Abstract
Purpose
To establish and validate a formula to predict spectral domain (SD)-optical coherence tomography (OCT) retinal nerve fiber layer (RNFL) thickness from time domain (TD)-OCT RNFL measurements and other factors.
Methods
SD-OCT and TD-OCT scans were obtained on the same day from healthy participants and patients with glaucoma. Univariate and multivariate linear regression relationships were analyzed to convert average Stratus TD-OCT measurements to average Cirrus SD-OCT measurements. Additional baseline characteristics included age, sex, intraocular pressure, central corneal thickness, spherical equivalent, anterior chamber depth, optic disc area, visual field (VF) mean deviation, and pattern standard deviation. The formula was generated using a training set of 220 patients and then evaluated on a validation dataset of 105 patients.
Results
The training set included 71 healthy participants and 149 patients with glaucoma. The validation set included 27 healthy participants and 78 patients with glaucoma. Univariate analysis determined that TD-OCT RNFL thickness, age, optic disc area, VF mean deviation, and pattern standard deviation were significantly associated with SD-OCT RNFL thickness. Multivariate regression analysis using available variables yielded the following equation: SD-OCT RNFL = 0.746 × TD-OCT RNFL + 17.104 (determination coefficient [R2] = 0.879). In the validation sample, the multiple regression model explained 85.6% of the variance in the SD-OCT RNFL thickness.
Conclusions
The proposed formula based on TD-OCT RNFL thickness may be useful in predicting SD-OCT RNFL thickness. Other factors associated with SD-OCT RNFL thickness, such as age, disc area, and mean deviation, did not contribute to the accuracy of the final equation.
Keywords: Glaucoma, Retinal nerve fiber layer, Spectral domain optical coherence tomography, Time domain optical coherence tomography
Glaucoma is a progressive disease characterized by pathological loss of ganglion cells and the retinal nerve fiber layer (RNFL) [1-3]. Detecting disease progression, which is evidenced by structural or functional changes in the retinas of patients with glaucoma, is essential to evaluate damage and the efficacy of therapy [4]. Repeated measurements of RNFL thickness in the same patient over time are an important component of glaucoma management.
Optical coherence tomography (OCT) provides cross-sectional imaging of the eye and enables evaluation and quantification of cross-sectional peripapillary RNFL thickness [5]. Time domain (TD)-OCT is a commonly used technique for which the Stratus OCT (Carl Zeiss Meditec, Dublin, CA, USA) is the most often used device. Recently, OCT technology has advanced considerably and now incorporates spectral domain (SD) imaging, which offers significant advantages over traditional TD-OCT techniques, including a faster scanning speed and higher-resolution RNFL imaging [6,7]. Many patients who have been scanned with Stratus OCT can now potentially be scanned with Cirrus OCT (Carl Zeiss Meditec) [8]. The clinical relevance of the new SD technology requires data from these devices to be compared with preexisting, widely accepted TD standards and with each other [9].
Previous studies have indicated that measurements with TD-OCT and SD-OCT instruments cannot be considered interchangeable, although the two types of measurements have been strongly correlated [8-14]. Equations based on regression models to calculate SD-OCT RNFL thickness measurements from TD-OCT RNFL measurements in patients with glaucoma have been previously proposed [8,15]. However, no equation has yet been developed that specifically estimates SD-OCT RNFL thickness in consideration of clinical and demographic variables.
The present study was designed to determine the relationship between RNFL thickness measurements from TD-OCT and SD-OCT in normal participants and patients with glaucoma and to develop a new formula using regression analysis to predict SD-OCT RNFL thickness that includes clinical and demographic factors. Cross-validation analysis was then used to evaluate the validity of this novel formula.
Materials and Methods
Participants
Participants were consecutively enrolled from the Glaucoma-Cataract Clinic of Severance Hospital at Yonsei University (Seoul, Korea) from January 2009 to June 2010. The Severance Hospital Institutional Review Board approved the protocol, and the study complied with the tenets of the Declaration of Helsinki. Informed consent was obtained from all participants prior to their participation in the study.
All participants underwent a full ophthalmic examination, which included measurements of visual acuity, refraction, and intraocular pressure (by Goldmann applanation tonometry), as well as slit lamp examination, gonioscopy, fundus examination with a 90 D lens, pachymetry (DGH-1000 instrument; DGH Technology Inc., Frazer, PA, USA), and visual field (VF) testing with standard automated perimetry (Humphrey field analyzer II with Swedish Interactive Thresholding Algorithm standard 24-2, Carl Zeiss Meditec). A reliable VF test result was defined as less than 20% fixation loss and false-positive and false-negative errors less than 15%. Axial ocular dimensions, including axial length and anterior chamber depth, were measured using partial laser interferometry (IOL master, Carl Zeiss Meditec). All eyes underwent Stratus TD-OCT and Cirrus SD-OCT after pupillary dilation (minimum diameter, 5 mm). Disc area measurements were obtained using the optic nerve head mode of Stratus OCT (Carl Zeiss Meditec). All measurements in any individual patient were performed within a single day.
Normal eyes had a best corrected visual acuity of 20 / 40 or better, with a refractive error between +3.00 and -8.00 diopters, intraocular pressure of 21 mmHg or lower, open angle on gonioscopy, normal fundus examination, normal-appearing optic nerve head, and reliable normal VF tests with normal glaucoma hemifield test results, as well as a normal mean deviation and pattern standard deviation (p > 0.05).
