Abstract
Marketing decisions, rather than scientific innovations, have guided the development and positioning of contraceptive products in recent years. I review the stalled progress in contraceptive development in the decades following the advent of the Pill in 1960 and then examine the fine-tuning of the market for oral contraceptives in the 1990s and 2000s. Although birth control has been pitched in the United States as an individual solution, rather than a public health strategy, the purpose of oral contraceptives was understood by manufacturers, physicians, and consumers to be the prevention of pregnancy, a basic health care need for women. Since 1990, the content of that message has changed, reflecting a shift in the drug industry's view of the contraception business. Two factors contributed to bring about this change: first, the industry's move away from research and development in birth control and second, the growth of the class of medications known as lifestyle drugs.
IN MARCH 2011, THE SAN Francisco Chronicle ran a front-page story on contraceptives. It began, “These days, choosing a form of birth control can seem as daunting as shopping for a new laptop computer – the technology is constantly changing and there are just so many options.”1 Even though scores of different brand-name and generic products are available on the American market, a closer inspection of the contraceptive landscape reveals a menu of birth control options that relies on science that is more than 50 years old. Since the Pill was first approved in 1960, birth control continues to work in only one of two ways: by preventing fertilization or by preventing ovulation. The barrier methods—condoms, diaphragms, cervical caps, and chemical spermicides—have existed for the better part of a century (and in the case of condoms, for centuries). The modern intrauterine devices (IUDs) became available in the early 1960s, but they merely improved on a method first introduced in the 1920s. Hormonal contraception—in which synthetic hormones, either progesterone alone or in combination with estrogen, prevent ovulation—was the truly innovative contribution made by the Pill. The newer methods that have come onto the market since 1990—the implant, the shot, the skin patch, and the vaginal ring—simply provide different delivery systems for the hormones to enter the bloodstream.2 Even the technologies behind these delivery systems (e.g., silastic capsules for the implant, transdermal materials for the patch) were developed in the 1960s and 1970s. In the world of contraception, scientific and technological innovation has been moribund for decades.
Why might women need new methods of contraception? A few statistics from 1990 confirm the inadequacy of available methods. An Institute of Medicine study3 of contraception that year reported that almost 3 million unintended pregnancies occurred annually in the United States as the result of contraceptive failure. Half of the 1.5 million abortions in the United States every year were performed to deal with pregnancies resulting from contraceptive failure. One million adolescent girls get pregnant each year. Of women younger than 50 years, 20% had been sterilized, with another 15% married to men who had vasectomies; these people chose to end their fertility rather than deal with contraceptive alternatives, but up to 10% of the women regretted their decision after remarriage or the death of a child.4 Although issues of affordability; cultural constraints; and access to health education, information sources, and contraceptives all influence the effective use of birth control, the physical aspects of existing contraceptive technologies also play a role in women's decisions about whether to use them.
Carl Djerassi, the chemist who first synthesized an orally active progesterone (which made oral hormonal contraception possible), predicted this static state of affairs 40 years ago in a prescient article in Science titled “Birth Control after 1984.”5 In 1989, he revisited the topic of contraceptive research and development in “The Bitter Pill” published in Science.6 He attributed the dearth of innovation to the withdrawal of American pharmaceutical companies from the field. In 1970, 13 major drug firms were actively pursuing birth control research and development (of which nine were American); by 1987, there were only four (with just one located in the United States). Little has changed since then, despite the continued success of the pharmaceutical industry and the expansion of small biotechnology enterprises. Djerassi identified three reasons for “Big Pharma's” flight from contraceptive research: (1) two decades of stringent and burdensome animal toxicology tests required by the US Food and Drug Administration (FDA), which greatly increased the time and expense of developing new products; (2) a negative portrayal of the industry by the media in the wake of Senator Gaylord Nelson's congressional inquiry into the safety of the Pill in 1970 and the Dalkon Shield IUD disaster a few years later; and (3) the increasingly litigious nature of American society, as the courts became the place to seek restitution for injuries or diseases attributed to drugs, medical devices, or other toxic substances. Twenty-two years later, the conclusion Djerassi wrote reads as an accurate reflection of our birth control landscape today:
All we can expect well into the beginning of the 21st century are minor modifications of existing methods: different delivery systems for steroids, possible improvements in sterilization techniques and barrier methods, more precise indications of the safe interval, and possibly a more realistic reconsideration of the IUD option. Such modest developments will extend contraceptive use patterns, but they will not affect our total dependence on conventional 19th and 20th century approaches to birth control.7
What has changed over the past several decades is how contraceptives—specifically, birth control pills—have been marketed. From the 1960s to the 1980s, pharmaceutical companies advertised birth control pills expressly for the purpose of birth control. Initial advertisements to physicians in medical journals (direct-to-consumer advertising was not allowed until the mid-1980s) promoted the novelty of hormonal control of fertility and the newly enlarged role of physicians in family planning; later advertisements focused on the benefits to women in planning when to have children. Pharmaceutical companies never marketed oral contraceptive products as beneficial to public health in the United States; their sales targets were individual physicians who catered to private patients. However, organizations such as the World Health Organization clearly recognized that the Pill was an “essential medicine,” one that met “the priority health care needs of the population” because of its “public health relevance, evidence on efficacy and safety, and comparative cost-effectiveness.”8 Indeed, birth control continued (and continues) to be a basic health care need for women of reproductive age, but pharmaceutical companies have found little incentive for investing in the innovation of new methods.
“Marketing decisions, rather than scientific innovations, have guided the development and positioning of next-generation contraceptive products.”
