Abstract
Low-grade myofibroblastic sarcoma (LGMS) is a rare, malignant tumor with myofibroblastic differentiation. Despite it being classified as a distinct entity by the World Health Organization, a few cases were reported in the oral and maxillofacial region. Here, a LGMS developed on the palate of a 73-year-old man who presented with a 1-cm tumor on the posterior border of the palate. Based on the histological and immunohistochemical features, a diagnosis of LGMS was established. The tumor was resected, and no recurrence was observed over 2 years. Although the tongue is the most preferred site for LGMS, it may occur in any region of the oral cavity.
Keywords: low-grade myofibroblastic sarcoma, oral, palate
Introduction
Myofibroblasts are derived from fibroblasts, and exist in various tissues such as normal connective tissues, granulation tissue and reactives inflammatory tissues.1 Occasionally, myofibroblasts undergo tumorgenic transformation and become malignant.2 A low-grade myofibroblastic sarcoma (LGMS) is a rare malignant tumor with myofibroblastic differentiation, and just a few cases have been reported in the oral and maxillofacial region.3 Here, we describe a patient with LGMS of the palate, and bibliographic considerations are reviewed.
Case report
A 73-year-old man was referred by his general dental practitioner to the Department of Oral and Maxillofacial Surgery (Kochi University, Kochi, Japan) regarding a tumor on the palate that had developed over a couple of months. There was no associated pain, or paraesthesia. A systematic examination revealed a fit and healthy man. His medical histories included a gastric ulcer, prostatic hyperplasia and cervical spondylotic radiculopathy. Physical examination revealed an elastic hard, 10 mm×10 mm mass on the posterior border of the palate. The mass was fixed to the underlying tissues with distinct margins. The surface mucosa was slightly reddish and irregular (Figure 1). An excisional biopsy of the palatal mass was performed, and microscopic examination revealed infiltrative spindle tumor cells surrounded by a fibrous capsule. The tumor cells were dense in some parts but sparse in other areas. The tumor cells had round-shaped or spindle nuclei, and the cytoplasm was eosinophilic. There were few mitotic cells, however, and atypical cells with large nuclei were observed (Figure 2).
Figure 1.
Intraoral photo at the initial visit. An elastic, hard, 10 mm×10 mm mass is seen on the posterior border of the palate.
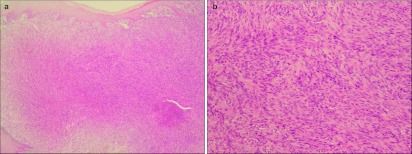
Figure 2.
Histology of the tumor. The tumor cells had round-shaped or spindle nuclei, and the cytoplasm was eosinophilic. Mitotic cells were sparse, and atypical cells with large nuclei were observed. Hematoxylin and eosin staining, a: ×40; b: ×200.
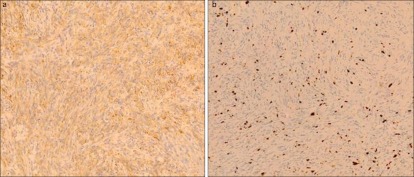
Immunohistochemistry revealed that most spindle cells were immunoreactive for muscle-specific actin (HHF35), and focally for α-smooth muscle actin (α-SMA) and MIB-1 (Figure 3), in contrast, immunostaining for other markers, such as CD34, CD68, desmin, epithelial membrane antigen (EMA), S-100 protein, cytokeratin (AE1/AE3), and p53 was not observed (Table 1). The patient was therefore diagnosed with LGMS. The surgical sample margins appeared to be tumor-free upon histological analysis. The patient was disease-free at the last examination, 2 years postoperatively (Figure 4).
Figure 3.
Immunohistochemical staining of the tumor. The spindle cells were focally immunoreactive for α-SMA (a: ×200) and MIB-1 (b: ×200). α-SMA, α-smooth muscle actin.