Glaucomatous eyes were defined as eyes with a glaucomatous VF defect confirmed by two reliable VF examinations and by the appearance of a glaucomatous optic disc with typical loss of neuroretinal rim as judged by slit lamp biomicroscopy (cup-to-disc ratio, >0.7; intereye cup asymmetry, >0.2; or neuroretinal rim notching, focal thinning, disc hemorrhage, or vertical elongation of the optic cup). Intraocular pressure was not used as a criterion for the glaucoma group. A field defect was defined as having three or more significant (p < 0.05) non-edged contiguous points with at least one at the p < 0.01 level, located on the same side of the horizontal meridian in the pattern deviation plot, classified as outside normal limits in the glaucoma hemifield test, and confirmed with at least two VF examinations. Only patients with open anterior chamber angle, a corrected visual acuity of 20 / 40 or better, and refractive error from +3.00 to -8.00 diopters were selected. Eyes with conditions affecting RNFL thickness measurements, such as diabetic retinopathy, degenerative or exudative retinopathy, optic nerve head drusen, peripapillary atrophy, or tilted disc syndrome, were excluded from the study [16-18]. Participants who had undergone previous ocular surgery or who had vitreous opacity were also excluded from the study.
Optical coherence tomography technique
Cross-sectional imaging of the peripapillary area was first performed using Stratus-OCT (software ver. 4.0.1). The average RNFL thickness was measured with the Fast RNFL scan program, which consisted of three sets of 256 A-scans along a circle with a 3.46 mm diameter centered on the optic disc, which was controlled by the examiner. The scanning took 1.92 seconds to complete.
The average RNFL thickness was then determined using the optic disc cube protocol on Cirrus OCT (software ver. 3.0). This protocol generates a cube of data through a 6-mm square grid by acquiring a series of 200 horizontal scan lines, each of which is composed of 200 A-scans. A calculation circle 3.46 mm in diameter and consisting of 256 A-scans was automatically positioned around the optic disc.
A single, well-trained technician performed all OCT examinations. The signal strength of each scan on the Stratus and Cirrus was at least 6 (range, 0 to 10). Scans with misalignment, segmentation failure, or decentration of the measurement circle were excluded from the analysis.
Training and validation sets
The cohort was randomly subdivided into a training set and a validation set. In total, 325 participants enrolled in the present study, of whom 220 were randomly selected as the training sample; the remaining 105 participants constituted the validation sample. The associations between TD-OCT RNFL thickness and SD-OCT RNFL thickness identified in the training set were then independently evaluated using the validation set.
Statistical methods
For cases in which both eyes of a patient were eligible for analysis, one eye was randomly selected to be evaluated for the present study. Scatter plots showing the differences between the two measurements and their averages were used to assess agreement between the two measurement types (SD-OCT and TD-OCT RNFL measurements, and observed and predicted SD-OCT RNFL measurements using our equation), as described by Bland and Altman [19]. The 95% limits of agreement, which were centered around the means of the differences, were also determined.
The relationships between OCT measurements and other baseline characteristics were assessed by linear regression applied to the training sample consisting of a random sample of 220 of the 325 participants. Demographic and clinical variables assessed in the current study included age, sex, intraocular pressure, central corneal thickness, spherical equivalent, axial length, anterior chamber depth, optic disc area, VF mean deviation, and pattern standard deviation. Factors demonstrating a significant relationship (a p-value less than 0.1 as determined by univariate regression analysis) were further analyzed using multiple stepwise regression analyses. A regression model for predicting SD-OCT RNFL measurements was established based on these results. Predicted SD-OCT RNFL thickness values were calculated according to this formula and compared with the actual SD-OCT RNFL thickness measurements to evaluate the performance of the prediction equation.
The regression coefficients calculated from the training sample were then applied to obtain predicted SD-OCT RNFL thicknesses in a separate validation sample consisting of 105 participants from the total sample group of 325 participants. Statistical analysis was performed using SPSS ver. 12.0.0 (SPSS Inc., Chicago, IL, USA). A p-value less than 0.05 was considered statistically significant.
Results
Participant characteristics
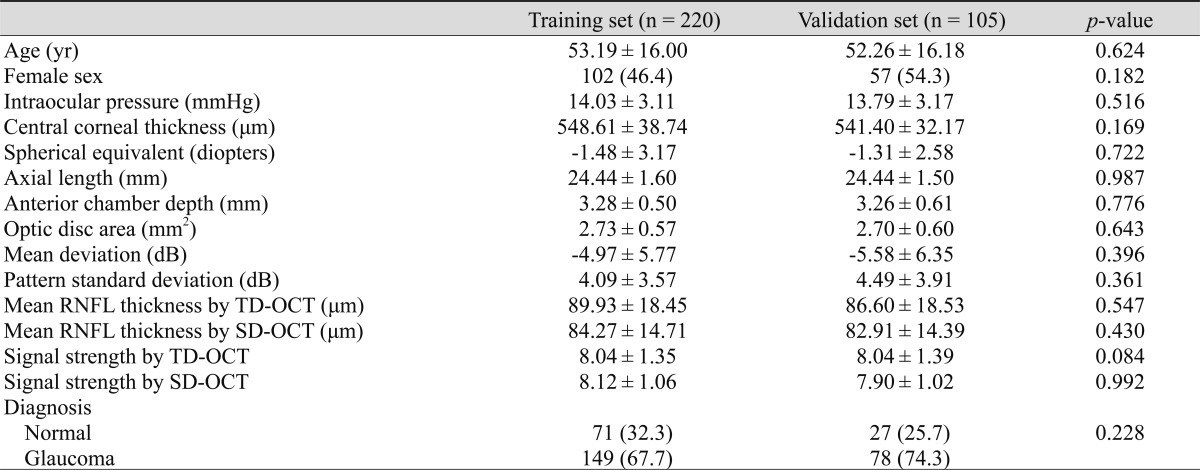
Measurements and evaluation results of 325 eyes from 325 patients were included in the present study. Patient characteristics of the training and validation sets are presented in Table 1. The mean age and sex proportions were similar between the training and validation samples. The training set included 71 healthy participants and 149 patients with glaucoma. The validation set included 27 healthy participants and 78 patients with glaucoma.
