Abstract
Background
Extranodal natural killer (NK)/T-cell lymphoma is a subtype of lymphoma that is derived from NK cells. It is considered as an aggressive form of non-Hodgkin's lymphoma because of frequent relapses and resistance to treatment. Relapsed NK/T-cell lymphoma often follows a fulminant course that is refractory to conventional chemotherapy treatment.
Methods
Several patients with extranodal NK/T-cell lymphoma showed long-term survival in spite of frequent relapses. Thus, the medical records of patients diagnosed with extranodal NK/T-cell lymphoma from 1995 to 2007 were reviewed and assessed.
Results
Of the 140 cases reviewed, 6 were selected (4.29%). Each of these patients had a minimum of 3 relapses or disease progression during the follow-up period, and their median overall survival was 66 months (range, 42-89 months). They were grouped according to the atypical clinical behavior observed: (1) repeated relapses or progression (≥3 times) during follow-up; and (2) long-term survival of more than 40 months, as the longest overall survival median was previously considered at approximately 40 months. The clinicopathological and laboratory characteristics of these patients were similar to those of other extranodal NK/T-cell lymphoma patients. However, 5 of the studied cases involved relatively lower expression of the proliferation-related antigen Ki-67 (<40-50%), indicating less proliferative activity. Clinically, they showed delayed relapse for at least 20 months after the initial complete remission.
Conclusion
Our observations suggest that the clinical behavior of some extranodal NK/T-cell lymphoma patients differs from the typical clinical course.
Keywords: Extranodal NK/T-cell lymphoma, Relapse, Survival, Indolent
INTRODUCTION
Extranodal natural killer (NK)/T-cell lymphoma is a subtype of the lymphoma that is derived from NK cells. It is considered as an aggressive form of non-Hodgkin's lymphoma (NHL) [1]. Approximately half of the patients generally relapse during follow-up, and relapsed NK/T-cell lymphoma patients often follow a fulminant course that is refractory to the conventional chemotherapy treatment. This accounts for an early sharp drop in the overall survival curves of extranodal NK/T-cell lymphoma patients [2-5]. A recent nationwide survey in Korea reported a 5-year overall survival of 49.5%, and most of the long-term survivors had rarely relapsed during their follow-up period [4].
However, not all extranodal NK/T-cell lymphoma patients follow a similar aggressive clinical course and rapidly relapse after remission. A recent case series has reported the clinical features of patients with relapses as late as 10-29 years after their initial remission [6]. In addition, another study designated self-limited NK-cell proliferation in the stomach, which was previously diagnosed as extranodal NK/T-cell lymphoma, as lymphomatoid gastropathy [7]. This accumulated evidence in support of disease entities that differ from the typical extranodal NK/T-cell lymphoma cases suggests that NK/T-cell lymphoma could be categorized as indolent. Therefore, we reviewed cases of extranodal NK/T-cell lymphoma patients demonstrating long-term survival as well as repeated remissions and relapses. In this study, we present cases of patients with long-term survival despite repeated relapses.
MATERIALS AND METHODS
Case records of all patients diagnosed with nasal extranodal NK/T-cell lymphoma, from 1995 to 2007, at the Samsung Medical Center and Korea University Medical Center were consecutively reviewed. Extranodal NK/T-cell lymphoma, nasal type, was diagnosed according to the World Health Organization classification system. Therefore, patients were diagnosed based on the presence of a tumor mass with histological features and immunophenotypes compatible with the NK/T-cell lymphoma (cCD3+, CD20-, CD56+, cytotoxic molecules+, and EBV [Epstein-Barr virus] in situ hybridization +). Other NHL subtypes, including myeloid/NK cell precursor acute leukemia, blastic NK cell lymphoma/precursor NK cell lymphoblastic leukemia, aggressive NK cell leukemia, and peripheral T-cell lymphoma unspecified were excluded. The selection criteria for cases with an atypical clinical course was repeated relapses (≥3 times) or progression during follow-up, in addition to a longer than 40-month survival, as the longest overall survival median was previously considered at approximately 40 months [2,4]. All relapses were proven by biopsy, and they demonstrated histological similarity to the original disease. Patient treatment at the time of diagnosis and relapse was performed at the attending physician's discretion. Thus, systemic chemotherapy and/or involved field radiation therapy were performed as primary treatment at diagnosis. The primary chemotherapy regimen used was CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) or a CHOP-like regimen. The median total radiation dose to the lesion was 40 Gy, and the daily dose for most patients was 2 Gy. After relapse, various salvage chemotherapy regimens were used including SMILE (solumedrol, methotrexate, ifosfamide, L-asparaginase, and etoposide), IMVP-16 (ifosfamide, methotrexate, etoposide, and prednisone), and GDP (gemcitabine, dexamethasone, and cisplatin).
