Abstract
Objective
HIV-related stigma has been shown to impede HIV-antibody testing and safer sexual practices in adults. Less is known about the effects of stigma on group-based prevention programs among at-risk youth. This study examined the longitudinal relationships between HIV-related stigma and gains in HIV-knowledge.
Methods
Data were provided by 1654 African-American adolescents who participated in a large multi-city prevention trial (Project iMPACCS). Participants were randomly assigned to an empirically-validated skill-based intervention (Focus on Youth) or a general health promotion control group. Both stigma and knowledge were assessed at pre- and post-intervention assessments.
Results
Results from a covariance model suggested that adolescents participating in FOY showed improvements in HIV-knowledge and decreases in HIV-related stigma when compared to controls. The treatment effect on HIV-related stigma was comprised of a direct effect and an indirect effect through change in HIV knowledge. After controlling for baseline associations between HIV-related stigma and HIV knowledge, higher baseline stigma was shown to reduce gains in knowledge in both the treatment and control groups.
Conclusions
Results suggest that HIV-stigma can interfere with how youth identify with and internalize messages from group-based prevention trials.
Keywords: HIV, Stigma, Adolescence, Knowledge, Prevention
INTRODUCTION
HIV-related stigma has been cited as a prominent and persistent barrier to care and prevention efforts (1–4). For individuals who are unaware of their HIV status, stigma has been shown to interfere with preventative behaviors such as routine HIV screening and safer sexual practices (1,2,5,6). It is thought that stigma hinders these behaviors because non-infected individuals seek to emotionally, cognitively and behaviorally distance themselves from HIV and people living with HIV, resulting in an underestimation of their personal susceptibility to infection (7,8).
Stigma may also interfere with the efficacy of group-based educational programs for at-risk youth. Similar to adults, youth who hold more stigmatizing beliefs about HIV may be less likely to identify with infected youth or those whom they perceive as being at risk for infection (9,10). Because they do not identify with the risk group, youth with elevated stigma may feel that they will not become infected and may be less likely to internalize and apply the skills and information presented in interventions. Relatively little is known about reducing stigma in uninfected youth or about how, or if, stigma might interfere with the effectiveness of group-based HIV prevention programs (11,12).
One mechanism through which stigma might interfere with prevention efforts is through its relationship with HIV knowledge. Knowledge and stigma are related (11,13,14) yet the nature of their relationship is unclear. Results from a number of intervention trials designed to reduce stigma among infected individuals have shown that providing HIV knowledge helps to reduce stigma (3,13,15,16), suggesting that changes in knowledge may lead to changes in stigma. There is evidence, however, that purely didactic HIV prevention approaches compared to interventions that combine knowledge with counseling or skill-based interventions (e.g., CBT, coping-skills) are less effective in reduce stigma (15). It is not clear why combination programs outperform information-only interventions, but this consistent finding suggests the relationship between HIV knowledge and stigma involves more than a unidirectional relationship linking decreased stigma with increased knowledge. To our knowledge, no study has tested the bidirectional relationships between HIV-related knowledge and HIV-related stigma.
For this study, we used data from a multi-city sample of African-American youth to examine the relationships among HIV-related stigma, knowledge of HIV, and participation in a validated group-based HIV prevention intervention [Focus on Youth (FOY); 17] or a general-health promotion group that included information about HIV[Promoting Health among Teens (PHAT)]. FOY is a knowledge- and skill-based small-group intervention designed in collaboration with community organizations to be delivered in community settings. FOY is designed to help youth identify HIV risk exposure in their communities, anticipate and prepare for risky situations, and reduce risky activities. Although the FOY did not directly target stigma, it provided knowledge, skills training, and self-efficacy enhancement in a small-group setting; thus, we expected FOY to increase HIV knowledge and reduce HIV-related stigma. Additionally, we expected that changes in knowledge would account for some, but not all, of the intervention’s effect on stigma.
Beyond expecting more change in the FOY group for knowledge and stigma, we expected that higher levels of stigma at baseline would interfere with the acquisition of knowledge from baseline to the 3-month follow-up in both FOY and PHAT groups. Further, the format and content of FOY were expected to facilitate increased knowledge by reducing the interference of baseline HIV stigma.