After largely abandoning these avenues of research, pharmaceutical companies moved their marketing of existing contraceptive products away from the function of fertility control. In the 1990s, manufacturers began to promote their new brands of oral contraceptives to both physicians and consumers explicitly as so-called lifestyle drugs. Lifestyle drugs—the term was coined in 1978—generally describe medications that are designed to improve a person's quality of life by treating less serious conditions; they also have been called cosmetic, life-enhancing, recreational, or discretionary.9 These new advertising campaigns emphasized the secondary effects of oral contraceptives—to treat less-serious conditions such as acne and premenstrual dysphoric disorder and to reduce the frequency of menstruation—rather than the primary indication for the prevention of pregnancy. This shift from control of fertility to control of pimples, moods, and the menstrual cycle indicates that pharmaceutical manufacturers chose to emphasize lifestyle options more than contraception for its own sake. Marketing decisions, rather than scientific innovations, have guided the development and positioning of next-generation contraceptive products in recent years.
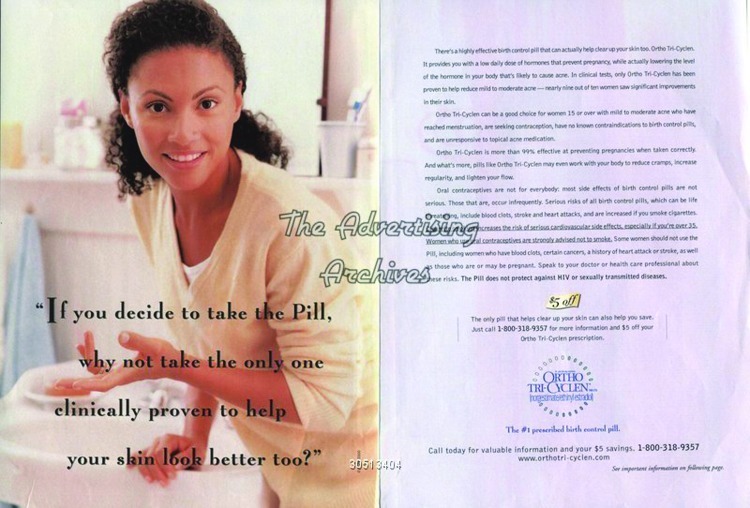
Ortho Tri-Cyclen advertisement.
Source. Image courtesy of the The Advertising Archives.
I review the stalled progress in contraceptive development in the decades following the advent of the Pill and then examine more closely the fine-tuning of the market for oral contraceptives in the 1990s and 2000s. Although birth control has always been pitched in the United States as an individual solution rather than as a public health strategy, the purpose of oral contraceptives was understood by manufacturers, physicians, and consumers to be the prevention of pregnancy, a basic health care need for women of reproductive age. Since 1990, the content of that message has changed, reflecting a shift in the drug industry's perception of the contraception business. This change was brought about by the industry's move away from research and development in birth control and by the growth of the class of medications known as lifestyle drugs; these two trends were influenced by economic, political, and cultural factors, which I discuss later in this article. In the final analysis, the status of contraceptive research and marketing today results from decisions made by the pharmaceutical industry to maximize profits and to minimize risks, decisions that have left women with birth control options that differ little from those available to their grandmothers in the previous century.
THE PRIMACY OF THE PILL
Margaret Sanger recognized the importance of reliable birth control for public health 100 years ago. Fifty years later, her dream of a “magic pill” became a reality when the FDA approved Enovid, the first progestin-estrogen oral contraceptive.10 The birth of the Pill in 1960 dramatically altered the contraceptive landscape for women during its first decades. In 1955, more than half of the American women who used birth control relied on either condoms or a diaphragm. Twenty-seven percent reported using a condom most recently, and 25% reported using a diaphragm. Ten years later, those figures had changed radically. In 1965, five years after the Pill was approved, 27% of American women reported use of the Pill, 18% used condoms, and just 10% relied on a diaphragm. By 1973, more than a third of American women (36%) used the Pill for birth control; only 13.5% reported using condoms, and a mere 3.4% used a diaphragm.11
The first advertisement for the first oral contraceptive, G. D. Searle's Enovid, showed the image of the mythical persona Andromeda breaking free from manacles around her wrist to symbolize the liberation of women from the threat of pregnancy. The copy read,
From the beginning, woman has been a vassal to the temporal demands—and frequently the aberrations—of the cyclic mechanism of her reproductive system. Now to a degree heretofore unknown, she is permitted normalization, enhancement, or suspension of cyclic function and procreative potential. This new physiologic control is symbolized in an illustration borrowed from Greek mythology—Andromeda freed from her chains.12
This advertisement appeared frequently in medical journals such as Obstetrics and Gynecology and JAMA: The Journal of the American Medical Association. Another advertisement for Enovid emphasized the novelty of the use of synthetic progesterone to alter the menstrual cycle: “the first fully feminine molecule for cyclic control of ovulation.”13 These advertisements made clear the revolutionary nature of oral hormonal contraception.
G. D. Searle had waited more than a year after receiving FDA approval to advertise Enovid in the pages of medical journals. The company worried about negative publicity and possible boycotts of its other products because of Roman Catholic opposition to contraception. Its fears were unfounded. When the success of G. D. Searle's Enovid became apparent, other pharmaceutical companies rushed to bring their own oral contraceptive brands to market. By 1970, Ortho, Syntex, Parke-Davis, Eli Lilly, Upjohn, Wyeth, and Mead Johnson had received FDA approval for birth control pills.14 The advertisements for these new pills became lengthier and glossier. Parke-Davis introduced Norlestrin with a three-page spread; Syntex's announcement of its product, Norinyl, occupied a full eight pages in Obstetrics and Gynecology.15 The Ortho Pharmaceutical Company touted the superiority of Ortho-Novum's package design; the “Dialpak” helped remind patients to take the pills daily.16 As the market became more crowded, each company sought to promote distinctive aspects of what were essentially similar products. These tactics were not unique to the realm of oral contraceptives; they were characteristic of the whole pharmaceutical enterprise, as companies increasingly produced slight variations on one another's products, what would later be described as “me-too” drugs.
