Abstract
Background
Hypercholesterolemia (HC) is a major risk factor in the development of coronary heart disease (CHD). Serum cholesterol is directly related to complications and mortalities associated with heart diseases. There are a few studies that describe HC among youths in the Arab Gulf countries. We sought to evaluate HC among young healthy university students to assess their risk of developing CHD.
Methods
Lipid profile of 166 students between the ages of 16-30 years (Mean: 20.49±2.96) were examined and blood glucose, total protein, albumin, thyroid stimulating hormone (TSH) and the inflammation marker high sensitivity CRP (hsCRP) were determined. Each volunteer filled a questionnaire about her/his lifestyle and personal and family medical histories and height and weight were measured to determine body mass index (BMI). The data were analyzed using SPSS version 17. Chi-Square was used to determine the relation between categorical variables. A p-value <0.05 was considered statistically significant.
Results
According to the American Heart Association criteria, 44 (26.5%) students were identified with primary hypercholesterolemia (PHC) in the first testing round. After proper health counseling, the same tests were repeated after 2-3 weeks in all 44 hypercholesterolemic students. We found only 26 (15.6%) of them to be hypercholesterolemic. There was a significant relation between high total cholesterol (TC) and high TC/HDLC, as well as high or very high hsCRP and high TC/HDLC (both, p<0.001). Males tend to have higher TC/HDLC and hsCRP than females (both p0.002 and 0.005, respectively). Family history of CHD was found in 8 students and obesity was recorded in 5 volunteers.
Conclusion
The results necessitate further studies in determining the cause of PHC. We predict a genetic element contributing to the high percentage of PHC in the current study.
Keywords: Hypercholesterolemia, hsCRP, Coronary Heart Disease (CHD), University Students
Introduction
Coronary heart disease (CHD) is the leading cause of death worldwide according to the World Health Organization. It is responsible for more than 17 million deaths around the world annually.1 Hypercholesterolemia (HC) is the most significant factor in causing CHD and stroke which is implicated in 56% of stroke deaths.1,2 HC is either primary or secondary; PHC is mostly due to sedentary lifestyle, unhealthy dietary habits or genetic disorders.3 In contrast, secondary HC is mainly due to medical conditions such as diabetes, chronic renal failure, hypothyroidism, and taking certain drugs such as; thiazides, and non-selective ß blockers.4
The normal values for lipids in children and young adults are defined according to age, sex, and ethnic background. Elevated cholesterol levels in early adulthood increase the risk for developing CHD later in life. It is reported that a cholesterol level determined at age 22 predicts the rate of development of CHD over the following 30 to 40 years.5,6 Additionally, about 50% of this age group (young adults) with high TC has five times the risk of a CHD event and nine times the risk of a myocardial infarction compared with those that have low TC levels over the ensuing 30 to 40 years.5,6 The National Cholesterol Education Program (NCEP) expert panel considers 4.40 mmol/L (170 mg/dL) of blood cholesterol levels in children and young adults over 10 years of age with risk factors, as borderline high.7-9 In contrast, adults’ blood cholesterol borderline high is 5.15 mmol/L (200 mg/dL). Framingham's Study regards cholesterol levels measured in young adults to be predictive of CHD mortality 10 years later.10 Several clinical parameters or biomarkers are used to assess the risk of CHD due to HC, among which are total cholesterol (TC), low density lipoprotein cholesterol (LDLC), and ratio of TC over high density lipoprotein cholesterol (HDLC).11-14
Several studies have reported on the prevalence of hypercholesterolemia and the risk of CHD in the Arab Gulf countries; however, most of them reported on HC and CHD risk among adults.15,16 Agarwal and his group found that more than 50% of Asian Arabs living in the United Arab Emirates are hypercholesterolemic.17 Also, 37% of Kuwaiti men over the age of 45 years are obese and 52% had elevated or high cholesterol levels.18 Al-Nuaim and his team reported that hypercholesterolemia to be 16% and 19% among Saudi males and females, respectively. They attributed the low percentage to the inclusion of young Saudis less than 30 years old in the studied sample.19 Importantly, the authors predicted that this percentage would increase due to contributing factors such as acquired nutritional habits, obesity and the lack of regular exercise; however, consanguinity and the genetic elements in PHC was never stressed.
High-sensitivity C-reactive protein (hsCRP) has emerged as a strong independent risk factor for predicting future cardiovascular events that adds prognostic information at all levels of LDL cholesterol and at all levels of the Framingham Risk Score.20-22 In a recent investigation, anti-inflammatory therapy, significantly reduced atherosclerosis, as well as blood level hsCRP.23,24
In this investigation, the lipid profile for nonsmoking apparently healthy young university students at the Arabian Gulf University, Kingdom of Bahrain were tested to determine the prevalence of HC and the risk level of developing CHD among the volunteers.
Methods
After the approval of the Ethics Committee at the Arabian Gulf University, 166 young, nonsmokers and apparently healthy medical or graduate students studying at the Arabian Gulf University, Kingdom of Bahrain were properly consented. The students investigated in this study were Saudis (85) and Bahrainis (81). The students were aged between 16-30 years old. Each volunteer filled a questionnaire about their medical history and their family medical history of HC, heart disease (fatal or non-fatal cardiac event), diabetes, hypertension and other disorders. Additionally, weight and height were measured to determine the body mass index (BMI; a major index of obesity) each volunteer was asked about her/his life style habits and conditions that cause secondary HC.
