Abstract
Objectives
This study was designed to develop a descriptive profile of parents and caregivers who bring their children to the emergency department for non-urgent issues as well as exploring the reasons for presenting to an urban hospital pediatric emergency department for non-urgent conditions. Such work is necessary in order to develop effective interventions.
Methods
A total of 106 parents/caregivers whose child was triaged with a non-emergent/urgent condition completed a 15–20 minute computerized survey (English and Spanish) in an urban pediatric emergency department.
Results
The majority of respondents described themselves as Latino (76%) and foreign-born (62%). About half (49%) reported having an annual income of less than $20,000 and 43% of respondents did not have health insurance for themselves. Almost all (95%) of the index children had a primary care physician and health insurance. In spite of being triaged as non-urgent, over half (63%) described their child’s condition as “very” or “extremely” urgent. About half of the respondents reported not receiving basic information on childhood illnesses from their child’s doctor. Reasons for non-urgent visits seemed to revolve around issues of convenience and perception of quality of care.
Conclusions
Interventions should focus on health literacy and ensure that parents are provided relevant and accurate education on pediatric illnesses and common safety concerns; by increasing parental education on pediatric health, parents may be better able to assess acuity of their child’s health issues.
Keywords: non-urgent ED use, health literacy, parent knowledge
INTRODUCTION
The emergency department (ED) continues to be a consistently utilized source of care for pediatric patients, often in spite of severity or acuity of the primary medical complaint. According to Berry et al., non-urgent cases comprise from 58% to 82% of pediatric ED (PED) visits and contribute to inefficiencies, overcrowding and adverse effects in an already taxed healthcare system.1 As long ED wait times persist, non-urgent ED visits have exacerbated problems related to overcrowding, such as adverse patient outcomes (morbidity/mortality), reduced quality of care (transport and treatment delays), impaired access (ambulance diversion and patient elopement), and provider losses, which result in resources being diverted from more acutely ill and injured patients.2,3 In addition, prolonged PED boarding time (defined as the cumulative number of hours all admitted patients spend waiting for an inpatient bed) and ED daily census are associated with barriers to access and quality, including increasing overall length of stay, time to triage, time to physician, and number of patient elopements.4
Our own research in an urban PED indicates that 58% of visits can be categorized as non-emergent and/or primary care treatable (Lu, Liu, Weiss, et al, in review). The present study is focused on exploring the reasons for presenting to an urban hospital PED for non-urgent conditions as well as creating a descriptive profile of parents and caregivers who bring their children to the ED for non-urgent issues. While a great deal of research has focused on the non-urgent use of the ED in the general population, research with pediatric populations is more limited. Pediatric patients are unique in that they rely on their parents or primary caregivers to serve as their “gatekeepers” to medical care. Thus, interventions designed for these populations must consider patient and primary caregiver characteristics. Such work is necessary to better understand the problem, develop the most effective interventions to reduce the problem and inform future research in this area.
Demographics
There are several factors associated with children and adolescents presenting to the ED with a non-urgent condition. Perhaps one of the most cited reasons is related to the types of insurance coverage and income levels. Publicly insured children and families with lower incomes are more likely to seek care in the ED setting, particularly for non-urgent reasons, and to overestimate medical urgency.5–11 In addition, when taking race and ethnicity into consideration, several studies report a positive correlation between minority status and non-urgent ED use among pediatric populations.5,6,12 Parental characteristics that are determinants include, having less than a high school education, utilizing the ED for their own care in the past, being the sole parent in the household, reporting higher stress levels, and a shorter length of stay in the United States are all shown to correlate with lower acuity ED use.5,6,8,13–15
Convenience and Referrals
Although the majority of patients presenting to the ED have a regular primary care physician (PCP), there are still many barriers encountered that discourage patients from accessing primary care. As obtaining care from a PCP in a timely manner proves to be increasingly difficult, the relatively immediate care provided in the ED poses a convenient alternative.1,16,17 A 2009 survey of physician appointment wait times in 15 metropolitan areas across the United States showed the average wait time for an appointment with a family practitioner was 20.3 days.18 The odds of presenting to the ED with a non-urgent complaint are doubled when difficulty obtaining care from a PCP with long wait times is perceived.19 Perceived convenience relating to hours of availability, location, and transportation also play an important role in influencing parents to bring their children to the ED for non-urgent reasons. Scheduling an appointment with the PCP during business hours can prove to be challenging for working parents who instead may find the 24-hour availability of the ED a more advantageous option as it can be accessed when the clinic is closed or if after-hours PCP appointments are unavailable.1,10,16,17 Furthermore, parental perceived difficulty in getting to the PCP office, reliance on public transportation, and living in close proximity to an ED or community health center also contribute to the convenience seen in utilizing the ED regardless of severity.5,20,21
In addition to these parental perceptions, referral to the ED by either the patient’s provider (e.g. PCP, nurse, after-hours provider, clinic staff) or insurance carrier often results in non-urgent ED visits. A survey of parents seeking non-urgent care in an ED conducted by Haltiwanger et al. show that a large proportion of these visits were referred by the PCP or clinic due to limited available appointments.17
Assessing Acuity
