Abstract
BACKGROUND
Atherosclerosis is one of the leading causes of mortality all around the world. Obesity is an independent risk factor for atherosclerosis and cardiovascular diseases (CVD). In this respect, we decided to examine the effect of the subgroups of weight on cardiovascular risk factors.
METHODS
This cross-sectional study was done in 2006 using the data obtained by the Iranian Healthy Heart Program (IHHP) and based on classification of obesity by the World Health Organization (WHO). In this study, the samples were tested based on the Framingham risk score, Metabolic Measuring Score (MMS) and classification of obesity. Chi-square and ANOVA were used for statistical analysis.
RESULTS
12514 people with a mean age of 38 participated in this study. 6.8% of women and 14% of men had university degrees (higher than diploma). Obesity was seen in women more than men: 56.4% of women and 40% of men had a Body Mass Index of (BMI) ≥ 25 Kg/m2. 13% of the subjects had FBS > 110 and13.9% of them were using hypertensive drugs. In this study, we found that all risk factors, except HDL cholesterol in men, increased with an increase in weight. This finding is also confirmed by the Framingham flowfigure for men and women.
CONCLUSION
One of every two Americans, of any age and sex, has a Body Mass Index of (BMI) ≥ 25 Kg/m2. Obesity associated CVD and other serious diseases. Many studies have been done in different countries to find the relationship between obesity and CVD risk factors. For example, in the U.S.A and Canada they found that emteropiotic parameters, blood presser and lipids increased by age(of both sexes). Moreover, another study done in China, which is a country in Asia like Iran, shows that BMI has an indirect effect on HDL cholesterol, LDL cholesterol and triglyceride. This data is consistent with the results of the current study. However, In China they found that this relationship in men is stronger than women, but our study reveals the opposite.
Keywords: Body Mass Index (BMI), Overweight, Cardiovascular Risk Factors, Framingham Risk Score, Metabolic Syndrome
Introduction
According to the studies in recent decades, atherosclerosis is the main cause of mortality in modern societies.1,2 In addition to diabetes and impaired glucose tolerance (IGT), which are accepted as the main cause of atherosclerosis, co morbidity of some other factors such as hypertension, hyperlipidemia, and blood glucose disorders can increase the risk of atherosclerosis to several times higher.3-7 The association of the above mentioned cases with some factors such as obesity and increased BMI (Body Mass Index) have been emphasized in certain studies.8-10obesity is an indepent risk factor for CHD and CVD events. Increased adipose tissue related to all cause mortality 11-12 It seems that association of other atherosclerosis risk factors with obesity has main ruls. In fact, it seems that many health problems and diseases would probably be more problematic if accompanied by obesity and increased BMI.13-15 Some of these cases are also true based on studies conducted in Iran and on the Persian race.16-18 However, by considering all the current studies, it seems that the correlation between various degrees of obesity and the prevalence of different types of risk factors have not clearly been identified either in Iran or in the world.19-21 Therefore, it was decided to compare various degrees of weight with conventional cardiovascular risk factors in an Iranian sample population in males and females.
Materials and Methods
The data of Isfahan Healthy Heart Program (IHHP) were used in this cross-sectional study. The Healthy Heart Program is a community-based interventional program which has been underway since 2000 in Isfahan, Najafabad and Arak, Iran.22
Data Collection
A questionnaire was completed for every participant, including demographic characteristics and studied medical history, by a general practitioner or a trained nurse. In addition to medical examination, weight measurement was done by the Seca scale in kilograms and height with a standard tape. BMI was measured through dividing weight by height squared (weight (kg)/height squared (cm2). The height and weight of the subjects were calculated while they wore minimum amount of clothing and no shoes. Waist circumference (WC) and hip circumference (HC) was measured based on the proposed protocol of the “National Study of Health and Nutrition Survey”. Through dividing WC by HC, waist to hip ratio was calculated. The study subjects were asked about their medical history, such as history of cardiovascular diseases or existence of current cardiovascular disease, current drug consumption, menopause status, and other alternative hormone therapies (in case they were used by the women). Employment status and other socio-demographic characteristics were asked through a standard questionnaire.22,23
Physical Examination and Various test Methods
In this study our subjects groups were based on BMI sub-groping classification (Table 1).