Table 1. Immunohistochemical findings.
| Markers | Immunoreactivity |
|---|---|
| α-SMA | + |
| Muscle-specific actin | + |
| EMA | − |
| S-100 | − |
| AE1/AE3 | − |
| CD34 | − |
| MIB-1 LI | 10% |
EMA, epithelial membrane antigen; α-SMA, α-smooth muscle actin.
Immunohistochemistry revealed that most spindle cells were immunoreactive for muscle specific actin, and focally for α-SMA and MIB-1, whereas immunostaining for other markers such as EMA, S-100 protein, cytokeratin (AE1/AE3) and CD34 was not observed.
Figure 4.
Intraoral photo 2 years after removal of the tumor. There is only scar on the posterior border of the palate, and no reoccurrence was observed.
Discussion
Myofibroblasts are mesenchymal spindle cells that are first observed in the granulation tissue of healing wounds, and play a role in the production of contractile force.1 Myofibroblasts exist under various reactive conditions, including reparative granulation tissue, granulomas, inflammatory pseudotumors, and various benign and malignant soft tissue tumors.4 LGMS used to be a controversial neoplasm, but has been reclassified as a distinct entity in the newly published World Health Organization classification of soft tissue tumors.2 However, intermediate- and high-grade myofibroblastic sarcomas were also documented in the literature.5,6,7 High-grade (pleomorphic) myofibroblastic sarcomas were described as pleomorphic sarcomas composed of atypical spindle, polygonal and giant cells showing the ultrastructural features of myofibroblastic differentiation and numerous mitotic figures.8
Histologically, LGMS is composed of slender spindle cells arranged in interlacing fascicles. The tumor cells have a scanty to moderate amount of eosinophilic or amphophilic cytoplasm and fusiform nuclei with mild nuclear pleomorphism and a low mitotic rate. Immunohistochemically, myofibroblastic sarcoma is immunopositive for vimentin, SMA, muscle-specific actin, calponin and fibronectin, rarely immunopositive for desmin, and immunonegative for laminin and type IV collagen.3,9 Furthermore, LGMS are no immunoreactive for s-100, EMA, cytokeratin or CD34.10 LGMS is easily confused with myofibroblasts composed of nodular fasciitis because of their morphological similarity and overlapping immunophenotype.11 However, unlike myofibroblastic sarcoma, the appearance is not monomorphic.12 In addition to nodular fasciitis, LGMS is differentiated from leiomyosarcoma, malignant fibrous histiocytoma, inflammatory myofibroblastic tumor and fibromatosis. Leiomyosarcoma has a well-delineated pushing margin and show longitudinally fibrillary cytoplasm and cigar-shaped vesicular nuclei with paranuclear vacuolation.7 Malignant fibrous histiocytoma shows anaplasia and multinucleated giant cells and marked cytological pleomorphism and nuclear atypia.7 Inflammatory myofibroblastic tumor is composed of myofibroblast and fibroblasts with inflammatory cell infiltration.7 Fibromatosis is characterized by fibroblasts and myofibroblasts in parallel alignment, but cytologic atypia and nuclear pleomorphism are absent.10 The specimen from our case was immunopositive for SMA and muscle-specific actin, and was immunonegative for EMA, s-100, AE1/AE3 and CD34. Histologically, infiltrative spindle tumor cells showed a myofibroblastic differentiation, and there were several atypical cells. Based on these findings, it was diagnosed as a LGMS.
LGMS mainly occurs in adults, and most frequently affects the deep soft tissues of the oral cavity (especially the tongue), limbs, trunk, or abdominal and pelvic cavities.2,13 The head and neck region, including the oral cavity, is the preferred location for LGMS; however, only few cases were reported of LGMS occurring in the oral and maxillofacial region.10 In the literature, there are 38 cases of LGMS in the oro-maxillofacial region, including our case (Table 2). The average age was 40.7 years (range: 2–85 years, median: 41 years), and the male to female ratio was 4∶3. The tongue was the most preferred site, followed by the maxilla and palate, mandible, nasal/paranasal cavity and deep tissue spaces including the parapharyngeal space. Our patient is the third case occurring in the palate.
