Abstract
Objectives. To determine the optimum strategy for increasing up-to-date (UTD) levels in older Americans, while reducing disparities between White, Black, and Hispanic adults, aged 65 years and older.
Methods. Data were analyzed from the 2008 Behavioral Risk Factor Surveillance System, quantifying the proportion of older Americans UTD with influenza and pneumococcal vaccinations, mammograms, Papanicolaou tests, and colorectal cancer screening. A comparison of projected changes in UTD levels and disparities was ascertained by numerically accounting for UTD adults lacking 1 or more clinical preventive services (CPS). Analyses were performed by gender and race/ethnicity.
Results. Expanded provision of specific vaccinations and screenings each increased UTD levels. When those needing only vaccinations were immunized, there was a projected decrease in racial/ethnic disparities in UTD levels (2.3%–12.2%). When those needing only colorectal cancer screening, mammography, or Papanicolaou test were screened, there was an increase in UTD disparities (1.6%–4.5%).
Conclusions. A primary care and public health focus on adult immunizations, in addition to other CPS, offers an effective strategy to reduce disparities while improving UTD levels.
Clinical preventive services (CPS), such as screening tests and vaccinations, are important interventions for identifying, forestalling, and preventing disease across the life span. They are typically delivered in primary care practices and, increasingly, in community settings.1 The Advisory Committee on Immunization Practices (ACIP)2 and the US Preventive Services Task Force (USPSTF)3 have established guidelines for the delivery of these services for adults aged 65 years and older. Recommendations for persons aged 65 years and older include the following core CPS: influenza and pneumococcal vaccinations (PPV), cardiovascular screenings, and colorectal cancer screening. Additional recommendations for women in this age range include mammography and, in certain circumstances, Papanicolaou (Pap) tests.
These core CPS are distinct in that they are ranked highly by the ACIP or USPSTF (grades A or B), and recommended based on demographic characteristics (age and gender) rather than on health condition, making them appropriate interventions for both primary care and public health. In 2010, a Healthy People 2020 objective was established to increase by 10% the proportion of older adults “up-to-date” (UTD) with core preventive services, from a 2008 baseline of 46.3% in men and 47.9% in women.4 Several studies confirmed that racial and ethnic minorities were less likely to receive each of these measures compared with their non-Hispanic White peers.5–7 Given a growing and increasingly diverse older US population,8 expanding access to and delivery of core CPS, while reducing racial and ethnic disparities in the receipt of these measures, is a priority.4 Developing an approach that integrates the work of the clinical and public health communities to accomplish this objective is likely to be the most effective strategy for achieving this goal. This integrated approach is supported by the recommendations of The Community Guide to Preventive Services9 and the Guide to Clinical Preventive Services,3 which together provide evidence-based recommendations across the prevention spectrum.10
With the goal of enhancing the linkages between community and primary care to facilitate the uptake of preventive services, we examine the question of which preventive service(s) are needed to maximally improve UTD levels while decreasing racial/ethnic disparities in UTD levels among adults aged 65 years and older. Health disparities refer to “differences in health outcomes between groups that reflect social inequalities,” and their elimination requires an enhanced understanding of which groups are most vulnerable, how the disparities can be corrected through available interventions, and monitoring over time.11 As part of this assessment, projected changes in UTD levels and disparities were calculated, based on comparing the impact of providing different core preventive services to persons in each racial/ethnic group who were missing a single service, using 2008 data as a baseline. Projected UTD changes for Blacks and Hispanics were compared with those for Whites. Because we analyzed an all-or-none measure, it was only when projecting increases in the delivery of preventive services for persons missing a single service that levels of being UTD and associated racial and ethnic disparities would change. From a programmatic standpoint, every person should receive every CPS recommended for him or her.