Although oral contraceptives were technically marketed only to physicians, consumers were deluged with information about the new pills in newspaper and magazine articles. As Jeremy Greene and David Herzberg have shown, drug companies employed public relations firms to ensure popular coverage of the latest prescription-only medications.17 In the decades before direct-to-consumer advertising, American women received ample exposure to news about this contraceptive breakthrough, and they went to their physicians to ask for prescriptions for the Pill. By the late 1960s, almost nine million American women were taking oral contraceptives to prevent pregnancy.
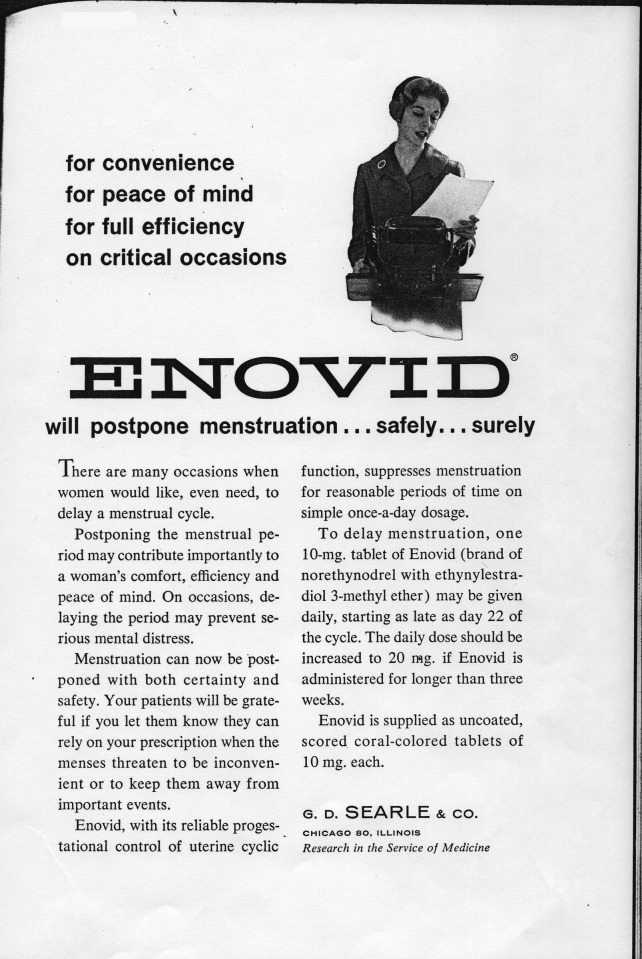
Enovid advertisement.
Source. Obstetrics and Gynecology 16 (November 1960).
Eager to capitalize on the success of hormonal contraception, researchers and birth control advocates sought other ways to deliver the hormones into women's bodies. The subdermal implant was one such adaptation. It was designed for users who could not or would not remember to take a daily pill, who did not want to be permanently sterilized, and who were unsuitable candidates for the IUD. Although the implant was not formally approved for use in the United States until 1990, research on this method began in the 1960s in the laboratories of the Population Council, a private nonprofit organization with an international focus on population and related concerns. The contraceptive shot was another new delivery form that was first developed by Schering AG. One injection provided three months of protection against pregnancy. In the United States, Upjohn applied for approval of its version, Depo-Provera, in the late 1960s. Like Norplant, which was marketed by Wyeth, Depo did not receive FDA approval until many years later, in 1992. However, in the 1960s, these developments, together with the IUD, which had been reintroduced into the American market earlier in the decade, seemed to promise further innovation in the realm of reversible contraception.
By the late 1980s, however, it was clear that this promise had not been realized. Along with Djerassi's “Bitter Pill” article came several other publications lamenting the deceleration in contraceptive innovation. A 1988 article in Family Planning Perspectives asked, “Whatever Happened to the Contraceptive Revolution?”18 A series of meetings held by the National Academy of Science resulted in a 1990 book called Developing New Contraceptives: Obstacles and Opportunities, which focused more on obstacles than on opportunities.19 In 1995, the editor of Family Planning Perspectives, Michael Klitsch, summarized the stasis in contraceptive research in an article titled “Still Waiting for the Contraceptive Revolution.”20
Klitsch reviewed the factors that others had identified as contributing causes of the slowdown. First, he noted the chilling effect of product liability costs, resulting from both individual and class action lawsuits against contraceptive manufacturers. Second, he pointed to the financial burden of increased government regulation of contraceptive products because the FDA required more stringent testing of experimental methods in animals and humans. Third, he enumerated several reasons for changes in public opinions about contraceptives. The enthusiasm over the Pill in the early 1960s had given way to concern about its side effects by the end of that decade, intensified by media coverage of these adverse health effects. Klitsch attributed greater public scrutiny of and skepticism toward contraceptives in the 1970s (especially those pharmaceuticals and devices available by prescription only) to the growing influence of the consumer movement and the women's movement. Although other drug classes also encountered these challenges, contraceptives faced the additional burden of morally freighted debates over their use. The political dimension of American attitudes toward contraception was further complicated in the 1980s by the emergence of HIV and AIDS, against which only barrier methods offered any protection, and by the increasingly acrimonious abortion conflict, which swept contraceptives into its maelstrom. Collectively, these factors thwarted enthusiasm for exploring novel approaches to preventing pregnancy. Finally, Klitsch reported that the pharmaceutical industry saw limited opportunities for growth (and profits) in the contraceptive sector of developed countries because the market was already saturated with existing products. Companies feared that new contraceptives would not attract enough new users to be profitable or that they might eat into the profits of their products already on the market. The safer bet was to stick with current product lines, tinkering here and there with the formulations but not making any major innovations.
