Abstract
Bronchopulmonary sequestration represents a spectrum of abnormalities. One of these abnormalities is an aberrant systemic arterial supply to a normal lung with no bronchial sequestration. These lesions were originally classified by Pryce as type 1. Most of these patients are asymptomatic but with time, many patients develop localized pulmonary hypertension, hemoptysis, and eventually high output cardiac failure. Multidetector computed tomography (MDCT) plays an important role in the diagnosis and planning of definitive treatment by identifying the origin and course of the aberrant artery. Definitive treatment can be surgical (lobectomy or segmentectomy) or endovascular.
Keywords: Sequestration, Pryce type 1, Hemoptysis
Introduction
Bronchopulmonary sequestration includes a spectrum of abnormalities. While the defining parameter is the presence of systemic arterial supply to a segment of lung parenchyma, the condition is often suspected based on the pulmonary parenchymal involvement noted on radiographs. Pryce type 1 sequestration, a less common variety, is characterized by systemic arterial supply to a normal lung with no bronchial sequestration and, hence, distinct in that the diagnosis is not suggested by a radiographic pattern. Thus, this condition should be considered as a differential diagnosis of hemoptysis. CT pulmonary angiography (CTPA) provides a noninvasive technique of diagnosis. Early radiological diagnosis is crucial as these patients are amenable to cure both by endovascular and minimally invasive surgical procedures.
Case Reports
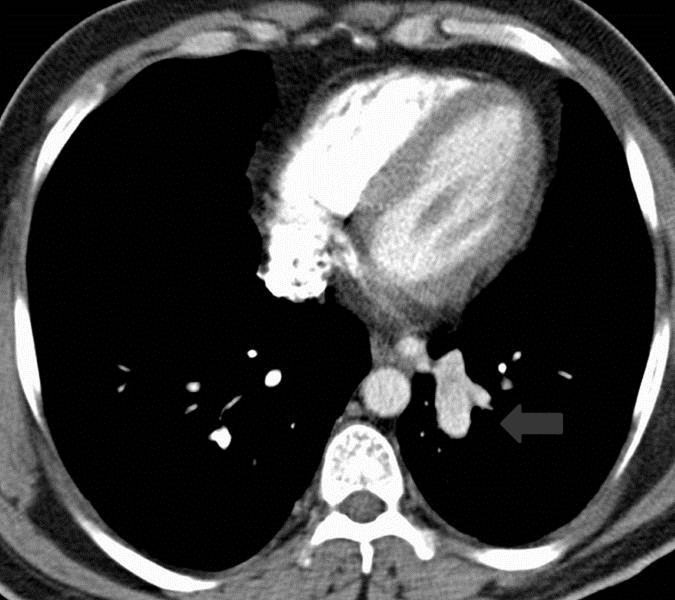
Case 1: A 41-year-old nonsmoker male was referred to the radiology department for CT with complaints of moderate hemoptysis for the past two years. The patient had no previous history of tuberculosis or recurrent chest infections. Bronchoscopy was unrevealing. A scout image from CT, (Fig. 1a), showed ill-defined left retrocardiac opacity. CT pulmonary angiography (CTPA) revealed an aberrant artery arising from the thoracic aorta and entering the left basal segments at the level of inferior pulmonary veins, (Figs. 1b-1d). The pulmonary parenchyma of this segment was normal. There were pulmonary arterial branches supplying this area. Subsequently, digital subtraction angiography (DSA) was undertaken which revealed an aberrant artery arising from the lower part of the thoracic aorta on the left side and entering the left basal lung segments and venous drainage into the left atrium, (Fig. 1e). Video-assisted thoracic surgical (VATS) ligation of the vessel was done.
Figure 1a.
A scout image from of the chest CT shows ill-defined retrocardiac opacity (arrow). This retrocardiac opacity correlates with the aberrant artery as shown in Fig. 1d.