For blood collection and testing; blood samples of each volunteer were collected in two vacutainers; after overnight fasting, a plain tube and an oxalate fluoride tube. The plain tube was used to analyze the high sensitivity C-reactive protein (hsCRP), total proteins (TP), albumin (ALB), thyroid stimulating hormones (TSH), and the lipid profile including total cholesterol (TC), triglyceride (TG), low density lipoprotein (LDL), and high density lipoprotein (HDL). In contrast, the oxalate fluoride tube was used to analyze Glucose (GLU). Analysis of these tests was performed in the biochemistry laboratory at Salmaniya Medical Complex (SMC). The Dimension® clinical chemistry system was used for the quantitative determination of TC, TG, ALB, TP and GLU. Also, the COBAS INTEGRA systems was used for the quantitative determination of serum HDL-C concentration. TSH was determined using the electro-chemiluminescence immunoassay ECLIA used on the Roche Elecsys 2010 and MODULAR ANALYTICS E170 (Elecsys module) immunoassay analyzers. LDL-Cholesterol was calculated according to Friedewald calculation = LDL-Cholesterol = Total Cholesterol - (HDL + Triglyceride / 2.18). (Table 1)
Table 1. Clinical chemistry data. Analytes tested, reference values and obtained results with the standard deviation of each analyte.25.
| Clinical Test | All Students | Females | Males | Comments | |||
|---|---|---|---|---|---|---|---|
| Range | Mean ± SD |
Range | Mean ± SD |
Range | Mean ± SD |
||
| Age | 16-30 | 20.49±2.96 | 16-30 | 20.4+3.04 | 18-30 | 20.90±2.75 | |
| Cholesterol (3.6-5.1mmol/L) | 2.50-7.50 | 4.39±0.90 | 2.70–7.50 | 4.41±0.92 | 2.50-6.50 | 4.28±0.875 | Lipid profile |
| Triglycerides (0.2-1.8mmol/L) | 0.20-3.90 | 0.78±0.51 | 0.20-3.90 | 0.74±0.54 | 0.40-2.50 | 0.90±0.42 | Lipid profile |
| HDL (1.03-1.9mmol/L) | 0.76-3.20 | 1.46±0.38 | 0.79-3.20 | 1.53+0.36 | 0.76-1.78 | 1.23±0.27 | Lipid profile |
| LDL (2.6-3.34mmol/L) | 0.80-6.34 | 2.84±0.98 | 0.90-6.34 | 2.84+1.00 | 0.80-4.89 | 2.84±0.91 | Lipid profile |
| hsCRP (0-1.1mg/dL | 0.04-14.10 | 2.32±3.23 | 0.04-14.1 | 1.72±2.02 | 0.11-6.33 | 1.378±1.35 | Inflammation marker |
| Glucose (3.6–5.6mmol/L) | 1.90-5.70 | 4.80±0.45 | 4.00-5.70 | 4.78±0.36 | 1.90-5.70 | 4.87±0.66 | Testing for DM |
| TSH (0.25–5.0mIU/L) | 0.50-4.70 | 3.99±0.79 | 0.50-4.70 | 1.60±0.82 | 0.56-4.50 | 1.88±1.38 | Thyroid disease |
| Total Protein (64–82g/L) | 65.0-85.0 | 73.56±3.41 | 65.0-83.0 | 73.0±3.79 | 70.0-85.0 | 75.42±3.53 | Kidney function |
| Albumin (38–50g/L) | 31.0-52.0 | 43.66±8.67 | 31.0-48.0 | 43.0±2.94 | 41.0-52.0 | 46.08+2.61 | Kidney function |
HDL: High density lipoproteinLDL: low density lipoprotein; hsCRP: high sensitivity CRP; DM: Diabetes mellitus; TSH: thyroid stimulating hormone
The number of volunteers investigated (166) was statistically significant for 95% confidence coefficient and a precision value of 0.03. The data were analyzed using SPSS version 17. Chi-Square test was used to determine the relation between categorical variables. A p-value less than 0.05 was considered statistically significant.
Results
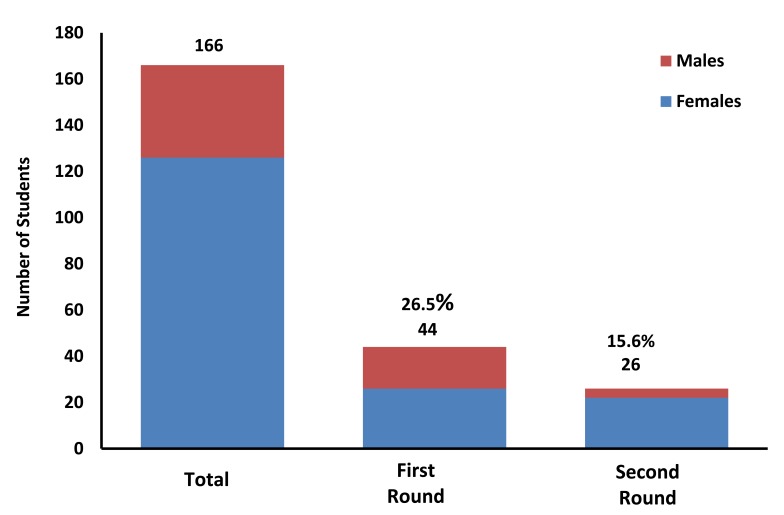
To determine total cholesterol, the American Heart Association (AHA) and the National Cholesterol Education Program (NCEP) standards were used for determining the total blood cholesterol level in the current study.7,26 A value of ≥5.1 mmol/L (200 mg/dL) was used as a cutoff value for determinating HC. In the first round of testing; 44 students (19 males and 25 females; 11.5% and 15.0%, respectively) of the investigated volunteers were found to have hypercholesterolemia and none of the 166 tested had secondary HC. The hypercholesterolemic students were counseled on healthy dietary habits and active life then measured the same set of analytes after 2-3 weeks. There was a significant reduction in the number of hypercholesterolemic students from 44 to 26 students (5 males and 21 females; 3% and 12.5%, respectively). Fig. 1 shows the results of the two rounds of testing and the gender distribution of the results. Table 2 shows the analytes concentration recorded in the second round for the 26 students.