METHODS
Data from the Behavioral Risk Factor Surveillance System (BRFSS) for the 50 states and the District of Columbia were used for the study. The BRFSS, sponsored by the Centers for Disease Control and Prevention (CDC) in collaboration with state health departments, conducts annual state-based telephone surveys of noninstitutionalized US adults aged 18 years and older concerning health practices related to the leading causes of death and disability.12
The UTD levels for persons aged 65 years and older by racial/ethnic group were ascertained from the BRFSS surveys in 2002, 2004, 2006, and 2008. Median response rates for the 2002, 2004, and 2006 BRFSS were, respectively, 44.5%,13 41.20%,14 and 35.4%.15 In-depth analysis was performed on the 2008 BRFSS dataset. In 2008, the median survey response rate was 53.3% (range 35.8% in Maryland to 65.9% in Kentucky). Data used in this study were limited to 121 365 respondents who were aged 65 years and older and either non-Hispanic White, non-Hispanic Black, or Hispanic of any race, (n > 1000). Asian/Pacific Islanders and American Indian/Alaska Native older adults were not included because their sample sizes among older men were each less than 500. Results were based on weighted data that accounted for different probabilities of selection and were adjusted to reflect the population distribution in each state by age and gender, or by age, race/ethnicity, and gender.
Measures
Measures of the receipt of selected CPS recommended by ACIP and the USPSTF1,2 for adults aged 65 years and older were used in the analyses. These included colorectal cancer screening, influenza and PPV immunization, as well as for women, a mammogram and a Pap test. Although some of these recommendations were subsequently adjusted, we used recommendations that were contemporaneous with the survey.
Blood pressure and cholesterol screenings, although recommended for all older adults, were not included in the analysis. The BRFSS has not asked questions about hypertension screening since 1999, when more than 95% of older adults reported they had their blood pressure checked in the past 2 years.16 Questions about cholesterol screening were not asked in all states in 2008, and were not incorporated into the UTD measure. However, analysis from a previous study suggested that including hypertension and cholesterol screening levels in this all-or-none measure would not make a large difference in the percentage of older Americans UTD on all services.17 Responses to all measures were coded as “yes” or “no” based on receipt of the preventive service according to contemporaneous schedules recommended by the ACIP and USPSTF. For example, adults could meet the recommendation for colorectal cancer screening by either having a fetal occult blood test within 1 year or having colonoscopy within 10 years, or sigmoidoscopy within 5 years. 18 However, we used a 10-year interval for sigmoidoscopy or colonoscopy because before 2008 the BRFSS question did not distinguish between the 2 interventions. Other “yes” responses included ever having a pneumonia vaccination, an influenza vaccination within the past year, and for women, a mammogram within 2 years and a Pap test within 3 years. Adults who had not received these tests or had the tests outside the designated schedule were assigned a “no” response for these services. Women who reportedly had a hysterectomy were coded as having met the recommendation for cervical cancer screening.
A variable was created to measure whether all recommendations had been met. This measure represented UTD status among adults aged 65 years and older and included 3 clinical preventive services for men (colorectal cancer screening, and influenza and pneumonia vaccination) and 5 for women (these 3 plus a mammogram and Pap test). Analyses were conducted to determine the percent of men and women, by racial/ethnic group, who received each individual service, the number of services received, and the percent UTD for all services.
Potential changes in both UTD levels and disparities were estimated by calculating the effect of providing each CPS to persons missing only that service to be UTD. These respondents were a subset of men who received 2 services (of a maximum of 3) and women who received 4 (of a maximum of 5). This approach was taken because it represents the minimum—and therefore most easily achievable—intervention that could bring about a change in UTD levels. Single services provided to persons missing more than 1 service would not change their UTD levels because it was an all-or-none measure. Changes were calculated for both genders as absolute and relative differences in UTD levels, comparing by gender, Whites and Blacks, and Whites and Hispanics. Only absolute differences in disparities were reported, given the accepted convention that when there are space limitations and, when the absolute and relative changes shifted in the same direction (which was the case in this study), only absolute differences are shown.19
Demographic and health-related characteristics of respondents were tabulated. These categories included age, gender, race/ethnicity, education, geography, and health insurance (“Do you have any kind of health care coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare?”). Whether a person received a routine checkup in the past 2 years was ascertained with the question: “About how long has it been since you last visited a doctor for a routine checkup? A routine checkup is a general physical exam, not an exam for a specific injury, illness, or condition.”