Table 2. LGMS in the oral and maxillofacial region.
| Case | Reference | Gender | Age/year | Site | Size/cm | Treatment | Reoccurrence |
|---|---|---|---|---|---|---|---|
| 1 | 16 | M | 75 | Parietal | NA | NA | Y |
| 2 | 16 | M | 85 | Face | NA | NA | N |
| 3 | 17 | F | 43 | Face | 1.5 | NA | N |
| 4 | 18 | F | 12 | Maxilla | 6.0 | NA | Y |
| 5 | 18 | M | 18 | Maxilla | NA | NA | Y |
| 6 | 18 | F | 9 | Mandible | NA | NA | Y |
| 7 | 18 | F | 13 | Tonsil | NA | NA | N |
| 8 | 18 | F | 9 | Mandible | NA | NA | N |
| 9 | 9 | F | 51 | Tongue | 2.5 | Local excision | N |
| 10 | 9 | M | 70 | Tongue | 1.4 | Local excision | N |
| 11 | 9 | M | 24 | Tongue | 1.5 | Local excision | N |
| 12 | 9 | M | 66 | Tongue | 1.8 | Wide excision | N |
| 13 | 9 | M | 19 | Mandible | 3.5 | Local excision, RT, CT | N |
| 14 | 19 | F | 71 | Parotid gland | 1.7 | Wide excision | N |
| 15 | 5 | M | 24 | Maxillary sinus | 4.0 | Wide excision | N |
| 16 | 5 | M | 49 | Maxilla | 8.0 | Wide excision | Y |
| 17 | 3 | M | 41 | Hard palate | 3.5 | Wide excision | N |
| 18 | 3 | M | 35 | Palate | 1.6 | Local excision | Y |
| 19 | 3 | F | 54 | Gingiva | 1.5 | Local excision | Y |
| 20 | 20 | F | 77 | Nasal cavity | 3.0 | Local excision | Y |
| 21 | 14 | F | 8 | Pterygoid region | 6.0 | Wide excision, CT | N |
| 22 | 14 | F | 2 | Temporal fossa | 2.9 | Wide excision | N |
| 23 | 21 | F | 37 | Cheek | 2.0 | Wide excision | N |
| 24 | 22 | F | 24 | Tongue | 2.0 | Local excision | N |
| 25 | 23 | M | 42 | Parapharyngeal space | NA | RT, CT | Y (dead) |
| 26 | 12 | M | 41 | Tongue | 1.7 | Local excision | Y |
| 27 | 24 | M | 28 | Lower lip | 2.0 | local excision | NA |
| 28 | 7 | M | 74 | Nasal cavity | 3.0 | NA | Y |
| 29 | 7 | M | 14 | Ethmoid sinus | 4.5 | NA | Y |
| 30 | 7 | M | 14 | Nasal cavity | 5.0 | NA | Y |
| 31 | 10 | M | 51 | Mandible | 3.0 | Wide excision | N |
| 32 | 10 | F | 61 | Tongue | 4.0 | Wide excision | N |
| 33 | 4 | F | 56 | Tongue base | 2.0 | Local excision, RT | N |
| 34 | 15 | M | 54 | Mandible | 6.0 | Local excision | N |
| 35 | current case | M | 73 | Palate | 1.0 | Local excision | N |
CT, chemotherapy; RT, radiotherapy.
The recurrence rate (RR) was 38.2%, including one fatal case. RR was the highest when tumor is sited in nasal cavity/paranasal sinus. Second is jawbone, followed by deep tissue space (Table 3). RR was 21.4% when tumor size was less than 3 cm, whereas that of over 3-cm tumor was 46.2%. As LGMS is associated with little symptoms, early detection may be difficult when tumors are in deep tissues, such as nasal cavity, paranasal sinus, jawbone and masticatory space, resulting high RR.