Assessing the severity of a child’s condition can prove to be both difficult and stressful in the face of illness or injury. Consequently, many non-urgent cases are perceived to be emergent enough to warrant a visit to the ED. Several studies examining the perceptions of parents and caregivers of non-urgent ED pediatric patients note their tendency to overestimate the acuity of the child’s condition.8,10,20 With respect to distinguishing between the ED and a PCP clinic visit, some respondents made no such distinction and instead saw both venues as equally appropriate sources of care for minor problems.16
PCP Experiences and Trust
In terms of quality of care, the ED is often believed to be superior considering the access to a greater amount of resources, such as laboratory tests and radiography.1 While many physician practices provide an on-call physician 24 hours a day for patients to contact as needed, some caregivers are unaware of this service or do not believe they can contact a PCP after hours.20
When comparing prior experiences with a PCP, negative experiences are associated with increased non-urgent ED utilization while positive experiences correlate with lower rates of non-urgent use. Negative experiences include problems with communication, general dissatisfaction with the PCP, deficiencies in preventive care, and being chastised for missed visits. Conversely, some positive experiences include high-quality timeliness of care, family centeredness, and realized access.12
Several studies also highlight how trust and perception influence the location and frequency of healthcare visits. Among the general population, minorities, particularly African Americans, are less likely to trust or have a positive perception of their physician when compared to non-Hispanic Whites.22–25 Furthermore, minorities who lacked physician continuity on repeat clinic visits or obtained medical care at facilities other than a physician’s office were more likely to report low trust.23,24
Interventions
As non-urgent ED utilization continues to contribute towards overcrowding, several programs have shown promise in reducing pediatric ED visits while simultaneously decreasing costs by avoiding expensive and unnecessary services in the ED. Some of these approaches included: utilizing standard social work practices to address problems affecting family functioning; providing extended primary care pediatric office hours, multiple access locations, and care coordination to Medicaid children; providing information about the importance of a primary care provider; and assistance with making an appointment with the provider of their choice. All of these methods resulted in a significant decrease in ED visits among participants who received the intervention.26–29
Given these issues, it is clear that there is no singular reason for why parents access EDs for non-urgent reasons. This study attempts to identify the most common reasons for presenting to an urban pediatric ED for non-urgent reasons. The common themes are discussed as well as recommendations for parent and provider education interventions.
MATERIALS AND METHODS
Setting
The setting for this study was Children’s Hospital Los Angeles (CHLA), a 286-bed, non-profit urban pediatric center that treats over 93,000 patients per year. CHLA is also a Level 1 Pediatric Trauma Center whose ED serves 65,000 patients a year. The ED is often overcrowded, with an average wait time of 99 minutes. The ED serves a multi-cultural population, with an average of 78% Latino, 8% African American, 5% Asian American, and 3% Whitea. Slightly less than half (48%) report English as their primary language spoken.
Participants and Sampling
Study respondents included 106 primary caregivers, defined as the parent and/or the legal guardian of the child that was brought to the ED. Inclusion criteria included being the primary caregiver of a child presenting to the ED, who was triaged as a semi-urgent or non-urgent (level 4 or 5 on a 5-point scale). All participants spoke either English or Spanish. The bilingual interview team worked in the ED over a two-week period for a total of 12 shifts, including 4 daytime, 4 evening and 4 weekend shifts. These different time periods were selected in order to ensure that data collection occurred during different times of day and days to capture a range of experiences and situations in the ED.
Targeted purposive sampling was used in that potential respondents whose children were triaged as semi-urgent or non-urgent were asked to participate in the computer-based survey. Interview staff approached potential respondents and explained the study and its purpose. Participants were assured that no identifying information would be collected from them and verbal consent was obtained. Caregivers who agreed to participate were taken to a private area of the ED (e.g., staff office, conference room, exam room) to complete the interview. Those who agreed to participate were provided a $20 cash incentive. This study received approval from the Institutional Review Board of Children’s Hospital Los Angeles.
Measures and Analysis
Participants completed a short (15–20 minutes) CASI (computer-assisted, self-interviewing) survey administered in either English or Spanish. The survey included the following sections and areas of inquiry.
Child Demographics
Participants were asked to report their child’s age, gender, race/ethnicity, health status (e.g., excellent, very good, good, fair, poor), insurance status, their child’s chief medical complaint and whether the child has a PCP.
Caregiver Demographics
Respondents were asked to report their age, race/ethnicity, household size, marital status, household income, education level, preferred language, immigration status, employment status, and insurance status.
ED Visit
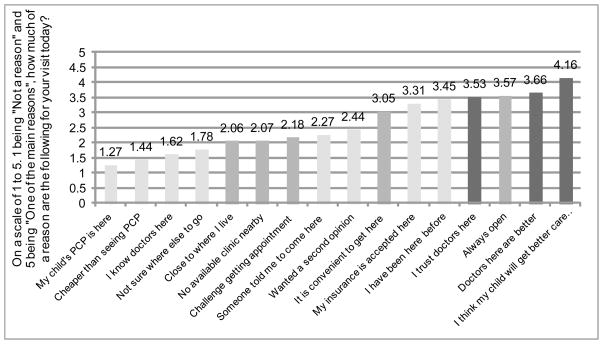
Participants were asked the following about the index ED visit: whether someone (e.g., doctor, staff, family member, friend/neighbor, insurance company) recommended they go to the ED and whether the child’s PCP was called prior to coming to the ED. Perceived urgency of the current visit was assessed by asking “Earlier you told me that you brought your child here due to ____. How urgent do you think this problem is for the child?” “Not at all urgent”, “A little urgent”, “Somewhat urgent” “Very urgent”, and “Extremely urgent”. Reasons for coming to the ED were assessed by asking “How much of a reason are the following for your visit to the CHLA emergency room today?” Sixteen potential reasons were provided and respondents were asked to rate each on a 5-point scale of “Not a reason”, “A little of the reason”, “Somewhat of a reason”, “A lot of the reason”, “One of the main reasons.” Respondents were also asked whether the child had seen another provider for the same issue in the last week, and their perceived urgency of the chief complaint.