Thus, tinkering is precisely what the major manufacturers did in the 1970s and 1980s. The progestin component had already been lowered in the 1960s from the initial strength of 10 milligrams to one milligram per pill. In response to studies that showed the risk of blood clotting in women who took oral contraceptives could be reduced with a lower dose of estrogen, manufacturers decreased the estrogen component from 80 to 100 micrograms to 50 micrograms and then even further to 35 micrograms. In the mid-1960s, several companies introduced sequential oral contraceptives, which required women to take estrogen-only pills for 14 days and then estrogen-progestin combination pills for six to seven days (followed, as usual, by seven days of placebo or no pills, to allow for a menstrual period). Within a few years, this regimen was found to increase the risk of uterine cancer, and these formulations were taken off the American market in the mid-1970s.21 In the 1980s, the multiphasics were introduced; with these brands, women took a series of two or three different estrogen-progestin combination pills (e.g., Ortho-Novum 7/7/7 was taken as follows: seven days of 0.5 mg progestin and 35 μg estrogen, then seven days of 0.75 mg progestin and 35 μg estrogen, then seven days of 1.0 mg progestin and 35 μg estrogen) to more closely mimic the cyclical fluctuations of sex hormones in a woman's body. All of these formulations were variations on the original birth control pill introduced in 1960: 21 days of oral tablets containing one of a half-dozen different synthetic progestins in combination with one of two synthetic estrogens.
Meanwhile, nonprofit organizations undertook much of the research, development, and testing of alternative delivery systems for hormonal contraception. The Population Council experimented with a vaginal ring for sustained release of hormones. It also managed the testing of implants in countries such as Chile, Finland, Denmark, Brazil, Jamaica, and the Dominican Republic prior to FDA approval. Only after the testing was complete and the Population Council's application for FDA approval was successful did Wyeth-Ayerst agree to market Norplant in the United States. Similarly, the World Health Organization coordinated multicenter studies of Depo-Provera, which then formed the basis for Upjohn's renewed appeal for FDA approval, awarded in 1992.
The World Health Organization also took the lead in pursuing a hormonal contraceptive for men. Beginning in the 1970s, the World Health Organization sponsored a worldwide network of chemical laboratories, located mainly in developing nations, to research male methods and later organized large multisite clinical trials to test the most promising of these methods. Pharmaceutical companies stayed away from male hormonal contraception until the late 1990s, when a few—most notably, the Dutch firm Organon—began to express interest.22 As we know, however, no male pill has yet come to fruition; one researcher noted recently, “The joke in the field is: The male pill's been five to 10 years away for the last 30 years.”23
In the case of Norplant, and perhaps the other long-acting contraceptive methods, the Population Council applied for FDA approval not to market Norplant in the United States but rather so that the State Department's Agency for International Development could make it available to population control programs in developing nations. Wyeth was licensed as the American distributor of Norplant, hoping to broaden its presence in the domestic contraceptive marketplace. Wyeth was already in the business of selling birth control, with several different Pill formulations, but it had relatively low expectations for Norplant in 1990, predicting that the implant would capture an additional one to two percent of the private sector and three to five percent of the public sector in total contraceptive sales.24
Seasonale advertisement.
Source. Obstetrics and Gynecology 102 (December 2003).
Indeed, Norplant never attracted more than two percent of American contraceptive users and for various reasons was taken off the market after just one decade. The other delivery methods also did not garner a significant segment of those using contraceptives.25 By 2008, just 3.2% used the injectable Depo-Provera (sold by Pfizer), 2.4% used a vaginal ring (Merck's Nuvaring), and a total of 1.1% used the patch (Ortho-McNeil's Ortho Evra) or the implant (Schering-Plough introduced Implanon in the United States in 2006). IUDs are used by 5.5%, just a fraction higher than the 5.2% who report relying on withdrawal as their primary means of contraception. The top of the contraceptive chart continues to be dominated by sterilization (27% of women had undergone tubal ligation, and 10% of their male partners had undergone vasectomies) and the Pill (28%), with condoms well behind in third place (16%).26
Condoms have become more popular since the advent of AIDS and HIV in the 1980s as the most effective way to prevent the transmission of disease, but they remain less effective than hormonal methods in preventing pregnancy. Some 13.5% of women reported using condoms in combination with another method to ensure against both pregnancy and sexually transmitted infections. Sterilization as a form of irreversible contraception began to rise in popularity in the 1970s in the wake of concerns about the safety of both oral contraceptives and IUDs and since the 1980s has remained the most common form of birth control in America.27 However, the Pill still reigns as the most widely used reversible type of contraception.
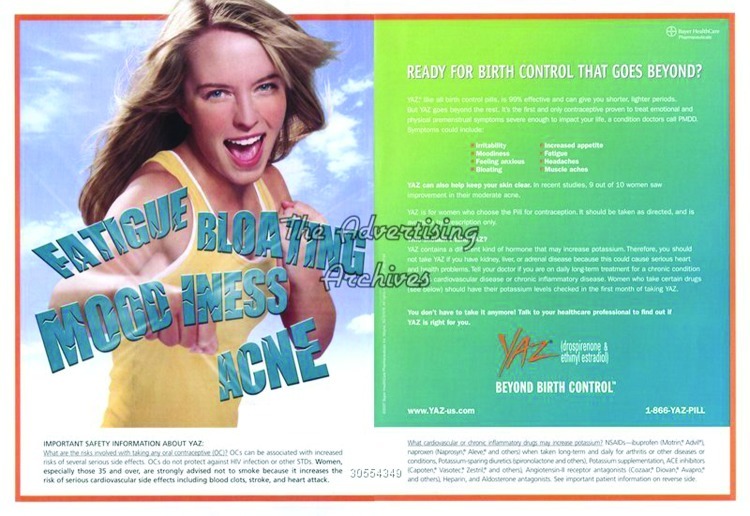
Yaz advertisement.
Source. Image courtesy of The Advertising Archives.
PROMOTING THE PILL ANEW
In recent decades, one trend in the marketing of birth control pills was the great expansion of the oral contraceptive marketplace. A dramatic increase in the number of different birth control pills available in the United States resulted from the Drug Price Competition and Patent Term Restoration Act of 1984, also known as the “Hatch-Waxman Act,” which set up the modern system of generic drug approval and regulation. By 2007, more than 90 brand-name and generic oral contraceptive products were on the market in the United States.28 Physicians, pharmacists, and women could choose pills based on price because the action of these contraceptives, or their therapeutic equivalence, was essentially the same.29 Brand-name manufacturers had to find a way to make their products stand out from the generic crowd.