METHODS
Participants
This study used baseline and 3-month follow-up data collected from 1654 African American adolescents during Project iMPPACS, a multilevel, multi-site HIV prevention-intervention (18). Participants were recruited using community-based outreach in two midsized matched cities in the northeastern U.S. and two midsized matched cities in the southeastern U.S. Eligibility criteria included age 13 to 18 years at the beginning of the study and being able to speak and read English. Of the 2146 adolescents invited to participate, 1654 were consented, assented and were assessed at baseline (77%). Of those who completed the baseline assessment, 1542 completed the 3-month follow-up (93%). All participants completing the baseline assessment were included in this study. Demographics for this sample are listed in Table 1.
Table 1.
Baseline characteristics of participants
| PHAT (n = 833) | FOY (n = 821) | |
|---|---|---|
| Site | ||
| Syracuse | 210 (25%) | 205 (25%) |
| Macon | 208 (25%) | 204 (25%) |
| Providence | 206 (25%) | 205 (25%) |
| Columbia | 209 (25%) | 207 (25%) |
| Age (Mean) | 15.08 (1.10) | 15.09 (1.09) |
| Gender (% Female) | 496 (60%) | 495 (60%) |
| Ethnicity (% Hispanic) | 31 (4%) | 47 (6%) |
| Free lunch (% Yes) | 618 (74%) | 598 (73) |
| Attends religious services | ||
| Never | 89 (11%) | 85 (10%) |
| Rarely | 257 (31%) | 301 (37%) |
| Monthly | 150 (18%) | 130 (16%) |
| Weekly | 337 (41%) | 305 (37%) |
| Sexually active (% Yes) | 502 (60%) | 486 (59%) |
Procedures
Participants were randomly assigned to either Focus on Youth (FOY; n = 821) or a general health promotion control group Promoting Health among Teens (PHAT; n = 833). Attrition rates were similar across both conditions (FOY: 6.3%; PHAT: 7.2%). After obtaining parental consent and participant assent, participants completed psychosocial measures using an audio computer-assisted self-interview (ACASI). The ACASI took approximately 45 minutes to complete and participants were compensated $30 for their time and effort.
Measures
The measures included participants’ report of demographic information, sexual activity, HIV-related knowledge, and HIV-related stigma. The reliability of measures used in Project iMPPACS has been reported previously (19). Participants’ previous sexual activity was obtained from one question asking whether they had ever had sexual intercourse, defined as every having vaginal or anal intercourse. HIV-knowledge was assessed using an 18-item scale (HIV-KQ-18) with three response options, mostly true, mostly false, or don’t know (19). Correct answers were summed, with a possible range of 0 to 18. The internal consistency of the HIV-KQ-18 for this study was α = .77 at baseline and α = .74 at the 3-month follow-up. Participants’ negative attitudes toward persons with HIV (e.g., “People who have HIV should be ashamed” and “I do not want to be friends with someone who has HIV”) were assessed using 7-items that were rated on a 6-point scale (1 = strongly disagree to 6 = strongly agree; (20). The internal consistency for this measure was α = .84 at baseline and α = .86 at the 3-month follow-up.
Analytical approach
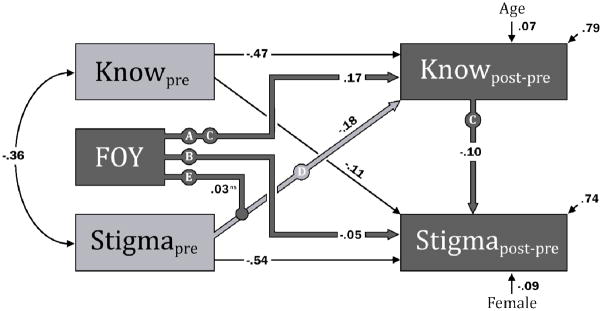
Covariance modeling was used to examine the study hypotheses. Covariance modeling allowed multiple outcomes to be simultaneously estimated, allowed for tests of indirect effects (e.g., treatment affecting stigma by way of increasing knowledge), and allowed us to account for the reciprocal influences between knowledge and stigma. A single model was used to test the hypotheses of this study (Figure 1). The model simultaneously regressed change in HIV knowledge and stigma on a treatment indicator (0=PHAT, 1=FOY), as well as on baseline measures of knowledge and stigma. Age, gender, and sexual experience were included as covariates. The moderating effect of FOY on the relationship between baseline stigma and change in knowledge was tested by including an interaction term consisting of baseline stigma and the treatment indicator. Maximum likelihood was used to derive the parameter estimates. Bias-corrected bootstrapped confidence intervals (2,000 draws) were used to provide robust inference for parameters in the model, especially for the indirect effects hypothesized in the model (21). All analyses were performed using Mplus 6.0 (22).
Figure 1.