Table 1.
Classification of various types of weight categories based on standards of WHO
| Incidence* of various diseases risk (based on normal weight** and waist circumference) | |||||
|---|---|---|---|---|---|
| BMI (Kg/m2) | Various obesity categories | men (102cm) ≤ 40 | men (102 cm) > 40 | ||
| women (88 cm) ≤ 35 | women (88 cm) > 35 | ||||
| Thin (under the normal weight) | < 18.5 | ||||
| Normal weight | 18.5 to 24.9 | ||||
| Overweight | 25.0 to 29.9 | ||||
| Obesity | 30.0 to 34.9 | I | Increased much | Increased much | |
| 35.0 to 39.9 | II | Increased very much | Increased very much | ||
| Excessive obesity | ≥ 40 | III | Increased excessively | Increased excessively | |
This table is related to the Methods section.
By incidence of various diseases risk, in fact we meant Type II Diabetes, Hypertension and Coronary Heart Diseases.
Increased waist circumference can be a sign for increased incidence of diseases even if their weight is normal.
The risk factors of cardiovascular diseases were measured based on strategies of the Adult Treatment Panel Guidelines-III (ATP-III) and according to different weight categories proposed by the World Health Organization.24-26 The blood pressure of the study subjects was measured through a mercury barometer according to the American Heart Association guidelines, according to which it was averagely done two times with a 30 minute interval.25 Thereafter, according to the contents of ATP-III, the diagnosis of hypertension was considered as a mean blood pressure equal or greater than mm Hg and/or taking antihypertensive drugs.25,26 Measuring the blood lipids level and/or measuring blood glucose was done after a 12-hour fasting period and total cholesterol, high density lipoprotein (HDL-C), triglyceride (TG) and blood sugar were directly measured by plasma. Thus, 5cc of blood was taken in serum form and was collected with a mix of ethylene diamine tetra acetic acid (EDTA) in order to count the blood cells. Moreover, total serum levels of cholesterol and triglyceride were determined by enzymatic methods through Auto analyzer ELAN/2000. In addition, HDL-C was determined by enzymatic methods similar to total serum levels of cholesterol through heparin-manganese precipitation procedure.22, 27,28
Cholesterol of low density lipoprotein (LDL-C) was measured by the Freidewald Equation. According to the guidelines of ATP-III, levels equal to or greater than 160 mg/dL were considered as high LDL.27,28 Provided that fasting blood glucose was equal to or greater than 126 mg/dL and/or he/she was currently under the treatment of diabetes (pill or insulin consumption), it was diagnosed as diabetes and provided that their fasting glucose was equal or greater than 100 mg/dL, it was reported as impaired glucose tolerance test. Smoking cigarettes and other types of tobacco were recorded based on the subjects self-reporting.22
After collecting and completing the data in the questionnaires, they were assessed through proposed methods of ATP-III and BMI based on WHO strategies and using the three following methods.24-26
Various methods for categorizing the study subjects
A) Framingham scoring system B) Simple evaluation method based on modifiable risk factors and C) An evaluation system assessed according to the presence or absence of measurement of the metabolic syndrome (MMC).29-31
A: risk of hard heart events are estimated for the next ten years, including acute myocardial infarction and/or sudden death based on some variables like total serum cholesterol, HDL-C, high systolic blood pressure and soon.
In the present study, because diabetes is known as an equivalent to CVD, the comorbidity mode was deleted from the figures.32-34
B: They were divided into three categories according to the recommendations of ATP-III:
B-1: Low risk people < 10% B-2: Medium risk people 10%-20% and B-3: High risk people > 20%.
In this study, each of the male and female groups was calculated in each three categories and then the whole population was studied to determine their risk of CVD based on different obesity categories and obesity strategies.
C: Counting different types of risk factors:
Risk factors of CVD incidence which were preventable and changeable by therapeutic methods have been determined in the clinical trial designs. In ATP-III strategies, it was determined that the assessment and measurement of each of these risk factors is a way in itself to determine the risk of CVD. It was calculated by smoking (any type of tobacco smoking during the past month), having hypertension based on blood pressure equal or greater than mm Hg and/or receiving antihypertensive drugs, HDL-C lower than 40 mg/dL, fasting glucose between 110 to 125 mg/dL and LDL-C equal or greater than 160 mg/dL.