Statistical Analysis
Statistical analysis was conducted in 2009 and 2010 using Stata software, version 9.0 (Stata Corp, College Station, TX). Pearson's χ2 test was used to determine whether selected demographic factors were associated with UTD levels, needing immunizations only, or any other combination of services. Racial/ethnic disparity was computed as the absolute percentage difference between UTD levels for non-Hispanic Whites and the comparison group.
RESULTS
Demographic and health-related characteristics of respondents are shown in Table A (available as a supplement to the online version of this article at http://www.ajph.org). These data are provided only for descriptive purposes. The component CPS that comprise the UTD measure, along with the self-reported rates of receipt of each one are presented in Table 1. PPV had the lowest level among all groups, except Black and White women. Among White women, colorectal cancer screening level was lowest, and among Black women, influenza vaccination was lowest. Mammography rates were similar for White, Black, and Hispanic women.
TABLE 1—
Receipt of Individual Services Comprising the Up-To-Date Measure, Men and Women, Aged 65 Years and Older: United States, 2008 BRFSS Self-Reports, Reduce Ethnic and Racial Disparities in the Delivery of Clinical Preventive Services
| Clinical Preventive Service and Demographic Variables | Men |
Women |
||||
| White (n = 33 417), % (95% CI) | Black (n = 1826), % (95% CI) | Hispanic (n = 1104), % (95% CI) | White (n = 60 422), % (95% CI) | Black (n = 4157), % (95% CI) | Hispanic (n = 2169), % (95% CI) | |
| Influenza vaccination | 72.3 (71.5, 73.0) | 57.2 (53.3, 61.1) | 62.1 (56.6, 67.2) | 72.0 (71.4, 72.5) | 54.6 (51.9, 57.2) | 65.3 (61.5, 69.0) |
| Pneumococcal vaccination | 66.4 (65.6, 67.2) | 46.6 (42.7, 50.6) | 46.9 (41.5, 52.3) | 70.9 (70.4, 71.5) | 56.1 (53.4, 58.7) | 52.1 (48.0, 56.1) |
| Colorectal cancer screening | 70.9 (70.1, 71.6) | 66.9 (63.1, 70.4) | 56.2 (50.7, 61.6) | 65.8 (65.2, 66.4) | 65.7 (63.1, 68.2) | 57.1 (53.0, 61.1) |
| Mammogram | 79.3 (78.8, 79.8) | 81.2 (79.1, 83.2) | 79.7 (76.2, 82.8) | |||
| Papanicolaou test | 67.5 (66.7, 68.3) | 73.6 (70.3, 76.6) | 70.9 (65.8, 75.5) | |||
Note. BRFSS = Behavioral Risk Factor Surveillance System; CI = confidence interval.
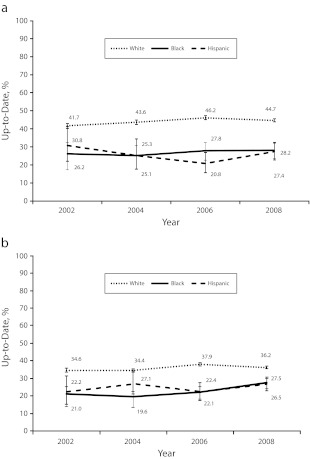
Table B (available as a supplement to the online version of this article at http://www.ajph.org) indicates low UTD levels for receipt of CPS among men and women in all racial/ethnic groups, ranging from 26.5% for Hispanic women to 44.7% for White men. Table B also indicates that among older adults who were not UTD, the largest proportion, more than one fourth, needed only 1 additional service to be UTD. This included 27.4% to 29.4% of all men (those who reported receipt of 2 services) and 25.6% to 27.9% of women (those with 4 services). Figure 1 shows that the low UTD rates and accompanying disparities between Blacks and Hispanics, respectively, compared with Whites (by gender), were persistent between 2002 and 2008. In 2008, absolute disparities ranged from 9.7% for White versus Hispanic women, to 17.3% for White versus Hispanic men.