Table 3. Reoccurrence and tumor site.
| Site | Reoccurrence cases/total cases | reoccurrence rate/% |
|---|---|---|
| Tongue | 1/8 | 12.5 |
| Jaw (incl. gingiva) | 5/9 | 55.5 |
| Nasal cavity/paranasal sinus | 4/5 | 80.0 |
| Palate | 1/3 | 33.3 |
| Deep tissue space | 2/4 | 50.0 |
| Others | 0/5 | 0.0 |
| Total | 13/34 | 38.2 |
Reoccurrence rate is the highest when tumor is sited in nasal cavity/paranasal sinus. Second is jawbone, followed by deep tissue space.
LGMS may cause focal recurrences and metastasis, and it has a relatively indolent course.7,14 It tends to recur locally rather than to metastasize.15 Radiotherapy or chemotherapy are not established treatments, and the importance of surgery is emphasized.14 Our case showed no recurrence 2 years postoperatively, but further observation is required.
References
- Tomasek JJ, Gabbiani G, Hinz B, et al. Myofibroblasts and mechano-regulation of connective tissue remodeling. Nat Rev Mol Cell Biol. 2002;3 5:349–363. doi: 10.1038/nrm809. [DOI] [PubMed] [Google Scholar]
- Mentzel T, Fletcher JA.Low grade myofibroblastic sarcomaIn: Fletcher CD, Unni KK, Mertens F ed. Pathology and genetics of tumours of soft tissue and bone. Lyon; IARC Press; 200294–95. [Google Scholar]
- Montgomery E, Goldblum JR, Fisher C. Myofibrosarcoma: a clinicopathologic study. Am J Surg Pathol. 2001;25 2:219–228. doi: 10.1097/00000478-200102000-00010. [DOI] [PubMed] [Google Scholar]
- Takacsi-Nagy Z, Murakozy G, Pogany P, et al. Myofibroblastic sarcoma of the base of tongue. Case report and review of the literature. Strahlenther Onkol. 2009;185 3:198–201. doi: 10.1007/s00066-009-1925-8. [DOI] [PubMed] [Google Scholar]
- Bisceglia M, Tricarico N, Minenna P, et al. Myofibrosarcoma of the upper jawbones: a clinicopathologic and ultrastructural study of two cases. Ultrastruct Pathol. 2001;25 5:385–397. doi: 10.1080/019131201317101261. [DOI] [PubMed] [Google Scholar]
- Meng GZ, Zhang HY, Bu H, et al. Myofibroblastic sarcoma of the nasal cavity and paranasal sinus: a clinicopathologic study of 6 cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104 4:530–539. doi: 10.1016/j.tripleo.2006.08.021. [DOI] [PubMed] [Google Scholar]
- Meng GZ, Zhang HY, Bu H, et al. Myofibroblastic sarcomas: a clinicopathological study of 20 cases. Chin Med J. 2007;120 5:363–369. [PubMed] [Google Scholar]
- Fisher C. Myofibroblastic malignancies. Adv Anat Pathol. 2004;11 4:190–201. doi: 10.1097/01.pap.0000131773.16130.aa. [DOI] [PubMed] [Google Scholar]
- Mentzel T, Dry S, Katenkamp D, et al. Low-grade myofibroblastic sarcoma: analysis of 18 cases in the spectrum of myofibroblastic tumors. Am J Surg Pathol. 1998;22 10:1228–1238. doi: 10.1097/00000478-199810000-00008. [DOI] [PubMed] [Google Scholar]
- Demarosi F, Bay A, Moneghini L, et al. Low-grade myofibroblastic sarcoma of the oral cavity. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108 2:248–254. doi: 10.1016/j.tripleo.2009.03.031. [DOI] [PubMed] [Google Scholar]
