Abstract
A 54-year-old female patient who had been undergoing anti-cancer chemotherapy and radiotherapy for seven years after surgery for left breast cancer visited our clinic for visual disturbance in the right eye at nine months after paclitaxel administration. The best-corrected visual acuity was 0.5 in the right eye and 1.0 in the left eye. The patient was diagnosed with maculopathy due to paclitaxel administration based on the finding of cystoid macular edema in the right eye on fundus examination and optical coherence tomography; however, no leakage was detected on fluorescein angiography. Thus, drug replacement was planned. On the other hand, no abnormal finding was observed in the left eye. However, as the anti-cancer effect of paclitaxel is significant, replacing paclitaxel with another agent was not warranted; therefore, maintenance therapy with methazolamide was performed before and after administering the anti-cancer agent. Aggravation of cystoid macular edema was prevented, and vision improvement was achieved by oral maintenance therapy with methazolamide. In addition, the same fundus findings as shown in the right eye were detected in the left eye at 16 months after paclitaxel administration. After administering methazolamide, macular thickness was reduced, and vision was improved in the left eye. Paclitaxel administration was discontinued due to cutaneous metastasis from the breast cancer, and another anti-cancer agent was then administered. No subsequent cystoid macular edema has occurred.
Keywords: Macular edema, Methazolamide, Paclitaxel
Paclitaxel is well known for its treatment effect on metastatic breast cancer. To date, various side-effects of paclitaxel have been reported. Joshi and Garretson [1] reported cystoid macular edema caused by paclitaxel. Based on this, we effectively prevented cystoid macular edema progression and treated it with oral administration of methazolamide without stopping paclitaxel administration once the cystoid macular edema occurred. Therefore, the authors of the present study report an atypical case for management of paclitaxel maculopathy.
Case Report
A 54-year-old female patient with no previous medical history of ocular disease and who had been undergoing anti-cancer chemotherapy and radiotherapy for seven years after surgery for left breast cancer visited our clinic for visual disturbance of the right eye nine months after paclitaxel (Genexol-PM; Samyang Co., Seoul, Korea) administration as anti-cancer therapy. The patient had completed ten cycles of chemotherapy with paclitaxel 300 mg/m2 every three or four weeks.
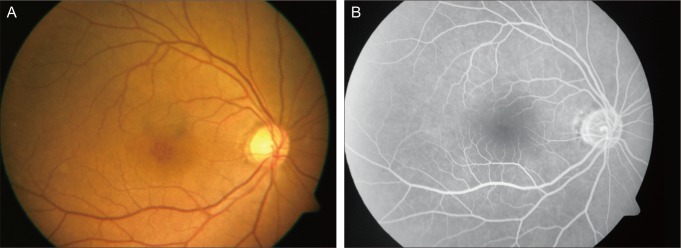
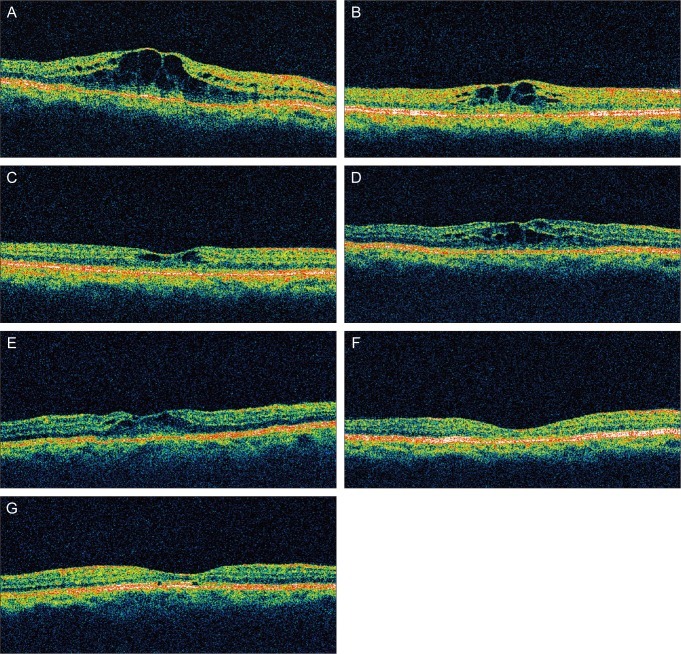
The best-corrected visual acuity (BCVA) was 0.5 in the right eye and 1.0 in the left eye, and intraocular pressure was within normal range in both eyes. Macular edema was detected in the right eye on fundus examination (Fig. 1A). Subsequently, optical coherence tomography (Stratus OCT; Carl Zeiss Meditec, Dublin, CA, USA) and fluorescein angiography were conducted. No particular finding was observed on fluorescein angiography (Fig. 1B); however, cystoid macular edema was found on optical coherence tomography (Fig. 2A), likely attributable to the paclitaxel administration. Thus, replacing paclitaxel with another anti-cancer agent was recommended. However, continuous paclitaxel administration during the treatment of macular edema was required by the Department of Breast Surgery as paclitaxel is a very effective anti-cancer agent. Therefore, replacement with another agent was not recommended. Planned anti-cancer therapy with paclitaxel was temporally withdrawn for one month, but a good outcome was not obtained. Subsequently, methazolamide (mezomin; BCWorld Pharm Co., Seoul, Korea) 150 mg was administered to treat the cystoid macular edema during discontinuation of paclitaxel. After a nine-day administration of methazolamide 150 mg, a significantly