Table 1.
Characteristics of the study population
Values are presented mean ± SD or as number (%).
RNFL = retinal nerve fiber layer; TD = time domain; OCT = optical coherence tomography; SD = spectral domain.
Comparison of Stratus OCT and Cirrus OCT retinal nerve fiber layer thickness measurements
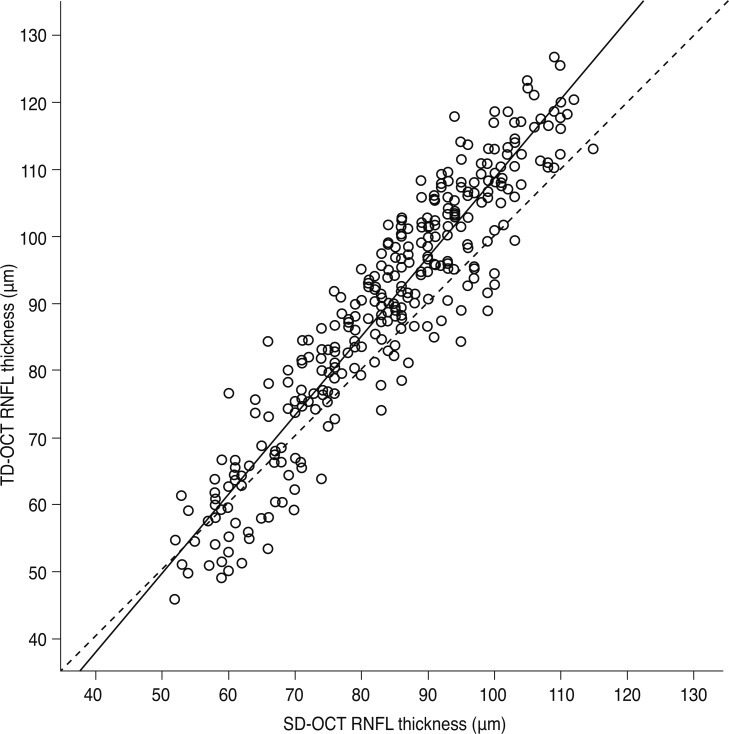
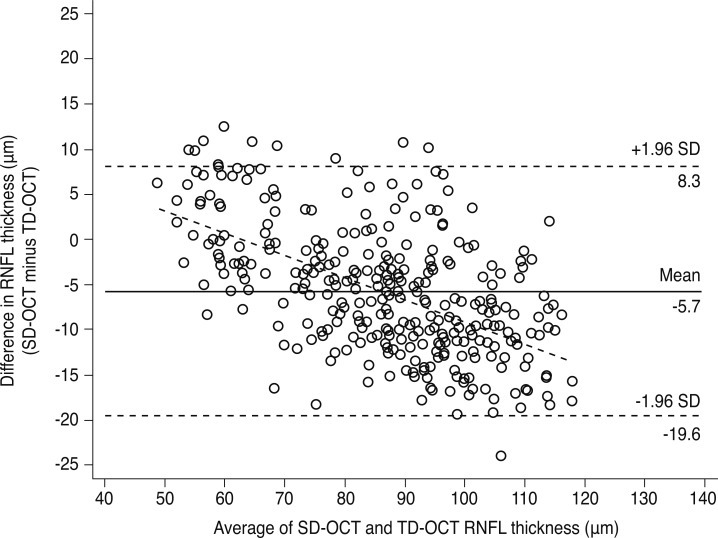
As shown in Fig. 1, TD-OCT RNFL measurements overestimated SD-OCT RNFL measurements, especially in cases of greater RNFL thickness (slope = 1.181, p < 0.001, R2 = 0.872, standard error [SE] of estimate = 6.61), although the measurements were highly positively correlated (r = 0.934, p < 0.001). Fig. 2 shows the Bland-Altman plots used to assess agreement of the mean RNFL measurements between the two devices. Analysis of the plot revealed a considerable discrepancy between the RNFL thickness measurements obtained by the two instruments. The limit of agreement range (95% confidence interval [CI]) of the mean RNFL thickness between the two OCTs was 27.9 µm. Additionally, a significant proportional bias of the mean RNFL thickness measurements existed between the Stratus and Cirrus devices (r = -0.233, p < 0.001). For thinner RNFLs, the Stratus measurements tended to be thinner than the Cirrus measurements, whereas for thicker RNFLs, Stratus measurements tended to be thicker than the Cirrus measurements. The mean measurement difference between the Stratus and Cirrus devices was -5.67 ± 7.11 µm (Cirrus OCT minus Stratus OCT RNFL thicknesses; 95% CI, -6.44 to -4.89).