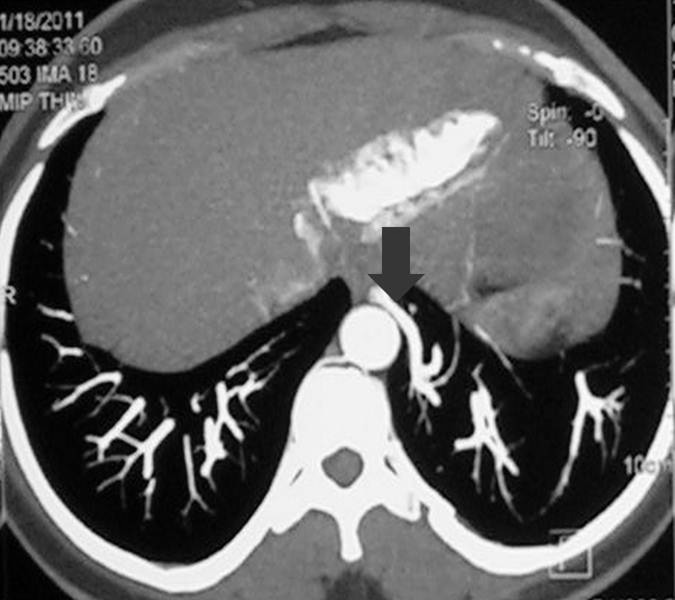
Figure 1b.
An axial CT section from CTPA in mediastinal window settings at the level of inferior pulmonary veins shows a nipple like structure (arrow) with enhancement similar to that of descending thoracic aorta at the mediastinal edge of the left basal lung segments, which on subsequent figures is shown to be an aberrant artery arising from the descending thoracic aorta. This pattern of origin of the aberrant artery from descending thoracic aorta and supply to the basal segment of left lower lobe represents the most common pattern.
Figure 1d.
Coronal reformatted MIP image from CTPA shows that the basal segments of the left lung receive their arterial supply from descending thoracic aorta via an aberrant artery (arrow).
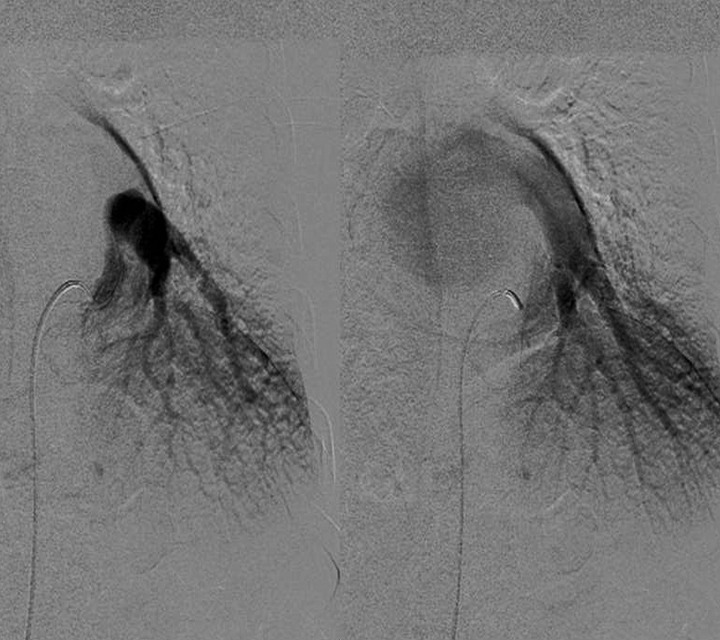
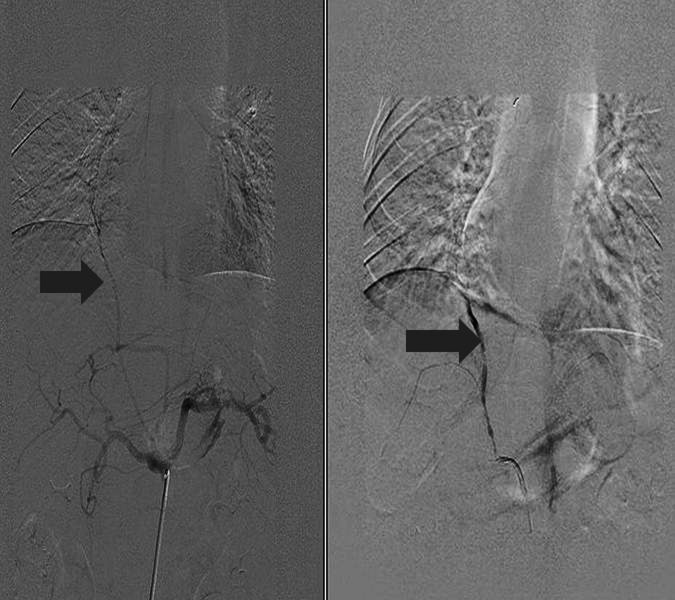
Figure 1e.