Figure 1.
Significant change in PHC after proper health counseling. One hundred and sixty six students were screened for their fasting lipid profile and other analytes. The first round of screening showed that 44 of them have high blood cholesterol. Counseling reduced the number to 26.
Table 2. Primary hypercholesterolemia was found in 26 students.
| Number | Age | Sex | TC | TG | HDL | LDL | TC/HDLC | hsCRP | BMI>30 | FH |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 27 | F | 7.5 | 1.4 | 1.00 | 6.40 | 7.50 | 14.10 | Yes | Yes |
| 2 | 25 | F | 7.5 | 3.0 | 0.86 | 5.73 | 8.72 | 7.50 | Yes | Yes |
| 3 | 19 | F | 7.3 | 1.5 | 1.37 | 5.98 | 5.33 | 5.49 | - | - |
| 4 | 21 | M | 6.5 | 1.2 | 1.05 | 4.89 | 6.19 | 3.19 | - | - |
| 5 | 18 | F | 6.3 | 0.6 | 1.16 | 5.49 | 5.43 | 1.91 | Yes | - |
| 6 | 21 | F | 6.2 | 1.2 | 1.36 | 3.70 | 4.56 | 1.39 | - | - |
| 7 | 19 | F | 6.1 | 1.1 | 1.27 | 4.33 | 4.80 | 1.10 | Yes | Yes |
| 8 | 20 | F | 6.1 | 1.0 | 1.30 | 4.50 | 4.69 | 8.50 | - | - |
| 9 | 24 | F | 6.1 | 0.5 | 2.08 | 4.92 | 2.93 | 0.43 | - | - |
| 10 | 19 | F | 6.0 | 0.9 | 1.44 | 4.15 | 4.17 | 0.40 | - | - |
| 11 | 19 | F | 6.0 | 0.4 | 2.30 | 3.51 | 2.60 | 0.31 | - | Yes |
| 12 | 18 | F | 5.9 | 0.6 | 2.32 | 4.56 | 2.47 | 0.33 | - | - |
| 13 | 20 | F | 5.8 | 0.3 | 1.85 | 3.81 | 3.14 | 0.91 | - | - |
| 14 | 24 | F | 5.7 | 0.5 | 1.72 | 3.75 | 3.33 | 0.15 | - | - |
| 15 | 26 | F | 5.7 | 0.6 | 1.60 | 4.69 | 3.56 | 0.19 | - | - |
| 16 | 21 | F | 5.6 | 0.6 | 1.44 | 3.88 | 3.89 | 0.85 | - | - |
| 17 | 18 | F | 5.5 | 0.5 | 1.71 | 4.49 | 3.27 | 0.40 | - | - |
| 18 | 19 | F | 5.3 | 0.4 | 2.11 | 3.01 | 2.51 | 0.20 | - | - |
| 19 | 20 | F | 5.3 | 0.9 | 1.67 | 3.21 | 3.17 | 0.95 | - | Yes |
| 20 | 22 | F | 5.3 | 0.8 | 1.15 | 3.78 | 4.60 | 0.51 | Yes | Yes |
| 21 | 24 | F | 5.3 | 0.6 | 1.75 | 4.22 | 3.03 | 0.48 | - | - |
| 22 | 21 | M | 5.2 | 1.1 | 1.34 | 3.60 | 3.88 | 0.16 | - | - |
| 23 | 23 | M | 5.2 | 1.1 | 0.83 | 3.87 | 6.27 | 3.21 | - | - |
| 24 | 20 | M | 5.1 | 0.8 | 1.18 | 3.55 | 4.32 | 3.93 | - | - |
| 25 | 20 | F | 5.1 | 0.6 | 1.69 | 3.59 | 3.01 | 0.88. | - | - |
| 26 | 20 | F | 5.1 | 1.0 | 1.55 | 3.93 | 3.29 | 0.15 | - | - |
| 27 | 19 | M | 5.0 | 0.7 | 1.03 | 3.65 | 4.85 | 0.55 | - | - |
| 28 | 25 | F | 5.0 | 0.8 | 1.02 | 4.17 | 4.90 | 3.29 | - | Yes |
| 29 | 28 | M | 5.0 | 0.8 | 1.23 | 4.07 | 4.07 | 1.37 | - | - |
| 30 | 19 | M | 5.0 | 0.9 | 0.78 | 4.23 | 6.41 | 2.25 | - | Yes |
| 31 | 19 | M | 4.9 | 1.2 | 1.07 | 3.28 | 4.58 | 1.45 | - | - |
| 32 | 19 | F | 4.7 | 3.9 | 1.00 | 1.94 | 4.70 | 3.02 | - | - |
| 33 | 19 | M | 4.6 | 2.5 | 0.76 | 3.10 | 6.05 | 0.28 | - | - |
| 34 | 21 | M | 4.4 | 0.4 | 1.02 | 3.75 | 4.31 | 1.30 | - | - |
| 35 | 20 | M | 3.4 | 1.6 | 0.82 | 2.29 | 4.15 | 1.38 | - | - |
| 36 | 19 | F | 3.3 | 2.7 | 0.79 | 1.27 | 4.18 | 6.33 | - | - |
Age, Sex, Total Cholesterol (TC), Triglycerides (TG), High Density Lipoprotein (HLD), Low Density Lipoprotein (LDL), and the ratio of TC/HDL, the inflammation marker hsCRP, Body Mass Index (BMI) and Family history of CHD (FH) are tabulated. Lipid profile analytes were assayed after 12 -14 hour fasting.