RESULTS
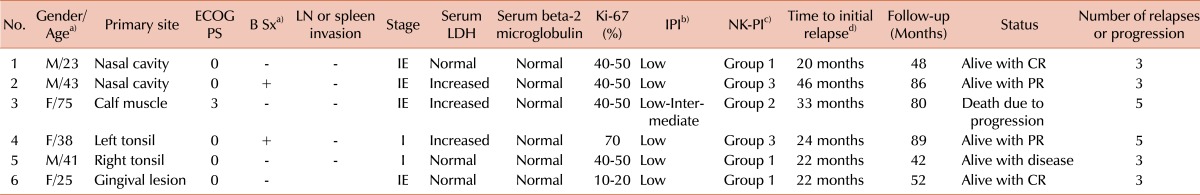
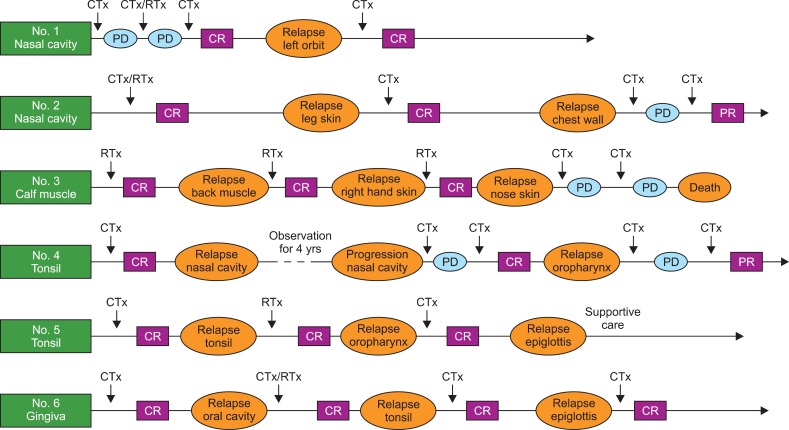
Patient characteristics at the time of diagnosis are summarized in Table 1. All patients presented with localized disease; hence, their International Prognostic Index (IPI) scores were low. The median time to initial relapse was 24 months (20-46 follow-up (Fig. 1). Patient 1 was a 23-year-old man with a mass obstructing the nasal cavity. The nasal mass progressed during chemotherapy and radiation therapy. A new orbital lesion developed 18 months after achieving complete remission (CR) through salvage chemotherapy. However, the patient was alive at the time of the study after the second complete remission (CR2) (Fig. 1). In patient 2 (a 43-year-old man), the leg skin tumor relapsed 46 months after the initial CR (Fig. 1). The patient achieved CR after salvage chemotherapy. However, he refused further treatment such as high-dose chemotherapy with autologous stem cell transplantation that was required to consolidate remission. Three years after CR2, relapse was detected in the chest wall. However, the patient was alive at the time of the study with partial remission, and his survival duration was 86 months (Table 1). Patient 3 was a 75-year-old woman presenting with a left calf muscle mass. She underwent radiation therapy because of her poor performance status, and she achieved CR. However, since her initial relapse in the back muscle, she showed repeated relapses that followed a wandering pattern from back muscle to nasal skin (Fig. 1). The time interval between diagnosis and initial relapse was 33 months. The patient died of disease progression after having survived for 80 months, despite 5 relapses. These 3 patients showed a wandering relapse pattern from nasal cavity to muscle and a long-term survival, in spite of frequent relapses. Cases 4-6 involved patients who had primary lesions of the oral cavity. Their initial relapse, 22-24 months after their initial CR, was followed by 3 other relapses. However, the relapse lesions were confined to the head and neck region, such as the oral and nasal cavities. Interestingly, patient 4, a 38-year-old woman, was alive with stable disease after the initial nasal cavity relapse. During that period, she had not been receiving any treatment (Fig. 1). Patient 5 (41-year-old man) was alive, with the disease, after his third relapse, despite refusing further treatment (Fig. 1). Patient 6 showed 3 relapses in the oral cavity during the 52-month follow-up period, and she was alive at the time of the study with no evidence of relapse. All patient samples were EBV-positive, although the positivity rate varied among the samples. The immunohistochemistry findings of the biopsy specimens collected at the time of diagnosis showed that Ki-67 expression level was less than 50% in 5 of the 6 patients. This indicated a relatively low tumor cell proliferation rate. The re-biopsy samples collected at relapse showed a similar Ki-67 expression pattern. Patient 4's Ki-67 expression level was especially low at relapse (<20%), which was much lower than that observed at diagnosis.
Table 1.