Fig. 1.
Relationship between thicknesses of spectral domain (SD)-optical coherence tomography (OCT) retinal nerve fiber layer (RNFL) and time domain (TD)-OCT RNFL (slope = 1.181, p < 0.001; intercept = -9.497; adjusted determination coefficient = 0.872; standard error of estimate = 6.61).
Fig. 2.
Bland-Altman plot comparing the mean retinal nerve fiber layer (RNFL) thickness measurements obtained with spectral domain (SD)-optical coherence tomography (OCT) and time domain (TD)-OCT. The difference between both measurements is plotted against the average of both measurements (slope = -0.233, p < 0.001). Mean difference ± standard deviation: SD-OCT minus TD-OCT, -5.67 ± 7.11 µm; 95% confidence interval, -6.44 to -4.89; limits of agreement, -19.6 to 8.3 µm.
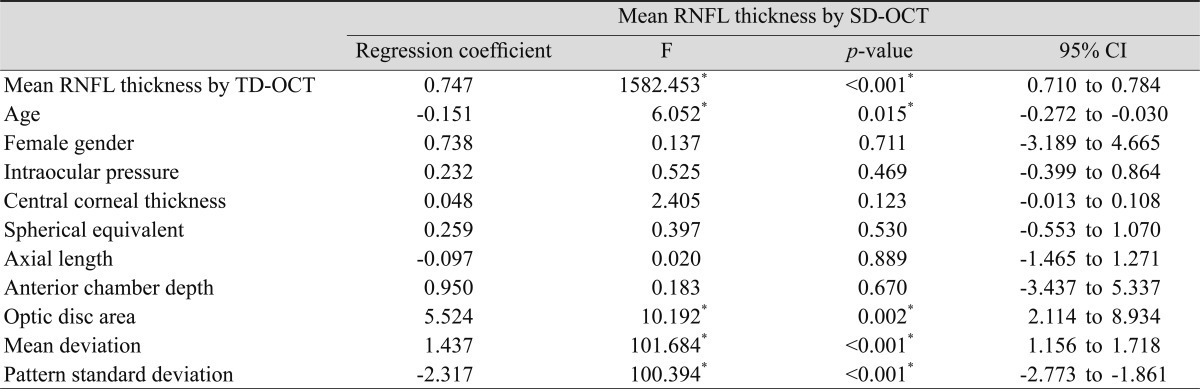
Prediction of SD-OCT RNFL thickness from multiple regression models
Univariate analysis indicated that TD-OCT RNFL thickness, age, optic disc area, VF mean deviation, and VF pattern standard deviation were significantly associated with SD-OCT RNFL thickness. In contrast, the effects of intraocular pressure, central corneal thickness, spherical equivalent, axial length, and anterior chamber depth on the estimated SD-OCT RNFL thickness were negligible (Table 2). Variables with a p-value less than 0.1 were included in the final model. Because mean deviation and pattern standard deviation were highly correlated with each other, only mean deviation was included in the multivariate stepwise regression analyses.
Table 2.
Predictors of SD-OCT RNFL thickness (univariate linear regression analysis, n = 220)
SD = spectral domain; OCT = optical coherence tomography; RNFL = retinal nerve fiber layer; CI = confidence interval; TD = time domain.
*Statistically significant values.
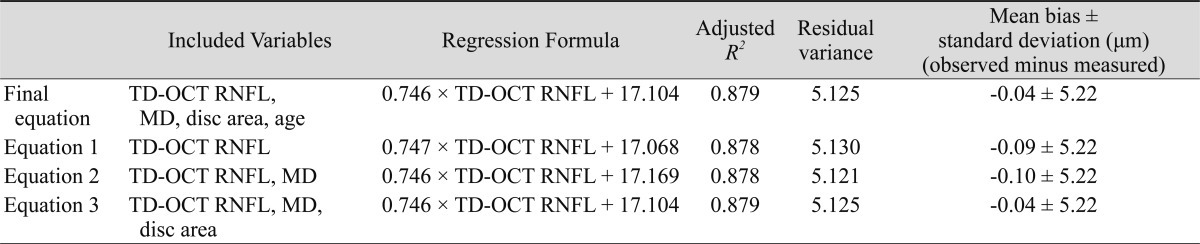
Table 3 shows the results of the multivariate stepwise regression analyses used for the prediction of SD-OCT RNFL thickness. The multiple linear regression analysis generated the following prediction equation: SD-OCT RNFL thickness = 0.746 × TD-OCT RNFL thickness + 17.104. The R2 value indicates that the model explains 87.9% of the variability between the TD-OCT and SD-OCT RNFL thicknesses (residual variance = 5.125). TD-OCT RNFL thickness was the only significant factor in the final model, which did not change based on inclusion of various variable combination sets. The R2 of the final equation was similar to that of an equation which did not consider any demographic or clinical variables (equation 1). Other equations for estimating SD-RNFL thickness also exhibited reasonable R2 and minimal bias.
Table 3.
Comparison of equations that predict SD-OCT RNFL thickness (multiple linear regression, n = 220)
SD = spectral domain; OCT = optical coherence tomography; RNFL = retinal nerve fiber layer; R2 = determination coefficient; TD = time domain; MD = mean deviation.