positive outcome was obtained regarding the cystoid macular edema in the right eye based on optical coherence tomography, and visual acuity in the right eye BCVA was slightly improved to 0.6 (Fig. 2B). Due to the improvement of macular edema, anti-cancer therapy with paclitaxel was resumed. Methazolamide 150 mg was orally administered every day for two weeks starting from seven days before anti-cancer agent administration. Two weeks after paclitaxel re-administration, BCVA was improved to 0.8, and cystoid macular edema was also improved (Fig. 2C). Subsequently, paclitaxel 300 mg/m2 was additionally administered once every month for a total of 13 times, and methazolamide 150 mg was administered every day for two weeks starting seven days before anti-cancer therapy initiation and continuing to seven days after the completion of anti-cancer therapy. During the period of anti-cancer agent administration, cystoid macular edema in the right eye did not progress as shown in the first visit, whereas a new cystoid macular edema occurred in the left eye after 20 cycles of paclitaxel chemotherapy, and the left eye BCVA decreased to 0.9 (Fig. 2D and 2E). After another anti-cancer agent was administered due to cutaneous metastasis from the breast cancer, no cystoid macular edema was observed on optical coherence tomography (Fig. 2F and 2G); BCVA of the right and left eyes were 0.6 and 0.8, respectively.
Fig. 1.
Fundus angiographic image of the right eye. (A) Marked central cystic change of the macula. (B) No fluorescein leakage on the macula.
Fig. 2.
Optical coherence tomographic images of both eyes. (A) Thick cystoid macular edema in the right eye before methazolamide treatment. (B) Improved cystoid macular edema in the right eye after methazolamide treatment for nine days. (C) Greatly improved cystoid macular edema in the right eye after methazolamide treatment for 23 days. (D) Slightly aggravated cystoid macular edema in the right eye after paclitaxel with methazolamide treatment. (E) Newly developed cystoid macular edema in the left eye during paclitaxel chemotherapy. (F) Complete resolution of the cystoid macular edema in the right eye after discontinuation of paclitaxel chemotherapy. (G) Complete resolution of the cystoid macular edema in the left eye after discontinuation of paclitaxel chemotherapy.
Discussion
Cystoid macular edema is a common cause of vision loss. In particular, juvenile X-linked retinoschsis, Goldmann-Favre syndrome, and niacin toxicity have been known to be causes of cystoid macular edema that shows no leakage on fluorescein angiography [2,3]. Until now, the mechanism of cystoid macular edema that shows no fluorescein leakage has not been identified and is thought to occur due to selective damage of the blood ocular barrier from molecules with a weight less than that of fluorescein. To treat this type of macular edema that shows no leakage on fluorescein angiography, the oral administration of acetazolamide has been known to be effective in chronic macular edema treatment, particularly in the treatment of concurrent macular edema in patients with chronic iridocyclitis and retinitis pigmentosa [4-6].
Joshi and Garretson [1] reported simultaneous paclitaxel maculopathy in both eyes, claiming the occurrence was due to intracellular fluid accumulation and the slight leakage of extracellular fluid caused by toxicity to Muller cells. In addition, Telander and Sarraf [7] reported simultaneous docetaxel-induced cystoid macular edema in both eyes as the outcome of fluid retention syndrome caused by docetaxel. They suggested that passage of fluid increases in the capillary due to fluid retention syndrome, which causes edema and protein leakage of the capillary, and cystoid macular edema occurs due to selective damage of the blood ocular barrier from molecules with a weight less than that of fluorescein or to slow fluid movement that cannot be detected on fluorescein angiography.