DSA images in arterial and venous phases confirm the origin of the aberrant artery, in addition to the normal pulmonary arterial supply, to the left lower lobe from the lower descending thoracic aorta and venous drainage into the left atrium via inferior pulmonary vein. This figure again highlights the most common pattern of origin of the aberrant artery and the venous drainage of the sequestrated segment. Patient subsequently underwent surgery.
A 41-year-old nonsmoker male presented with complaints of moderate hemoptysis for the past two years. The patient had no previous history of tuberculosis or recurrent chest infections. (Figs. 1a-1e)
Figure 1c.
The corresponding axial section in lung window setting shows normal lung parenchyma.
Case 2: A 27-year-old female presented to the medicine outpatient department with recurrent mild to moderate hemoptysis for 2 months. She denied any history of recurrent chest infections and there was no history of pulmonary tuberculosis. Chest radiograph was normal. The patient had a previous CECT chest which was interpreted as normal. CT angiography was undertaken. The CT images, (Figs. 2a-2c), revealed an aberrant artery arising from the abdominal aorta supplying the right middle lobe which was not showing any other abnormality. Pre-embolization and post-embolization DSA images revealed the origin of the aberrant artery from celiac axis. Glue embolization of the anomalous vessel was done, (Fig. 2d) and patient was cured of her symptoms.
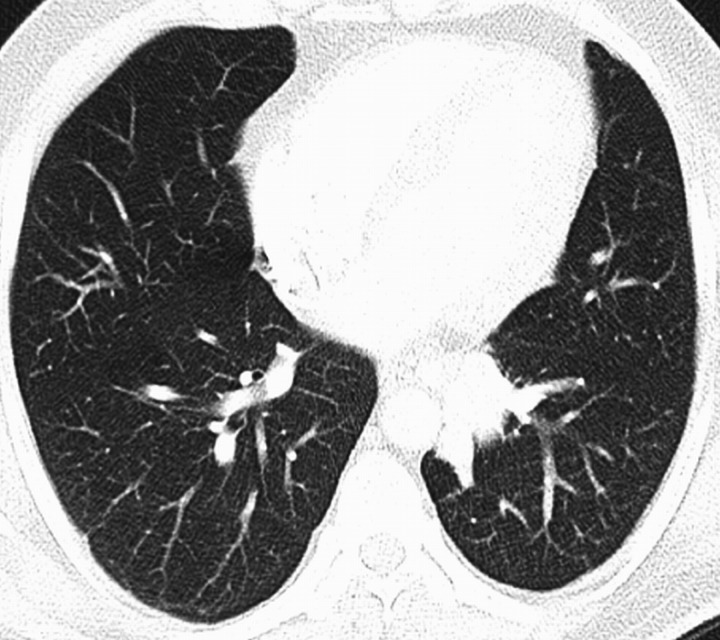
Figures 2a & 2b.