One tactic was to develop alternative forms of synthetic progesterone. A so-called third generation was developed in the early 1980s. Following the first-generation molecules, norethynodrel (used in G. D. Searle's Enovid) and norethindrone (used in Syntex's Norinyl and Ortho's Ortho-Novum), and the second-generation molecules, such as levonorgestrel (used in Norplant as well as in oral contraceptives), these compounds had high progestational activity and lower androgenic activity. The high progestational activity meant that lower doses could be used; the lower androgenic activity meant fewer side effects, such as hirsutism and acne, that sometimes accompanied the older synthetic progestins. Desogestrel, for example, was tested and approved for use in Europe in the 1980s; it became available in the United States in 1992, in the form of Organon's Desogen and Ortho-McNeil's Ortho-Cept.30 That same year, Ortho-McNeil also released Ortho Tri-Cyclen, which used norgestimate. Like desogestrel, norgestimate was described as a third-generation progestin, and, like desogestrel, it had lower androgenic activity than other progestins. Ortho used this lower androgenic activity as the basis for its application to the FDA for approval of Ortho Tri-Cyclen for the treatment of acne. Although physicians had been prescribing oral contraceptives off-label for acne treatment since the 1960s, Ortho Tri-Cyclen was the first to get formal FDA approval for this indication, in addition to its approved use in pregnancy prevention. Thus, a second tactic used by brand-name manufacturers was to expand the approved indications for certain oral contraceptives.
A third tactic rebranded oral contraceptives as drugs to suppress monthly menstruation. In 2003, DuraMed, a subsidiary of Barr Pharmaceuticals, received FDA approval to market Seasonale, the first extended-cycle oral contraceptive. Seasonale was designed to be taken in three-month cycles, instead of the usual three-week cycles of other formulations, thus reducing the number of bleeding periods from 12 to four per year.31 As in the case of acne, the knowledge that taking oral contraceptives continually would eliminate monthly periods was not new. In fact, the first advertisement for Enovid in 1960 promoted it not for contraceptive purposes but rather to postpone menstruation “for convenience, for peace of mind, for full efficiency on critical occasions.”32 Even the advertisements that finally did promote Enovid for contraception also made mention of menstrual suppression. Consider the text of the Andromeda advertisement referenced earlier:
From the beginning, woman has been a vassal to the temporal demands—and frequently the aberrations—of the cyclic mechanism of her reproductive system. Now to a degree heretofore unknown, she is permitted normalization, enhancement, or suspension of cyclic function [emphasis added] and procreative potential.33
In 2003, Barr formalized this indication. After receiving FDA approval, the company created specialized packaging for Seasonale that incorporated three months’ worth of pills into a single dispenser. It developed a promotional campaign that targeted physicians with sales visits, educational materials, and sample kits and a parallel campaign that targeted women with direct-to-consumer advertising in magazines and on television and the Internet.34
The most recent expansion in indications for oral contraceptives has been Bayer's successful petition in 2006 to market its Yaz brand as a treatment for premenstrual dysphoric disorder and acne. Yaz has yet another synthetic form of progesterone, drosperinone, which was initially approved in 2001 for Bayer's Yasmin brand. Bayer's brands have been extraordinarily successful; in 2006, Yasmin owned 17% of the global sales of oral contraceptives.35 In 2009, Yaz was the best-selling oral contraceptive on the American market. Moreover, it was the 21st best-seller among all prescription drugs in terms of number of prescriptions filled (almost 10 million), and it ranked 50 overall in terms of retail sales ($700 million).36
Manufacturers aggressively marketed these new uses for oral contraceptives (acne treatment, premenstrual dysphoric disorder treatment, and menstrual suppression) directly to consumers, thanks to the permission granted for pharmaceutical advertising in print media in the mid-1980s and the extension of that advertising to television in 1997. Of course, direct-to-consumer advertising only expanded the ways in which consumers could get information about prescription drugs. Indeed, consumers have been actively engaged in selecting their own medications for centuries. In the modern era—after the Durham-Humphrey Amendment to the Food, Drug, and Cosmetic Act established the category of prescription-only drugs in the United States in 1951—access to drugs became more restricted. Nevertheless, public relations efforts, as discussed earlier, ensured that consumers were made aware of the latest pharmaceutical products available from the local pharmacy with a prescription from a physician. The oral contraceptive is an excellent example of such a prescription drug, and the practice of women going to their physicians and asking for the Pill to prevent pregnancy dates to the early 1960s.
The advertising of oral contraceptives for their secondary effects that began in the 1990s raises the question of whether the pharmaceutical industry is now marketing birth control pills as lifestyle drugs, a term that became a full-fledged member of the scientific and popular lexicon in 1998. A study of English-language uses of the terms lifestyle drugs and lifestyle medicines found only a few dozen mentions per year in the scientific literature (as indexed by MEDLINE, Embase, and PubMed) and the popular literature (as indexed by LexisNexis) before 1998; that year, the number shot up to more than 400. From 1998 to August 2003, the terms appeared some 2600 times.37
It seems inaccurate, and anachronistic, to describe the birth control pill as the first lifestyle drug, as some historians have suggested.38 Although it was the first prescription medication meant to be taken by healthy people, this categorization diminishes the significance of oral contraceptives in meeting a critical and basic health need for both individuals and populations—namely, the need for a reliable and effective method for preventing pregnancy. However, in the more recent marketing of oral contraceptives, do these new indications fit the description of a lifestyle drug?
“The advertising of oral contraceptives for their secondary effects that began in the 1990s raises the question of whether the pharmaceutical industry is now marketing birth control pills as lifestyle drugs, a term that became a full-fledged member of the scientific and popular lexicon in 1998.”