FIGURE 1—
Percentage of (a) men and (b) women aged 65 years and older up-to-date by selected racial/ethnic groups in 2002, 2004, 2006, and 2008 using the Behavioral Risk Factor Surveillance System (BRFSS): United States, Reduce Ethnic and Racial Disparities in the Delivery of Clinical Preventive Services.
Note. BRFSS surveys are cross-sectional, with different respondents each year.
The percentages of adults, by racial/ethnic group and gender, who needed each specific service, and only that service to be UTD are shown in Table 2. Table 2 identifies which CPS for each gender and racial/ethnic group was likely to yield the greatest increases in UTD levels from improvements in the delivery of those services. For White men and women, this service was colorectal cancer screening, whereas for Black women it was influenza vaccination. For Black men and all Hispanics, it was PPV.
TABLE 2—
Percent of White, Black, or Hispanic Adults Aged 65 Years and Older Who Needed the Single Service Indicated to Be UTD: United States, 2008 BRFSS Self-Reports, Reduce Ethnic and Racial Disparities in the Delivery of Clinical Preventive Services
| Men |
Women |
|||||
| White | Black | Hispanic | White | Black | Hispanic | |
| Influenza vaccination | 6.2 | 7.0 | 5.0 | 5.4 | 9.3 | 4.5 |
| PPV | 10.6 | 13.7 | 12.6 | 6.3 | 7.2 | 8.5 |
| CRC screening | 12.6 | 8.1 | 9.8 | 9.8 | 6.4 | 8.2 |
| Mammogram | 2.9 | 2.0 | 2.2 | |||
| Papanicolaou test | 3.4 | 1.4 | 2.2 | |||
| Total | 29.4 | 28.7 | 27.4 | 27.9 | 26.4 | 25.6 |
Note. BRFSS = Behavioral Risk Factor Surveillance System; CRC = colorectal cancer screening; PPV = pneumococcal vaccination; UTD = up-to-date.
The potential increases in UTD levels and the accompanying changes in disparities with Whites—when the missing service was provided to persons lacking only that service—are shown, respectively, in Figures 2 and 3. Although there was an increase in UTD levels for each service delivered to both genders (Figure 2), a reduction in disparities occurred only with increased delivery of certain services (Figure 3). A reduction in disparities followed when PPV was provided (smaller disparities for Blacks and Hispanics, both genders), and when influenza vaccination was provided (smaller disparities for Black men and women, but not for Hispanic men and women). Figures 2 and 3 also indicate that the largest improvements in UTD levels and disparities occurred when vaccinations were delivered to persons missing either or both influenza and PPV. These results reflect that the absolute disparity at baseline for vaccinations was greater than for cancer screenings. By contrast, there was an increase in disparities for Blacks and Hispanics when colorectal cancer screening, Pap test, or mammography was provided to all persons missing only those services.
FIGURE 2—
Current up-to-date levels (%) for (a) men and (b) women aged 65 years and older compared with levels if persons who needed 1 service or both vaccinations received the service(s), in 2008 using the Behavioral Risk Factor Surveillance System: United States, Reduce Ethnic and Racial Disparities in the Delivery of Clinical Preventive Services.
Note. CRC = colorectal cancer; PPV = pneumococcal vaccination; UTD = up-to-date.
FIGURE 3—
Current absolute up-to-date disparity (%) with Whites compared with disparity (%) if (a) men and (b) women aged 65 years and older who needed 1 service or both vaccinations received the service(s), in 2008 using the Behavioral Risk Factor Surveillance System (BRFSS): United States, Reduce Ethnic and Racial Disparities in the Delivery of Clinical Preventive Services.
