a regimented diagnosis-specific treatment[54]. The demonstration of nearly identical outcomes across transdiagnostic and diagnosis-specific groups provides additional, albeit preliminary, evidence supporting the efficacy of transdiagnostic CBT. Although this RCT included only social anxiety disorder, generalized anxiety disorder and panic disorder for the purposes of direct comparison to diagnosis-specific treatments, in clinical practice transdiagnostic treatments may be extended to include additional anxiety disorders, and may be particularly beneficial for the treatment of anxiety disorder not otherwise specified, as treatment protocols for this disorder are lacking[54]. Finally, transdiagnostic group CBT has the benefit of potentially easing dissemination and increasing access to evidence based treatments for anxiety.
Acknowledgments
This research was supported by an NIMH Mentored Research Scientist Development Award (MH073920).
References
- 1.Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behav Ther. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 2.McEvoy PM, Nathan P, Norton PJ. Efficacy of transdiagnostic treatments: A review of published outcome studies and future research directions. J Cog Psychother. 2009;23:27–40. [Google Scholar]
- 3.Norton PJ. Toward a clinically-oriented model of anxiety disorders. Cog Behav Ther. 2006;35:88–105. doi: 10.1080/16506070500441561. [DOI] [PubMed] [Google Scholar]
- 4.Barlow DH. Anxiety and its disorders. 2nd ed Guilford; New York: 2002. [Google Scholar]
- 5.Craske MG. Anxiety disorders: psychological approaches to theory and treatment. Westview; Boulder, CO: 1999. [Google Scholar]
- 6.Brown TA, Campbell LA, Lehman CL, et al. Current and lifetime comorbidity of the DSMIV anxiety and mood disorders in a large clinical sample. J Abnorm Psychol. 2001;110:585–599. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- 7.Norton PJ, Barrera TL, Mathew AR, et al. Effect of transdiagnostic CBT for anxiety on comorbid diagnoses: A benchmarking study. doi: 10.1002/da.22018. [DOI] [PubMed] [Google Scholar]
- 8.McManus F, Shafran R, Cooper Z. What does a `transdiagnostic' approach have to offer the treatment of anxiety disorders? British Journal of Clinical Psychology. 2010;49:491–505. doi: 10.1348/014466509X476567. [DOI] [PubMed] [Google Scholar]
- 9.Erickson DH, Janeck AS, Tallman K. Transdiagnostic group CBT for anxiety: Clinical experience and practical advice. J Cog Psychoth. 2009;23:34–43. [Google Scholar]
- 10.Clark DA, Taylor S. The transdiagnostic perspective on cognitive-behavioral therapy for anxiety and depression: New wine for old wineskins? J Cog Psychoth. 2009;23:60–66. [Google Scholar]
- 11.Erickson DH. Group cognitive behavioural therapy for heterogeneous anxiety disorders. Cog Behav Ther. 2003;32:179–186. doi: 10.1080/16506070310001686. [DOI] [PubMed] [Google Scholar]
- 12.Norton PJ. An open trial of a transdiagnostic cognitive-behavioral group therapy for anxiety disorder. Behav Ther. 2008;39:242–250. doi: 10.1016/j.beth.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 13.Norton PJ, Price EP. A meta-analytic review of cognitive-behavioral treatment outcome across the anxiety disorders. J Nerv Mental Dis. 2007;195:521–531. doi: 10.1097/01.nmd.0000253843.70149.9a. [DOI] [PubMed] [Google Scholar]
- 14.Hofmann SG, Smits JAJ. Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo-controlled trials. J Clinic Psychiatry. 2008;69:621–632. doi: 10.4088/jcp.v69n0415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ellard KK, Fairholme CP, Boisseaux CL, et al. Unified protocol for the transdiagnostic treatment of emotional disorders: Protocol development and initial outcome data. Cog Behav Pract. 2010;17:88–101. doi: 10.1016/j.cbpra.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Norton PJ, Hope DA. Preliminary evaluation of a broad-spectrum cognitive-behavioral group therapy for anxiety. J Behav Ther Exp Psychiatry. 2005;36:79–97. doi: 10.1016/j.jbtep.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 17.Norton PJ, Hayes SA, Hope DA. Effects of a transdiagnostic group treatment for anxiety on secondary depressive disorders. Dep Anx. 2004;20:198–202. doi: 10.1002/da.20045. [DOI] [PubMed] [Google Scholar]