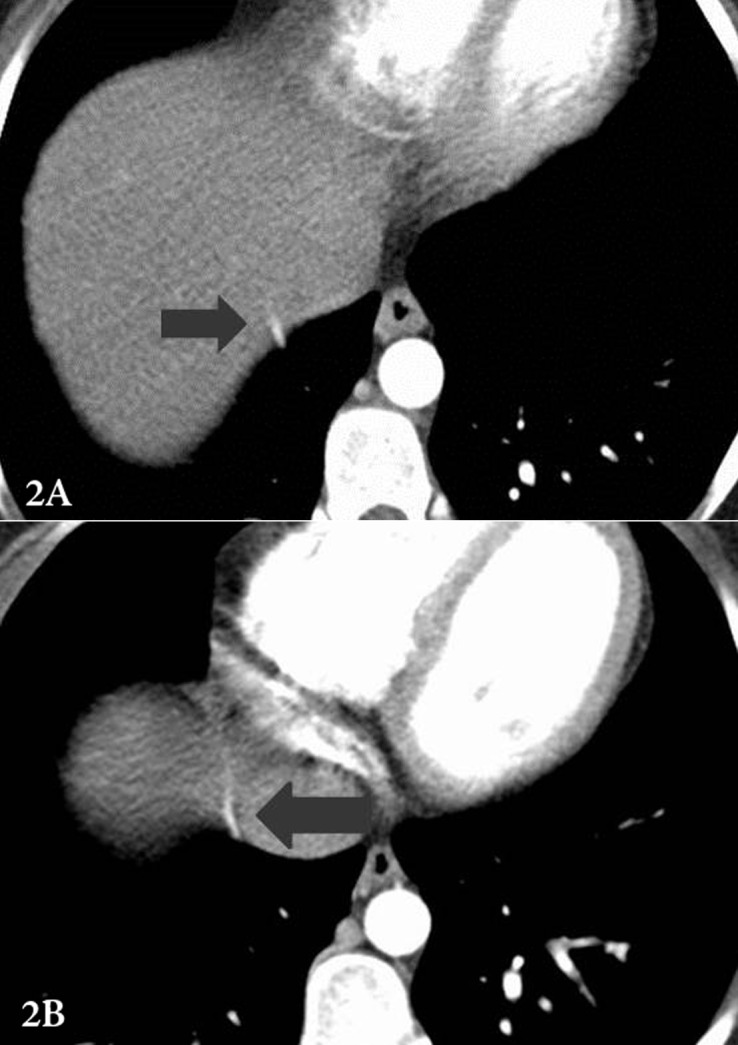
Serial axial CT sections in mediastinal window setting show an aberrant vessel coursing along the diaphragm upwards suggesting an infra-diaphragmatic origin (arrow). However the exact origin of this vessel and lung segment which it supplies is not apparent on these two axial sections; this is well demonstrated on the DSA images shown subsequently.
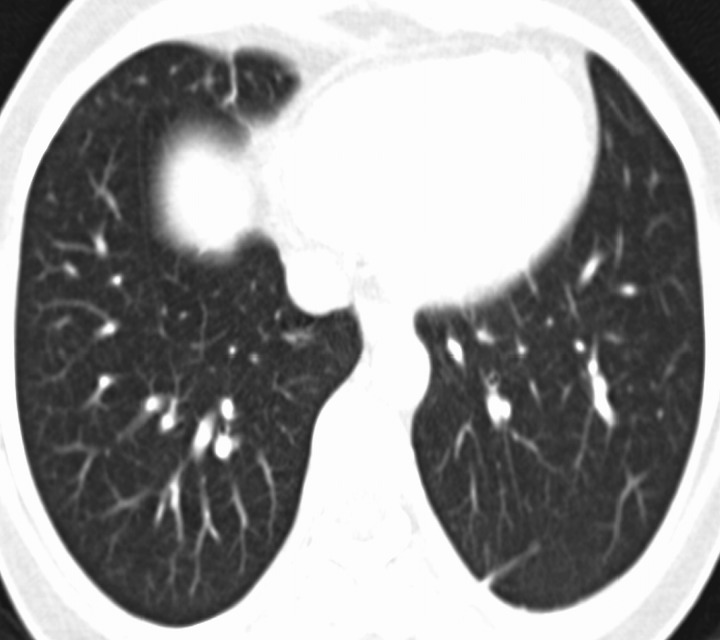
Figure 2c.
An axial CT section in lung window setting shows no significant pulmonary parenchymal abnormality.
Figure 2d.
Pre-embolization and post-embolization DSA images.
A 27-year-old female presented with recurrent mild to moderate hemoptysis for 2 months. There was no history of recurrent chest infections or pulmonary tuberculosis. Chest radiograph was normal. (Figs. 2a & 2b)
Selective celiac artery angiogram shows the origin of the aberrant artery from the celiac axis (arrow). This vessel traverses a long course to supply the middle lobe of the right lung. This combination of aberrant origin from the celiac axis and supply to the right middle lobe is extremely rare. In addition, there was pulmonary arterial supply (not shown). The post-embolization angiogram reveals the occlusion of aberrant channel (arrow).