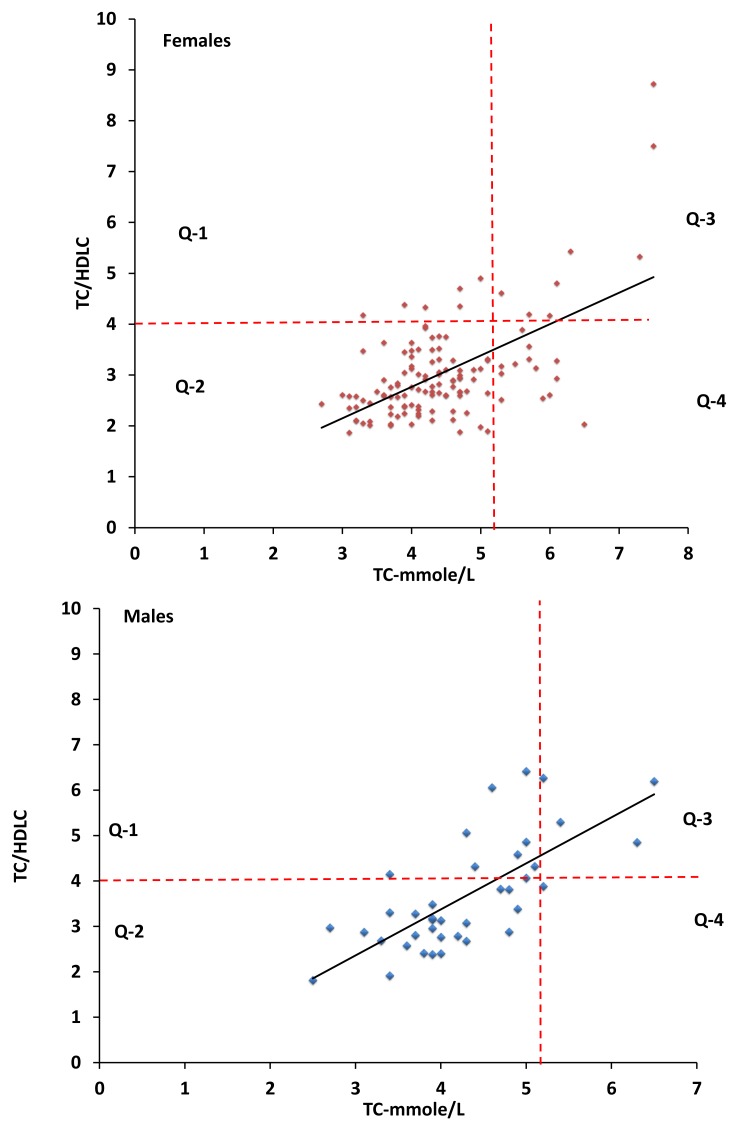
The ratio of Total Cholesterol/High Density Lipoprotein Cholesterol (TC/HDLC) was examinde in this study since it is established that low levels of high density lipoprotein cholesterol (HDLC) is a risk factor in developing CHD. Investigators found that the ratio of TC/HDLC ≥4.0 correlates positively with higher risk of developing CHD.8 Thus we determined the TC/HDLC in all students. Of the 26 hypercholesterolemic students, we found 12 (46.2%) students with a ratio of TC/HDLC ≥4.0, in contrast; 14 (53.8%) students have a ratio of <4.0, (Table 2). There is a positive relation between high TC and high TC/HDLC (p<0.001). As shown in Fig. 2, 12/26 (46.2%) have a high ratio of TC/HDLC while 10/140 (7.1%) students have high ratio of TC/HDLC from those with normal or low blood cholesterol levels group.
Figure 2.
Positive correlation between high TC and TC/HDLC. 46.2% of the 26 volunteers with high cholesterol (TC) have high ratio of TC/HDLC (Q-3 in both graphs), while only 9.1% could be detected in the volunteers with normal or low cholesterol (Q-1 in both graphs). The cutoff values for TC and TC/HDLC are drawn in dashed lines.
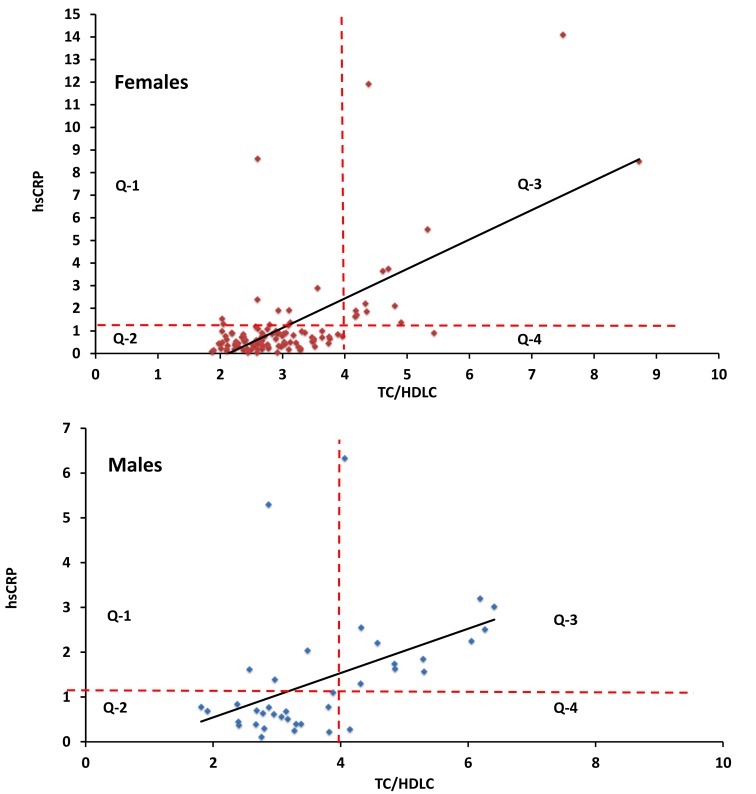
High sensitivity CRP (hsCRP) was also studied since it is established that CHD is a disorder of both inflammation and hyperlipidemia.27-30 Also, large scale studies have established that individuals with 1.0 to 3.0 mg/L hsCRP have moderate risk for CHD while ≥3.0 mg/L are at high risk. Therefore, the inflammation biomarker hsCRP was measured in all volunteers. High sensitivity CRP was high or very high in 18/22 (81.8%) students with high ratio of TC/HDL-C; while it was high only in 14/145 (9.7%) students with low TC/HDL-C (p≥0.001). (Fig. 3)
Figure 3.