PCP Education
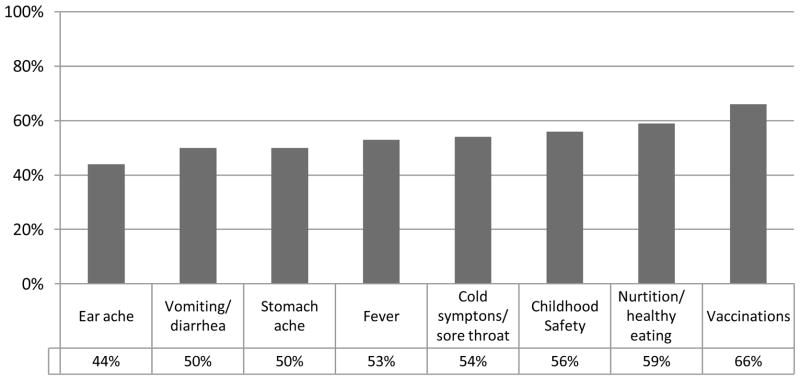
Participants were asked whether their child’s PCP provides them general child-health education as recommended by the American Academy of Pediatrics (AAP). These areas included: childhood safety, vaccinations and nutrition as well as general information on childhood fever, cold symptoms or sore throat, vomiting or diarrhea, stomach ache, and ear ache.
Perceived Access to Care
Caregivers were asked to assess their confidence in accessing health care. They were asked whether the child’s PCP speaks their preferred language and to what extent they understand the medical information provided by the PCP (e.g., not at all, a little, somewhat, completely). In addition, we assessed caregivers’ confidence in accessing care on a 5-point scale including: calling their child’s PCP for medical advice, making medical appointments for their child, asking doctors questions about their child’s health, and being able to talk with their health insurance company.
Statistical analyses were conducted using Stata 10. Because the current study is largely descriptive, results presented are based on univariate analyses of key variables of interest. Results from frequency analyses characterized key demographics (e.g., age, ethnicity, employment) of the study sample. The cross-tabulation procedure was then used to identify categorical distribution of key variables based on immigration status and racial/ethnic groups. Chi-square analyses were used to test whether some of these categorical variables were significantly different.
RESULTS
Table 1 presents the demographics of the primary caregiver. The majority (76%) identified as Latino/Hispanic, 10% as African American, 7% as White/Caucasian and 5% as Asian. Slightly over a third (36%) were single/never married, and about half (54%) were married or living with a domestic partner. About half (49%) reported an annual household income of less than $20,000 and an additional 23% reported making between $20,000 and $29,999. The average household size was 4.37 people. Forty-five percent of mothers had less than a high school education and an additional 30% were high school graduates. Forty-three percent of caregivers did not have medical insurance for themselves. Sixty-two percent were born outside the United States, with 5% of those reporting to be foreign-born living here five years or less. Slightly more than half (55%) identified English as their preferred language to receive health-related information with an additional 43% identifying Spanish. One-third reported visiting the ED for his/her own health in the past 12 months.
Table 1.
Caregiver Demographics (N=106)
| Characteristic | N (%) or Mean | |
|---|---|---|
| Gender | Female | 92 (87) |
| Male | 14 (13) | |
| Age | 18–25 | 33 (31) |
| 26–35 | 42 (40) | |
| 36–45 | 28 (26) | |
| 46–55 | 3 (3) | |
| Ethnicity | Asian/Asian American | 5 (5) |
| African American/Black | 11 (10) | |
| Caucasian/White | 7 (7) | |
| Hispanic/Latino | 81 (76) | |
| Other | 2 (2) | |
| Marital status | Single, never married | 38 (36) |
| Married/living with domestic partner | 57 (54) | |
| Separated or divorced | 10 (9) | |
| Widowed | 1 (1) | |
| Household Income | less than $20,000 | 52 (49) |
| $20,000 – $29,999 | 24 (23) | |
| $30,000 – $39,999 | 8 (8) | |
| $40,000 + | 10 (10) | |
| Prefer not to answer | 12 (11) | |
| Caregiver’s Education | Less than high school | 46 (49) |
| High school graduate | 29 (31) | |
| Some college and beyond | 19 (20) | |
| Insurance status | No insurance | 46 (43) |
| Insured | 60 (57) | |
| Private insurance only | 15 (14) | |
| Public insurance | 41 (39) | |
| Other | 4 (4) | |
| Transportation to ED | Personal or family car | 58 (55) |
| Received a ride/public transit | 48 (45) | |
| Foreign born | Yes | 62 (59) |
| Foreign born caregiver time in US | 3–5 years | 5 (5) |
| 6–10 years | 18 (11) | |
| more than 10 years | 39 (37) | |
| Employment | Part time or full time | 50 (48) |
| Not working, looking for work | 27 (26) | |
| Average household size | 4.37 | |
| Preferred language | English | 58 (55) |
| Spanish | 46 (43) | |
| Korean | 2 (2) | |
| ED visit, past 12 months | Yes | 35 (33) |
Table 2 presents demographic data on the patient/child brought to the ED. Half of the patients were two years old or younger and an additional 23% were between 3 and 5 years of age. The majority (75%) identified as Latino/Hispanic, 11% as African American, 6% as Caucasian/White and 5% as Asian. Twenty percent reported that their child had a chronic condition such as diabetes, cancer, asthma or autism, though based on the triage scoring system, such patients had a chief complaint unrelated to their underlying medical condition in order to have been triaged as semi-urgent or non-urgent. When asked to identify the primary reason for their visit, the most common response was fever (22%) followed by gastrointestinal issues (18%), ear/eye infections (11%) cold symptoms/sore throat (9%) and rashes (9%). About a third (31%) had seen another provider for the same issue in the last week. Most (95%) of the pediatric patients had some kind of medical insurance (of those, 80% reported public insurance coverage). Almost all (94%) reported that their child had a primary care provider.