Note. CRC = colorectal cancer; PPV = pneumococcal vaccination; UTD = up-to-date.
DISCUSSION
The results of this study indicate that in 2008, consistent with earlier years, UTD levels among adults aged 65 years and older were low, and that there were significant racial and ethnic disparities in the receipt of a core set of CPS.
Although the study’s analytic approach quantified the differing impact on UTD levels and disparities for persons missing a specific CPS, it remains important for older adults to receive all recommended preventive services. Our analysis suggested that the largest reduction in disparities from the expanded delivery of a single preventive service would come from efforts to increase the receipt of PPV. Efforts to provide influenza and PPV to older adults would lead to an important decrease in UTD disparities between Whites and Hispanics, and erase UTD disparities between Whites and Blacks, if those vaccinations are delivered to persons missing only vaccinations to be UTD. Furthermore, the UTD levels for all race/ethnic groups would significantly improve.
The findings of this study were consistent with other studies on adult vaccination disparities, which found that coverage among Blacks and Hispanics was significantly lower than among Whites.5–7 Studies identified several barriers to adult vaccinations. One study identified perception and knowledge barriers; for example, Blacks and Hispanics who were aged 65 years and older were found to be more concerned about side effects from influenza vaccine and more likely to believe that receiving a flu shot was unnecessary or caused influenza, compared with Whites.20 Blacks and Hispanics were also less aware of recommendations for PPV.
The use of an adult all-or-none measure such as being UTD can raise the bar on performance,21 because a person is UTD only if all recommended services are delivered. The measure is fully scalable and can be employed to assess the provision of services at the practice level, the health plan, the community, the state, and the nation. The recently established Healthy People 2020 objective that seeks to increase the proportion of older adults who are UTD with CPS represents a recognition of the importance of improving the provision of core screenings and vaccinations, and suggests that tracking delivery 1 service at a time—although necessary and useful—may not be sufficient to achieve overall population targets for preventive services.
Our findings suggested a need for improved integration between the clinical and public health communities. Past experience with programs, such as the National Breast and Cervical Cancer Early Detection program, in which public health and clinical communities work together to increase the delivery of breast and cervical cancer screening to low-income women, have been particularly effective in eliminating disparities, particularly in the area of mammography, as shown in the present analysis.22 Public health brings strengths in community engagement and in the delivery of health communications messages that can complement the work of the clinical community in delivering these important services. Effective strategies in integration might include using traditional clinical and nontraditional community locations. Public health efforts that offer influenza vaccination with various combinations of other CPS, including mammography and colorectal cancer screening, have been tested, with promising results.23,24 Many preventive services are portable and deliverable in either clinical or community settings. Capitalizing on that flexibility and extending the use of an appropriate electronic information infrastructure can improve uptake and health outcomes.25
One such strategy, developed by the nonprofit organization Sickness Prevention Achieved through Regional Collaboration (SPARC), established local structures of accountability for the community-wide delivery of multiple CPS.26 The SPARC model envisions a collaboration of local prevention providers and stakeholders, brought together by a “neutral convener,” such as a local health department or area agency on aging. These collaborations plan and deploy CPS at access points across communities, working collaboratively with medical practices. With an emphasis on local systems and on CPS delivery, the SPARC model makes an impact at both the individual and population level. It sits astride a crucial “grey zone” between public health and medical care, identified as a transitional level in the health impact pyramid.27 As 1 example, a SPARC project designed to improve access to mammograms placed outreach workers at community influenza clinics to schedule mammograms for women overdue for screening. The program was endorsed by local physicians, and screening results were sent directly to the patient’s medical home. The study found that mammography use following access through influenza clinics was approximately twice that of women attending influenza clinics where access to mammography was not offered.23