In the present case, retinal findings such as retinal traction of the vitreous body and underlying diseases that may cause cystoid macular edema were not observed. Furthermore, considering the disappearance of cystoid macular edema after discontinuation of paclitaxel, cystoid macular edema occurrence was likely caused by paclitaxel. Because there was no indication of systemic fluid retention, cystoid macular edema was presumed to occur as a result of cellular toxicity derived from the suppression of intracellular microtubule reorganization.
Unlike the two previously mentioned cases, in the present case study, cystoid macular edema initially occurred in one eye and later in both eyes. Cystoid macular edema was induced in the right eye by paclitaxel after 11 treatment cycles, whereas cystoids macular edema in the left eye was induced by paclitaxel at 20 cycles. This result suggests that maculopathy caused by drugs including paclitaxel initially may occur in one eye, but eventually occurs in both eyes with long-term administration. In addition, drug discontinuation is known to be the best treatment for cystoid macular edema caused by drugs such as paclitaxel. However, in cases with a potential risk of cancer metastasis due to drug discontinuation or change, as shown in the present case study, oral maintenance therapy with methazolamide could be alternatively applied. Oral maintenance therapy with methazolamide is not likely to assure the complete prevention of cystoid macular edema as a new cystoid macular edema occurred in the left eye during the administration of oral maintenance therapy with methazolamide in the present case. Therefore, systemic chemotherapy with paclitaxel can cause unilateral cystoid macular edema in short-term treatment. However, long-term treatment with paclitaxel can also cause bilateral cystoid macular edema. Although oral maintenance therapy with methazolamide cannot completely prevent cystoid macular edema, it may help to prevent progression of cystoid macular edema and severe vision loss.
Several studies have reported that cystoid macular edema in patients with retinitis pigmentosa was effectively treated with carbonic anhydrase inhibitor eye drops with less complications than oral agents [8,9]. In the cases of uneasy oral administration of a carbonic anhydrase inhibitor or increased risk of complications, carbonic anhydrase inhibitor eye drops could be used to treat cystoid macular edema. Further studies on the use of carbonic anhydrase inhibitors in eye drops are necessary.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Joshi MM, Garretson BR. Paclitaxel maculopathy. Arch Ophthalmol. 2007;125:709–710. doi: 10.1001/archopht.125.5.709. [DOI] [PubMed] [Google Scholar]
- 2.Semb KA, Aamdal S, Oian P. Capillary protein leak syndrome appears to explain fluid retention in cancer patients who receive docetaxel treatment. J Clin Oncol. 1998;16:3426–3432. doi: 10.1200/JCO.1998.16.10.3426. [DOI] [PubMed] [Google Scholar]
- 3.Spirn MJ, Warren FA, Guyer DR, et al. Optical coherence tomography findings in nicotinic acid maculopathy. Am J Ophthalmol. 2003;135:913–914. doi: 10.1016/s0002-9394(02)02296-1. [DOI] [PubMed] [Google Scholar]
- 4.Farber MD, Lam S, Tessler HH, et al. Reduction of macular oedema by acetazolamide in patients with chronic iridocyclitis: a randomised prospective crossover study. Br J Ophthalmol. 1994;78:4–7. doi: 10.1136/bjo.78.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fishman GA, Gilbert LD, Anderson RJ, et al. Effect of methazolamide on chronic macular edema in patients with retinitis pigmentosa. Ophthalmology. 1994;101:687–693. doi: 10.1016/s0161-6420(94)31277-2. [DOI] [PubMed] [Google Scholar]
- 6.Miyake Y, Awaya S, Takahashi H, et al. Hyperbaric oxygen and acetazolamide improve visual acuity in patients with cystoid macular edema by different mechanisms. Arch Ophthalmol. 1993;111:1605–1606. doi: 10.1001/archopht.1993.01090120027008. [DOI] [PubMed] [Google Scholar]
- 7.Telander DG, Sarraf D. Cystoid macular edema with docetaxel chemotherapy and the fluid retention syndrome. Semin Ophthalmol. 2007;22:151–153. doi: 10.1080/08820530701457373. [DOI] [PubMed] [Google Scholar]
- 8.Fishman GA, Apushkin MA. Continued use of dorzolamide for the treatment of cystoid macular oedema in patients with retinitis pigmentosa. Br J Ophthalmol. 2007;91:743–745. doi: 10.1136/bjo.2006.107466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grover S, Apushkin MA, Fishman GA. Topical dorzolamide for the treatment of cystoid macular edema in patients with retinitis pigmentosa. Am J Ophthalmol. 2006;141:850–858. doi: 10.1016/j.ajo.2005.12.030. [DOI] [PubMed] [Google Scholar]