Part of the problem in making this assessment is the vagueness of the concept of lifestyle drugs. No single definition exists, although there seems to be some consensus on the broad contours of the category, if not on the specific drugs and indications within that classification. The authors of a piece in the British Medical Journal in 2000 provided this working description:
a lifestyle drug is one used for ‘non-health’ problems or for problems that lie at the margins of health and well-being… . A wider definition would include drugs that are used for health problems that might be better treated by a change in lifestyle.39
Joel Lexchin, an associate professor in family and community medicine at the University of Toronto, concurred in a commentary in the Canadian Medical Association Journal. He proposed that lifestyle drugs fell into two groups: “any drug intended or used for a problem that falls into the border zone between the medical and social definitions of health” and “those intended to treat diseases that result from a person's lifestyle choices.”40 A Nature Medicine writer offered a vague description illustrated with examples: lifestyle drugs were “medicines that treat conditions associated with lifestyle such as weight-loss tablets, anti-smoking agents, impotence therapies and hair restorers.”41 Most commentators agree that the definition is variable, depending on the patient and the context in which he or she is experiencing a given condition for which a drug product might be prescribed. In the 2000s, most also agreed that the issue was not merely one of semantics but also associated with serious financial implications as managed care and third-party payers debated whether to pay for certain drug classes.
Given these definitions, it would be hard to argue that oral contraceptives taken solely for the purpose of controlling fertility should be considered lifestyle drugs. Birth control pills are not cosmetic, enhancing, recreational, or discretionary but confer a significant health benefit (the avoidance of pregnancy) on their users. However, the secondary effects for which some brands are promoted can fit the lifestyle characterization. Acne, periodic moodiness, and monthly bleeding are common conditions that constitute inconveniences, unpleasantness, and varying degrees of suffering, but they are not life threatening or wholly debilitating.
The newest brands of birth control pills are not being marketed solely for the primary indication of family planning. For example, advertisements for Seasonale and its more recent iteration, Seasonique, promote freedom from menstruation, not freedom from pregnancy.42 Yaz's slogan, “Beyond Birth Control,” signaled that its real purpose was to deal with the miseries resulting from menstruation, such as headaches, irritability, and pimples.43 Pharmaceutical manufacturers are not selling contraception per se as a lifestyle option; rather, they pitch menstruation as an annoying condition to be ameliorated by their products. The emphasis on secondary effects instead of the primary indication in advertisements represents an attempt to differentiate products in a crowded field because no one brand can claim superior efficacy in the prevention of pregnancy.44 When the contraceptive aspect takes a back seat, the Pill appears to be a veritable lifestyle drug.
As a result, oral contraceptives have found themselves on lists of lifestyle drugs, along with antidepressants and treatments for erectile dysfunction, smoking addiction, obesity, wrinkles, and male pattern balding.45 This shift in image has economic implications: for example, BlueChoice HealthPlan of South Carolina included several brands of oral contraceptives on its “2011 Lifestyle Medication List” of drugs not covered under the plan's pharmacy benefit.46
Note that Bayer's “beyond birth control” claims for Yaz have not gone unchallenged. In 2009, the FDA objected to the misleading nature of Yaz television commercials and forced Bayer to run a revised $20 million advertising campaign as a corrective.47 Yaz is also the subject of thousands of lawsuits filed by women who experienced adverse health effects. Its synthetic progesterone and its indications may be different from those of earlier oral contraceptives, but this kind of litigation is not new. Since the 1960s, women have turned to the courts to seek restitution for injuries or diseases they believed were caused by hormonal contraceptives, including not only the oral pills but also the subdermal implants, skin patches, and vaginal rings. Recall that the increasingly litigious nature of American society was one of the reasons cited by Carl Djerassi to explain why the pharmaceutical industry moved away from contraceptive research and development in the 1980s.
The trend to sue for damages in courts of law has not been limited to hormonal contraceptives. More than 4000 lawsuits were brought against A. H. Robins, the manufacturer of the Dalkon Shield IUD, which led that company to file for bankruptcy in 1985 and three other companies to take their IUDs off the American market.47 In 1986, a woman won a $5.1 million lawsuit against Ortho Pharmaceutical for her claim that its contraceptive jelly product caused deformities in her infant.49 In the 1990s, some 50 000 women had joined class action lawsuits against Norplant.50 American Home Products, Wyeth's parent company, eventually settled the largest suit for a modest $54 million, but just two months later, it cost the same company $3.75 billion to settle the lawsuits over fenfluramine/phentermine, the diet pill combination that caused heart valve damage in users.51 Around the same time, more than 19 000 individuals filed lawsuits against Dow Corning and other manufacturers of silicone breast implants. A class action suit resulted in a settlement that set aside $4.25 billion for claimants around the world.52 Pharmaceuticals and medical devices designed for long-term use, such as contraceptives, or for cosmetic purposes, such as breast implants, are particularly susceptible to consumer lawsuits.
Today, women looking to join suits against Yaz as potential claimants can easily find information at Web sites such as http://www.yaz-side-effects-lawyer.com, http://www.yaz-yasmin-lawsuit.com, and http://yazlawsuit-info.com. Similar sites exist for those women seeking to file claims against the birth control patch, Ortho-Evra. These lawsuits represent women's dissatisfaction with existing methods of contraception. This dissatisfaction suggests that birth control might have something in common with another “feminine technology”: brassieres. According to historian of technology Judith McGaw, when women are asked about their bra decisions, they “talk in terms of making the best of a limited array of choices or finding something less unsatisfactory than their previous choice.”53 In similar fashion, women make the best of the limited array of contraceptives and choose the one that is least unsatisfactory. Pharmaceutical companies have been content with this status quo, offering women small lifestyle add-ons to basically the same old oral contraceptives, seeking to maximize profits and minimize losses rather than to develop true innovations in birth control. Therefore, for the past 50 years, the Pill has retained the dubious honor of being the least unsatisfactory choice in contraception for American women.
Acknowledgments
I thank Carl Djerassi, Jeremy Greene, Lara Marks, and the three anonymous reviewers from the American Journal of Public Health for their comments on previous drafts of this article.