Delivery of multiple CPS does not preclude efforts that focus exclusively on adult vaccinations across all race/ethnic groups. This study provided particularly strong support for policies that encourage the concurrent delivery of influenza and PPVs, which were already shown in community settings to significantly increase delivery levels of PPVs. 28 Another promising program of this kind is Vote & Vax, which encourages immunizers to set up flu shot clinics for voters and nonvoters at polling places on Election Day. Approximately 70% of persons who vote are aged 50 years and older. In 2008, Vote & Vax delivered more than 21 000 flu shots on a single day and found that approximately half those immunized were not regular flu shot recipients. Among African-American and Hispanic recipients, 60.2% and 64.8%, respectively, were not regular recipients.29 Furthermore, research suggested that campaigns that provide preventive care information to older Black men and women through informal and trusted conduits like beauty salons, barbershops, churches, and other community-based organizations might offer an effective way to reduce disparities in care.30
This study had a number of limitations. First, the BRFSS relied on self-reported data. Depending on the measure, self-reports could result in overestimates or underestimates compared with data sources, such as health care records. Services that were recommended at less frequent intervals, such as PPV, might be more likely to be underreported. The BRFSS validation study of PPV delivery indicated that patients’ recall of receiving a vaccination within 3 years was good (87%).31 No studies assessed validity of self-reported PPV by race/ethnicity. Unfamiliarity with medical terms and telescoping32 (recalling events more recently than they actually occurred) could affect the validity of self-reported CPS and probably resulted in overestimates.33,34 A review article by Nelson et al.35 rated the validity of self-reports for mammography, Pap test, colorectal cancer screening, and PPV as moderate and the validity for influenza vaccination as high. Second, households without telephones and cellular-only telephone households were excluded from the survey. Their omission might have resulted in an underestimation or overestimation of delivery rates.36,37 Third, the BRFSS did not include information on the 4.9% of adults 65 years and older who were institutionalized in 2008.38 Fourth, the BRFSS questions limited the ability to adequately determine compliance with Pap test recommendations for women aged 65 years and older. The USPSTF recommends against core screening for cervical cancer for women in this age group if they have had sufficient recent Pap tests with no abnormal results and were not otherwise at increased risk for cervical cancer.39 Without Pap test histories, we could not ascertain which of these older women might not need further Pap testing. Finally, the estimated UTD projections made in this study were based on receipt of a single CPS by persons missing only that service. It is possible that community- and clinic-based efforts to increase the provision of services would predominantly reach persons who were missing more than 1 service. As noted, UTD rates would not change unless all the missing services were provided.
This study documented the extent and persistence of disparities in the receipt of preventive services, and pointed toward a strategy that might yield significant improvements. Efforts to increase adult vaccination are essential to improving overall UTD levels and to eliminating racial and ethnic disparities in receipt of a core set of CPS.
Acknowledgments
Funding for this research was provided by the Centers for Disease Control and Prevention (CDC).
The authors would like to thank Dr. Michael Alderman for comments and suggestions on earlier drafts of this article.
Note. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the CDC.
Human Participant Protection
Because the BRFSS is a surveillance system, the CDC’s institutional review board determined that the BRFSS was exempt from its review.