Positive correlation between inflammation and high levels of TC/HDLC. 81.8% of the volunteers with high ratio of TC/HDLC (Q-3 in both graphs) have high or very high hsCRP. In contrast, 9.7% of the volunteers with low TC/HDLC have high hsCRP (Q-1 in both graphs). The cutoff values for TC and TC/HDLC are drawn in dashed lines.
The effect of gender and the risk associated with CHD was also studied. According to the AHA, males have a greater risk than females for CHD and they tend to have these problems earlier in life. In the current study, 12/45 (26.7%) and 14/45 (31.1%) of males were found to have high TC/HDLC and hsCRP, respectively; while a lower incidence was reported in female with 14/121 (11.6%) and 18 (14.9%), (p=0.002 and 0.005, respectively). (Figs. 2, 3)
Obesity and family history were also considered in this study. Among the volunteers, 8 students were reported to have a family history of cardiac events and five of these students were obese with BMI >30. (Table 2)
Discussion
This study shows a relatively high percentage of hypercholesterolemia among young university students. A higher frequency of PHC was observed in males than in females, a consensus accepted in the scientific community.31 Using the formula provided by the National Institutes of Health (NIH, USA),32 the data from the current study may be used to calculate the risk factor of developing a CHD event in the next ten years among the study participants. The presence of family history of CHD in students with high risk indicates the possibility of having a genetic element in CHD. Obesity also contributed to the risk of CHD in five students (3%). Although controversial, factors causing PHC can be controlled by lifestyle modifications, genetic counseling and administration of drugs such as statins.1,33
For adolescents and young adults at low risk, lipid profile testing is not ordered routinely. Also, there is no consensus among experts in the field for the definition of hypercholesterolemia. However, the American National Heart, Lung, and Blood Institute and the National Cholesterol Education Program define HC according to CHD risk factors score of each of individual.7 Thus, for individuals with 0-1 risk factors (as with the current study participants), normal LDLC would be ≤4.2 mmol/L; TC would be ≤5.1 mmol/L and TC/HDLC ≤4. The three guidelines are combined in a Venn diagram as shown in Fig. 4. Ten students (nine females and one male) among the studied group exhibited high or very high levels in all three critria.
Figure 4.
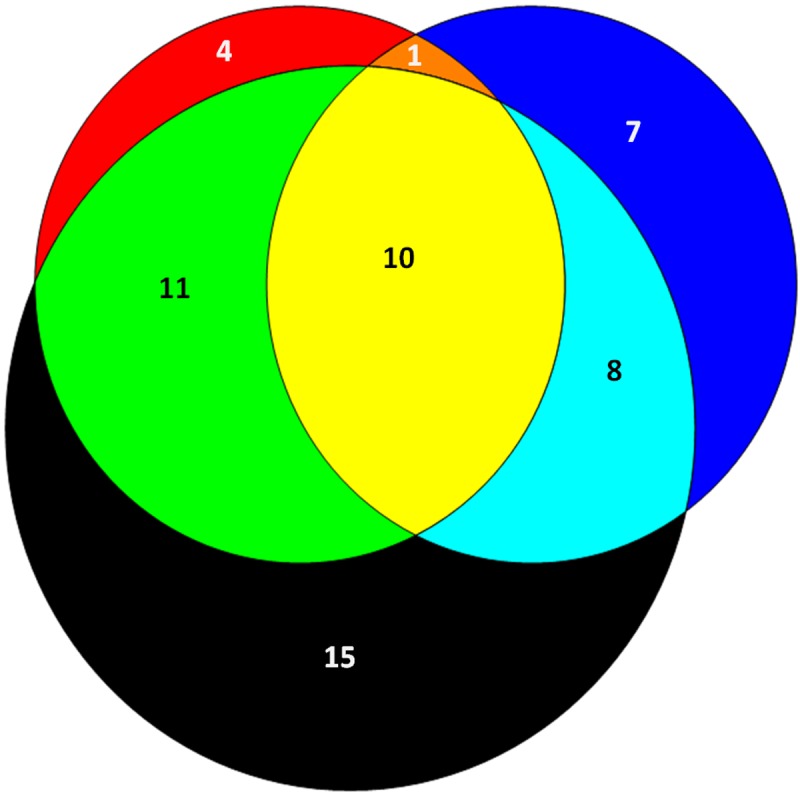
Venn diagram summarizing the three criteria used to define hypercholesterolemia in individuals with no CHD risk factors. The red circle represents students with total cholesterol TC ≥5.1 mmol/L, the black circle represents students with LDL ≥3.4 mmol/L, and the blue circle represents students with TC/HDL ≥4.0. Ten students (9 females and one male) in the yellow area have high levels of TC, LDL, and TC/HDLC.