- Meng GZ, Zhang HY, Zhang Z, et al. Myofibroblastic sarcoma vs nodular fasciitis: a comparative study of chromosomal imbalances. Am J Clin Pathol. 2009;131 5:701–709. doi: 10.1309/AJCPV6H2WSYXLKFB. [DOI] [PubMed] [Google Scholar]
- Jay A, Piper K, Farthing PM, et al. Low-grade myofibroblastic sarcoma of the tongue. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104 5:e52–e58. doi: 10.1016/j.tripleo.2007.06.004. [DOI] [PubMed] [Google Scholar]
- Fujiwara M, Yuba Y, Wada A, et al. Myofibrosarcoma of the nasal bone. Am J Otolaryngol. 2005;26 4:265–267. doi: 10.1016/j.amjoto.2004.11.017. [DOI] [PubMed] [Google Scholar]
- Keller C. Low-grade myofibrosarcoma of the head and neck: importance of surgical therapy. J Pediatr Hematol Oncol. 2004;26 2:119–120. doi: 10.1097/00043426-200402000-00013. [DOI] [PubMed] [Google Scholar]
- Niedzielska I, Janic T, Mrowiec B. Low-grade myofibroblastic sarcoma of the mandible: a case report. J Med Case Reports. 2009;10 3:8458. doi: 10.4076/1752-1947-3-8458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyden BP, Banerjee SS, Harris M, et al. A study of spindle cell sarcomas showing myofibroblastic differentiation. Ultrastruct Pathol. 1991;15 4/5:367–378. doi: 10.3109/01913129109016246. [DOI] [PubMed] [Google Scholar]
- Eyden BP, Christensen L, Tagore V, et al. Myofibrosarcoma of subcutaneous soft tissue of the cheek. J Submicrosc Cytol Pathol. 1992;24 3:307–313. [PubMed] [Google Scholar]
- Smith DM, Mahmoud HH, Jenkins JJ, 3rd, et al. Myofibrosarcoma of the head and neck in children. Pediatr Pathol Lab Med. 1995;15 3:403–418. doi: 10.3109/15513819509026976. [DOI] [PubMed] [Google Scholar]
- Bisceglia M, Magro G. Low-grade myofibroblastic sarcoma of the salivary gland. Am J Surg Pathol. 1999;23 11:1435–1436. doi: 10.1097/00000478-199911000-00021. [DOI] [PubMed] [Google Scholar]
- Kondo S, Yoshizaki T, Minato H, et al. Myofibrosarcoma of the nasal cavity and paranasal sinus. Histopathology. 2001;39 2:216–217. doi: 10.1046/j.1365-2559.2001.1232e.x. [DOI] [PubMed] [Google Scholar]
- Artopoulou II, Lemon JC, Clayman GL, et al. Stent fabrication for graft immobilization following wide surgical excision of myofibroblastic sarcoma of the buccal mucosa: a clinical report. J Prosthet Dent. 2006;95 4:280–285. doi: 10.1016/j.prosdent.2006.02.023. [DOI] [PubMed] [Google Scholar]
- Laco J, Simakova E, Slezak R, et al. Low grade myofibroblastic sarcoma of tongue: a case report. Cesk Patol. 2006;42 3:150–153. [PubMed] [Google Scholar]
- Takahama A, Jr, Nascimento AG, Brum MC, et al. Low-grade myofibroblastic sarcoma of the parapharyngeal space. Int J Oral Maxillofac Surg. 2006;35 10:965–968. doi: 10.1016/j.ijom.2006.03.027. [DOI] [PubMed] [Google Scholar]
- Imanguli MM, Karai LJ, Shanti RM, et al. Myofibroblastic tumor of the lower lip in a patient with X-linked hypogammaglobulinemia and isolated growth hormone deficiency: a case report. J Oral Maxillofac Surg. 2007;65 6:1219–1222. doi: 10.1016/j.joms.2005.12.041. [DOI] [PubMed] [Google Scholar]