- 18.Erickson DH, Janeck A, Tallman K. Group cognitive-behavioral group for patients with various anxiety disorders. Psychiatric Services. 2007;58:1205–1211. doi: 10.1176/ps.2007.58.9.1205. [DOI] [PubMed] [Google Scholar]
- 19.Schmidt NB, Buckner JD, Pusser A, et al. Randomized controlled trial of False Safety Behavior Elimination Therapy (F-SET): A unified cognitive behavioral treatment for anxiety psychopathology. Behav Ther. doi: 10.1016/j.beth.2012.02.004. in press. [DOI] [PubMed] [Google Scholar]
- 20.Craske MG, Stein MB, Sullivan G, et al. Disorder-specific impact of coordinated anxiety learning and management treatment for anxiety disorders in primary care. Arch Gen Psychiatry. 2011;68:378–388. doi: 10.1001/archgenpsychiatry.2011.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Craske MG, Rose RD, Lang A, et al. Computer-assisted delivery of cognitive behavioral therapy for anxiety disorders in primary-care settings. Depr Anx. 2009;26:235–242. doi: 10.1002/da.20542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Norton PJ. A randomized clinical trial of transdiagnostic CBT for anxiety disorder by comparison to relaxation training. Behav Ther. doi: 10.1016/j.beth.2010.08.011. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McEvoy PM, Nathan P. Effectiveness of cognitive behaviour therapy for diagnostically heterogeneous groups: A benchmarking study. J Consult Clin Psychol. 2007;75:344–350. doi: 10.1037/0022-006X.75.2.344. [DOI] [PubMed] [Google Scholar]
- 24.Norton PJ, Philipp LM. Transdiagnostic approaches to the treatment of anxiety disorders: A meta-analytic review. Psychother: Theory, Res, Pract, Train. 2008;45:214–226. doi: 10.1037/0033-3204.45.2.214. [DOI] [PubMed] [Google Scholar]
- 25.Piaggio G, Elbourne DR, Altman DG, et al. Reporting of noninferiority and equivalence randomized trials: An extension of the CONSORT statement. JAMA. 2006;295:1152–1160. doi: 10.1001/jama.295.10.1152. [DOI] [PubMed] [Google Scholar]
- 26.Brown TA, Di Nardo PA, Barlow DH. Anxiety disorders interview schedule for DSM-IV. Adult Version Graywind; Albany, NY: 1994. [Google Scholar]
- 27.Heimberg RG, Dodge CS, Hope DA, et al. Cognitive behavioral group treatment for social phobia: Comparison with a credible placebo. Cog Ther Res. 1990;14:1–23. [Google Scholar]
- 28.National Institute of Mental Health Clinical global impressions scale. Psychopharm Bull. 1985;21:839–843. [Google Scholar]
- 29.Spielberger CD. Manual for the State-Trait Anxiety Inventory (STAI) Consulting Psychologists Press; Palo Alto, CA: 1983. [Google Scholar]
- 30.Fisher PL, Durham RC. Recovery rates in generalized anxiety disorder following psychological therapy: An analysis of clinically significant change in the STAIT across outcome studies since 1990. Psychol Med. 1999;29:1425–1434. doi: 10.1017/s0033291799001336. [DOI] [PubMed] [Google Scholar]
- 31.Shear MK, Brown TA, Barlow DH, et al. Multicenter Collaborative Panic Disorder Severity Scale. Am J Psychiatry. 1997;154:1571–1575. doi: 10.1176/ajp.154.11.1571. [DOI] [PubMed] [Google Scholar]
- 32.Newman MG, Kachin KE, Zuellig AR, et al. The social phobia diagnostic questionnaire: Preliminary validation of a new self-report diagnostic measure of social phobia. Psychol Med. 2003;33:623–635. doi: 10.1017/s0033291703007669. [DOI] [PubMed] [Google Scholar]
- 33.Roemer L, Borkovec M, Posa S, et al. A self-report diagnostic measure of generalized anxiety disorder. J Behav Ther Exp Psychiatry. 1995;26:345–350. doi: 10.1016/0005-7916(95)00040-2. [DOI] [PubMed] [Google Scholar]
- 34.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory—II. The Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- 35.Borkovec TD, Nau SD. Credibility of analogue therapy rationales. J Behav Ther Exp Psychiatry. 1972;3:257–260. [Google Scholar]