Table 2.
Patient/Child Demographics
| Characteristic | N (%) | |
|---|---|---|
| Age | 0 – 2 years | 53 (50) |
| 3 – 5 years | 24 (23) | |
| 6 – 17 years | 29 (27) | |
| Ethnicity | Asian/Asian American | 3 (3) |
| African American/Black | 12 (11) | |
| Caucasian/White | 6 (6) | |
| Hispanic/Latino | 79 (75) | |
| Other | 5 (5) | |
| Chronic condition | Yes | 21 (20) |
| Chief complaint | Fever | 23 (22) |
| Cold symptoms/sore throat | 10 (9) | |
| Digestive system | 19 (18) | |
| Ear/eye infection | 12 (11) | |
| Headache | 2 (2) | |
| Trouble breathing | 6 (6) | |
| Rash | 10 (9) | |
| Accident/injury | 7 (7) | |
| Another reason | 17 (16) | |
| Saw other provider for same problem in past week | Yes | 32 (31) |
| Child health status | Poor | 3 (3) |
| Fair | 16 (15) | |
| Good | 21 (20) | |
| Very good | 29 (27) | |
| Excellent | 37 (35) | |
| Insurance Status | Insured | 101 (95) |
| Child has a PCP | Yes | 100 (94) |
Table 3 presents information related to the index ED visit. Interestingly, 63% of caregivers perceived the level of urgency to be “very” or “extremely” urgent with a smaller percentage (11%) perceiving the issue to be “not at all” or “a little” urgent. The descriptive data indicate that about 40% of caregivers called their child’s doctor prior to coming to the ED. When looking at ethnic/racial differences, foreign-born Latino caregivers were more likely to present to the ED without consulting a doctor or other advisor compared to U.S.-born respondents. (47% v. 79%). In general, less than half (43%) of caregivers reported that someone recommended they come to the ED. Among those with recommendations, the most common recommendation came from the child’s doctor or staff from the doctor’s office (54%) followed by a family member (31%) and friend/neighbor (16%).
Table 3.
ED Visit Information
| N (%) | ||
|---|---|---|
| Perceived visit urgency | Not at all urgent | 1 (1) |
| A little urgent | 10 (10) | |
| Somewhat urgent | 27 (26) | |
| Very urgent | 44 (43) | |
| Extremely urgent | 21 (20) | |
| Call doctor prior to ED visit | Yes | 42 (40) |
| Foreign-born (n=59) | 12 (21)* | |
| U.S. Born (n=47) | 21 (55)* | |
| Someone recommended you come to ED today? | Yes | 45 (43) |
| Who recommended ED visit (N=45) | My child’s regular doctor/provider | 21 (47) |
| Staff who answers calls at doctor’s office | 3 (7) | |
| A family member | 14 (31) | |
| A friend or neighbor | 7 (16) | |
| My health insurance company | 0 (0) | |
| Nurse advisory line | 2 (4) | |
| Someone else | 2 (4) |
Denominator is total number of foreign-born and U.S. born, respectively
Caregiver education
The American Academy of Pediatrics (AAP) and the American Academy of Family Physicians both provide guidelines on numerous pediatric patient topics. The survey asked caregivers what types of information they have received from their child’s primary care provider based on this list. As shown in Figure 1, about half of respondents reported receiving information, with the most common type reported being childhood immunizations (66%) and childhood nutrition/healthy eating (59%). The least common type reported included “what to do when your child has an earache” (44%), “what to do when your child has a stomach ache” (50%) and “what to do when your child has vomiting and/or diarrhea” (50%).
Figure 1.
Primary Care Provider Education Received
Access to care
Based on prior patient experiences in the ED, it was thought that a lack of confidence or knowledge on how to access care may be related to visits to the ED for non-urgent reasons. The survey results indicate that 64% of respondents felt “confident”, “very” or “extremely” confident in calling their child’s doctor for medical advice. In addition, most (82%) of the caregivers felt “confident”, “very” or “extremely” confident in their ability to make medical appointments for their child. Caregivers felt greater confidence in their ability to ask providers questions about their child’s health with 95% reporting feeling “confident”, “very” or “extremely” confident. Caregivers felt somewhat less confident in their ability to talk with someone from their health insurance plan about benefits or services with 70% feeling at least confident in this area.