According to WHO, HC is a global health problem that has to be monitored and controlled. However, very few studies address this issue in our area.1 The Bahrain Ministry of Health reported that more than 60% of Bahrainis over 19 years of age are either obese or overweight, and CHD is the main cause of death (40%) among Bahrainis.34 Additionally, the Clinical Chemistry Laboratory at Salmaniya Medical Complex receives around 5000 lipid profile samples monthly from all satellite centers in the country, 25% of which are hypercholesterolemic (Dr. Das, personal communications).
Hypercholesterolemia by itself is not a disease, but it is a metabolic imbalance that contributes to several diseases mainly CHD. Excess circulating cholesterol and low density lipoprotein (LDL) damage the endothelium of the coronary artery and promote inflammation culminating in restriction of the coronary artery and plaque rupture. On the other hand, substantial evidence supports the role of inflammation in atherogenesis where more than 50% of heart attacks and strokes occur among individuals with normal or low blood cholesterol. Thus, inflammation markers such as hsCRP, proinflammatory cytokines, acute phase reactants and others should be considered in determining the risk of CHD.22,35
Young people with a high cholesterol levels are more likely to be unaware of this elevation because they have not been tested and are more likely to ignore it since they are not experiencing symptoms. Acquired HC due to high fat diet, primarily saturated fats, coupled with inactive lifestyle can be reversed by modifying both. Indeed, several studies consider HDL an atheroprotective molecule due to its anti-inflammatory effects.35
The majority of PHC is due to inactivity and unhealthy diet. Though generally, the contribution of defective genes involved in the metabolism of lipids plays a minor role in causing acquired HC.36 However, sometimes the contribution of genetics in PHC could be significant where founder mutations are present.37 Recently, we discovered a founder mutation in the gene coding for low density lipoprotein receptor (LDLR) in two unrelated Arab families that descended from Adnan and Qahtan, the fathers of Arabs.38 Alternatively, elevated blood lipid levels could be associated with genetic variations (SNPs) in different loci.39,40
Pletcher et al. 2010, reported that non-optimal levels of LDL (high) and HDL (low) cholesterol during young adulthood are independently associated with CHD two decades later. Thus, cholesterol screening is recommended by the age of 20 for overweight young adults and those with family history of CHD.41,42 The greatest challenge for the public health workers is to assess the prevalence of PHC and reduce the cost of this asymptomatic disorder through signaling on modifiable and non-modifiable risk factors. The burden of these diseases is not limited to claiming lives, but also to escalating costs of health care. About 17% of American adults have high blood cholesterol. The associated direct and indirect costs of CHD in the United States are between $300-$500 billion annually (AHA, 2010).26
Among the limitations of this study is the sample gender composition; however, this is close to the institution’s student composition, where female students represent 70%. However, the number of students (166) was statistically significant for 95% confidence coefficient and a precision value of 0.03. Irrespective of the interpretations, more studies are needed in the area of epidemiology to establish the prevalence of HC among the entire population and not only young healthy individuals.
Conclusion
The prevalence of secondary HC is expected to be high among Arabs, especially in the Arab Gulf area. Abdel-Aal et al. 2008 found approximately 80% of Jordanian patients with diabetes mellitus type 2 (DM-2) are hypercholesterolemic.43 The International Diabetes Federation reported DM-2 prevalence in six Arab countries (Bahrain, Egypt, Kuwait, Oman, Saudi Arabia and United Arab Emirates) with the UAE (reaching almost 20%) being among the 10 countries in the world with the highest diabetes prevalence.44 The prevalence is projected to be higher in the coming years. High prevalence of primary and secondary hypercholesterolemia will burden the economy of the Arab nations, thus we recommend rapid intervention through screening programs, education, counseling, and cholesterol lowering drug administration.
Acknowledgements
We thank the students who participated in this study and the Student Counsel at the Arabian Gulf University for their valuable help in recruiting the volunteer students. We thank Dr. Abdel-Rahman Al-Musaiger for his comments and critical review of the article and Dr. Yas Sultani from the Arabian Gulf University for helpful discussion. Additionally, we thank the Clinical Chemistry Lab staff at Salmaniya Medical Complex for their valuable help. The authors declare that there is no conflict of interest.
References
- 1.World Health Organization. Prevention of Cardiovascular Disease: guidelines for assessment and management of cardiovascular Risk. 2007.