Standardized model of HIV Knowledge and HIV Stigma.
Explanatory footer: Although estimated, non-significant parameters were not presented in the figure. Analyses also controlled for sexual experience, which was not related to any parameters included in the model. Letters were used to label paths discussed in text: A) the direct effect of treatment on HIV-knowledge, B) the direct effect of treatment on HIV-stigma, C) the indirect effect of treatment on HIV-stigma via HIV-knowledge, D) the effect of baseline HIV-stigma on change in HIV-knowledge, and E) the moderating effect of treatment on path D. ns = not significant.
RESULTS
Treatment Effects
The effects of FOY vs. PHAT were tested by examining the direct effect of treatment on change in HIV knowledge (Figure 1: Path A) and the total effect of treatment on HIV stigma (Figure 1: Path B + Path C). As expected, FOY showed more change in knowledge (unstandardized (b) = 1.16 (95% CI = .85 to 1.46); standardized (β) = .17) and more change in stigma (b = −.89 (−1.48 to −.36); β = −.07). The effect sizes for these differences were Cohen’s d = .30 and d = .09, respectively.
Direct and Indirect effects for HIV stigma
The effect of treatment on HIV stigma was separated into the indirect effect through change in knowledge (Figure 1: Path C) and the direct effect of treatment on stigma (Figure 1: Path B). Both the indirect effect (b = −.23 (−.38 to −.11); β = −.02) and direct effect of FOY (b = −.66 (−1.26 to −.12); β = −.05) were significant.
Longitudinal Relationships HIV Knowledge and Stigma
As expected, HIV Knowledge and HIV Stigma were related at the baseline (r = −.36) and across time. Controlling for baseline relationships, higher Stigma at the pre-assessment was related to fewer gains in HIV Knowledge (Figure 1: Path D; b = −.08 (−.11 to −.05); β = −.18). Similarly, higher HIV knowledge at pre-assessment was related to reduced HIV Stigma (b = −.19 (−.29 to −.08); β = −.11). Contrary to expectations, treatment condition did not moderate the relationship between baseline stigma and change in HIV-knowledge (Figure 1: Path E; b = .02 (−.02 to .06); β = .03).
DISCUSSION
This study examined the longitudinal relationships between HIV-related knowledge and stigma using data from a large, multi-site trial of a validated skills-based youth intervention, Focus on Youth (FOY). Overall, we found support for our hypotheses that FOY would result in improved HIV knowledge and reduced stigma. Change in knowledge, although not sufficient to reduce risk behavior, is likely necessary for risk reduction (23); if true, then improving knowledge in at-risk youth is important, especially given the low levels of initial HIV-related knowledge among these youth (i.e., 50% correct; (24).
Improvements in knowledge were demonstrated by the FOY group; youth participating in this group showed a moderate increase in knowledge compared to youth in the control intervention (Cohen’s d = .30). This effect size observed is similar to other efficacious interventions (25). A smaller effect was seen for HIV-related stigma (d = .09). Consistent with previous literature, the effect on HIV stigma was composed of an indirect relationship through change in HIV knowledge, and a direct relationship from FOY. This direct relationship likely represents the effect of including multiple modalities of intervention, such as didactics, skill building and personalizing risk. This finding is similar to findings in infected youth that suggest interventions that combine treatment modalities more effectively reduce stigma than those that rely solely on didactic approaches (15).
Although FOY impacted HIV stigma in multiple ways as hypothesized, the total effect was minimal. This small impact could be due to the primary focus of FOY on reducing risk behavior rather than an explicit focus on HIV stigma. Additionally, the hypothesis for stigma reduction was derived from a literature that largely addressed reducing stigma in HIV-infected individuals, and while the pattern of results was consistent with the literature, the impact of stigma on HIV knowledge could be different for non-infected individuals. These results suggest caution when generalizing from HIV-infected individuals to non-infected youth (7).
Our second set of hypotheses addressed the longitudinal relationships between HIV stigma and knowledge. Because adolescents with higher levels of stigma were expected to be less likely to identify with youth whom they perceived as being risky, they were thought to be less likely to internalize the intervention. Stigma, therefore, was expected to block the acquisition of HIV-related knowledge. It was further hypothesized that if the intervention effectively reduced stigma, the antagonistic relationship between stigma and knowledge would be lower in FOY versus PHAT. The first hypothesis was supported, the second was not. The model showed that baseline stigma interfered with knowledge acquisition. After adjusting for the baseline relationship between HIV knowledge and stigma, those who reported more HIV stigma at baseline showed less improvement in knowledge. This relationship, however, was the same for both FOY and PHAT, which although contrary to what we expected, was consistent with the previously discussed weak treatment effect for HIV stigma. Results from this study suggest that HIV-related stigma likely interferes with the acquisition of HIV-related knowledge, and suggests that current approaches employed in validated interventions may not be sufficient to adequately reduce stigma.