Relationship between predicted SD-OCT RNFL thickness and measured thickness
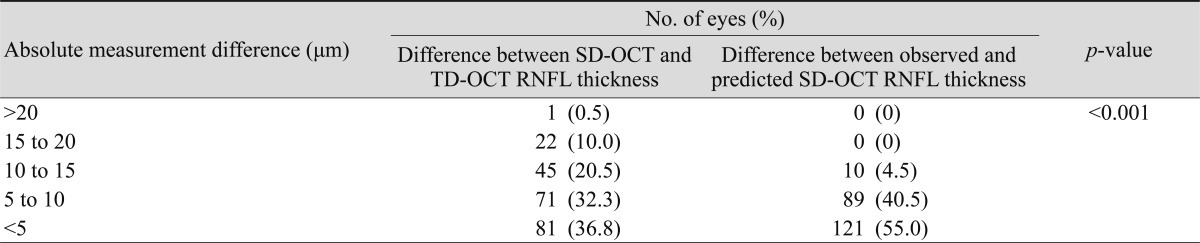
Table 4 shows the categorical comparison of the absolute difference between the TD-OCT and SD-OCT measurements or between the observed and predicted SD-OCT RNFL thicknesses. For RNFLs of average thickness, the difference between the SD-OCT and TD-OCT measurements was within 10 µm in 152 (69.1%) patients and within 5 µm in 81 (36.8%) patients. SD-OCT and TD-OCT measurements differed by more than 15 µm in 23 (10.5%) patients. Comparing the observed and calculated SD-OCT RNFL measurements using our formula revealed no measurements differences greater than 15 µm. A predicted average RNFL thickness within 10 µm of the observed measurement was detected in 210 (95.5%) eyes and that within 5 µm of the observed measurement was detected in 121 (55.0%) eyes.
Table 4.
Categorical comparison of difference between absolute measurements (Fisher's exact test, n = 220)
SD = spectral domain; OCT = optical coherence tomography; TD = time domain; RNFL = retinal nerve fiber layer.
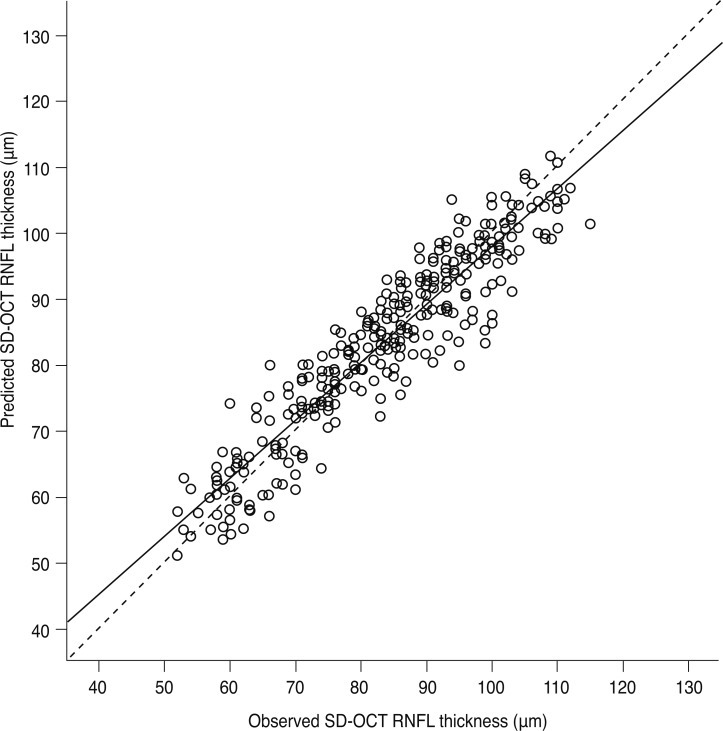
Fig. 3 shows a scatter plot of the measured versus predicted SD-OCT RNFL thickness values as determined by our regression model. As expected, the RNFL thickness measurements predicted with our formula systematically deviated only minimally from the measured SD-OCT RNFL thickness (slope = 0.881, p < 0.001, R2 = 0.872, SE of estimate = 4.93).
Fig. 3.
Relationship between observed and predicted spectral domain (SD)-optical coherence tomography (OCT) retinal nerve fiber layer (RNFL) thickness (slope = 0.881, p < 0.001; intercept = 10.019; adjusted determination coefficient = 0.872; standard error of estimate = 4.93).
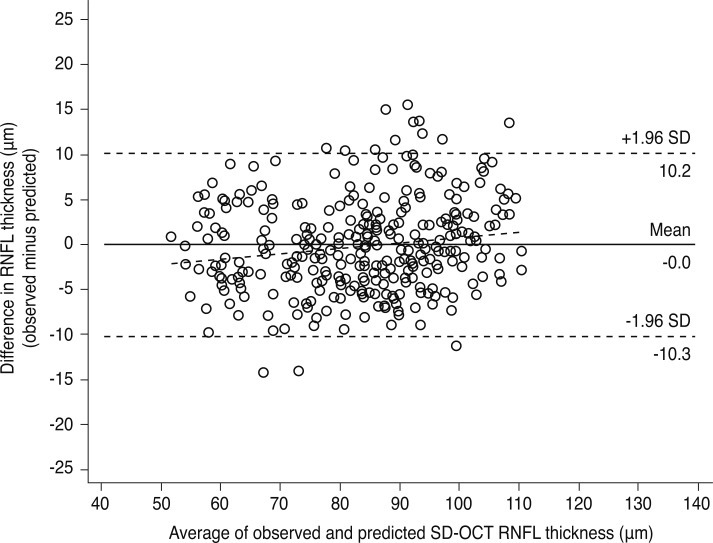
A Bland-Altman plot showing the agreement in SD-OCT RNFL thickness between observed and predicted measurements is shown in Fig. 4. This analysis demonstrated good agreement between measured and predicted SD-OCT RNFL thicknesses. Estimated RNFL thicknesses calculated by our equation showed minimal bias compared to the observed RNFL thicknesses (mean measurement difference, -0.04 ± 5.22 µm; measured minus predicted RNFL thicknesses; 95% CI, -0.61 to 0.53). The slope of the regression line of the difference between the measured and predicted values compared to the average of the two was slightly positive and statistically significant, indicating the existence of proportional bias (r = 0.060, p = 0.004). The plots demonstrate a wide range of agreement between observed and predicted RNFL thickness measurements (limit of agreement width, 20.5 µm).