Reasons for Visit
Respondents were asked to indicate on a 5-point scale how much of a reason sixteen potential motives for coming to the ED were. Data indicate that the primary reasons fall into two large categories: convenience and trust/confidence in the ED doctors. As Figure 2 presents, the most prevalent reasons for coming to the ED that day included: “I think my child will get better care here” (4.16), “Doctors here are better” (3.66), “Always open” (3.57), “I trust doctors here” (3.53), and “I have been here before” (3.45). Among the least common reasons were “My child’s primary care doctor is here” (1.27), “My insurance is accepted here” (1.44), “I know doctors here” (1.62), and “Not sure where else to go” (1.78).
Figure 2.
Reasons for Visiting the ED
CONCLUSION
The data presented here indicate that use of the ED for non-urgent medical conditions is a complex issue, without a single driving factor. While the issues are complex, they do require additional study to develop effective interventions that can minimize non-urgent use of the ED as ED utilization is costly and not the most effective means of providing primary care, managing chronic conditions or coordinating pediatric care.
The survey data provide a demographic profile of caregivers presenting to the ED for non-urgent cases. These indicate that this is a primarily Latino sample, with a majority born outside the United States and about half indicating a preference for Spanish as their language to receive health-related information. These demographic profiles are similar to what others have reported.1,5–12 In addition, this is a low income group with low health insurance rates among caregivers. The pediatric patients in this study are primarily under the age of five. Almost all of them have both health insurance and a primary care provider. The most common reasons for their visits included flu-like symptoms (e.g., fever, digestive, sore throat).
When examining data about the index non-urgent visits, what emerged is the limited ability of caregivers to accurately judge the urgency of the presenting condition. A surprising 63% of the caregivers assessed their child’s current condition (which was triaged as among the lowest acuity) as very or extremely urgent. This indicates there may be a lack of basic education around childhood illnesses and how to best treat common conditions such as fever, vomiting, diarrhea or cold symptoms. This is reflected in the percentages of caregivers who reported receiving basic medical information (e.g., what to do when your child has a fever, cold, ear ache) from their child’s doctor where, in general, about half of the respondents reported receiving this type of information. While these were not extraordinarily low percentages of parents reporting a lack of education, given that these are basic anticipatory guidelines from the AAP, it is worth noting that about half of the primary care doctors are not providing this kind of education during well child visits (or parents do not recall receiving this information). If the latter, this may be an indication that the format in which material is presented is not the most effective format. Regardless, these are important areas for further investigation. It should also be noted that the majority of respondents felt very confident in their ability to ask providers questions about their child’s health and also indicated they understood the information provide to them about their child’s health.
In addition, the survey found that less than half of the caregivers called their child’s doctor prior to coming to the ED. This is in spite of the fact that the majority of the respondents felt confident in their ability to call their child’s doctor and make appointments for them. The data also indicate that when calling their doctors’ offices, many reported that the doctors or staff from the office recommended that they come to the ED for the current condition. There are a number of possible reasons for this, including a lack of available appointments at the primary care clinic and misunderstandings about the severity of the condition on the part of the staff or parent describing the issues. The data also indicate that foreign-born respondents were more likely to present to the ED without calling their child’s doctor or asking for others’ opinions. Similarly, Zandieh and colleagues found that non-urgent use of the ED was more likely among the general Hispanic respondents in their study in New York30. While our study is more specific to foreign-born respondents, this may indicate a cultural norm in that the typical way to access care in their home country was to simply present to the ED.
Finally, the survey data indicate that caregivers generally feel confident in their abilities to access care for their children. In addition, almost all of the pediatric patients included in this study had a primary care doctor. Thus, the question remains why do parents come to the ED for non-urgent conditions? Part of the answer may lie in the limited child health education provided to parents. Another part of that answer may be related to the convenience of the ED, with regards to hours and location, as well as caregivers’ trust and confidence in medical providers. When asked to identify the reasons for coming to the our PED, among the most common were those related to confidence and quality of care. Caregivers seemed to believe that their child would receive a higher quality of care in our PED. While caregivers did not indicate that that they have developed a close relationship or rapport with the our ED physicians (as evidenced by the low score of “I know the doctors here” on the reasons for visit scale) simply having been to the ED before, and perhaps having a positive experience, seemed to be one of the driving reasons for the current visit.
When reviewing these results, it is interesting to note that caregivers appear to feel that they will receive higher quality care at our PED than at their child’s PCP. Others have noted this issue of trust in other studies, with some noting that minority groups, particularly Latinos, are less likely to trust their PCP.22–24 However, this is an area of concern given the fractured nature of ED services, which generally lacks continuity of care. Prior research has noted that the inability of the ED to provide continuity of care has created challenges in that children with the lowest continuity of care are the most likely to have visited the ED and to be hospitalized when compared with children with medium and high continuity of care.31 Clearly the ED is neither designed to provide preventive care nor to serve as a source for referral; this is the responsibility of the PCP. Interventions with PCPs may be of primary import given recent research that indicates PCPs did not perceive the non-urgent use of the ED as a significant enough problem to warrant change in physician-care practices or parent care-seeking behavior.32
In addition to quality of care, convenience and access also seem to be related to coming to the ED for non-urgent visits. This is similar to findings from others.1,16,17 Issues that may impact convenience include inability to get timely appointments, access to medical services 24-hours a day and transportation to clinics.