There are a number of limitations that should be considered when interpreting findings from this study. First, the modeling tested directional causal relationships between HIV knowledge and HIV stigma; these assumptions, however, cannot be verified using the current study, as it was not designed to test the causal relationships between these two variables. Second, all of the measures used in the study were self-report and any relationships due to common assessment modality cannot be assessed using these data. Third, the FOY intervention was not specifically designed to reduce stigma. However, FOY is validated and widely implemented (17,26), and it illustrates how HIV-related stigma may interfere with group-based interventions and suggests current practices may not be sufficient to reduce stigma in at-risk youth. Finally, the sample was randomly selected, and caution should be used when generalizing to other populations and other geographical regions
This study is among the first to explore the role of HIV stigma in group-based prevention programs used with at-risk adolescents. There is also some evidence in adults that HIV stigma interferes with HIV knowledge and behavioral intentions to engage in safer sexual practices (14). Unfortunately, little is known about reducing HIV-related stigma in non-infected youth and there is a need for more research on how to reduce stigma in at-risk youth (16). It is also important to understand how to incorporate stigma reduction into existing efficacious HIV prevention interventions. Reducing HIV-related stigma in at-risk youth promises to remove a frequently cited barrier to prevention efforts, as well as boosting the efficacy of group-based HIV prevention interventions.
Table 2.
HIV Knowledge and HIV Stigma Pre- and Post-intervention
| PHAT (n = 833) | FOY (n = 821) | |
|---|---|---|
| Mean (stderr) | ||
| HIV Knowledge: Pre | 9.02 (0.13) | 9.07 (0.14) |
| HIV Knowledge: Post | 9.99 (0.14) | 11.13 (0.14) |
| HIV Stigma: Pre | 16.31 (0.26) | 16.81 (0.27) |
| HIV Stigma: Post | 14.88 (0.26) | 14.26 (0.26) |
Acknowledgments
Funding: This research was supported by National Institutes of Health grant UO1MH066785, a collaborative project awarded to participating sites: Rhode Island Hospital, Emory University, Syracuse University, University of South Carolina, and University of Pennsylvania and by a National Institutes of Mental Health Program in Child/Adolescent Biobehavioral HIV Research Training at Rhode Island Hospital/Brown University (T32-MH-07878, PI: L. Brown).
References
- 1.Fortenberry JD, McFarlane M, Bleakley A, Bull S, Fishbein M, Grimley DM, et al. Relationships of stigma and shame to gonorrhea and HIV screening. Am J Public Health. 2002;92(3):378–381. doi: 10.2105/ajph.92.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klein SJ, Karchner WD, O’Connell DA. Interventions to prevent HIV-related stigma and discrimination: findings and recommendations for public health practice. J Public Health Manag Pract. 2002;8(6):44–53. doi: 10.1097/00124784-200211000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Mahajan AP, Sayles JN, Patel VA, Remien RH, Ortiz D, Szekeres G, et al. Stigma in the HIV/AIDS epidemic: A review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):S67–S79. doi: 10.1097/01.aids.0000327438.13291.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Valdiserri RO. HIV/AIDS stigma: An impediment to public health. Am J Public Health. 2002;92(3):341–342. doi: 10.2105/ajph.92.3.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bartlett JG, Branson BM, Fenton K, Hauschild BC, Miller V, Mayer KH. Opt-out testing for human immunodeficiency virus in the united states: Progress and challenges. JAMA. 2008;300(8):945–951. doi: 10.1001/jama.300.8.945. [DOI] [PubMed] [Google Scholar]
- 6.Darrow WW, Montanea JE, Gladwin H. AIDS-related stigma among Black and Hispanic young adults. AIDS Behav. 2009;13(6):1178–1188. doi: 10.1007/s10461-009-9601-7. [DOI] [PubMed] [Google Scholar]
- 7.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nyblade L. Measuring HIV stigma: Existing knowledge and gaps. Psychol Health Med. 2006;11(3):335–345. doi: 10.1080/13548500600595178. [DOI] [PubMed] [Google Scholar]