References
- 1.Shenson D. Putting prevention in its place: the shift from clinic to community. Health Aff (Millwood). 2006;25(4):1012–1015 [DOI] [PubMed] [Google Scholar]
- 2.National Center for Immunization and Respiratory Disease General recommendations on immunization— recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2011;60(No. RR-2):1–64 [PubMed] [Google Scholar]
- 3.US Preventive Services Task Force Guide to Clinical Preventive Services 2010-2011. Washington, DC: 2010 [PubMed] [Google Scholar]
- 4.US Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2020. Available at: http://healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicid=31. Accessed May 18, 2012
- 5.Straits-Tröster KA, Kahwati LC, Kinsinger LSet al. Racial/ethnic differences in influenza vaccination in the Veterans Affairs healthcare system. Am J Prev Med. 2006;31(5):375–382 [DOI] [PubMed] [Google Scholar]
- 6.Winston CA, Wortley PM, Lees KA. Factors associated with vaccination of Medicare beneficiaries in five U.S. communities: results from the Racial and Ethnic Adult Disparities in Immunization Initiative Survey, 2003. J Am Geriatr Soc. 2006;54:303–310 [DOI] [PubMed] [Google Scholar]
- 7.Wortley P. Who’s getting shots and who’s not: racial/ethnic disparities in immunization coverage. Ethn Dis. 2005;15(2 suppl 3):S3-4–S3-6 [PubMed] [Google Scholar]
- 8.Hobbs F, Damon BL, Taeuber CM. Sixty-Five Plus in the United States. Washington, DC: U.S. Department of Commerce, Economics, and Statistics Administration, Bureau of the Census; 1996 [Google Scholar]
- 9.Community Preventive Services Task Force. What Is the Community Guide? Available at: http://www.thecommunityguide.org/index.html. Accessed May 18, 2012. [DOI] [PubMed]
- 10.Ockene JK, Edgerton EA, Teutsch SMet al. Integrating evidence-based clinical and community strategies to improve health. Am J Prev Med. 2007;32:244–252 [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention CDC health disparities and inequalities report – United States, 2011. MMWR. 2011;60(Suppl):1–116 [PubMed] [Google Scholar]
- 12. Behavioral Risk Factor Surveillance System. Available at: http://www.cdc.gov/brfss. Accessed May 18, 2012.
- 13. BRFSS Annual Survey Data. 2002 Summary Data Quality Report. Available at: http://www.cdc.gov/brfss/technical_infodata/2002QualityReport.htm. Accessed May 18, 2012.
- 14. BRFSS Annual Survey Data. 2004 Summary Data Quality Report. Available at: http://www.cdc.gov/brfss/technical_infodata/2004QualityReport.htm. Accessed May 18, 2012.
- 15.BRFSS 2006 Summary Data Quality Report. Available at: ftp://ftp.cdc.gov/pub/Data/Brfss/2006SummaryDataQualityReport.pdf. Accessed May 18, 2012
- 16.Centers for Disease Control and Prevention State-specific trends in self-reported blood pressure screening and high blood pressure—United States, 1991–1999. MMWR Morb Mortal Wkly Rep. 2002;51:456–460 [PubMed] [Google Scholar]
- 17.Shenson D, Bolen J, Adams M. Receipt of preventive services by elders based on composite measures, 1997-2004. Am J Prev Med. 2007;32:11–18 [DOI] [PubMed] [Google Scholar]
- 18.US Preventive Services Task Force Screening for colorectal cancer: recommendation and rationale. Ann Intern Med. 2002;137:129–131 [DOI] [PubMed] [Google Scholar]
- 19.Agency for Healthcare Research and Quality (AHRQ) Future Directions for the National Healthcare Quality and Disparities Reports. Available at: http://www.ahrq.gov/research/iomqrdrreport. Accessed May 18, 2012
- 20.Singleton JA, Santibanez T, Wortley P. Influenza and pneumococcal vaccination of adults aged ≥65: racial/ethnic differences. Am J Prev Med. 2005;29(5):412–420 [DOI] [PubMed] [Google Scholar]
- 21.Nolan T, Berwick DM. All-or-none measure raises the bar on performance. JAMA. 2006;295(10):1168–1170 [DOI] [PubMed] [Google Scholar]