- 2.Tirschwell DL, Smith NL, Heckbert SR, Lemaitre RN, Longstreth WT, Jr, Psaty BM. Association of cholesterol with stroke risk varies in stroke subtypes and patient subgroups. Neurology 2004. Nov;63(10):1868-1875 10.1212/01.WNL.0000144282.42222.DA [DOI] [PubMed] [Google Scholar]
- 3.Annabelle Rodriguez-Oquendo. Peter O, Kwiterovich, Jr. Dyslipidemias, in Inborn Metabolic Diseases Diagnosis and Treatment, John Fernandes et al., editors, Springer, 2006;389-409. [Google Scholar]
- 4.Fogari R, Zoppi A, Corradi L, Preti P, Mugellini A, Lusardi P. Beta-blocker effects on plasma lipids during prolonged treatment of hypertensive patients with hypercholesterolemia. J Cardiovasc Pharmacol 1999. Apr;33(4):534-539 10.1097/00005344-199904000-00004 [DOI] [PubMed] [Google Scholar]
- 5.Washington RL. Interventions to reduce cardiovascular risk factors in children and adolescents. Am Fam Physician 1999. Apr;59(8):2211-2218 [PubMed] [Google Scholar]
- 6.Cleeman JI, Grundy SM. National Cholesterol Education Program recommendations for cholesterol testing in young adults. A science-based approach. Circulation 1997. Mar;95(6):1646-1650 10.1161/01.CIR.95.6.1646 [DOI] [PubMed] [Google Scholar]
- 7.The national cholesterol education program http://www.nhlbi.nih.gov/about/ncep/ncep_pd.htm
- 8.Carleton RA, Dwyer J, Finberg L, Flora J, Goodman DS, Grundy SM, et al. Report of the Expert Panel on Population Strategies for Blood Cholesterol Reduction. A statement from the National Cholesterol Education Program, National Heart, Lung, and Blood Institute, National Institutes of Health. Circulation 1991. Jun;83(6):2154-2232 10.1161/01.CIR.83.6.2154 [DOI] [PubMed] [Google Scholar]
- 9.LaRosa JC, Hunninghake D, Bush D, Criqui MH, Getz GS, Gotto AM, Jr, et al. The cholesterol facts. A summary of the evidence relating dietary fats, serum cholesterol, and coronary heart disease. A joint statement by the American Heart Association and the National Heart, Lung, and Blood Institute. The Task Force on Cholesterol Issues, American Heart Association. Circulation 1990. May;81(5):1721-1733 10.1161/01.CIR.81.5.1721 [DOI] [PubMed] [Google Scholar]
- 10.Anderson KM, Castelli WP, Levy D. Cholesterol and mortality. 30 years of follow-up from the Framingham study. JAMA 1987. Apr;257(16):2176-2180 10.1001/jama.1987.03390160062027 [DOI] [PubMed] [Google Scholar]
- 11.Berns MA, de Vries JH, Katan MB. Determinants of the increase of serum cholesterol with age: a longitudinal study. Int J Epidemiol 1988. Dec;17(4):789-796 10.1093/ije/17.4.789 [DOI] [PubMed] [Google Scholar]
- 12.Wannamethee SG, Shaper AG, Ebrahim S, Ebrahim S. HDL-Cholesterol, total cholesterol, and the risk of stroke in middle-aged British men. Stroke 2000. Aug;31(8):1882-1888 10.1161/01.STR.31.8.1882 [DOI] [PubMed] [Google Scholar]
- 13.Lemieux I, Lamarche B, Couillard C, Pascot A, Cantin B, Bergeron J, et al. Total cholesterol/HDL cholesterol ratio vs LDL cholesterol/HDL cholesterol ratio as indices of ischemic heart disease risk in men: the Quebec Cardiovascular Study. Arch Intern Med 2001. Dec;161(22):2685-2692 10.1001/archinte.161.22.2685 [DOI] [PubMed] [Google Scholar]
- 14.Horenstein RB, Smith DE, Mosca L. Cholesterol predicts stroke mortality in the Women’s Pooling Project. Stroke 2002. Jul;33(7):1863-1868 10.1161/01.STR.0000020093.67593.0B [DOI] [PubMed] [Google Scholar]
- 15.Abalkhail BA, Shawky S, Ghabrah TM, Milaat WA. Hypercholesterolemia and 5-year risk of development of coronary heart disease among university and school workers in Jeddah, Saudi Arabia. Prev Med 2000. Oct;31(4):390-395 10.1006/pmed.2000.0713 [DOI] [PubMed] [Google Scholar]
- 16.Al Riyami AA, Afifi M. Clustering of cardiovascular risk factors among Omani adults. East Mediterr Health J 2003. Sep-Nov;9(5-6):893-903 [PubMed] [Google Scholar]
- 17.Agarwal MM, Hughes PF, Haliga AA, Newman P, Sheekh-Hussen MM, Shalabi AG. Relevance of cholesterol screening in the United Arab Emirates. A preliminary study. Eur J Epidemiol 1995. Oct;11(5):581-585 10.1007/BF01719312 [DOI] [PubMed] [Google Scholar]
- 18.Jackson RT, Al-Mousa Z, Al-Raqua M, Prakash P, Muhanna AN. Multiple coronary risk factors in healthy older Kuwaiti males. Eur J Clin Nutr 2002. Aug;56(8):709-714 10.1038/sj.ejcn.1601379 [DOI] [PubMed] [Google Scholar]
- 19.Al-Nuaim AR, Al-Rebeann K, Al-Mazrou Y, Al-Attas O, Al-Daghari N. Serum total, fractionated cholesterol concentration distribution and prevalence of hypercholesterolemia in Saudi Arabia, regional variation. Ann Saudi Med 1997. Mar;17(2):179-184 [DOI] [PubMed] [Google Scholar]
- 20.Ridker PM, Rifai N, Rose L, Buring JE, Cook NR. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med 2002. Nov;347(20):1557-1565 10.1056/NEJMoa021993 [DOI] [PubMed] [Google Scholar]
- 21.Arnett DK, Jacobs DR, Jr, Luepker RV, Blackburn H, Armstrong C, Claas SA. Twenty-year trends in serum cholesterol, hypercholesterolemia, and cholesterol medication use: the Minnesota Heart Survey, 1980-1982 to 2000-2002. Circulation 2005. Dec;112(25):3884-3891 10.1161/CIRCULATIONAHA.105.549857 [DOI] [PubMed] [Google Scholar]