Endnotes
- 1. Erin Allday, “Shots, Patches among Alternatives to the Pill,” San Francisco Chronicle, March 15, 2011.
- 2. For historical studies of the implant and the shot, see Elizabeth Siegel Watkins, “From Breakthrough to Bust: The Brief Life of Norplant, the Contraceptive Implant,” Journal of Women's History 22 (Fall 2010): 88–111; Elizabeth Siegel Watkins, “The Social Construction of a Contraceptive Technology: An Investigation of the Meanings of Norplant,” Science, Technology, and Human Values 36 (2011): 33–54; and Wendy Kline, “Bodies of Evidence: Activists, Patients, and the FDA Regulation of Depo-Provera,” Journal of Women's History 22 (Fall 2010): 64–87. To date, there have been no historical studies of the patch or the ring; however, scores of articles are available in the medical literature on these two methods (and hundreds of articles on contraceptive implants and shots, the two older methods). For recent news articles on the patch and the ring, see The implant initially consisted of six silicone rods implanted in a woman's arm that slowly released a synthetic form of the hormone progesterone over a five-year period; the versions currently available consist of one or two rods. The shot is an intramuscular injection of synthetic progesterone administered every 90 days. The patch is a transdermal patch applied to the skin that gradually releases synthetic progesterone and estrogen; a new patch is applied weekly for three of every four weeks. The ring is a flexible plastic ring that slowly releases synthetic progesterone and estrogen; it is inserted into the vagina and left in place for three weeks. “FDA Panel Backs Benefit of Birth Control Patch Despite Risks,” USA Today, December 9, 2011, http://yourlife.usatoday.com/health/medical/womenshealth/story/2011-12-09/FDA-panel-backs-benefit-of-birth-control-patch-despite-risks/51769232/1 (accessed January 4, 2012); and Jim Edwards, “At Merck, an Undercover Video and 40 Deaths Plague Nuvaring Birth Control Brand,” CBS News, April 19, 2011, http://www.cbsnews.com/8301-505123_162-42848006/at-merck-an-undercover-video-and-40-deaths-plague-nuvaring-birth-control-brand/?tag=bnetdomain (accessed January 4, 2012)
- 3. Luigi Mastroianni Jr, Peter J. Donaldson, and Thomas T. Kane, eds., Developing New Contraceptives: Obstacles and Opportunities (Washington, DC: National Academy Press, 1990) [PubMed]
- 4. Teri Randall, “United States Loses Lead in Contraceptive Choices, R&D; Changes in Tort Liability, FDA Review Urged,” JAMA: The Journal of the American Medical Association 268 (1992): 176–7. [DOI] [PubMed]
- 5. Carl Djerassi, “Birth Control after 1984,” Science 169 (1970): 941–51. [DOI] [PubMed]
- 6. Carl Djerassi, “The Bitter Pill,” Science 245 (1989): 356–61. [DOI] [PubMed]
- 7. Ibid., 360.
- 8. World Health Organization, “Essential Medicines,” http://www.who.int/topics/essential_medicines/en (accessed September 19, 2011)
- 9. Claus Møldrup, “The Use of the Terms ‘Lifestyle Medicines’ or ‘Lifestyle Drugs,’” Pharmacy World & Science: PWS 26, no. 4 (2004): 193–6. [DOI] [PubMed]
- 10. Elizabeth Siegel Watkins, On the Pill: A Social History of Oral Contraceptives, 1950-1970 (Baltimore, MD: Johns Hopkins University Press, 1998), 14, 141.
- 11. Ibid., 61–2; Leslie Aldredge Westoff and Charles F. Westoff, From Now to Zero: Fertility, Contraception and Abortion in America (Boston, MA: Little, Brown, 1968), 64; Christine A. Bachrach, “Contraceptive Practice among American Women, 1973-1982,” Family Planning Perspectives 16, no. 6 (1984): 253–9. [PubMed]
- 12. Obstetrics and Gynecology 18 (1961): 62–3.
- 13. Obstetrics and Gynecology 19 (1962): 114–5.
- 14. Suzanne White Junod, “Women Over 35 Who Smoke: A Case Study in Risk Management and Risk Communications, 1960-1989,” in Medicating Modern America: Prescription Drugs in History, eds. Andrea Tone and Elizabeth Siegel Watkins. (New York: NYU Press, 2007), 117–9.
- 15. Obstetrics and Gynecology 23 (1964)
- 16. Obstetrics and Gynecology 21 (February 1963). For more on the Dialpak, see Patricia Peck Gossel, “Packaging the Pill,” in Manifesting Medicine: Bodies and Machines, ed. Robert Bud. (New York: Taylor & Francis, 1999), 105–21.
- 17. Jeremy A. Greene and David Herzberg, “Hidden in Plain Sight: Marketing Prescription Drugs to Consumers in the Twentieth Century,” American Journal of Public Health 100 (2010): 793–803. [DOI] [PMC free article] [PubMed]
- 18. Richard Lincoln and Lisa Kaeser, “Whatever Happened to the Contraceptive Revolution?,” Family Planning Perspectives 20 (1988): 20–4. [PubMed]
- 19. Mastroianni Jr, Developing New Contraceptives.
- 20. Michael Klitsch, “Still Waiting for the Contraceptive Revolution,” Family Planning Perspectives 27 (1995): 246–53. [PubMed]
- 21. Junod, “Women Over 35 Who Smoke,” 106.
- 22. Nelly Oudshoorn, The Male Pill: A Biography of a Technology in the Making (Durham, NC: Duke University Press, 2003)
- 23. Dr. John Amory, quoted in Elizabeth Landau, “Where's the Male Birth Control Pill?” CNN Health, May 7, 2010, http://articles.cnn.com/2010-05-07/health/future.contraceptives.male.pill_1_sperm-production-male-birth-control-pill-progestin?_s=PM: HEALTH (accessed May 18, 2011)
- 24. Watkins, “From Breakthrough to Bust,” 91–2.