Fig. 4.
Bland-Altman plot showing observed versus predicted spectral domain (SD)-optical coherence tomography (OCT) retinal nerve fiber layer (RNFL) thickness. The difference between both measurements is plotted against the average of both measurements (slope = 0.060, p = 0.004). Mean difference ± standard deviation: observed minus predicted, -0.04 ± 5.22 µm; 95% confidence interval, -0.61 to 0.53; limits of agreement, -10.3 to 10.2 µm).
Verification of the prediction model
The validation dataset confirmed that SD-OCT RNFL thickness was directly correlated with the TD-OCT RNFL thickness. The multiple regression model explained 85.6% of the variance of the SD-OCT RNFL thicknesses in the validation sample (residual variance = 5.481).
Discussion
Detecting disease progression in patients with glaucoma is essential for patient monitoring and to evaluate the efficacy of therapy. The present study provides an equation that can predict SD-OCT RNFL measurements using conventional TD-OCT RNFL measurements. Other formulas have been proposed to calculate SD-OCT RNFL thicknesses [8,15], but none have adjusted for demographic and clinical variables. To improve the predictive accuracy of our equation, clinical and demographic variables were included in addition to the TD-OCT RNFL measurements. Univariate analysis showed that factors associated with greater SD-OCT RNFL thickness included greater TD-OCT RNFL thickness, younger age, larger disc area, higher mean deviation, and lower pattern standard deviation. Stepwise multiple regression analysis was then used to determine the best combination set of variables to predict SD-OCT RNFL thickness. The results of the analysis indicated that the best and final equation included only TD-OCT RNFL thickness.
Discrepancies between TD-OCT and SD-OCT measurements
OCT measurements are not interchangeable and should be interpreted considering the various scanning protocols and segmentation algorithms of different devices [9,10]. The reason underlying this difference in OCT techniques may be that new OCT systems involve improved axial resolution compared to the previous generation [20]. By producing higher resolution scans compared to TD-OCT, SD-OCT may provide measurements that reflect a more accurate delineation of RNFL margins [11]. Alternatively, the discrepancy in measurements may be related to intrinsic differences between the instruments and software edge-detection algorithms that measure the RNFL [11,14]. The segmentation algorithms for TD-OCT and SD-OCT are different: Cirrus identifies the bottom of the nerve fiber layer, whereas Stratus localizes the top of the ganglion cell layer [8]. Another reason for the differences may be because the scan registration process performed by the Cirrus algorithms is fully automated, which reduces the likelihood of operator error [10,11,14,20,21].
Bland-Altman plots showed that, for thinner RNFLs, the Stratus measurement values tended to be smaller compared to values determined by Cirrus. In cases of great RNFL thicknesses, Stratus measurements tended to be thicker than measurements determined by Cirrus. These results are generally consistent with earlier studies reporting differences in the measurement values between 3D OCT-1000 (Topcon Inc., Paramus, NJ, USA) and Stratus OCT [12], RTVue-100 (Optovue Inc., Fremont, CA, USA) and Stratus OCT [13], and Cirrus OCT and Stratus OCT [8-11,21]. A possible explanation why Cirrus OCT yields thicker measurements in severely diseased eyes and thinner measurements in healthy eyes compared to Stratus OCT is the difference in the inclusion of exposed blood vessels in the measurements [8]. In cases of thin RNFLs, the TD-OCT algorithm is not sufficiently sensitive to local changes and includes few of the blood vessels in regions where most of the axons are lost, while the SD-OCT algorithm incorporates most of the blood vessels when determining RNFL thickness. In contrast, the SD-OCT algorithm is sensitive to local signal changes and thus does not include the shadows of the blood vessels present in thick RNFLs, whereas TD-OCT does include shadows from major blood vessels [12].
Consideration of covariates in predicting SD-OCT RNFL thickness
In the present study, the authors attempted to develop a valuable prediction model for RNFL measurements using a new imaging device considering both clinical and demographic variables. Multivariate analysis results indicated that no factors were useful as covariates for constructing a predictive formula for SD-OCT RNFL thickness. The results showed that a formula considering clinical and demographic variables was not able to more precisely predict SD-OCT RNFL thickness than a simple formula. A possible explanation is that the relationship between clinical/demographic variables and TD-OCT RNFL measurements is very similar to the relationship between these variables and SD-OCT RNFL measurements. RNFL thickness as measured by TD-OCT was associated with age (p = 0.002), disc area (p = 0.004), mean deviation (p < 0.001), pattern standard deviation (p < 0.001), and signal strength (p < 0.001). Consistent with TD-OCT, RNFL thickness as measured by SD-OCT was associated with age (p = 0.015), optic disc area (p = 0.002), mean deviation (p < 0.001), pattern standard deviation (p < 0.001), and signal strength (p = 0.010).