Summary of patients.
a)Age at diagnosis. b)International prognostic index: Age, Performance, Extranodal involvement, Ann Arbor stage, serum LDH (Lactate dehydrogenase). Low: 0 or 1 risk factors, Low-Intermediate: 2 risk factors. c)NK-Prognostic index [4]: Presence of "B" symptoms, Ann Arbor stage ≥III, serum LDH >1×upper normal limit, and regional lymph node (N1-3, not M1). Group 1: none; Group 2: 1 risk factors; Group 3: 2 risk factors; Group 4: 3 or 4 risk factors. d)Time interval between the initial complete remission and the initial relapse.
Abbreviations: No, number; ECOG, Eastern Cooperative Oncology Group; PS, performance status; Sx, symptoms; LN, lymph node.
Fig. 1.
Patient clinical course. Abbreviations: CTx, chemotherapy; RTx, radiation therapy; CR, complete remission; PR, partial remission; PD, progression of disease.
DISCUSSION
These 6 patients have shown at least 3 relapses or progression during their follow-up period, and have an overall survival median of 66 months (range, 42-89 months). This long-term survival is significantly higher than the previously reported extranodal NK/T-cell lymphoma overall survival median, which ranged from 19.6 months to less than 50 months [2-4, 8]. However, the clinical and laboratory characteristics of these patients themselves do not distinguish them from other extranodal NK/T-cell lymphomas patients (Table 1). All patients were categorized as low or low-intermediate risk because of low international prognostic index scores, which is similar to other extranodal NK/T-cell lymphoma patients. We then constructed an NK-prognostic index. Accordingly, 3 patients were categorized as group 1 (no risk), and the other 3 patients had 2 or 3 risk factors (Table 1) [4].
We reviewed the pathology of these patients in search of possible pathological observations that could explain the atypical clinical courses followed by these patients. However, their morphology and immunohistochemistry characteristics were similar to that of other NK/T-cell lymphoma patients, except for the relatively lower Ki-67 expression levels (<40-50%) observed in all patients, except in patient 4. These Ki-67 expression levels may indicate lower proliferative activity than that in aggressive cases, and they are consistent with a recent report on the prognostic power of Ki-67 expression [9]. Therefore, these patients were grouped according to the atypical clinical behavior observed: (1) repeated relapses or progression (≥3 times) during their follow-up and (2) long-term survival for more than 40 months.
Clinically, the relapse characteristics of these patients can be detailed as described. First, 2 different relapse patterns were observed. Patients 1, 2, and 3 showed a wandering relapse pattern from nasal cavity to muscle. However, in patients 4, 5, and 6, the primary site of involvement and relapse lesions were confined to the head and neck region, such as oral and nasal cavities. The impact of these different relapse patterns on clinical outcomes such as survival, as well as the biological and pathological differences between these patterns is unclear. Further studies are needed to clarify these points.
Second, although the time interval between CR and initial relapse varied from 20 to 46 months, all patients showed a progression-free period of at least 20 months This is a relatively delayed relapse compared to relapses that commonly lead to a fatal clinical course. Relapsed extranodal NK/T-cell lymphomas are usually characterized by a rapid relapse or progression, during or immediately after treatment. They are also often followed by a fulminant aggressive course that results in resistance to treatment and death. Thus, delayed relapse as observed in these patients may influence the evaluation results of overall prognosis in extranodal NK/T-cell lymphoma. Previously, some delayed relapses similar to those observed in our patients have been reported. The longest delayed relapse case was observed in a sinonasal tract NK/T-cell lymphoma patient with a 12-year relapse after initial CR [10]. A longer than 5-year relapse, after initial CR, was also reported in the retrospective analysis [2].
The reasons behind the delayed relapse and indolent clinical course that allow long-term survival, despite repeated relapses, are unknown. However, one possible explanation is the presence of minimal residual lymphoma cells in a dormant state. NK/T-cell lymphoma usually runs an aggressive clinical course. Nevertheless, the relatively lower Ki-67 expression level (<40-50%) reported in most of our patients suggests the presence of lymphoma cells with biological characteristics similar to that of indolent lymphoma. This may explain the atypical clinical course observed in our patients, and It is supported by the fact that patients 4 and 5 lived with the disease for longer than 2 years without treatment (Fig. 1). Another possible hypothesis is the occurrence of a second NK/T-cell lymphoma. It has been reported that the Asian population is particularly affected by chronic active EBV infection [11]. EBV-infected NK cells may evolve from a polyclonal to a monoclonal state, eventually leading to the development of overt NK-cell lymphoma. Thus, clonal evolution of residual EBV-infected NK-cells may result in a second NK/T-cell lymphoma, after initial lymphoma eradication. However, tumor specimens were unavailable for examination in order to confirm clonality. The clinicopathological features of NK/T-cell lymphoma patients with late relapses, some as late as 10-29 years after initial remission, were recently reported [6]. These cases may support the possibility of second NK/T-cell lymphoma developing from premalignant EBV-infected NK cells. However, it has been reported that some patients also followed an aggressive clinical course after relapse, contradicting with the indolent clinical course observed in our cases after relapse. Thus, not all patients follow an indolent clinical course after late relapse, which hints at the possibility of selection bias.