- 25.Watkins, “From Breakthrough to Bust,” and Watkins, “The Social Con struction of a Contraceptive Technology.”
- 26. Guttmacher Institute, “Facts on Contraceptive Use in the United States” (June 2010), http://www.guttmacher.org/pubs/fb_contr_use.html (accessed May 18, 2011). Historian Lara Marks reports that there were 430 brands of oral contraceptives worldwide in 1992. See Lara V. Marks, Sexual Chemistry: A History of the Contraceptive Pill (New Haven, CT: Yale University Press, 2001), 77.
- 27. Rebecca M. Kluchin, Fit to Be Tied: Sterilization and Reproductive Rights in America, 1950-1980 (New Brunswick, NJ: Rutgers University Press, 2009)
- 28. American College of Obstetricians and Gynecologists, “ACOG Committee Opinion No. 375: Brand Versus Generic Oral Contraceptives,” Obstetrics and Gynecology 110 (2007): 447–8. [DOI] [PubMed]
- 29. Daniel Carpenter and Dominique A. Tobbell, “Bioequivalence: The Regulatory Career of a Pharmaceutical Concept,” Bulletin of the History of Medicine 85, no. 1 (2011): 93–131. [DOI] [PubMed]
- 30. Information about drug formulations and FDA approval dates for new drugs can be found at the Drugs@FDA Web site, http://www.accessdata.fda.gov/scripts/cder/drugsatfda (accessed May 18, 2011)
- 31. Laura Mamo and Jennifer Ruth Fosket, “Scripting the Body: Pharmaceuticals and the (Re)Making of Menstruation,” Signs: Journal of Women in Culture and Society 34 (2009): 925–49.
- 32. Watkins, On the Pill, 37.
- 33. Obstetrics and Gynecology 18 (1961): 62–3.
- 34. Barr Pharmaceuticals Inc, “Annual Report” (June 30, 2004), 13, http://www.secinfo.com/dsvr4.19rf.htm (accessed May 18, 2011). For an interesting discussion of the “naturalness” of menstrual suppression, see Lara Marks, “Preface to the Paperback Edition,” in Sexual Chemistry: A History of the Contraceptive Pill (New Haven, CT: Yale University Press, 2010), xxiv.
- 35. Business Insights, “Lifestyle Drugs Market Outlook” (December 2007), http://www.hcmarketplace.com/supplemental/6392_sampleissue.pdf (accessed May 18, 2011)
- 36. “Top 200 Drugs for 2009 by Units Sold,” http://www.drugs.com/top200_units.html (accessed May 18, 2011); “Top 200 Drugs for 2009 by Sales,” http://www.drugs.com/top200.html (accessed May 18, 2011)
- 37. Møldrup, “The Use of the Terms ‘Lifestyle Medicines’ or ‘Lifestyle Drugs,’ ” 193–6. [DOI] [PubMed]
- See, for example, Suzanne White Junod and Lara Marks, “Women's Trials: The Approval of the First Oral Contraceptive Pill in the United States and Great Britain,” Journal of the History of Medicine and Allied Sciences 57, no. 2 (2002): 117–60. [DOI] [PubMed]
- 39. David Gilbert, Tom Walley, and Bill New, “Lifestyle Medicines,” British Medical Journal 321 (2000): 1341–4, quote on 1341. [DOI] [PMC free article] [PubMed]
- 40. Joel Lexchin, “Lifestyle Drugs: Issues for Debate,” Canadian Medical Association Journal 164 (2001): 1449–51, quote on 1449. [PMC free article] [PubMed]
- 41. Tim Atkinson, “Lifestyle Drug Market Booming,” Nature Medicine 8, no. 9 (2002): 909. [DOI] [PubMed]
- 42. Mamo and Fosket, “Scripting the Body,” 937.
- 43. Natasha Singer, “A Birth Control Pill that Promised Too Much,” New York Times, February 11, 2009.
- 44. I am grateful to Jeremy A. Greene for sharing his insight on primary versus secondary effects in the marketing of the Pill.
- 45. Johns Hopkins Medicine, “Health Alerts: What Is a Lifestyle Drug?,” http://www.johnshopkinshealthalerts.com/alerts/prescription_drugs/JohnsHopkinsPrescriptionDrugsHealthAlert_3241-1.html (accessed May 18, 2011)
- 46. BlueChoice HealthPlan, “2011 Lifestyle Medication List.” BlueChoice HealthPlan, South Carolina, http://www.bluechoicesc.com/./bluechoice/./lifestyle-medications.pdf (accessed May 9, 2012)
- 47.Singer, “A Birth Control Pill that Promised Too Much.”
- 48. Randall, “United States Loses Lead in Contraceptive Choices,” 176–8. [DOI] [PubMed]
- 49. Ibid., 178.
- 50. “Citizen's Petition Before the FDA Requesting Withdrawal for Sale of Norplant” (June 27, 1996). Docket #96P-0215, Records of the US Food and Drug Administration, Rockville, MD. See also Cynthia M. Klaisle and Philip D. Darney, “From Launch to Litigation: Norplant in America,” Contraception 11 (2000): 595.
- 51. David J. Morrow, “Fen-Phen Maker to Pay Billions in Settlement of Diet-Injury Cases,” New York Times, October 8, 1999, A1.
- 52. For a scholarly analysis of the effect and meaning of the breast implant litigation, see Sheila Jasanoff, “Science and the Statistical Victim: Modernizing Knowledge in Breast Implant Litigation,” Social Studies of Science 32 (2002): 37–69. For a more popular treatment, see Marcia Angell, Science on Trial: The Clash of Medical Evidence and the Law in the Breast Implant Case (New York: WW Norton, 1997) [DOI] [PubMed]
- 53. Judith A. McGaw, “Why Feminine Technologies Matter,” in Gender & Technology: A Reader, eds. N. E. Lerman, R. Oldenziel, and A. P. Mohun (Baltimore, MD: Johns Hopkins University Press, 2003), 13–36, quote on 19.