Remaining unpredictability
In the present study, RNFL values estimated using our formula derived from TD-OCT RNFL measurements were consistent with the observed SD-OCT RNFL measurements, and the average bias (-0.04 ± 5.22, observed minus estimated) and proportional bias (slope = 0.060, p < 0.001) were quite small. However, the limit of agreement range (average bias ± 1.96 standard deviation of the difference) was relatively broad (-10.3 to 10.2 µm). The limits of axial resolution for the Stratus OCT and Cirrus OCT instruments is taken as 10 µm and 5 µm, respectively [20,22]. The 95% limit of agreement between the observed and predicted values was 20.5 µm and was greater than the limit of resolution of both the Stratus OCT and the Cirrus OCT.
Measurement variations may have contributed to the large range of the agreement limit in the current study. The clinical utility of any instrument depends on the reproducibility of its measurements. With SD technology, the image acquisition time and resolution are improved compared with those of the TD-OCT technique. The reproducibility of RNFL measurements with the SD-OCT was reported to be higher than that with the TD-OCT both in normal participants and in patients with glaucoma [23,24]. However, our formula calculated SD-OCT RNFL thickness from TD-OCT RNFL values. Therefore, predicted SD-OCT RNFL measurements have greater test-retest variability than those expected with actual SD-OCT scanning.
Limitations
The present study has several limitations. The study included a small number of participants, and the validation sample was drawn from the same population as the training sample. Thus, the performance of the equation in populations with different distributions of patient characteristics may not be the same as the performance observed in the validation sample. Signal strength was not considered in the present study. Because signal strength has been shown to affect RNFL thickness measurements using TD-OCT [25], the differences in signal strength between the two instruments may be a possible cause of variability [11,26]. However, only scans with adequate signal strength were included in the present study, and no differences in signal strength were observed between scans taken with the two devices (paired t-test, p = 0.437). Lastly, caution should be taken in direct application of this formula in everyday clinical practice. Although this formula has a definite practical advantage in SD-OCT RNFL prediction, the limit of agreement widths between observed and predicted SD-OCT RNFL thicknesses were high, and the difference between measurements was greater than 5 µm in 45% of the patients. A comprehensive general assessment is required to interpret the predicted values.
Conclusions
In the present study, equations were developed to predict SD-OCT RNFL thickness using multiple regression applied to a randomly-selected training sample of 220 patients and validated in 105 patients in the study cohort. The findings indicate that the application of this formula yields an accurate SD-OCT RNFL thickness predicted from TD-OCT RNFL thickness in healthy participants and patients with glaucoma. The inclusion of other clinical and demographic factors to correct TD-OCT RNFL thickness did not improve the prediction accuracy in this study group. Validation with a larger cohort and broader distribution of other possible confounding variables is warranted.
Acknowledgements
This study was supported by a grant of the Korea Health technology R&D Project, Ministry of Health & Welfare, Republic of Korea (A101727, CYK and A110395, NRK).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Quigley HA, Dunkelberger GR, Green WR. Retinal ganglion cell atrophy correlated with automated perimetry in human eyes with glaucoma. Am J Ophthalmol. 1989;107:453–464. doi: 10.1016/0002-9394(89)90488-1. [DOI] [PubMed] [Google Scholar]
- 2.Quigley HA, Miller NR, George T. Clinical evaluation of nerve fiber layer atrophy as an indicator of glaucomatous optic nerve damage. Arch Ophthalmol. 1980;98:1564–1571. doi: 10.1001/archopht.1980.01020040416003. [DOI] [PubMed] [Google Scholar]
- 3.Sommer A, Miller NR, Pollack I, et al. The nerve fiber layer in the diagnosis of glaucoma. Arch Ophthalmol. 1977;95:2149–2156. doi: 10.1001/archopht.1977.04450120055003. [DOI] [PubMed] [Google Scholar]
- 4.Giangiacomo A, Garway-Heath D, Caprioli J. Diagnosing glaucoma progression: current practice and promising technologies. Curr Opin Ophthalmol. 2006;17:153–162. doi: 10.1097/01.icu.0000193089.52561.ac. [DOI] [PubMed] [Google Scholar]
- 5.Schuman JS, Hee MR, Puliafito CA, et al. Quantification of nerve fiber layer thickness in normal and glaucomatous eyes using optical coherence tomography. Arch Ophthalmol. 1995;113:586–596. doi: 10.1001/archopht.1995.01100050054031. [DOI] [PubMed] [Google Scholar]
- 6.Kim NR, Lee ES, Seong GJ, et al. Spectral-domain optical coherence tomography for detection of localized retinal nerve fiber layer defects in patients with open-angle glaucoma. Arch Ophthalmol. 2010;128:1121–1128. doi: 10.1001/archophthalmol.2010.204. [DOI] [PubMed] [Google Scholar]