- 9.Moore S, Rosenthal D. Adolescent invulnerability and perceptions of AIDS risk. J Adolescent Res. 1991;6(2):164–180. [Google Scholar]
- 10.Macintyre K, Rutenberg N, Brown L, Karim A. Understanding perceptions of HIV risk among adolescents in KwaZulu-Natal. AIDS Behav. 2004;8(3):237–250. doi: 10.1023/B:AIBE.0000044072.71361.b3. [DOI] [PubMed] [Google Scholar]
- 11.Heijnders M, Van Der Meij S. The fight against stigma: An overview of stigma-reduction strategies and interventions. Psychol Health Med. 2006;11(3):353. doi: 10.1080/13548500600595327. [DOI] [PubMed] [Google Scholar]
- 12.Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 2003;57(1):13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- 13.Yang H, Li X, Stanton B, Fang X, Lin D, Naar-King S. HIV-related knowledge, stigma, and willingness to disclose: A mediation analysis. AIDS Care. 2006;18(7):717–724. doi: 10.1080/09540120500303403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kalichman S, Simbayi L, Cain D, Jooste S, Skinner D, Cherry C. Generalizing a model of health behaviour change and AIDS stigma for use with sexually transmitted infection clinic patients in Cape Town, South Africa. AIDS Care. 2006;18(3):178–182. doi: 10.1080/09540120500456292. [DOI] [PubMed] [Google Scholar]
- 15.Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: what have we learned? AIDS Educ Prev. 2003;15(1):49–69. doi: 10.1521/aeap.15.1.49.23844. [DOI] [PubMed] [Google Scholar]
- 16.Sengupta S, Banks B, Jonas D, Miles MS, Smith GC. HIV interventions to reduce HIV/AIDS stigma: A systematic review. AIDS Behav. 2010 doi: 10.1007/s10461-010-9847-0. Available at: http//www.springerlink.com/index/10.1007/s10461-010-9847-0. [DOI] [PMC free article] [PubMed]
- 17.Stanton BF, Li X, Ricardo I, Galbraith J, Feigelman S, Kaljee L. A randomized, controlled effectiveness trial of an AIDS prevention program for low-income African-American youths. Arch Pediatr Adolesc Med. 1996;150(4):363–372. doi: 10.1001/archpedi.1996.02170290029004. [DOI] [PubMed] [Google Scholar]
- 18.Romer D, Sznitman S, DiClemente R, Salazar LF, Vanable PA, et al. Mass media as an HIV-prevention strategy: Using culturally-sensitive messages to reduce HIV-associated sexual behavior of at-risk African-American youth. AM J Public Health. 2009;99(12):2150–2159. doi: 10.2105/AJPH.2008.155036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carey MP, Schroder KEE. Development and psychometric evaluation of the brief HIV knowledge questionnaire. AIDS Educ Prev. 2002;14(2):172–182. doi: 10.1521/aeap.14.2.172.23902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalichman SC, Simbayi LC, Jooste S, Toefy Y, Cain D, Cherry C, et al. Development of a brief scale to measure AIDS-related stigma in South Africa. AIDS Behav. 2005;9(2):135–143. doi: 10.1007/s10461-005-3895-x. [DOI] [PubMed] [Google Scholar]
- 21.MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivar Behav Res. 2004;39(1):99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Muthén L, Muthén B. Mplus User’s Guide. 5. Los Angeles, CA: Muthen & Muthén; 1998. [Google Scholar]
- 23.Donovan B, Ross MW. Preventing HIV: determinants of sexual behaviour. Lancet. 2000;355(9218):1897–1901. doi: 10.1016/S0140-6736(00)02302-3. [DOI] [PubMed] [Google Scholar]
- 24.Swenson R, Rizzo CJ, Brown LK, Vanable P, Carey M, Valois RF, et al. HIV knowledge and its contributions to sexual health behaviors of low-income African American adolescents. J Natl Med Assoc. doi: 10.1016/s0027-9684(15)30772-0. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Albarracín D, Gillette JC, Earl AN, Glasman LR, Durantini MR, Ho M. A test of major assumptions about behavior change: A comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychol Bull. 2005;131(6):856–897. doi: 10.1037/0033-2909.131.6.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu Y, Stanton BF, Galbraith J, Kaljee L, Cottrell L, Li X, et al. Sustaining and broadening intervention impact: A longitudinal randomized trial of 3 adolescent risk reduction approaches. Pediatrics. 2003;111(1):e32–e38. doi: 10.1542/peds.111.1.e32. [DOI] [PubMed] [Google Scholar]