It should also be noted that because age and family history in CVD are highly variable and unreliable items, we ignored them in this study.
D: Measurement of metabolic syndrome (MMC): Because in the ATP-III protocol, it has been specifically stated that the presence of metabolic syndrome increases the risk of CVD, using ATP-III, presence or absence of metabolic syndrome in both men and women was separately determined based on their BMI categories.30,31
In this study, metabolic syndrome could be diagnosed, if it had 3 out of the 5 of the following features:
a: Abdominal adiposity a) as WC greater than 88 cm (35 inches) in women or greater than 102 cm (40 inches) in men b) Triglyceride equal to or greater than 150 mg/dL c) Fasting glucose equal to or greater than 100 mg/dL d) HDL-C less than 50 mg/dL and e) blood pressure equal or greater than mm Hg.
We should note again that in this study “comorbidity” means interaction between presence of both diabetes and CVD in the study subjects which we deleted.
Statistical Methods
In this study, investigating the marital status and also the correlation between gender and education, different categories of obesity, employment status and smoking were conducted through SPSS Software version 15 by the chi-square method (χ2). In addition, first the blood sugar level of the study subjects were categorized and then we used χ2 method. We used this method for evaluating hypertension (presence or absence of blood pressure equal or greater than 140/90 mm Hg) separating each of the weight categories according to sex.
ANOVA test was used in both sexes’ groups in order to compare different weight levels for mean systolic and diastolic blood pressure, HDL-C, LDL-C and fasting blood sugar and age.
Results
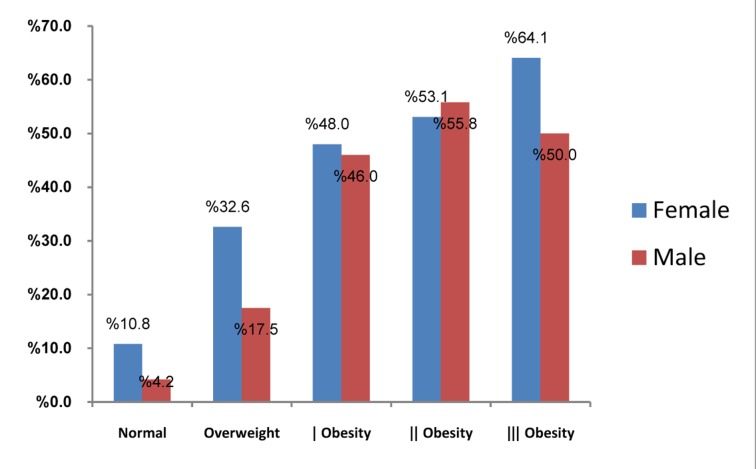
Table 1 is the categorization table for obesity based on reference of the WHO which was given in the methods section of the essay. Table 2 shows demographic characteristics of the study subjects. Of the 12,514 people, there were 6342 females and 6087 males and the mean age of the two groups was close to each other and it was approximately 38 years. In the study population, 6.8% and 14.9% of women and men respectively had higher education (higher than high school graduation). Overweight and obesity were more prevalent in women than in men.
Table 2.
Demographic characteristics of the study population
| Female |
Male |
Total |
|
|---|---|---|---|
| Age | 37.82 ± 14.109 | 38.15 ± 14.92 | |
| PERCENT | PERCENT | ||
| Higher education | 6.8 | 14.9 | 10.8 |
| Employed | 5.8 | 79.9 | 42.3 |
| Married | 81.1 | 78.2 | 79.7 |
| Smoker | 0.9 | 28.1 | 14.3 |
| Normal Weight | 38.5 | 53.8 | 46.1 |
| Overweight | 34.4 | 31.5 | 33 |
| Obesity I | 17.1 | 7.4 | 12.3 |
| Obesity II | 3.8 | 0.9 | 2.4 |
| Obesity III | 1.1 | 0.2 | 0.6 |
| FBS < 110 | 1.4 | 1.3 | 1.3 |
| HTN* > 150/90 or taking antihypertensive | 14.6 | 13.2 | 13.9 |
HTN: Hypertension
Moreover, 1.3% of the study subjects had an FBS greater than 110 and 13.9% of them had blood pressure greater than mm Hg or received antihypertensive drugs (Table 2).