Finally, the caregivers in our sample in general over-estimated the urgency of the ED visit, with the majority assessing their child’s condition as urgent. Again, this is similar to what others have noted in that parents tend to overestimate the acuity of their child’s condition.8,10,20 This tendency could be addressed through the development of interventions that ensure parents are provided accurate anticipatory guidelines for their child’s health. This information needs to be provided in a culturally appropriate and understandable manner, keeping the health literacy of caregivers and patients in mind.
Given the current healthcare and economic situations, it is not practical to consider interventions which require clinics to extend their hours or to increase staffing to accommodate additional patients, without increasing Medi-Cal reimbursements or other financial incentives. Researchers and others must consider more economically sound interventions that can address the myriad of structural barriers (e.g., insurance coverage, limited community clinics, cultural competency, payment structures) that impact access to care.
A recent study completed by the Agency for Healthcare Research and Quality (AHRQ) found that low health literacy is linked to poorer health status and a higher risk of death.33 This report also found an association between low health literacy in all adults and more frequent use of hospital emergency rooms and inpatient care. More than 75 million English-speaking adults in the United States have limited health literacy, defined as the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions. Thus, lower health literacy makes it difficult for parents, the “gatekeepers” to their child’s health, to make decisions about their own and their children’s healthcare. Thus, interventions addressing health literacy may have an effect not only on non-urgent ED visits, but also preventive care and understanding medical labels and instructions.
Given the health disparities in low income and minority groups, addressing access to care and other structural barriers that contribute to these health disparities may be key to improving the patient experience. For example, a successful recent intervention with Head Start included training parents on the use of a low-literacy health book to respond to common childhood illnesses in order to decrease ED visits for common childhood illness symptoms.34 The intervention was found to have a statistically significant impact on improving parental care for common acute illnesses in children as the average number of emergency room visits decreased 58% among study participants.
There are a number of limitations to this study. First, the findings rely on respondents’ self-reported behaviors, which cannot be independently verified. In addition, we only recruited caregivers who presented to the ED whose children’s conditions were triaged to be non-urgent, thus comparisons to demographics, perceptions and behaviors to those presenting to the ED with more urgent conditions cannot be made. Also, this study relied on a convenience sample and a relatively small number of participants. Thus, generalizations cannot be made to the larger population. Given these limitations, we cannot ascertain correlations within the data as presented. This may limit our ability to recommend the implementation of interventions given our inability to ascertain causality. In addition, while the use of CASI surveys may minimize potential interviewer bias, it should be noted that respondents’ tendency to rate quality of the doctors and care received at the index PED higher than other providers, may be related to interviewer bias. Finally, we did not interview community providers. Given that respondents indicated they felt they would receive higher quality of care at the ED, it would be recommended that the perspectives of community providers also be included in this analysis to understand the challenges and obstacles they face in providing medical care.
However, in spite of these limitations, we believe that these data help to provide a snapshot of the perceptions and behaviors of caregivers presenting to the ED for non-urgent reasons. There are some conflicting findings in this study, specifically related to caregivers’ perceived confidence in being able to navigate the often very complex healthcare system. In general, parents feel confident in their abilities to make appointments, question their providers and understand the information provided. However, only 40% of the caregivers in this sample called their PCP prior to presenting to the ED. There appears to be a disconnection in the connectivity between perceived confidence and action. A better understanding of this is needed before effective interventions can be developed and implemented with providers.
The data collections methods presented here limit the ability to identify how and what interventions might be most effective in addressing the non-urgent use of the PED. However, given the descriptive data presented here and prior research that has identified similar issues and patterns, it can be inferred that interventions that address issues such as low health literacy and its related issues such as navigation of the health care system, knowledge of common childhood illnesses and communication with healthcare professionals, may have a positive impact on this misuse of the PED.
The data do indicate that only about half of the caregivers recall receiving information on basic child health from their child’s PCP, contrary to the AAP recommendations. Providers and clinic administrators should consider different approaches to ensure that this information is provided to parents, perhaps through videos while waiting for an appointment, web-based applications or easy to understand written materials that can be efficiently provided in the clinic environment, and that parents are encouraged to ask questions about the materials presented to them.
In order to improve caregivers’ ability to access timely and quality preventive care for their children, we should consider how relatively low cost interventions such as the Head Start training program can be implemented in clinics and other healthcare institutions. The Centers for Disease Control and Prevention created the National Action Plan to Improve Health Literacy. Healthcare providers should be encouraged to adopt this Plan at the practice-level to ensure the provision of meaningful patient care and education.
Table 4.
Perceived Access to Care and Ability to Navigate Healthcare System
| N (%)* | ||
|---|---|---|
| Confidence in calling PCP for medical advice (N=96) | Not at all confident | 15 (16) |
| Slightly confident | 20 (21) | |
| Confident | 23 (24) | |
| Very confident | 19 (20) | |
| Extremely confident | 19 (20) | |
| Confidence in being able to make medical appointments for child (N=102) | Not at all confident | 12 (12) |
| Slightly confident | 5 (5) | |
| Confident | 28 (27) | |
| Very confident | 23 (22) | |
| Extremely confident | 34 (33) | |
| Confidence in asking doctors or providers questions about the child’s health and condition (N=100) | Not at all confident | 3 (3) |
| Slightly confident | 2 (2) | |
| Confident | 12 (14) | |
| Very confident | 32 (31) | |
| Extremely confident | 51 (50) | |
| Confident in being able to talk with someone from your health insurance about benefits and services (N=97) | Not at all confident | 12 (12) |
| Slightly confident | 16 (16) | |
| Confident | 18 (18) | |
| Very confident | 21 (21) | |
| Extremely confident | 30 (31) | |
| Child’s PCP speaks preferred language (N=97) | Yes | 90 (93) |
| No | 7 (7) | |
| Understand medical information PCP gives about child’s health (N=97) | Not at all | 2 (2) |
| A little | 6 (6) | |
| Somewhat | 12 (12) | |
| Completely | 77 79) |
Percentages may not add up to 100% due to rounding
Acknowledgments
This project was supported through the Los Angeles Clinical and Translational Science Institute Pilot Awards Grant # (M01-RR000043).