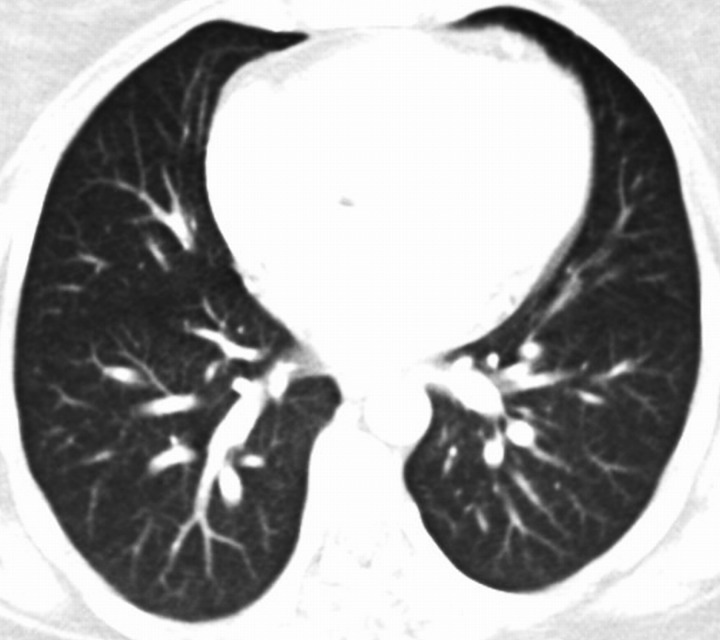
Case 3: A 32-year-old female was referred to us for a CTPA for complaints of intermitent mild-to-moderate hemoptysis for the past 6 years, otherwise, she was well. There was no history of past tuberculosis and patient did not suffer bleeding from any other site. She was thoroughly investigated to exclude other causes of hemoptysis. Chest radiograph showed no significant abnormality. Bronchoscopy was normal. CT maximal intensity projection (MIP) image, (Fig. 3a) showed an aberrant artery arising from the descending thoracic aorta supplying the posterior basal segment of the left lung. The lung parenchyma showed paucity of vessels in the left basal lung segments, (Fig. 3b). Endovascular intervention (embolization) was planned but as the hemoptysis was intermitent, patient refused treatment.
Figure 3a.
An axial MIP image from CTPA reveals an aberrant artery arising from the lower part of the descending thoracic aorta and coursing towards the posterior basal segment of the left lower lobe with paucity of pulmonary vessels in this lung segment (arrow).
Figure 3b.
The corresponding lung window axial section image demonstrates paucity of vessels in the basal segments of the left lower lobe. Apart from this, the lung parenchyma is normal.
A 32-year-old female was referred to us for a CTPA of the chest for complaints of intermitent mild to moderate hemoptysis for past 6 years. Other than this symptom, patient was well. There was no significant past history. She was widely investigated but no cause of hemoptysis could be detected. Chest radiograph showed no significant abnormality. Bronchoscopy was normal. (Figs. 3a & 3b)
Discussion
Systemic arterial supply to a lung with normal bronchial communication (without bronchial sequestration) and without cardiovascular or pulmonary abnormalities is a rare congenital abnormality.1 It is of two types: isolated systemic arterial supply to normal lung (ISSNL) and systemic arterial supply associated with normal pulmonary artery (dual supply).2 It is included in the "sequestration spectrum" as originally proposed by Sade et al.3 According to the original classification of pulmonary sequestration by Pryce et al,1 this abnormality is classified as Pryce type 1. In type 2, the systemic artery supplies both normal and abnormal lung, having no communication with the tracheobronchial tree. In type 3, only noncommunicating abnormal lung receives the aberrant systemic artery.
The embryogenesis of this condition is believed to be due to failure of regression of the primitive aortic branches to the developing lung bud.4 During normal lung development, the primary lung bud receives a vascular plexus from the dorsal aorta which regresses with the development of the main pulmonary artery. The hemodynamics of the involved lung segment is adversely affected by transmission of systemic pressure to the low pressure pulmonary vasculature. Focal pulmonary hypertension develops with a potential for development of high-output cardiac failure.