All the risk factors such as systolic and diastolic blood pressure, FBS, LDL, TG, Total cholesterol and WC increase both in men and women with increased BMI and subsequently higher degrees of obesity. These changes were not significant in HDL reduction in men.
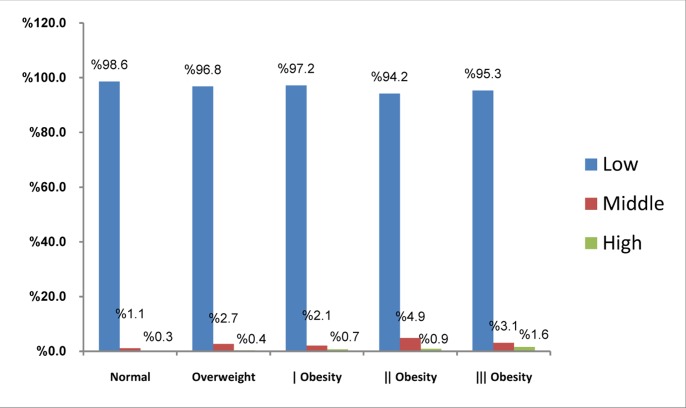
Moreover, in figure 1-a, the frequency percentage of preventable risk factors in women are shown based on different contents of BMI in which 70% of those with normal BMI had no risk factors but 27.3% of women had one risk factor and 3.5% had two or more risk factors.
Figure 1-a.
The frequency percentage of CVD incidence based on different BMI categories in women CVD: Cardiovascular diseases; BMI: Body Mass Index
An increase in BMI can also increase the comorbidity of a number of risk factors; so that in obesity II, 13.7% of the study subjects had two or more risk factors and 42% had one risk factor. However, in those with obesity III, the percentage of those with two or more risk factors was reduced to 9.4% and on the contrary, the percentage of those with one risk factor was increased to 48.4%.
Figure 1-b demonstrates a similar situation in men. In this group, increased number of risk factors was changed uniformly and in the obesity III group, most of the subjects (41.67%) are those with two or more risk factors. Moreover, in this figure the more the BMI increased, the more the number of people in the high risk category increased (Figures 1a and 1-b).
Figure 1-b.
The frequency percentage of CVD incidence based on different BMI categories in men CVD: Cardiovascular diseases; BMI: Body Mass Index
In the above figures, the risk of suffering from cardiovascular diseases in the next 10 years are shown separately for men and women and it is indicated that in the men’s group, by the increasing of obesity levels, the number of high risk people are increased for cardiovascular diseases However, in low and medium groups, there was no significant difference between obesity levels. There was also no significant difference between BMI values in the women’s group (Figure 1-b).
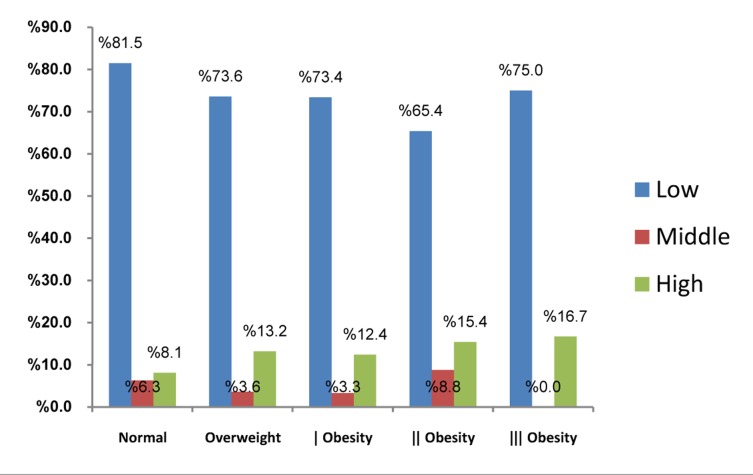
In Figure 2, changes of various factors in measurement of metabolic syndrome are illustrated in different weight categories (BMI) for both sexes. As indicated, increased BMI, both in men and women, could increase the changes of various factors in the incidence of metabolic syndrome (Figure 2 and Table 1).