- 36.Butler G, Cullington A, Munby M, et al. Exposure and anxiety management in the treatment of social phobia. J Consult Clin Psychol. 1984;52:642–650. doi: 10.1037//0022-006x.52.4.642. [DOI] [PubMed] [Google Scholar]
- 37.Norton PJ. Group cognitive-behavioral therapy of anxiety: A transdiagnostic treatment manual. Guilford; New York: 2012. [Google Scholar]
- 38.Norton PJ, Hope DA. The “Anxiety Treatment Protocol”: A Group Case Study Demonstration of a Transdiagnostic Group CBT for Anxiety Disorders. Clin Case Stud. 2008;7:538–554. [Google Scholar]
- 39.Craske MG, Barlow DH. Mastery of your anxiety and panic. New York, Oxford: 2007. [Google Scholar]
- 40.Heimberg RG, Becker RE. Cognitive-behavioral group therapy for social phobia: Basic mechanisms and clinical strategies. Guilford Press; New York: 2002. [Google Scholar]
- 41.Dugas MJ, Robichaud M. Cognitive-behavioral treatment for generalized anxiety disorder: From science to practice. Routledge; New York: 2007. [Google Scholar]
- 42.Dugas MJ, Ladouceur R, Léger E, et al. Group cognitive behavioral therapy for generalized anxiety disorder: Treatment outcome and long-term follow-up. J Consult Clin Psychol. 2003;71:821–825. doi: 10.1037/0022-006x.71.4.821. [DOI] [PubMed] [Google Scholar]
- 43.Telch MJ, Lucas JA, Schmidt NB, et al. Group cognitive-behavioral therapy of panic disorder. Behav Res Ther. 1993;31:279–287. doi: 10.1016/0005-7967(93)90026-q. [DOI] [PubMed] [Google Scholar]
- 44.Wiens BL. Choosing an equivalence limit for noninferiority or equivalence studies. Control Clin Trials. 2002;23:2–14. doi: 10.1016/s0197-2456(01)00196-9. [DOI] [PubMed] [Google Scholar]
- 45.Hedman E, Andersson G, Ljótsson B, et al. Internet-based cognitive behavior therapy vs. cognitive behavioral group therapy for social anxiety disorder: A randomized controlled non-inferiority trial. PloS ONE. 2011;6:e18001. doi: 10.1371/journal.pone.0018001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lovell K, Cox D, Haddock G, et al. Telephone administered cognitive behaviour therapy for treatment of obsessive compulsive disorder: Randomised controlled non-inferiority trial. BMJ. 2006;333:883. doi: 10.1136/bmj.38940.355602.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hedeker D. An introduction to growth modeling. In: Kaplan D, editor. The Sage Handbook of Quantitative Methodology for the Social Sciences. Sage; Thousand Oaks, CA: 2004. pp. 215–234. [Google Scholar]
- 48.Muthén B, Satorra A. Complex sample data in structural equation modeling. In: Marsden P, editor. Sociol Methodology. 1995. pp. 216–316. [Google Scholar]
- 49.Sharp DM, Power KG, Swanson V. A comparison of the efficacy and acceptability of group versus individual cognitive behavior therapy in the treatment of panic disorder and agoraphobia in primary care. Clin Psychol Psychother. 2004;11:73–82. [Google Scholar]
- 50.Craske MG. Anxiety disorders: Psychological approaches to theory and treatment. Westview Press; Boulder, CO: 1999. [Google Scholar]
- 51.Ledley DR, Heimberg RG, Hope DA, et al. Efficacy of a manualized and workbook-driven individual treatment for social anxiety disorder. Behav Ther. 2009;40:414–424. doi: 10.1016/j.beth.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 52.Clark DA. Cognitive behavioral therapy for anxiety and depression: Possibilities and limitations of a transdiagnostic perspective. Cog Behav Ther. 2009;38:29–34. [PubMed] [Google Scholar]
- 53.McHugh RK, Murray HW, Barlow DH. Balancing fidelity and adaptation in the dissemination of empirically-supported treatments: The promise of transdiagnostic interventions. Behav Res Ther. 2009;47:946–953. doi: 10.1016/j.brat.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mansell W, Harvey A, Watkins E, et al. Conceptual foundations of the transdiagnostic approach to CBT. J Cog Psychother. 2009;23:6–19. [Google Scholar]