The basal segments of left lower lobe are the most commonly affected site,5,6 (cases 1 and 3), although rarely other sites can be affected (case 2 in whom right middle lobe was affected). The systemic artery most commonly arises from the thoracic aorta,7 (case 1), but can arise from abdominal aorta or celiac axis (cases 2 and 3) and even more rarely from left subclavian and internal mammary artery. These vessels usually enter the lung at the level of pulmonary hilum or at the level of inferior pulmonary ligaments. The venous drainage is normal and accomplished by inferior pulmonary vein draining into the left atrium.
Most patients are asymptomatic.8 The most common symptom is hemoptysis. This is related to the higher pressure of systemic circulation compared to pulmonary circulation. Other manifestations include exertional dyspnea, murmur in the lower chest and congestive heart failure due to left heart overload. Chest radiographs show ill-defined retrocardiac opacity corresponding to the anomalous artery. CT angiography can demonstrate the origin and course of aberrant artery with the advantage of multiplanar and 3-D reconstructions. Conventional angiography has been superseded by CT angiography with the advent of multidetector CT (MDCT) but remains an important problem solving tool and plays a vital role in the endovascular management of these patients. Treatment options include surgery (lobectomy and segmentectomy), when aberrant systemic artery is the only supply, and occlusion of the aberrant vessel by surgical ligation or endovascular treatment (embolization), when the involved segment has dual blood supply.2
Conclusion
Early diagnosis of anomalous systemic artery to a normal lung is based on a high degree of suspicion in a patient with otherwise non-explained hemoptysis. CT angiography provides an excellent non-invasive modality for establishing the diagnosis. The condition can be treated by endovascular techniques, VATS or surgery.
Acknowledgements
The authors reported no conflict of interest and no funding was received for this work.
References
- 1.Pryce DM. Lower accessory pulmonary artery with intralobar sequestration of lung; a report of seven cases. J Pathol Bacteriol 1946. Jul;58(3):457-467 10.1002/path.1700580316 [DOI] [PubMed] [Google Scholar]
- 2.Irodi A, Cherian R, Keshava SN, James P. Dual arterial supply to normal lung: within the sequestration spectrum. Br J Radiol 2010. May;83(989):e86-e89 10.1259/bjr/30458107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sade RM, Clouse M, Ellis FH., Jr The spectrum of pulmonary sequestration. Ann Thorac Surg 1974. Dec;18(6):644-658 10.1016/S0003-4975(10)64417-7 [DOI] [PubMed] [Google Scholar]
- 4.Ellis K. Fleischner lecture. Developmental abnormalities in the systemic blood supply to the lungs. AJR Am J Roentgenol 1991. Apr;156(4):669-679 [DOI] [PubMed] [Google Scholar]
- 5.Kurosaki Y, Kurosaki A, Irimoto M, Kuramoto K, Itai Y. Systemic arterial supply to normal basal segments of left lower lobe: CT findings. J Comput Assist Tomogr 1993. Nov-Dec;17(6):857-861 10.1097/00004728-199311000-00004 [DOI] [PubMed] [Google Scholar]
- 6.Miyake H, Hori Y, Takeoka H, Takuma M, Kawagoe T, Mori H. Systemic arterial supply to normal basal segments of the left lung: characteristic features on chest radiography and CT. AJR Am J Roentgenol 1998. Aug;171(2):387-392 [DOI] [PubMed] [Google Scholar]
- 7.Campbell DC, Jr, Murney JA, Dominy DE. Systemic arterial blood supply to a normal lung. JAMA 1962. Oct;182:497-499 10.1001/jama.1962.03050430171028b [DOI] [PubMed] [Google Scholar]
- 8.Miller EJ, Singh SP, Cerfolio RJ, Schmidt F, Eltoum IE. Pryce’s type I pulmonary intralobar sequestration presenting with massive hemoptysis. Ann Diagn Pathol 2001. Apr;5(2):91-95 10.1053/adpa.2001.23026 [DOI] [PubMed] [Google Scholar]