Figure 2.
Prevalence of metabolic syndrome (MMS) based on different BMI categories in the study population
Discussion
The present study demonstrated that all the cardiac risk factors increased by an increase of BMI both in men and women and the changes were only non-significant for HDL-C reduction in men. Overweight and obesity are two of the common health problems in modern societies so that their prevalence has been increased globally.32,33 According to recent studies, one out of two American adults is obese or overweight. This means that their BMI is higher than 25 and in fact this statistic has increased by 5% compared with three decades ago and this obvious value increase can be seen in any age and sex.33,34 In addition, according to other studies, excessive weight is associated with increased cardiovascular events, type II diabetes mellitus, hypertension, stroke, dyslipidemia and also degenerative bone diseases (osteoarthritis) or increased prevalence of some cancers. 35-37
Therefore, in the present study, we investigated the cardiovascular events in different subcategories of the society based on age and sex and by considering different weight categories in different countries and races. For instance, in a study in Canada, it was determined that BMI in both men and women is increased with aging and simultaneously systolic and diastolic blood pressure also increased. Furthermore, in a study in Canada, different parameters of lipids increased without any correlation with sex and weight. All the mentioned results were in accordance with the present study.38-40
On the other hand, in a study in China, which is an Asian country similar to Iran, it was indicated that BMI changes had an inverse correlation with BMI and HDL-C; but had a direct correlation with LDL-C, Total cholesterol and TG. This was in accordance with the findings of the present study. In the study conducted in China, specifically BMI changes and mean values of cardiovascular risk factors are slightly more in men than in women.38,39 While such a result was not seen in the present study by reviewing the obtained results and changes figures based on metabolic risk factors. However, by comparing the China results with the results of the present study which was calculating incidence risk of cardiovascular events during the next ten years, we found similar results. However, it should be noted that diabetic patients were excluded from the present study and those were studied who had impaired FBS but had no history of diabetes and this item also increased with increased BMI. Moreover, in the study of Frank et al. about the association of diabetes mellitus with abdominal adiposity in old women, there was also a direct correlation between incidence of diabetes and increased weight which was in accordance with the present study.37-42
According to some studies in Iran in which overweight and obesity were considered as a unit without any classification, it was indicated that increased BMI was seen in both sexes. It was particularly observed more among young women than men.18,19,40,42
According to another study, there was also no overweight and obesity classification, it was indicated that changes of blood pressure, diabetes, increased total cholesterol, and TG and decreased HDL-C were significantly different for those with overweight and obesity compared with normal weight people.16,23 All the above items are in accordance with the present study. In addition, weight specifically increased LDL-C and we also found a similar result. In the above mentioned study, it was indicated that mean values of different blood lipids, FBS and mean blood pressure of the study subjects with normal weight was different to those with obesity and/or high weight, which was also in accordance with the present study. However, in previous studies, there was also a correlation between overweight and obesity, with hypertension and changes of blood lipids, which was in accordance with the present study.19,41
In the present study, although different categories of overweight and obesity were reviewed with CVD risk factors, we only considered BMI. While perhaps it would have been more appropriate if we had investigated WC, HC and WHR too. In addition, we only assessed mean years of education and their mean age and further studies are recommended to review the effect of different ages and different educational grades on weight.
According to the researchers conducted by the Third National Health and Nutrition Examination Survey (NHANES III) during 1994-1998, it was determined that the prevalence of obesity is increasing for both sexes of any age.42-46 Moreover, according to the studies of Siidiro Poulus et al, coronary artery diseases and different items resulted from it such as stroke or peripheral vascular injuries are specifically associated with obesity.31 In other words, according to the statements of the American Heart Association, obesity is a major and controllable risk factor for CVD so that high weight is a predicting risk factor for probable existence of atherosclerosis and can have effect on its classic risk factors.42-44 In fact, increased relative risk of CVD in various weight categories can particularly be seen, this was also seen in the present study.8,45,46 It has been announced that risk of fatal and nonfatal cardiovascular events in men in their middle ages will increase to 72% if their BMI is between 25 to 29 Kg/m2. In the present study, history of diabetic diseases co morbidity with CVDs was removed. However, reviewing the figures related to the 10-year risk of cardiovascular events showed that an increased risk of CVD is associated with increased blood sugar, but this was not observed in women. However, given that the increasing prevalence of obesity and also the direct and indirect association of being overweight with many conventional cardiovascular risk factors, all the general practitioners and expert physicians should be trained about obesity, and its relevant items and risks should be identified properly and accurately. Particularly for general practitioners who have a limited and certain amount of time in frequency of examinations for each patient.