Footnotes
Based on CHLA administrative data from 2006-2009
References
- 1.Berry A, Brousseau D, Brotanek JM, Tomany-Korman S, Flores G. Why do parents bring children to the emergency department for nonurgent conditions? A qualitative study. Ambulatory Pediatrics. 2008;8:360–367. doi: 10.1016/j.ambp.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 2.Hoot NR, Aronsky D. Systematic review of emergency department crowding: Causes, effects and solutions. Annals of Emergency Medicine. 2008;52(2):126–136. doi: 10.1016/j.annemergmed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simon H, Hirsh D, Rogers A, Massey R, DeGuaman M. Pediatric Emergency Department Overcrowding: Electronic Medical Record For Identification Of Frequent, Lower Acuity Visitors. Can We Effectively Identify Patients For Enhanced Resource Utilization? Journal of Emergency Medicine. 2009;36(3):311–316. doi: 10.1016/j.jemermed.2007.10.090. [DOI] [PubMed] [Google Scholar]
- 4.Timm N, Ho M, Luria J. Pediatric Emergency Department Overcrowding and Impact on Patient Flow Outcomes. Acad Emerg Med. 2008 Sep;15(9):832–837. doi: 10.1111/j.1553-2712.2008.00224.x. [DOI] [PubMed] [Google Scholar]
- 5.Halfon N, Newacheck PW, Wood DL, St Peter RF. Routine emergency department use for sick care by children in the United States. Pediatrics. 1996;98:28–34. [PubMed] [Google Scholar]
- 6.Huang CJ, Poirier MP, Cantwell JR, Ermis PR, Isaacman DJ. Prudent layperson definition of an emergent pediatric medical condition. Clinical Pediatrics. 2006;45:149–155. doi: 10.1177/000992280604500206. [DOI] [PubMed] [Google Scholar]
- 7.Luo X, Liu G, Frush K, Hey LA. Children’s health insurance status and emergency department utilization in the United States. Pediatrics. 2003;112:314–319. doi: 10.1542/peds.112.2.314. [DOI] [PubMed] [Google Scholar]
- 8.Phelps K, Taylor C, Kimmel S, Nagel R, Klein W, Puczynski S. Factors associated with emergency department utilization for nonurgent pediatric problems. Archives of Family Medicine. 2000;9:1086–1092. doi: 10.1001/archfami.9.10.1086. [DOI] [PubMed] [Google Scholar]
- 9.Piehl MD, Clemens CJ, Joines JD. Decreasing emergency department use by children enrolled in the Medicaid program by improving access to primary care. Archives of Pediatrics & Adolescent Medicine. 2000;154:791–795. doi: 10.1001/archpedi.154.8.791. [DOI] [PubMed] [Google Scholar]
- 10.Soliday E, Hoeksel R. Factors related to paediatric patients’ emergency department utilization. Psychology, Health & Medicine. 2001;6(1):5–12. [Google Scholar]
- 11.Suruda A, Burns T, Knight S, Dean J. Health insurance, neighborhood income, and emergency department usage by Utah children 1996–1998. BMC Health Services Research. 2005 Apr;5(29) doi: 10.1186/1472-6963-5-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brousseau DC, Gorelick MH, Hoffmann RG, Flores G, Nattinger AB. Primary care quality and subsequent emergency department utilization for children in Wisconsin medicaid. Academic Pediatrics. 2009;9(1):33–39. doi: 10.1016/j.acap.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 13.Mistry RD, Hoffmann RG, Yauck JS, Brousseau DC. Association between parental and childhood emergency department utilization. Pediatrics. 2005;115:147–151. doi: 10.1542/peds.2004-1798. [DOI] [PubMed] [Google Scholar]
- 14.Raphael JL, Zhang Y, Liu H, Giardino AP. Parenting stress in US families: implications for paediatric healthcare utilization. Child: care, health and development. 2009;36(2):216–224. doi: 10.1111/j.1365-2214.2009.01052.x. [DOI] [PubMed] [Google Scholar]
- 15.Weathers AC, Novak SP, Sastry N, Norton EC. Parental nativity is an important factor associated with where children usually go for health care. Maternal and Child Health Journal. 2008;12:499–508. doi: 10.1007/s10995-007-0278-0. [DOI] [PubMed] [Google Scholar]
- 16.Goepp J, Chin N, Massad J, Edwards L. Pediatric Emergency Department Outreach: Solving Medical Problems or Revealing Community Solutions? Journal of Health Care for the Poor and Underserved. 2004 Nov;15(4):522–529. doi: 10.1353/hpu.2004.0060. [DOI] [PubMed] [Google Scholar]
- 17.Haltiwanger KA, Pines JM, Martin ML. The pediatric emergency department: A substitute for primary care? Western Journal of Emergency Medicine. 2006;7(2):26–30. [PMC free article] [PubMed] [Google Scholar]