- 22.Adams EK, Breen N, Joski PJ. Impact of the National Breast and Cervical Cancer Early Detection Program on mammography and Pap test utilization among white, Hispanic, and African-American women: 1996–2000. Cancer. 2007;109(suppl 2):348–358 [DOI] [PubMed] [Google Scholar]
- 23.Shenson D, Cassarino L, DiMartino Let al. Improving access to mammography through community-based influenza clinics: a quasi-experimental study. Am J Prev Med. 2001;20(2):97–102 [DOI] [PubMed] [Google Scholar]
- 24.Potter MB, Phengrasamy L, Hudes ES, McPhee J, Walsh JM. Offering annual fecal occult blood tests at annual flu shot clinics increases colorectal cancer screening rates. Ann Fam Med. 2009;7:17–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alemi F, Alemagno SA, Goldhagen Jet al. Computer reminders improve on-time immunization rates. Med Care. 1996;34(10, suppl):OS45–OS51 [DOI] [PubMed] [Google Scholar]
- 26.Shenson D, Benson B, Harris A. Expanding the delivery of preventive services through community collaboration: the SPARC model. Prev Chronic Dis. 2008;5(1):A20. [PMC free article] [PubMed] [Google Scholar]
- 27.Frieden TR. A framework for public health action: the health action pyramid. Am J Public Health. 2010;100(4):590–595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shenson D, Quinley J, DiMartino D, Stumpf P, Caldwell M, Lee T. Pneumococcal immunizations at flu clinics: the impact of community-wide outreach. J Community Health. 2001;26(3):191–201 [DOI] [PubMed] [Google Scholar]
- 29.Shenson D, Adams M, Benson W, Clough J. Vote & Vax: Delivering vaccinations at polling places. Poster Presentation. 44th National Immunization Conference. Atlanta, GA. April 20, 2010.
- 30.Musa D, Schulz R, Harris R, Silverman M, Thomas SB. Trust in the health care system and the use of preventive health services by older black and white adults. Am J Public Health. 2009;99:1293–1299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shenson D, DiMartino D, Bolen J, Campbell M, Liu P, Singleton J. Validation of self-reported pneumococcal vaccination in behavioral risk factor surveillance surveys: experience from the SPARC (Sickness Prevention Achieved through Regional Collaboration) program. Vaccine. 2005;23(8):1015–1020 [DOI] [PubMed] [Google Scholar]
- 32.Sudman SN, Bradburn NM. Effects of time and memory factors on response in surveys. J Am Stat Assoc. 1973;68:805–815 [Google Scholar]
- 33.Nelson DE, Bland S, Powell-Griner Eet al. State trends in health risk factors and receipt of clinical preventive services among U.S. adults during the 1990s. JAMA. 2002;287(20):2659–2667 [DOI] [PubMed] [Google Scholar]
- 34.Newell SA, Girgis A, Sanson-Fisher RW, Savolainen NJ. The accuracy of self-reported health behaviors and risk factors relating to cancer and cardiovascular disease in the general population: a critical review. Am J Prev Med. 1999;17(3):211–229 [DOI] [PubMed] [Google Scholar]
- 35.Nelson DE, Holtzman D, Bolen J, Mack KA, Stanwyck CA, Mack KA. Reliability and validity of measures from the Behavioral Risk Factor Surveillance System (BRFSS). Soz Praventivmed. 2001;46(suppl 1):S3–S42 [PubMed] [Google Scholar]
- 36.Hu SS, Balluz L, Battaglia MP, Frankel MR. Improving public health surveillance using a dual-frame survey of landline and cell phone numbers. Am J Epidemiol. 2011;173:703–711 [DOI] [PubMed] [Google Scholar]
- 37.Thornberry OT, Massey JT. Trends in the United States telephone coverage across time and subgroup. : Groves RM, Biemer PP, Lyberg LR, Massey JT, Nichols WL, Telephone Survey Methodology. New York, NY: John Wiley & Sons; 1988:25–49 [Google Scholar]
- 38. US Census Bureau. 2011. Available at: http://www.census.gov/compendia/statab/2011/tables/11s0035.pdf. Accessed May 18, 2012.
- 39.Smith RA, Cokkinides V, von Eschenbach ACet al. American Cancer Society guidelines for the early detection of cancer. CA Cancer J Clin. 2002;52(1):8–22 [DOI] [PubMed] [Google Scholar]