Acknowledgments
The Persian version of this article has previously published of J Iran Univ Med Sci: 2010, No: 72; 31-41.
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Libby P. The pathogenesis of atherosclerosis. In: Kasper Dl, Branwald E, Fauci AS, Hauser SL, Longo DL., editors. Harrison's Principles of international medicine. New York: MC Graw Hill Company; 2005. pp. 1425–30. [Google Scholar]
- 2.Batalla A, Reguero R, Gubero GL, Sanmartin JC, Hevia Sieres, Ravina T. Severity of early coronary disease and cardiovascular risk factors. International symposium on atherosclerosis. 2000:25–9. [Google Scholar]
- 3.Zimmet P. Epidemiology of diabetes mellitus and associated cardiovascular risk factors. Am J Med. 2005;118(sl2):35–85. doi: 10.1016/j.amjmed.2005.01.044. [DOI] [PubMed] [Google Scholar]
- 4.Esteghamati A, Abbasi M, Nakhjavani M, Yousefizadeh A, Basa AP, Afshar H. Prevalence of diabetes and other cardiovascular risk factors in an Iranian population with acute coronary syndrome. Cardiovasc Diabetol. 2006;17(5):15. doi: 10.1186/1475-2840-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Surdacki A, Stochmal E, Szurkowska M, Bode-Boger SM, Martens-Lobenhoffer J, Stochmal A, et al. On traditional atherosclerotic risk factors and extent of coronary atherosclerosis in patients with combined impaired fasting glucose and impaired glucose tolerance. Metabolism. 2007;56(1):77–86. doi: 10.1016/j.metabol.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 6.Adult treatment. Executive Summary of the third report of the national cholesterol education program (NCEP) Export panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001;285(19):2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 7.Kannel WB. Fifty years of Frarningham Study contributions to understanding hypertension. J Hum Hypertens. 2000;14(2):83–90. doi: 10.1038/sj.jhh.1000949. [DOI] [PubMed] [Google Scholar]
- 8.Huang Z, Willett WC, Manson JE, Rosner B, Stampfer MJ, Speizer FE, et al. Body weight, weight change, and risk for hypertension in women. Ann Intern Med. 1998;128(2):81–8. doi: 10.7326/0003-4819-128-2-199801150-00001. [DOI] [PubMed] [Google Scholar]
- 9.Redon J. Hypertension in obesity. Nutr Metab Cardiovasc Dls. 2001;11(5):344–53. [PubMed] [Google Scholar]
- 10.Strawbridge WJ, Wallhagen MI, Shema SJ. New NHLBI clinical guidelines for obesity and overweight will they promote health. Am J Public Health. 2000;90(3):340–3. doi: 10.2105/ajph.90.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aronne LJ. Epidemiology Morbidity and treatment of over weigh and obesity. J Clin psychiatry. 2001;(Suppl 23):62. [PubMed] [Google Scholar]
- 12.National Heart, Lung and Blood Institute. The Practical Guide Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. 2001. Available from: www.nhlbi.nih.gov/guidelines/obesity/prctgd_c.pdf.