- 18.Merritt Hawkins & Associates. 2009 Survey of Physician Appointment Wait Times. Irving, TX: Merritt Hawkins & ASsociates; 2009. [Google Scholar]
- 19.Brousseau DC, Bergholte J, Gorelick MH. The Effect of Prior Interactions With a Primary Care Provider on Nonurgent Pediatric Emergency Department Use. Arch Pediatr Adolesc Med. 2004 Jan 1;158(1):78–82. doi: 10.1001/archpedi.158.1.78. [DOI] [PubMed] [Google Scholar]
- 20.Doobinin K, Heidt-Davis P, Gross T, Isaacman D. Nonurgent pediatric emergency department visits: Care-seeking behavior and parental knowledge of insurance. Pediatric Emergency Care. 2003 Feb;19(1):10–14. doi: 10.1097/00006565-200302000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Ludwick A, Fu R, Warden C, Lowe RA. Distances to emergency department and to primary care provider’s office affect emergency department use in children. Academic Emergency Medicine. 2009;16:411–417. doi: 10.1111/j.1553-2712.2009.00395.x. [DOI] [PubMed] [Google Scholar]
- 22.Boulware L, Cooper L, Ratner L, LaVeist T, Powe N. Race and Trust in the Health Care System. Public Health Reports. 2003 Jul-Aug;118:358–365. doi: 10.1016/S0033-3549(04)50262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Doescher M, Saver B, Franks P, Fiscella K. Racial and Ethnic Disparities in Perceptions of Physician Style and Trust. Arch Fam Med. 2000 Nov-Dec;9:1156–1163. doi: 10.1001/archfami.9.10.1156. [DOI] [PubMed] [Google Scholar]
- 24.Halbert C, Armstrong K, Gandy O, Shaker L. Racial Differences in Trust in Health Care Providers. Arch Intern Med. 2006 Apr;166:896–901. doi: 10.1001/archinte.166.8.896. [DOI] [PubMed] [Google Scholar]
- 25.Rajakumar K, Thomas S, Musa D, Almario D, Garza M. Racial Differences in Parents’ Distrust of Medicine and Research. Arch Pediatr Adolesc Med. 2009 Feb;163(2):108–114. doi: 10.1001/archpediatrics.2008.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grossman LK, Rich LN, Johnson C. Decreasing nonurgent emergency department utilization by Medicaid children. Pediatrics. 1998;102:20–24. doi: 10.1542/peds.102.1.20. [DOI] [PubMed] [Google Scholar]
- 27.Herman AD, Mayer GG. Reducing the use of emergency medical resources among Head Start families: A pilot study. Journal of Community Health. 2004;29(3):197–208. doi: 10.1023/b:johe.0000022026.20770.f4. [DOI] [PubMed] [Google Scholar]
- 28.Ross J, Roberts D, Campbell J, Solomon K, Brouhard B. Effects of Social Work Intervention on Nonemergent Pediatric Emergency Department Utilization. Health & Social Work. 2004 Nov;29(4):263–273. doi: 10.1093/hsw/29.4.263. [DOI] [PubMed] [Google Scholar]
- 29.Wang C, Villar M, Mulligan D, Hansen T. Cost and Utilization Analysis of a Pediatric Emergency Department Diversion Project. Pediatrics. 2005 Nov;116(5):1075–1079. doi: 10.1542/peds.2004-2093. [DOI] [PubMed] [Google Scholar]
- 30.Zandieh SO, Gershel JC, Briggs WM, Mancuso CA, Kuder JM. Revisiting Predictors of Parental Health Care-Seeking Behaviors for Nonurgent Conditions at One Inner-City Hospital. Pediatric Emergency Care. 2009;25(4):238–243. doi: 10.1097/pec.0b013e31819e350e. 210.1097/PEC.1090b1013e31819e31350e. [DOI] [PubMed] [Google Scholar]
- 31.Christakis D, Mell L, Koepsell T, Zimmerman F, Connell F. Association of Lower Continuity of Care With Greater Risk of Emergency Department Use and Hospitalization in Children. Pediatrics. 2001 Mar;103(3):524–529. doi: 10.1542/peds.107.3.524. [DOI] [PubMed] [Google Scholar]
- 32.Brousseau DC, Nimmer MR, Yunk NL, Nattinger AB, Greer A. Nonurgent emergency-department care: Analysis of parent and primary physician persepctives. Pediatrics. 2011;127(2):e375–e381. doi: 10.1542/peds.2010-1723. [DOI] [PubMed] [Google Scholar]
- 33.DeWalt D, Callahan L, Hawk V, et al. Health Literacy Universal Precautions Toolkit. Vol. 2010 Rockville, MD: Agency for Healthcare Research and Quality; Apr, 2010. [Google Scholar]
- 34.Herman A, Jackson P. Empowering Low-Income Parents with Skills to Reduce Excess Pediatric Emergency Room and Clinic Visits through a Tailored Low Literacy Training Intervention. Journal of Health Communication. 2010;15:895–910. doi: 10.1080/10810730.2010.522228. [DOI] [PubMed] [Google Scholar]