Thus far, the proportion of patients showing this atypical clinical course among the total extranodal NK/T-cell lymphoma patient population is unclear. The patients selected in this study represented 4.29% of the 140 patients who were reviewed (90 patients from Samsung Medical Center; 50 from Korea University Medical Center). Therefore, a small group of patients (less than 5%) may follow this atypical clinical course. In conclusion, our experience suggests that some patients show a clinical behavior that diverges from the typical extranodal NK/T-cell lymphoma clinical course. Therefore, patients with indolent clinical courses, similar to the patients in this study, can be found among aggressive non-Hodgkin's lymphoma patients. Additional studies should be performed to evaluate the incidence and biological characteristics of such extranodal NK/T-cell lymphoma patients who follow an atypical clinical course.
References
- 1.Kim GE, Cho JH, Yang WI, et al. Angiocentric lymphoma of the head and neck: patterns of systemic failure after radiation treatment. J Clin Oncol. 2000;18:54–63. doi: 10.1200/JCO.2000.18.1.54. [DOI] [PubMed] [Google Scholar]
- 2.Chim CS, Ma SY, Au WY, et al. Primary nasal natural killer cell lymphoma: long-term treatment outcome and relationship with the International Prognostic Index. Blood. 2004;103:216–221. doi: 10.1182/blood-2003-05-1401. [DOI] [PubMed] [Google Scholar]
- 3.Kim BS, Kim TY, Kim CW, et al. Therapeutic outcome of extranodal NK/T-cell lymphoma initially treated with chemotherapy result of chemotherapy in NK/T-cell lymphoma. Acta Oncol. 2003;42:779–783. doi: 10.1080/02841860310010682. [DOI] [PubMed] [Google Scholar]
- 4.Lee J, Suh C, Park YH, et al. Extranodal natural killer T-cell lymphoma, nasal-type: a prognostic model from a retrospective multicenter study. J Clin Oncol. 2006;24:612–618. doi: 10.1200/JCO.2005.04.1384. [DOI] [PubMed] [Google Scholar]
- 5.Ng SB, Lai KW, Murugaya S, et al. Nasal-type extranodal natural killer/T-cell lymphomas: a clinicopathologic and genotypic study of 42 cases in Singapore. Mod Pathol. 2004;17:1097–1107. doi: 10.1038/modpathol.3800157. [DOI] [PubMed] [Google Scholar]
- 6.Au WY, Kim SJ, Yiu HH, et al. Clinicopathological features and outcome of late relapses of natural killer cell lymphomas 10-29 years after initial remission. Am J Hematol. 2010;85:362–363. doi: 10.1002/ajh.21663. [DOI] [PubMed] [Google Scholar]
- 7.Takeuchi K, Yokoyama M, Ishizawa S, et al. Lymphomatoid gastropathy: a distinct clinicopathologic entity of self-limited pseudomalignant NK-cell proliferation. Blood. 2010;116:5631–5637. doi: 10.1182/blood-2010-06-290650. [DOI] [PubMed] [Google Scholar]
- 8.Kim SJ, Kim BS, Choi CW, et al. Treatment outcome of front-line systemic chemotherapy for localized extranodal NK/T cell lymphoma in nasal and upper aerodigestive tract. Leuk Lymphoma. 2006;47:1265–1273. doi: 10.1080/10428190600565651. [DOI] [PubMed] [Google Scholar]
- 9.Kim SJ, Kim BS, Choi CW, et al. Ki-67 expression is predictive of prognosis in patients with stage I/II extranodal NK/T-cell lymphoma, nasal type. Ann Oncol. 2007;18:1382–1387. doi: 10.1093/annonc/mdm183. [DOI] [PubMed] [Google Scholar]
- 10.Kren L, Depowski P, Wu A. Sinonasal (angiocentric) T/NK cell lymphoma: report of a case with a -12-year history free of recurrent/residual disease and a sudden deterioration. Cesk Patol. 2002;38:113–116. [PubMed] [Google Scholar]
- 11.Cohen JI, Kimura H, Nakamura S, Ko YH, Jaffe ES. Epstein-Barr virus-associated lymphoproliferative disease in non-immunocompromised hosts: a status report and summary of an international meeting, 8-9 September 2008. Ann Oncol. 2009;20:1472–1482. doi: 10.1093/annonc/mdp064. [DOI] [PMC free article] [PubMed] [Google Scholar]