- 13.Boland LL, Folsom AR, Rosamond WD. Hyperinsulinemia, dyslipidemia and obesity as risk factors for hospitalized gall- bladder disease: Aprospective study. Ann Epidemiol. 2002;12(2):131–40. doi: 10.1016/s1047-2797(01)00260-5. [DOI] [PubMed] [Google Scholar]
- 14.Fujioka K. Management of obesity as a chronic disease: No pharmacologic, pharmacologic and surgical options. Obes Res. 2002;10(Suppl 2):116S–23S. doi: 10.1038/oby.2002.204. [DOI] [PubMed] [Google Scholar]
- 15.Mirmiran P, Esmaillzadeh A, Azizi F. Detection of cardiovascular risk factors by anthropometry measures in Tehranian adults: Receiver operating characteristic (ROC) curve analysis. Eur J clin Nutr. 2004;58(8):1110–8. doi: 10.1038/sj.ejcn.1601936. [DOI] [PubMed] [Google Scholar]
- 16.Boshtam M, Rafie M, Sarraf-Zadegan N. Obesity and its association with other cardiovascular risk factors in Isfahan population: Isfahan CVD Risk factor survey. Aterosclerose. 1997;1(4):7–11. [Google Scholar]
- 17.Rashidi B. Mohammadpour M. Vafa R, Karandish M. Prevalence of obesity in Iran. Obesity Reviews. 2005;6(3):191–2. doi: 10.1111/j.1467-789X.2005.00174.x. [DOI] [PubMed] [Google Scholar]
- 18.Mohammadpour-Ahranjani B, Rashidi A, Karandish M, Eshraghian MR, Kalantari N. Prevalence of overweight and obesity in adolescent Tehran students, 2000-2001: An epidemic health problem. Public Health Nutr. 2004;7(5):645–8. doi: 10.1079/phn2003593. [DOI] [PubMed] [Google Scholar]
- 19.Bahrami H, Sadatsafavi M, Pourshams A, Kamangar F, Nouraei M. Hypertension in an Iranian cohort study; Iranian women experience higher rates ofobesity and hypertension than American women. BMC Public Health. 2006;20(6):158. doi: 10.1186/1471-2458-6-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moayeri H, Bidad K, Aghamohammadi A, Rabbani A, Anari S, Nazemi L, et al. Overweight and obesity and their associated factors in adolescents in Tehran, Iran, 2004-2005. Eur J Pediatr. 2006;165(7):489–93. doi: 10.1007/s00431-006-0101-8. [DOI] [PubMed] [Google Scholar]
- 21.Millan Nunez-Cortés. Relation of obesity and cardiovascular risk in Spain. Int J Vitam Nutr Res. 2006;76(4):200–7. doi: 10.1024/0300-9831.76.4.200. [DOI] [PubMed] [Google Scholar]
- 22.Sarraf-Zadegan N, Sadri G, Malek Afzali, Baghaei M, Mohammadi Fard, Shahrokhi S, et al. Isfahan Healthy Heart Programme: a comprehensive integrated community-based programme for cardiovascular disease prevention and control. Design, methods and initial experience. Acta Cardiol. 2003;58(4):309–20. doi: 10.2143/AC.58.4.2005288. [DOI] [PubMed] [Google Scholar]
- 23.National Institute. Over-weight, obesity, and health risk-National task force on the prevention and treatment obesity. Arch Int Med. 2000;160(7):898–904. doi: 10.1001/archinte.160.7.898. [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization. Global database on obesity and body mass index in adults. 2001. Available from: http://www.who.int/nut/db_bmi.htm.
- 25.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. Seventh Report of the joint National committee on prevention, detection, evaluation, and treatment of high blood pressure hypertension. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. Obesity epidemic puts millions at risk. 2001. Available from: http://www.who.int/archives/inf-pr-1997/en/pr 97-46.html.