- 22.Tsimikas S, Willerson JT, Ridker PM. C-reactive protein and other emerging blood biomarkers to optimize risk stratification of vulnerable patients. J Am Coll Cardiol 2006. Apr;47(8)(Suppl):C19-C31 10.1016/j.jacc.2005.10.066 [DOI] [PubMed] [Google Scholar]
- 23.Natarajan P, Cannon CP. Could direct inhibition of inflammation be the "next big thing" in treating atherosclerosis? Arterioscler Thromb Vasc Biol 2010. Nov;30(11):2081-2083 10.1161/ATVBAHA.110.213793 [DOI] [PubMed] [Google Scholar]
- 24.Sarov-Blat L, Morgan JM, Fernandez P, James R, Fang Z, Hurle MR, et al. Inhibition of p38 mitogen-activated protein kinase reduces inflammation after coronary vascular injury in humans. Arterioscler Thromb Vasc Biol 2010. Nov;30(11):2256-2263 10.1161/ATVBAHA.110.209205 [DOI] [PubMed] [Google Scholar]
- 25.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972. Jun;18(6):499-502 [PubMed] [Google Scholar]
- 26.American Heart Association (AHA) URL http://www.cdc.gov/chronicdisease/resources/publications/AAG/dhdsp.htm
- 27.Ridker PM, Buring JE, Cook NR, Rifai N. C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of 14 719 initially healthy American women. Circulation 2003. Jan;107(3):391-397 10.1161/01.CIR.0000055014.62083.05 [DOI] [PubMed] [Google Scholar]
- 28.Koenig W. C-reactive protein: risk assessment in the primary prevention of atherosclerotic disease. Has the time come for including it in the risk profile? Ital Heart J 2001. Mar;2(3):157-163 [PubMed] [Google Scholar]
- 29.Mora S, Musunuru K, Blumenthal RS. The clinical utility of high-sensitivity C-reactive protein in cardiovascular disease and the potential implication of JUPITER on current practice guidelines. Clin Chem 2009. Feb;55(2):219-228 10.1373/clinchem.2008.109728 [DOI] [PubMed] [Google Scholar]
- 30.Koenig W. Is hsCRP Back on Board? Implications from the JUPITER Trial. Clin Chem 2009. Feb;55(2):216-218 10.1373/clinchem.2008.115915 [DOI] [PubMed] [Google Scholar]
- 31.Fodor G, Tzerovska R. Coronary heart disease: is gender important? J Men's Health 2004;1(1):32-37 [Google Scholar]
- 32.NIH URL: (http://hp2010.nhlbihin.net/atpiii/calculator.asp?usertype=prof).
- 33.Versmissen J, Oosterveer DM, Yazdanpanah M, Defesche JC, Basart DC, Liem AH, et al. Efficacy of statins in familial hypercholesterolaemia: a long term cohort study. BMJ 2008;337:a2423 10.1136/bmj.a2423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.http://www.moh.gov.bh/PDF/Publications/Statistics/HS2009/PDF/CH03-vital%20stat_2009.pdf Downloaded April 2011.
- 35.Haas MJ, Mooradian AD. Inflammation, high-density lipoprotein and cardiovascular dysfunction. Curr Opin Infect Dis 2011. Jun;24(3):265-272 10.1097/QCO.0b013e328344b724 [DOI] [PubMed] [Google Scholar]
- 36.Ford ES, Capewell S. Proportion of the decline in cardiovascular mortality disease due to prevention versus treatment: public health versus clinical care. Annu Rev Public Health 2011;32:5-22 10.1146/annurev-publhealth-031210-101211 [DOI] [PubMed] [Google Scholar]
- 37.Dedoussis GV, Schmidt H, Genschel J. LDL-receptor mutations in Europe. Hum Mutat 2004. Dec;24(6):443-459 10.1002/humu.20105 [DOI] [PubMed] [Google Scholar]
- 38.Shawar SM, Al-Drees MA, Ramadan AR, Ali NH, Alfadhli SM. The Arabic allele: a single base pair substitution activates a 10-base downstream cryptic splice acceptor site in exon 12 of LDLR and severely decreases LDLR expression in two unrelated Arab families with familial hypercholesterolemia. Atherosclerosis 2012. Feb;220(2):429-436 10.1016/j.atherosclerosis.2011.10.045 [DOI] [PubMed] [Google Scholar]
- 39.Waterworth DM, Ricketts SL, Song K, Chen L, Zhao JH, Ripatti S, et al. Wellcome Trust Case Control Consortium Genetic variants influencing circulating lipid levels and risk of coronary artery disease. Arterioscler Thromb Vasc Biol 2010. Nov;30(11):2264-2276 10.1161/ATVBAHA.109.201020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Park MH, Kim N, Lee JY, Park HY. Genetic loci associated with lipid concentrations and cardiovascular risk factors in the Korean population. J Med Genet 2011. Jan;48(1):10-15 10.1136/jmg.2010.081000 [DOI] [PubMed] [Google Scholar]
- 41.Pletcher MJ, Bibbins-Domingo K, Liu K, Sidney S, Lin F, Vittinghoff E, et al. Nonoptimal lipids commonly present in young adults and coronary calcium later in life: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Ann Intern Med 2010. Aug;153(3):137-146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gooding HC, de Ferranti SD. Cardiovascular risk assessment and cholesterol management in adolescents: getting to the heart of the matter. Curr Opin Pediatr 2010. Aug;22(4):398-404 10.1097/MOP.0b013e32833a6e22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abdel-Aal NM, Ahmad AT, Froelicher ES, Batieha AM, Hamza MM, Ajlouni KM. Prevalence of dyslipidemia in patients with type 2 diabetes in Jordan. Saudi Med J 2008. Oct;29(10):1423-1428 [PubMed] [Google Scholar]
- 44.International Diabetes Federation. Diabetes Atlas, 3rd Edition. 2007; Downloaded from URL: http://www.diabetesatlas.org/sites/default/files/IDF%20Diabetes%20Atlas-2007%20%283rd%20edition%29.pd