- 7.Leitgeb R, Hitzenberger C, Fercher A. Performance of fourier domain vs. time domain optical coherence tomography. Opt Express. 2003;11:889–894. doi: 10.1364/oe.11.000889. [DOI] [PubMed] [Google Scholar]
- 8.Knight OJ, Chang RT, Feuer WJ, Budenz DL. Comparison of retinal nerve fiber layer measurements using time domain and spectral domain optical coherent tomography. Ophthalmology. 2009;116:1271–1277. doi: 10.1016/j.ophtha.2008.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang J, Liu X, Wu Z, et al. Macular and retinal nerve fiber layer thickness measurements in normal eyes with the Stratus OCT, the Cirrus HD-OCT, and the Topcon 3D OCT-1000. J Glaucoma. 2011;20:118–125. doi: 10.1097/IJG.0b013e3181d786f8. [DOI] [PubMed] [Google Scholar]
- 10.Takagishi M, Hirooka K, Baba T, et al. Comparison of retinal nerve fiber layer thickness measurements using time domain and spectral domain optical coherence tomography, and visual field sensitivity. J Glaucoma. 2011;20:383–387. doi: 10.1097/IJG.0b013e3181efb371. [DOI] [PubMed] [Google Scholar]
- 11.Vizzeri G, Weinreb RN, Gonzalez-Garcia AO, et al. Agreement between spectral-domain and time-domain OCT for measuring RNFL thickness. Br J Ophthalmol. 2009;93:775–781. doi: 10.1136/bjo.2008.150698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hood DC, Raza AS, Kay KY, et al. A comparison of retinal nerve fiber layer (RNFL) thickness obtained with frequency and time domain optical coherence tomography (OCT) Opt Express. 2009;17:3997–4003. doi: 10.1364/oe.17.003997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gonzalez-Garcia AO, Vizzeri G, Bowd C, et al. Reproducibility of RTVue retinal nerve fiber layer thickness and optic disc measurements and agreement with Stratus optical coherence tomography measurements. Am J Ophthalmol. 2009;147:1067–1074. 1074.e1. doi: 10.1016/j.ajo.2008.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sung KR, Kim DY, Park SB, Kook MS. Comparison of retinal nerve fiber layer thickness measured by Cirrus HD and Stratus optical coherence tomography. Ophthalmology. 2009;116:1264–1270. 1270.e1. doi: 10.1016/j.ophtha.2008.12.045. [DOI] [PubMed] [Google Scholar]
- 15.Hong S, Seong GJ, Kim SS, et al. Comparison of peripapillary retinal nerve fiber layer thickness measured by spectral vs. time domain optical coherence tomography. Curr Eye Res. 2011;36:125–134. doi: 10.3109/02713683.2010.533807. [DOI] [PubMed] [Google Scholar]
- 16.Lim MC, Tanimoto SA, Furlani BA, et al. Effect of diabetic retinopathy and panretinal photocoagulation on retinal nerve fiber layer and optic nerve appearance. Arch Ophthalmol. 2009;127:857–862. doi: 10.1001/archophthalmol.2009.135. [DOI] [PubMed] [Google Scholar]
- 17.Katz BJ, Pomeranz HD. Visual field defects and retinal nerve fiber layer defects in eyes with buried optic nerve drusen. Am J Ophthalmol. 2006;141:248–253. doi: 10.1016/j.ajo.2005.09.029. [DOI] [PubMed] [Google Scholar]
- 18.Moschos MM, Triglianos A, Rotsos T, et al. Tilted disc syndrome: an OCT and mfERG study. Doc Ophthalmol. 2009;119:23–28. doi: 10.1007/s10633-009-9165-x. [DOI] [PubMed] [Google Scholar]
- 19.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 20.Moreno-Montanes J, Olmo N, Alvarez A, et al. Cirrus high-definition optical coherence tomography compared with Stratus optical coherence tomography in glaucoma diagnosis. Invest Ophthalmol Vis Sci. 2010;51:335–343. doi: 10.1167/iovs.08-2988. [DOI] [PubMed] [Google Scholar]
- 21.Leung CK, Cheung CY, Weinreb RN, et al. Retinal nerve fiber layer imaging with spectral-domain optical coherence tomography: a variability and diagnostic performance study. Ophthalmology. 2009;116:1257–1263. 1263.e1–1263.e2. doi: 10.1016/j.ophtha.2009.04.013. [DOI] [PubMed] [Google Scholar]
- 22.Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science. 1991;254:1178–1181. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mwanza JC, Chang RT, Budenz DL, et al. Reproducibility of peripapillary retinal nerve fiber layer thickness and optic nerve head parameters measured with cirrus HD-OCT in glaucomatous eyes. Invest Ophthalmol Vis Sci. 2010;51:5724–5730. doi: 10.1167/iovs.10-5222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu H, de Boer JF, Chen TC. Reproducibility of retinal nerve fiber layer thickness measurements using spectral domain optical coherence tomography. J Glaucoma. 2011;20:470–476. doi: 10.1097/IJG.0b013e3181f3eb64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu Z, Vazeen M, Varma R, et al. Factors associated with variability in retinal nerve fiber layer thickness measurements obtained by optical coherence tomography. Ophthalmology. 2007;114:1505–1512. doi: 10.1016/j.ophtha.2006.10.061. [DOI] [PubMed] [Google Scholar]
- 26.Lee ES, Kim NR, Seong GJ, et al. Effect of signal strength on agreements for retinal nerve fiber layer thickness measurement and its color code classification between Stratus and Cirrus optical coherence tomography. J Glaucoma. 2011;20:371–376. doi: 10.1097/IJG.0b013e3181efb3a7. [DOI] [PubMed] [Google Scholar]