- 27.Warnick GR, Benderson J, Albers JJ. Dextransulfat Mg2+ precipitation procedure for high-density lipoprotein cholesterol. Clinical Chemistry. 1982;28(6):1379–388. [PubMed] [Google Scholar]
- 28.Friedwald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical Chemistry. 1972;18(6):499–502. [PubMed] [Google Scholar]
- 29.Ghandehari H, Kamal-Bahl S, Bassin SL, Wong ND. Abdominal obesity and the spectrum of globalcardiometabolic risks in US adults. International Journal of Obesity. 2009;33(2):239–48. doi: 10.1038/ijo.2008.252. [DOI] [PubMed] [Google Scholar]
- 30.Madhavi RP, Yanek LR, Taryn F, Becker M, Becker MD. Assessment of Global Coronary Heart Disease Risk in Overweight and Obese African-American Women. Obesity Research. 2003;11(5):660–67. doi: 10.1038/oby.2003.94. [DOI] [PubMed] [Google Scholar]
- 31.Siidiro Poulus, Karvounaris SA, Boumpas DT. Metabolic syndrome in rheumatic diseases: Epidemiology, path physiology and clinical implications. Arthritis Res Ther. 2008; 10(3):207. doi: 10.1186/ar2397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gaziano M, Manson J, Ridker P. Primary and secondary prevention of coronary heart disease. 8th ed. Philadelphia: W.B. Saunders Company; 2008. pp. 1119–48. [Google Scholar]
- 33.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults,1999-2000. JAMA. 2002;288(14):1772–3. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 34.Galuska DA, Will JC, Serdula MK, Ford ES. Arehealth care professionals advising obese patients to loseweight? JAMA. 1999;282(16):1576–8. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- 35.Fontaine KR, Haaz S, Bartlett SJ. Are overweight and obese adults with arthritis being advised to lose weight? J Clin Rheumatol. 2007;13(7):12–5. doi: 10.1097/01.rhu.0000256168.74277.15. [DOI] [PubMed] [Google Scholar]
- 36.Garfmkel L. Overweight and cancer. Ann Intern Med. 1985;103(6):1034–36. doi: 10.7326/0003-4819-103-6-1034. [DOI] [PubMed] [Google Scholar]
- 37.Schroder H, Elosua R, Vila J, Marti H, Covas MI, Marrugat J. Secular Trends of Obesity and Cardiovascular Risk Factors in a Mediterranean Population. Obesity. 2007;15(3):557–62. doi: 10.1038/oby.2007.574. [DOI] [PubMed] [Google Scholar]
- 38.Sauvaget C, Ramadas K, Thomas G, Vinoda J, Thara S, Sankaranarayanan R, et al. Body mass index,weightchange and mortality risk in a prospective study in India. Int J Epidemiol. 2008;37(5):990–1004. doi: 10.1093/ije/dyn059. [DOI] [PubMed] [Google Scholar]
- 39.Hu FB, Wang B, Chen C, Jin Y, Yang J, Stampfer MJ, et al. Body mass index and cardiovascular risk factors in a rural Chinese population. Am J Epidemiol. 2000;151(1):88–97. doi: 10.1093/oxfordjournals.aje.a010127. [DOI] [PubMed] [Google Scholar]
- 40.Poirier P. Targeting abdominal obesity in cardiology can we be effective. Can J Cardiol. 2008;24(Suppl D):13D–17D. doi: 10.1016/s0828-282x(08)71044-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Katzel LI, Busby-Whitehead MJ, Goldberg AP. Adverse effects of abdominal obesity on lipoproteinlipids in healthy older men. Exp Gerontol. 1993;28(4-5):411–20. doi: 10.1016/0531-5565(93)90067-n. [DOI] [PubMed] [Google Scholar]
- 42.Chumlea WC, Guo SS, Kuczmarski RJ, Flegal KM, Johnsoin Ch, Heymsfield SB, et al. Body composition estimates from NHANE SIII bioelectrical impedance data. INT Jobes Relat Metab Disord. 2002;26(12):1596–609. doi: 10.1038/sj.ijo.0802167. [DOI] [PubMed] [Google Scholar]
- 43.Aronne LJ. Classification of obesity and assessment of obesity-related health risks. Obes Res. 2002;10(2):105S–15S. doi: 10.1038/oby.2002.203. [DOI] [PubMed] [Google Scholar]
- 44.Oirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, Eckel RH. American Heart Association; Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Obesity and cardiovascular disease: path physiology, evaluation, and effect of weight loss: An update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113(6):898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- 45.Li C, Engstrom G, Hedblad B, Calling S, Berglund G, Janzon L. Sex differences in the relationships between BMI, WHR and incidence of cardiovascular disease: a population-based cohort study. Int J Obes. 2006;30(12):1775–81. doi: 10.1038/sj.ijo.0803339. [DOI] [PubMed] [Google Scholar]
- 46.Allison DB, Fontain KR, Manson JE, Stevens J, VanItallie TB. Annual deaths attributable to obesity in the United States. JAMA. 1999;282(16):1530–8. doi: 10.1001/jama.282.16.1530. [DOI] [PubMed] [Google Scholar]